Abstract
Bladder being a content of inguinal hernias is a rare event and it being the sole component is extremely uncommon. Usually, elderly obese males are affected and symptomatology depends on the extent of bladder involvement. However, recognition of this entity is important in the treatment of LUTS as well as to avoid inadvertent bladder injury during hernia repair.
Keywords: Bilateral, bladder, inguinal hernia
INTRODUCTION
Bladder can be a component of various hernias like inguinal, femoral, obturator, ischiorectal or those of the abdominal wall. Up to four percent of inguinal hernias have bladder as a content. Bladder being the sole component in inguinal hernias is very rare.[1] We report a case of bilateral inguinal vesical hernia, which, to the best of our knowledge, has not been reported previously in literature.
CASE REPORT
A 50-year-old gentleman presented with dull right flank pain since three months. There was no hematuria, weight loss or lower urinary tract symptoms (LUTS). Physical examination was unremarkable. Contrast enhanced computed tomogram (CECT) revealed a right interpolar hypervascular renal mass suggestive of renal cell carcinoma.
The CECT incidentally picked up bilateral inguinal hernias with bladder protruding anteroinferiorly on both sides. The herniating bladder was seen as a fluid-filled structure contiguous with the rest of the bladder bilaterally, which was easily demonstrated on the axial images [Figure 1] with further confirmation of the same on reformatted sagittal and coronal sections [Figure 2]. There was no evidence of bowel or any other structure in the hernia. This gave the appearance of a ‘Mickey mouse’, with the bladder protrusion into bilateral hernias mimicking its ears and rest of the bladder resembling its face.
Figure 1.
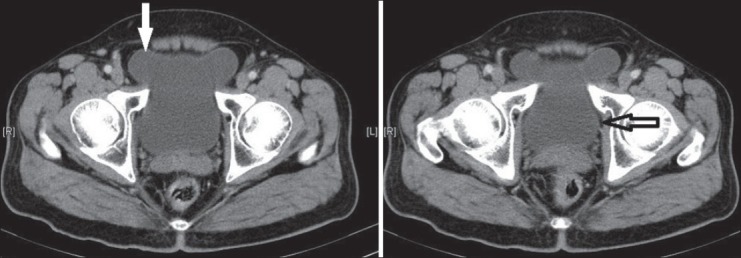
Axial image – Bilateral vesical inguinal hernia resembling ‘Mickey mouse’. White arrow: ‘Mickey mouse’ ears, black arrow: ‘Mickey mouse’ face
Figure 2.
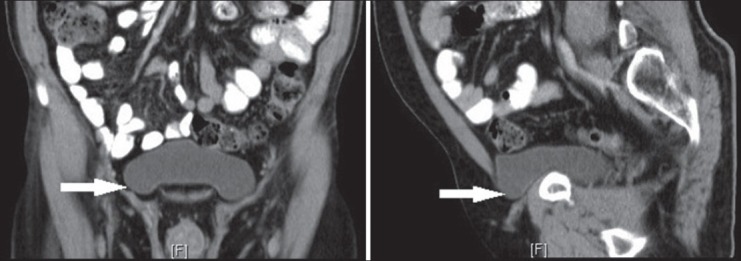
Coronal and sagittal images – Bilateral inguinal vesical hernia (white arrows)
DISCUSSION
Inguinoscrotal vesical hernias are rare. Bladder herniation can involve a small portion to more than half of the bladder–termed as ‘massive inguinoscrotal hernia’. In infants, protrusion of the lateral aspect of bladder base may be normally seen (bladder ears) and should not be misinterpreted as bladder hernia.[2]
Males are affected more commonly than females (2.3:1). Predisposing conditions include lax abdominal wall, decreased bladder tone, weakness of pelvic floor, pelvic mass lesions, obesity, trauma and history of LUTS or hernia repair. A mere seven percent of bladder hernias are diagnosed preoperatively with 16% picked up postoperatively due to complications and the rest diagnosed intraoperatively.[1,2,3,4]
Patients may be asymptomatic or present with an inguinoscrotal swelling which reduces after voiding. Uncommonly, two-stage micturition may be reported, with second micturition done by external compression of the swelling (Mery's syndrome).[3,4]
Imaging is not indicated routinely and these are usually detected incidentally. Urographic studies show wide-mouthed, rounded protrusion of the bladder wall directed inferolaterally. Indirect signs include lateral ureteral displacement, small bladder volume and incomplete bladder base visualization.[2]
The yield of hernia on ultrasound can be increased using Valsalva maneuver, making the patient stand, or two stage voiding.[3] CECT and magnetic resonance imaging are comprehensive tools for detection of presence and complications of bladder hernia. These may reveal bladder pointing towards the side of the hernia with bladder base angulated anteroinferiorly.[2]
We report this case for its unique nature and peculiar radiological findings.
CONCLUSION
Hernias seldom warrant imaging, and vesical inguinal hernias being extremely rare are usually detected incidentally. However, clinicians need to be aware of these and keep a high index of suspicion, especially in elderly obese males with inguinal hernia and LUTS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Westera J, Meyer J, Reynolds J, Lambrianides AL. Massive inguinoscrotal bladder hernia. JSCR. 2012;5:5. doi: 10.1093/jscr/2012.5.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bacigalupo L, Bertolotto M, Barbiera F, Pavlica P, Lagalla R, Mucell R, et al. Imaging of urinary bladder hernias. Am J Roentgenol. 2005;184:546–51. doi: 10.2214/ajr.184.2.01840546. [DOI] [PubMed] [Google Scholar]
- 3.Verbeeck N, Larrousse C, Lamy S. Diagnosis of inguinal bladder hernias: The current role of sonography. JBR-BTR. 2005;88:233–6. [PubMed] [Google Scholar]
- 4.Kim KH, Kim MU, Jeong WJ, Lee YS, Kim KH, Park KK, et al. Incidentally detected inguinoscrotal bladder hernia. Korean J Urol. 2011;52:71–3. doi: 10.4111/kju.2011.52.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]


