Abstract
Background:
Anesthetic management of elderly patients is a challenge as aging makes them more susceptible to hemodynamic fluctuations during regional anesthesia. This study was aimed to compare the clinical efficacy of epidural 0.75% ropivacaine fentanyl (RF)– with 0.5% bupivacaine–fentanyl (BF) for hemiarthroplasty in high-risk elderly patients.
Methods:
Sixty elderly consented patients of either sex with American Society of Anesthesiologist ASA II and III, scheduled for elective hemiarthroplasty were randomized into two Groups of 30 patients to receive epidural study solution of 15 mL of 0.75% Ropivacaine or 0.5% Bupivacaine with 1 mL fentanyl (50 μg). The hemodynamic variability with onset and duration of sensory and motor blocks were recorded. The adequacy and quality of surgical anesthesia were assessed. The post-epidural nausea and vomiting, shivering, respiratory parameters, or any other side effects were also recorded.
Results:
There was no difference in the demographic profile between groups. The mean onset time to achieve sensory block to the T10 dermatome was rapid in the Group BF (12.4±6.9 vs. 17.5±3.7 min in Group RF). The mean time to achieve motor block was 17.5±3.4 min in Group BF versus 21.7±7.8 min in Group RF. The intraoperative hemodynamic fluctuations showed statistically significant differences between groups. The pruritis was observed in five patients but post-epidural shivering, nausea, vomiting, respiratory depression, or urinary retention were not observed in any patient.
Conclusion:
Epidural 0.75% Ropivacaine with fentanyl showed better clinical profile as compared to 0.5% Bupivacaine with fentanyl for hemiarthroplasty in elderly patients.
Keywords: Bupivacaine, elderly population, epidural anesthesia, fentanyl, hemiarthroplasty, ropivacaine
INTRODUCTION
Anesthetic management of elderly patients can be a challenge due to limited organ reserve and their compromised organ function. Age is the predictor of anesthetic stress of cardiorespiratory functions and increases the mortality in patients undergoing major surgery. These patients show a relatively high (30-60%) prevalence of coexisting cardiovascular and pulmonary disorders.[1]
Administration of general anesthesia or central neuraxial anesthesia is challenging in the elderly patients due to numerous pathophysiological alterations and functional changes.[2] They require a clinically precise skilled anesthetic management to facilitate the early recovery. Neuraxial anesthetic blockade has a definite advantage in elderly patients over general anesthesia, due to reduce surgical stress and blood loss and improve respiratory and bowel function with decreased incidence of deep vein thrombosis. But the hemodynamic fluctuations in elderly patients are exaggerated even with conventional doses of local anesthetics and manifested as hypotension and bradycardia.[3] Recent studies have shown that no single anesthetic technique is superior for elderly patients in minimizing the perioperative hemodynamic fluctuations and post-operative delirium.[4,5,6]
Ropivacaine (RF), an amide local anesthetic, has shown its clinical efficacy and safety for regional anesthetic techniques with minimal hemodynamic fluctuations and systemic toxicity. The onset of sensory analgesia begins at 10-25 min after epidural administration of 2-4 h duration. Ropivacaine blocks sensory fibers more readily than motor fiber. The delayed onset time of sensory block in epidural anesthesia may be accelerated by adding adjuvants like opioids or other anesthetics.[7,8]
Considering the age and poor cardiorespiratory reserve of elderly patients and merits of Ropivacaine and fentanyl, the study was aimed to evaluate epidural 0.75% Ropivacine–fentanyl versus 0.5% bupivacaine fentanyl for hemiarthroplasty in high-risk elderly patients.
METHODS
This prospective blind randomized clinical study was conducted on 60 elderly patients of ASA physical status II and III of either sex aged 65 to 85 years with weight 60-90 kg and height 150-170 cm, scheduled for elective hemiarthroplasty under epidural anesthesia from August 2011 to March 2012. After approval by the Institutional Ethical Committee and written informed consent, all patients were subjected to pre-anesthetic assessment. Patients having any abnormality of the spine, cutaneous infection and local cellulitis at the site, coagulation disorders, allergy to local anesthetic, history of opioid dependence, or neurological disorders were excluded from the study. Before enrolment for the study, patients were explained about the method of sensory and motor assessments. All patients were pre-medicated with oral Ranitidine 150 mg and alprazolam 0.25 mg, night before surgery.
The patients were randomized according to computer generated random numbers into two equal groups of 30 patients each to receive epidural solution of 15 mL of 0.75% Ropivacaine or 0.5% Bupivacaine with 1 mL fentanyl (50 μg). The total volume of drug solution was 16 mL. The study drug solutions were prepared by one of the anesthesiologist who was not involved in patient's assessment.
In the operation theatre, routine hemodynamic monitoring of arterial blood pressure, heart rate, electrocardiography, and pulse oximetery was performed. Pre-loading with intravenous infusion of ringer lactate was stared at the rate of 10 mL/kg of body weight before the initiation of epidural block.
Epidural anesthesia was administered in the lateral decubitus position at L3-4 or L2-3 interspace with an 18-G Tuohy needle by loss of resistance method. With the bevel of the Tuohy needle in cephalic direction, an epidural catheter was inserted 5 cm into epidural space and secured. The position of catheter was checked by negative aspiration for blood or cerebro-spinal fluid CSF. Patients were laid supine and a test dose of 3 mL of 2% lidocaine containing 1:200,000 epinephrine was administered to detect intrathecal or intravenous injection. After 3 min, the patients received either 15 mL of 0.75% Ropivacaine (112.5 mg) or 0.5% Bupivacaine (75 mg) along with 1 mL fentanyl (50 μg) with a rate of 3 mL/10 s through epidural catheter.
The onset of sensory blockade with maximal cephalad spread was assessed by bilateral pin prick method along the midclavicular line using a short beveled 27-gauge hypodermic needle. The onset of sensory block was defined as the time from epidural injection to the occurrence of sensory block at dermatome level T10. The onset of motor blockade was assessed using a modified Bromage scale (0-3): 0 = no power impairment and able to raise straight leg against resistance; 1 = unable to raise straight leg but able to flex knee; 2 = unable to flex knee but able to move ankle joint; and 3 = unable to move hip, knee, or ankleno motor activity. The onset of motor block was defined as the time from epidural injection to the occurrence of motor block at each scale. The surgical anesthesia was considered effective when T10 dermatome was anesthetized.
Hemodynamic parameters of heart rate and arterial blood pressure were observed continuously and recorded every 5 min after administering epidural anesthesia until the patient transferred to the post-anesthesia room. Supplemental oxygen at the rate of 3 L/min was administered via a Hudson face mask during the surgery. Hypotension was defined as a fall in systolic blood pressure (SBP) of >20% of baseline value or <100 mm Hg and was treated with increment doses of mephentermine 6 mg and additional ringer lactate solution. Bradycardia (heart rate <50 beats/min) was treated with intravenous atropine. Side effects of pruritis, nausea, vomiting, respiratory depression, and post-epidural shivering were recorded and managed accordingly.
Post-operative analgesia was administered on demand through epidural catheter with 3 mL of local anesthetic with 1 mL (50 μg) fentanyl, diluted with 6 mL normal saline (10 mL) for each top up. They were followed up for any side effect till their hospital stay.
At the end of study, all data were compiled and the results were expressed as mean±SD for the statistical analysis. Parametric data were analyzed using Students’ t-test and Mann–Whitney U test. The non-parametric data were analyzed using Chi-square test. A P<0.05 was considered statistically significant.
RESULTS
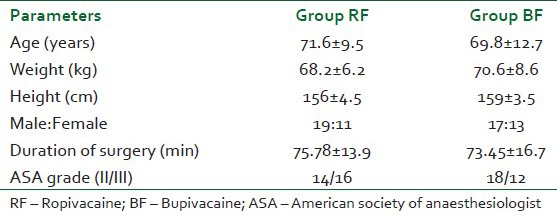
This study has comparatively evaluated the clinical efficacy of epidural Ropivacaine 0.75% versus 0.5% Bupivacaine with fentanyl in 60 elderly consented patients, scheduled for elective hemiarthroplasty. The demographic profile was comparable between groups. The age of patients ranged between 65 to 85 years and majority of patients were males with weight of 60-90 kg. There was no protocol deviation pre-operatively and intraoperatively. All patients were successfully operated upon and were cooperative with subsequent assessment. The mean duration of hemiarthroplasty was 77.79±17.54 min [Table 1].
Table 1.
Demographic profile of patients
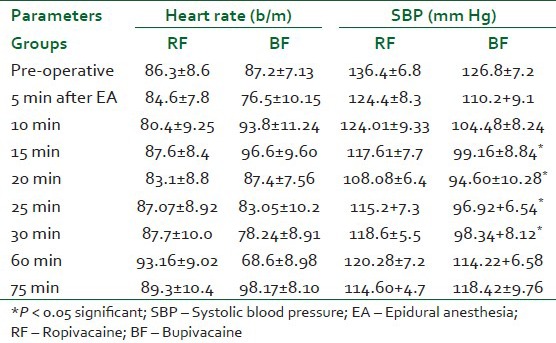
The hemodynamic characteristics of the baseline pre-operative heart rate and SBP along with intraoperative hemodynamic variations of heart rate and SBP at different time intervals are shown in Table 2. The mean values of heart rate and SBP did not show significant decline from the base values in Group RF but there was statistically significant variations in Group BF. The episodes of hypotension and bradycardia were treated with atropine, boluses of mephentermine, and rapid intravenous infusion.
Table 2.
Hemodynamic parameters of heart rate and systolic blood pressure
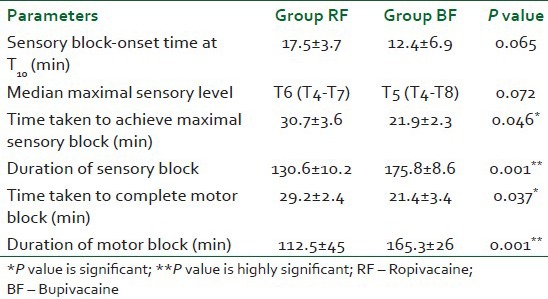
The sensory and motor block characteristics of both groups are shown in Table 3. The mean onset time of adequate sensory analgesia at T10 dermatome was faster (12.4±6.9 min) in Group BF versus 17.5±3.7 min in Group RF. The mean maximal cephalad level for sensory block was not statistically different but the mean time taken to reach the maximal sensory level was statistically significant (P<0.046). The duration of sensory blockade was prolonged in BF Group with statistically highly significant difference (P<0.001) as calculated by student t test. The statistically significant difference was observed between groups for mean onset time for motor block of Bromage scale three. The onset of motor block was rapid in Group BF (P<0.037) and was of longer duration than RF Group. The duration of motor blockade was shorter than sensory analgesia in Group RF.
Table 3.
Sensory and motor block profile of epidural anesthesia with fentanyl
Mild pruritis was observed in only two patients of Group RF and three patients of BF Group which required no treatment. The ventilatory frequency and peripheral oxygen saturation were comparable between groups. No patients suffered from post-epidural shivering, nausea or vomiting, respiratory depression, and urinary retention in any group. There were no post-operative transient neurological symptoms in any patient.
DISCUSSION
This study has clinically evaluated the relative efficacy of epidural Ropivacaine versus Bupivacaine with fentanyl for hemiarthroplasty in elderly patients by assessing the hemodynamic fluctuations, sensory and motor block characteristics along with post-operative outcome and it has demonstrated the adequate surgical anesthesia with stable intraoperative hemodynamic parameters with epidural Ropivacaine with fentanyl as compared to epidural Bupivacaine with fentanyl. Ropivacaine was found to be safer for regional anesthetic techniques due to its reduced systemic toxicity and greater differentiation between duration of sensory and motor blockade. No episodes of hypotension, nausea and vomiting, headache, post-epidural shivering, and urinary retention have occurred in any patients during the study. A prompt return to the pre-operative mental status was observed in our study after epidural anesthesia with fentanyl after hemiarthroplasty.
Peduto et al. reported that epidural injection of 15 mL of either 0.5% levobupivacaine or 0.75% Rpoivacaine produced similar epidural blockade in patients undergoing lower limb surgery.[9] This study has also demonstrated that epidural RF produced the adequate surgical anesthesia as produced by epidural BF but of shorter duration.
The study of Polley et al. has shown that Ropivacaine was significantly less potent than bupivacaine, with a potency ratio of 0.6,[10] which was evident from this study as the onset of sensory and motor blockade, was statistically delayed with epidural Ropivacaine as compared to Bupivacaine at clinically equivalent doses. Recent studies, comparing Ropivacaine with Bupivacaine, found that epidural Ropivacaine produces a blockade which is substantially similar to that produced by equivalent concentrations and doses of Bupivacaine.[11,12]
The potency of Ropivacaine may be altered by co-administration with other anesthetics or opioid analgesics.[13] A synergistic interaction between local anesthetics and epidural opioids has been reported. They act independently via different mechanisms. Local anesthetics block propagation and generation of neural action potential by a selective effect on sodium channels, whereas opioid acts on the opioids receptors to increase potassium conductance. Thus, combination of local anesthetics and opioids may effectively inhibit multiple areas of neuronal excitability, thus enhances the potency of surgical anesthesia.[14] Fields et al. showed that dorsal roots (primary afferent tissues) contain opioid-binding sites and fentanyl acts either directly on the spinal nerve or by penetrating the dura to act at the spinal roots.[15]
CONCLUSION
Epidural 0.75% Ropivacine with fentanyl (RF) showed better clinical profile as compared to 0.5% Bupivacaine with fentanyl (BF) for hemiarthroplasty in elderly patients as it provided adequate surgical anesthesia and less intraoperative hemodynamic fluctuation. No fentanyl-related side effects have occurred. Considering the age and poor cardiorespiratory reserve, the epidural Rpoivacaine with fentanyl should be considered anesthetic technique of choice for hemiarthroplasty in high-risk elderly patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Liu LL, Leung JM. Predicting adverse postoperative outcomes in patients aged 80 years or older. J Am Geriatr Soc. 2000;48:405–12. doi: 10.1111/j.1532-5415.2000.tb04698.x. [DOI] [PubMed] [Google Scholar]
- 2.Chung F, Meier R, Lautenschlager E, Carmichael FJ, Chung A. General or spinal anesthesia: Which is better in the elderly? Anesthesiology. 1987;67:422–7. doi: 10.1097/00000542-198709000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Yeager MP, Glass DD, Neff RK, Brinck-Johnsen T. Epidural anesthesia and analgesia in high-risk surgical patients. Anesthesiology. 1987;66:729–36. doi: 10.1097/00000542-198706000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hole A, Terjesen T, Breivik H. Epidural versus general anaesthesia for total hip arthroplasty in elderly patients. Acta Anaesthesiol Scand. 1980;24:279–87. doi: 10.1111/j.1399-6576.1980.tb01549.x. [DOI] [PubMed] [Google Scholar]
- 5.O’Hara DA, Duff A, Berlin JA, Poses RM, Lawrence VA, Huber EC, et al. The effect of anesthetic technique on postoperative outcomes in hip fracture repair. Anesthesiology. 2000;92:947–57. doi: 10.1097/00000542-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Davis FM, Laurenson VG. Spinal anaesthesia or general anaesthesia for emergency hip surgery in elderly patients. Anaesth Intensive Care. 1981;9:352–8. doi: 10.1177/0310057X8100900406. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal A, Verma RK, Shrivastava S. Ropivacaine-The latest local anesthetic in the Indian Market. J Anesth Clin Pharmacol. 2010;26:223–8. [Google Scholar]
- 8.Eledjam JJ, Ripart J, Viel E. Clinical application of ropivacaine for the lower extremity. Curr Top Med Chem. 2001;1:227–31. doi: 10.2174/1568026013395317. [DOI] [PubMed] [Google Scholar]
- 9.Peduto VA, Baroncini S, Montanini S, Proietti R, Rosignoli L, Tufano R, et al. A prospective, randomized, double-blind comparison of epidural levobupivacaine 0.5% with epidural ropivacaine 0.75% for lower limb procedures. Eur J Anaesthesiol. 2003;20:979–83. doi: 10.1017/s0265021503001583. [DOI] [PubMed] [Google Scholar]
- 10.Polley LS, Columb MO, Naughton NN, Wagner DS, van de Ven CJ. Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor: Implications for therapeutic indexes. Anesthesiology. 1999;90:944–50. doi: 10.1097/00000542-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Brockway MS, Bannister J, McClure JH, McKeown D, Wildsmith JA. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth. 1991;66:31–7. doi: 10.1093/bja/66.1.31. [DOI] [PubMed] [Google Scholar]
- 12.Boztuş N, Bigat Z, Karsli B, Saykal N, Ertok E. Comparison of ropivacaine and bupivacaine for intrathecal anesthesia during outpatient arthroscopic surgery. J Clin Anesth. 2006;18:521–5. doi: 10.1016/j.jclinane.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Ozgurel O. Comparison of fentanyl added to ropivacaine or bupivacaine in spinal anesthesia. Reg Anesth Pain Med. 2003;28:23. Abs 89. [Google Scholar]
- 14.Cherng CH, Yang CP, Wong CS. Epidural fentanyl speeds the onset of sensory and motor blocks during epidural ropivacaine anesthesia. Anesth Analg. 2005;101:1834–7. doi: 10.1213/01.ANE.0000184131.06529.35. [DOI] [PubMed] [Google Scholar]
- 15.Fields HL, Emson PC, Leigh BK, Gilbert RF, Iversen LL. Multiple opiate receptor sites on primary afferent fibres. Nature. 1980;284:351–3. doi: 10.1038/284351a0. [DOI] [PubMed] [Google Scholar]


