Abstract
Context
Psychiatric disorders are prevalent among incarcerated juveniles. Most juveniles eventually return to their communities, where they become the responsibility of the community mental health system. Yet, no large-scale study has examined psychiatric disorders after youth leave detention.
Objective
To examine changes in prevalence and persistence of disorders during the 5 years after detention, focusing on sex and racial/ethnic differences.
Design
Prospective longitudinal study with up to 5 interviews (N = 1829). To ensure representation of key demographic subgroups, the randomly selected sample was stratified by sex, race/ethnicity (African American, non-Hispanic white, and Hispanic), age, and legal status (juvenile or adult court).
Setting
The Northwestern Juvenile Project, sampling youth from the Cook County Juvenile Temporary Detention Center, Chicago, Illinois.
Participants
Detained youth, 10 to 18 years at baseline interview.
Main Outcome Measures
At baseline, the Diagnostic Interview Schedule for Children Version 2.3. At follow-ups, the Diagnostic Interview Schedule for Children, Version IV (Child and Young Adult versions) and the Diagnostic Interview Schedule, Version IV (substance use disorders and antisocial personality disorder).
Results
Five years after baseline, more than 45% of males and nearly 30% of females had one or more psychiatric disorders with associated impairment. Substance use disorders were the most common disorders; males, however, had higher rates over time (5 years after baseline, adjusted odds ratio [AOR], 2.61; 95% CI, 1.96–3.47). Non-Hispanic whites and Hispanics also had higher rates of substance use disorders compared with African Americans (respectively, AOR, 1.96, 95% CI, 1.54–2.49; AOR, 1.59, 95% CI, 1.24–2.03). Females had higher rates of major depression over time (AOR, 1.59, 95% CI, 1.22–2.08).
Conclusions
Although prevalence rates of most psychiatric disorders declined over time, a substantial proportion of delinquent youth continue to have disorders. There were notable sex and racial/ethnic differences in the prevalence and persistence of disorders.
INTRODUCTION
Psychiatric disorders are prevalent among incarcerated juveniles.1–14 A 2008 literature review concluded that psychiatric disorders are substantially more common in adolescents in detention than among adolescents in the general population.14 The Northwestern Juvenile Project found that at intake to detention, even after excluding conduct disorder, more than 60% of juvenile detainees met diagnostic criteria with diagnosis-specific impairment for one or more psychiatric disorders.15 Among youth incarcerated for nine months, Karnik et al.16 found even higher rates: about 90% of detainees had a psychiatric disorder other than conduct disorder or oppositional defiant disorder. Using the lower rate,15 an estimated 55,000 of the 92,854 youth held in U.S. correctional facilities each day17 have one or more psychiatric disorders.
Many psychiatric disorders are likely to persist as these juveniles become young adults. Risk factors for psychiatric disorders are common among delinquent youth: maltreatment,18–20 dysfunctional families,19, 21 family substance abuse, 18 and brain injury. 22 Because delinquent youth have few protective factors to offset these risks, many are vulnerable to continued psychiatric morbidity as they age.18
Despite its importance, few longitudinal studies have examined the prevalence and persistence of psychiatric disorders after youth leave detention. Instead, studies of delinquent youth have focused on the association between psychiatric disorders and criminal recidivism, antisocial behavior, or social functioning.23–26 We could find only one longitudinal study of the persistence and prevalence of psychiatric disorders in detained youth. Harrington et al27 found that two years after detention, many mental health problems persisted or worsened. Their sample, however, excluded females, was 80% white, and was too small (n=97) to permit detailed analyses. Moreover, the study was conducted in the United Kingdom, limiting generalizability to juvenile detainees in the United States.
The related literature – longitudinal studies of “high-risk” youth – also provides little information. Youth with histories of detention have been included in studies of high -risk youth: the homeless,28, 29 youth living in impoverished or high-crime neighborhoods,30–34 and the offspring of parents who used substances or had psychiatric disorders.29, 35–46 Yet, none of these studies distinguished between youth with and without histories of detention. (Summary tables are available from the authors.)
Delinquent youth are also under represented in general population longitudinal studies, such as household-based surveys (e.g., Great Smoky Mountains Study of Youth,47, 48 the National Comorbidity Surveys,49–51 National Epidemiologic Survey on Alcohol and Related Conditions52) and studies drawn from school-based samples (e.g., Oregon Adolescent Depression Project,53, 54 Pittsburgh Youth Study55) and general pediatric clinics.56, 57 Household surveys typically exclude persons in correctional institutions.47, 50, 58–61 School-based samples omit youth who are truant or miss school because they are detained.53–55, 62–65 Samples drawn from general pediatric clinics omit youth who do not receive medical care.56, 57 Even if sampled initially, youth may be lost to follow-up when they are incarcerated because they cannot be found, and because studying prisoners requires special procedures and approvals from the Secretary of Health and Human Services.66
In sum, to our knowledge, no large-scale longitudinal study has examined the prevalence and persistence of psychiatric disorders after youth leave detention. This omission is critical. Juvenile detainees have a median length of stay of only two weeks.67 Thus, juvenile detainees become a community public health problem when they are released and may continue to burden society as they age. Epidemiologic studies are the first step to improve prevention and treatment in correctional facilities and in the community. 68 Data are also needed to address health disparities, a priority of Healthy People 202069 and the Institute of Medicine. 70 Of the approximately one-half million incarcerated youth and young adults (ages 24 and younger), nearly 70% are African American or Hispanic,17, 71 compared with one -third in the general population.72
This study presents data from the Northwestern Juvenile Project, the first comprehensive longitudinal study of psychiatric disorders in youth after they leave detention. The sample is large (N=1829), racially/ethnically diverse, and includes both males and females. We examine changes in the prevalence and persistence of disorders during the five years after detention, focusing on sex and racial/ethnic differences.
METHODS
Sample and Procedures
Baseline Interviews
We recruited a stratified random sample of 1829 youth at intake to the Cook County Juvenile Temporary Detention Center (CCJTDC) in Chicago, Illinois, between November 20, 1995, and June 14, 1998. The CCJTDC is used for pretrial detention and for offenders sentenced for fewer than 30 days. To ensure adequate representation of key subgroups, we stratified our sample by sex, race/ethnicity (classified via self-identification as African American, non-Hispanic white, or Hispanic), age (10–13 years or ≥14 years), and legal status (processed in juvenile or adult court). Final sampling fractions for strata ranged from 0.108 to 0.689.
All detainees who were awaiting the adjudication or disposition of their case were eligible to participate in the study. Among these, 2275 detainees were randomly selected; 4.2% (34 youth and 62 parents or guardians) refused to participate. There were no significant differences in refusal rates by sex, race/ethnicity, or age. Twenty-seven youth left the detention center before an interview could be scheduled; 312 left CCJTDC while we attempted to locate their caretakers for consent. Eleven others were excluded from the sample because they were unable to complete the interview. The final sample size was 1829: 1172 males, 657 females; 1005 African Americans, 296 non-Hispanic whites, 524 Hispanics, 4 “other” race/ethnicity ; age range, 10 to 18 years (mean, 14.9 years; median, 15 years ) (see eTable 1).
Face-to-face structured interviews were conducted at the detention center in a private area, most within 2 days of intake.
Follow-up Interviews
Our design included: (1) follow-up interviews at 3 and 4.5 years after baseline for the entire sample; and (2) two additional interviews at 3.5 and 4 years after baseline for a random subsample of 997 subjects (600 males and 397 females).
For each follow-up, we interviewed participants irrespective of where they were living: in the community (approximately two-thirds of interviews); at correctional facilities (nearly 30% of interviews); or by telephone if they lived more than two hours away (<5% of interviews).
Participants were paid $25 for the 2-to 3 -hour baseline interview and $50 for each of the 3-to 4 -hour follow-up interviews. Most interviewers had graduate degrees in psychology or an associated field and had experience interviewing at-risk youth; one-third were fluent in Spanish. All interviewers were trained for at least 1 month. For each wave, consistency across interviewers was established and maintained via scripted mock interviews following training and mid-wave. Additional information on our methods is in eAppendix 1 and is published elsewhere.15, 73, 74
Procedures to Obtain Assent and Consentat Baseline and Follow -Up
For all interviews, participants signed either an assent form (if they were <18 years old) or a consent form (if they were ≥18 years old). The Northwestern University Institutional Review Board and the Centers for Disease Control and Prevention Institutional Review Board approved all study procedures and waived parental consent for persons younger than 18 years, consistent with federal regulations regarding research with minimal risk.75 We nevertheless attempted to contact parents of minors to obtain their consent and to provide them with information on the study, and used an independent participant advocate to represent the minors’ interests75(see eAppendix 1).
Measures
Baseline
We used the Diagnostic Interview Schedule for Children, version 2.3 (DISC 2.3),76, 77 the most recent English and Spanish versions then available. This version of the DISC, based on the DSM-III-R, assesses the presence of disorders in the past six months. The DISC 2.3 is highly structured, contains detailed symptom probes, has acceptable reliability and validity, and requires relatively brief training.76, 78–81 Because the DISC 2.3 did not include posttraumatic stress disorder (PTSD), we used the module from the Diagnostic Interview Schedule for Children, version IV (DISC-IV) when it became available, 13 months after the study began.73 Additional detail on baseline diagnostic decisions can be found elsewhere.15, 73, 74
Follow-up Interviews
We administered the DISC-IV (Child and Young Adult versions), based on the DSM-IV, to assess for schizophrenia, mood disorders, anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), and disruptive behavior disorders in the past year.82, 83 Impairment was defined as moderate impairment in at least one area of functioning (Criterion A).84 We present prevalence rates of disorder with and without the impairment criterion; our analyses of changes in disorder over time use disorders with impairment.
To assess substance use disorders and antisocial personality disorder (APD) at follow-up, we administered the Diagnostic Interview Schedule, version IV (DIS-IV).85, 86 We used the DIS-IV to assess substance use disorders because the DISC-IV is not sufficiently detailed for our population. Antisocial personality disorder was assessed for participants 18 years and older (who were no longer eligible for childhood disruptive behavior disorders). Disorders are assessed for the year prior to the interview. Consistent with the National Comorbidity Survey Replication,50 participants who met criteria for substance use disorder or APD with “partial recovery” were scored as having the disorder.
We did not implement DSM exclusionary criteria.
Comparability of Diagnoses Over Time
Our diagnostic measures changed over time for three reasons: (1) the release of the DISC-IV (based on the DSM-IV criteria) mid -study; (2) aging out of childhood disruptive behavior disorders by some participants; and (3) our need to use a more comprehensive measure of substance use disorder (DIS-IV) for the follow-up interviews.
To check that changes in prevalence rates over time were not due to changes in measurement, we conducted sensitivity analyses. We created a set of adjusted scoring algorithms to maximize comparability among the DISC 2.3, DISC-IV, and DIS-IV criteria, while minimizing alterations (see eAppendix 2). All analyses were run twice, with and without these adjusted criteria. Because there were no substantive differences in findings and to enable comparisons with other studies, we present results using the original, unadjusted diagnoses.
Statistical Analysis
Prevalence Rates of Disorder at Specific Time Points
Because some participants were interviewed more often than others, we used a subset of interviews to summarize prevalence rates at 3 time points: baseline (Time 0), Time 1, and Time 2.
Time 1. Time 1 is the first follow-up interview, but excludes interviews that occurred more than 18 months after the interview due date. Using a narrower window would restrict the generalizability of our findings because, in this high-risk and highly mobile population, participants can be difficult to track. Median time between baseline and Time 1 was 3.0 years (mean [SD], 3.2 [0.3] years; range, 2.7–4.5 years). For simplicity, we refer to the Time 1 interview as occurring approximately 3 years after baseline. eTable 1, which summarizes sample demographics and retention rates, shows that 90.7% of participants had a Time 1 interview.
Time 2. For each participant, Time 2 consists of the earliest follow-up interview that occurred approximately 4.5 years after baseline. As with Time 1, we excluded interviews that occurred more than 18 months after this due date. The median time between baseline and the Time 2 interview was 4.7 years (mean [SD], 4.9 [0.4]; range, 4.3–6.0 years). To ensure that prevalence rates reflect temporally distinct cross-sections of the sample, we required at least 16 months between the Time 1 and Time 2 interviews. We subsequently refer to the Time 2 interview as occurring approximately 5 years after baseline. eTable 1 shows that 85.3% of participants had a Time 2 interview.
To generate prevalence rates that reflect CCJTDC’s population, each participant was assigned a sampling weight augmented with a nonresponse adjustment to account for missing data.87 Taylor series linearization was used to estimate standard errors.88, 89
Changes in Prevalence Over Time
We used all available interviews: an average of 3.9 interviews per person (range, 1–5 interviews per person); 88.7% of participants had every scheduled interview. Using generalized estimating equations (GEEs),90 we fit marginal models examining: (1) differences in the prevalence of disorders by sex and race/ethnicity over time; and (2) changes in disorders as youth aged. Disorder was modeled as binomial with a logit link function. We used a robust sandwich estimator with an unstructured correlation matrix; in the few instances when models failed to converge, we specified an exchangeable correlation structure. All statistically significant (p < .05) odds ratios contrasting sex and racial/ethnic differences are noted in the text and come from the GEEs. Unless otherwise noted, these odds ratios contrast sex and race/ethnicity over time. Only the odds ratios in Table 3 and eTables 4, 5, and 6 compare prevalence at Time 1 or Time 2; these were estimated using logistic regression.
Table 3.
| Disorder | Males
|
Females
|
OR (95% CI) for Persistence to Time 1, M vs F | OR (95% CI) for Persistence to Time 2, M vs F | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Disorder Present at Baseline (n) | % (SE) Persisting
|
Disorder Present at Baseline (n) | % (SE) Persisting
|
|||||||||
| Time 1 | Time 2 | Time 1 | Time 2 | |||||||||
| Any Disorderc | 335 | 52.1 | (5.8) | 48.7 | (6.1) | 233 | 54.0 | (4.2) | 34.9 | (4.9) | ||
| Any Mood Disorder | 163 | 28.0 | (6.1) | 18.9 | (5.7) | 144 | 30.4 | (4.6) | 20.9 | (4.2) | ||
| Any Major Mood Disorder | 127 | 18.8 | (5.6) | 17.3 | (6.1) | 124 | 25.9 | (4.7) | 19.2 | (4.3) | ||
| Maniad | 16 | --- | --- | --- | --- | 8 | --- | --- | --- | --- | ||
| Major depression | 116 | 20.0 | (6.2) | 15.7 | (6.3) | 118 | 25.3 | (4.7) | 17.9 | (4.2) | ||
| Hypomaniad | 16 | --- | --- | --- | --- | 2 | --- | --- | --- | --- | ||
| Dysthymia | 98 | 1.6 | (1.0) | 0.0 | 87 | 3.8 | (2.2) | 3.9 | (2.2) | |||
| Any Anxiety Disorderc | 50 | 6.3 | (3.1) | 14.8 | (9.7) | 58 | 19.3 | (6.3) | 17.3 | (7.1) | ||
| Generalized anxiety disorder | 34 | 18.8 | (11.3) | 0.0 | 35 | 9.4 | (5.2) | 10.4 | (7.0) | |||
| Panic disorderd | 3 | --- | --- | --- | --- | 7 | --- | --- | --- | --- | ||
| Post-traumatic stress disorderc | 37 | 5.8 | (3.6) | 4.0 | (2.9) | 42 | 4.5 | (3.2) | 5.4 | (3.7) | ||
| Any Disruptive Behavior Disorder | 388 | 36.6 | (4.7) | 31.1 | (4.7) | 230 | 30.7 | (4.8) | 10.5 | (2.4) | 3.83 (1.98, 7.43) | |
| Any Substance Use Disordere | 517 | 38.0 | (3.8) | 34.3 | (3.8) | 266 | 30.5 | (4.6) | 18.2 | (2.7) | 1.95 (1.09, 3.51) | 3.68 (2.10, 6.44) |
| Alcohol use disordere | 219 | 30.4 | (5.6) | 29.3 | (5.7) | 127 | 16.2 | (3.4) | 12.3 | (3.3) | 2.66 (1.21, 5.85) | 3.62 (1.49, 8.77) |
| Drug use disordere | 482 | 28.4 | (3.7) | 23.1 | (3.4) | 246 | 22.6 | (5.2) | 13.6 | (2.4) | 2.96 (1.59, 5.51) | |
SE = Standard error; OR = Odds Ratio; CI = Confidence Interval; M = Male; F = Female
Rates of persistence and their associated standard errors are weighted to adjust for sampling design and reflect the demographic characteristics of the Cook County Juvenile Temporary Detention Center.
Persistence is presented for disorders assessed with impairment criteria, with the exception of hypomania, which has no impairment criteria for diagnosis. We do not present rates of persistence for disorders assessed only for juveniles or adults (Attention-deficit/hyperactivity disorder, conduct disorder, oppositional defiant disorder, or antisocial personality disorder).
Assessed at baseline for participants who were interviewed after the DISC-IV post-traumatic stress disorder module became available (n = 541 males and 374 females).
Rates of persistence are not presented for disorders with fewer than 20 cases at baseline.
Odds ratios describing gender differences in the persistence of substance use disorders are adjusted for number of days incarcerated in the past year.
All GEE models included covariates for sex, race/ethnicity (African American, Hispanic, non-Hispanic white), and aging (time since baseline). We also included age at baseline (10–18 years) and legal status at detention (processed in juvenile or adult court) because they were stratification characteristics. The four participants who identified as “other” race/ethnicity at baseline were excluded. We estimated models with quadratic terms for aging when the linear term was statistically significant. When main effects were significant, we estimated models with the corresponding interaction terms. Only interaction terms or quadratic aging terms that reached statistical significance were included in final models. For models with significant interactions between sex and aging, we report model-based odds ratios for sex differences at 3 and 5 years after baseline. GEE models were estimated with sampling weights to account for study design. We examined the sensitivity of our models to attrition by using weights that combined the probability of being sampled with the probability of dropping out.91 Results (available from the authors) were substantially similar.
GEE analyses were conducted on disorders (with the impairment criterion) except for (1) schizophrenia, because there were too few cases; (2) hypomania, because participants with this disorder were significantly more likely to be missing follow-up data than those without (33% vs 11%, p < .05); and (3) diagnoses assessed only for juveniles (ADHD, conduct disorder, oppositional defiant disorder) or adults (APD)—because nearly all participants turned 18 years old during the follow-up period. Instead, we estimated changes over time in any disruptive behavior disorder, defined as conduct disorder or oppositional defiant disorder (for participants <18 years) or APD (for participants 18 years).
Because detention may alter access to substances, all models describing substance use disorders included linear and quadratic terms for time incarcerated prior to the interviews. When substance use disorder was measured at a follow-up interview, we used number of days incarcerated in the past year because disorders were assessed in the past year. When substance use disorder was measured at the baseline interview (and therefore assessed in the past 6 months), we used time incarcerated in the past 90 days, the best available estimate. All analyses were conducted using Stata 11 software and its survey routines.92
RESULTS
Prevalence
Overview
Table 1 and Table 2 show prevalence rates of disorder—computed with and without the impairment criterion—at baseline, Time 1, and Time 2 for males and females. At Time 2, more than 45% of males and nearly 30% of females had any disorder (with impairment). Even excluding disruptive behavior disorders, 37% of males and 25% of females had any disorder.
Table 1.
| Disorder | With impairment | Without impairment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Baseline | Time 1 | Time 2 | Baseline | Time 1 | Time 2 | |||||||
| % | (SE) | % | (SE) | % | (SE) | % | (SE) | % | (SE) | % | (SE) | |
|
|
|
|
|
|
|
|
||||||
| Any Disorderc | 61.8 | (4.1) | 51.7 | (2.8) | 46.5 | (2.9) | 67.0 | (4.0) | 57.9 | (2.7) | 51.7 | (2.9) |
| Any Disorder, Except Behavioralc | 60.2 | (4.1) | 45.1 | (2.7) | 36.9 | (2.7) | 64.4 | (4.0) | 50.7 | (2.8) | 42.4 | (2.8) |
| Schizophreniad | --- | --- | 0.2 | (0.1) | 0.1 | (0.1) | --- | --- | 0.2 | (0.1) | 0.1 | (0.1) |
| Any Mood Disorder | 15.8 | (1.8) | 14.9 | (1.9) | 8.8 | (1.6) | 18.8 | (1.9) | 16.2 | (2.0) | 9.7 | (1.7) |
| Any Major Mood Disorder | 12.7 | (1.7) | 9.5 | (1.6) | 6.4 | (1.4) | 14.3 | (1.8) | 10.5 | (1.6) | 7.3 | (1.5) |
| Mania | 2.0 | (0.7) | 0.5 | (0.2) | 0.7 | (0.4) | 2.2 | (0.8) | 0.6 | (0.2) | 0.7 | (0.4) |
| Major depression | 11.0 | (1.6) | 9.1 | (1.5) | 6.4 | (1.4) | 13.0 | (1.7) | 10.1 | (1.6) | 7.3 | (1.5) |
| Hypomaniae | 2.1 | (0.7) | 6.3 | (1.4) | 2.1 | (0.7) | 2.1 | (0.7) | 6.3 | (1.4) | 2.1 | (0.7) |
| Dysthymia | 9.9 | (1.5) | 1.1 | (0.6) | 1.0 | (0.6) | 12.2 | (1.7) | 1.5 | (0.7) | 1.0 | (0.6) |
| Any Anxiety Disorder c | 10.8 | (2.7) | 9.8 | (1.6) | 7.7 | (1.6) | 16.7 | (3.2) | 10.8 | (1.6) | 9.2 | (1.7) |
| Generalized anxiety disorder | 3.8 | (1.0) | 2.6 | (0.9) | 1.9 | (0.9) | 7.1 | (1.3) | 2.6 | (0.9) | 1.9 | (0.9) |
| Panic disorder | 0.1 | (0.1) | 1.4 | (0.5) | 0.5 | (0.2) | 0.3 | (0.1) | 2.2 | (0.6) | 1.0 | (0.5) |
| Post-traumatic stress disorderc | 7.9 | (2.3) | 7.6 | (1.4) | 5.4 | (1.3) | 10.9 | (2.6) | 8.0 | (1.4) | 6.4 | (1.4) |
| Attention-deficit/hyperactivity disorder (< 18 y)f | 11.2 | (1.5) | 6.5 | (2.3) | 4.2 | (2.3) | 16.6 | (1.8) | 7.0 | (2.3) | 5.6 | (2.7) |
| Any Disruptive Behavior Disorderg | 29.5 | (2.2) | 21.9 | (2.2) | 22.1 | (2.4) | 41.8 | (2.4) | 28.7 | (2.4) | 26.1 | (2.5) |
| Conduct disorder (< 18 y)f | 24.3 | (2.0) | 20.5 | (3.8) | 9.3 | (3.2) | 37.8 | (2.4) | 29.7 | (4.6) | 13.9 | (4.0) |
| Oppositional defiant disorder (< 18 y)f | 12.6 | (1.6) | 15.7 | (3.8) | 10.0 | (3.4) | 14.5 | (1.7) | 17.6 | (4.0) | 10.6 | (3.6) |
| Antisocial personality disorder (>= 18 y)h | NA | NA | 20.4 | (2.4) | 22.2 | (2.4) | NA | NA | 26.6 | (2.7) | 26.2 | (2.5) |
| Any Substance Use Disorder | 45.7 | (2.5) | 29.4 | (2.4) | 28.0 | (2.4) | 50.7 | (2.5) | 37.3 | (2.6) | 32.2 | (2.5) |
| Alcohol use disorder | 19.9 | (2.0) | 15.6 | (1.9) | 17.1 | (2.0) | 25.9 | (2.2) | 18.6 | (2.0) | 19.0 | (2.0) |
| Drug use disorder | 42.3 | (2.4) | 22.0 | (2.2) | 18.8 | (2.0) | 45.4 | (2.5) | 30.2 | (2.4) | 23.4 | (2.2) |
SE = Standard error; y = years; NA = Not applicable
Descriptive statistics are weighted to adjust for sampling design and reflect the demographic characteristics of the Cook County Juvenile Temporary Detention Center.
Because some participants were interviewed more often than others, we used a subset of interviews to summarize prevalence rates at 3 time points: baseline (Time 0), Time 1 and Time 2. The sample consisted of n = 1172, 1054, and 993 males at baseline, Time 1, and Time 2, respectively.
Assessed at baseline for participants who were interviewed after the DISC-IV post-traumatic stress disorder module became available (n = 541 males).
Not assessed at baseline.
Because there are no impairment criteria for a diagnosis of hypomania, prevalence rates of hypomania with and without impairment are the same.
Assessed for participants younger than 18 years old (n = 1172, 350, and 96 males at baseline, Time 1, and Time 2, respectively).
For participants younger than 18, Any Disruptive Behavior disorder is defined as having conduct disorder or oppositional defiant disorder. For participants 18 and older, it is defined as having antisocial personality disorder.
Assessed for participants 18 and older at Time 1 and Time 2 (n = 704 and 897 males, respectively). Not assessed at baseline because the sample consisted of juveniles.
Table 2.
| Disorder | With impairment | Without impairment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Baseline | Time 1 | Time 2 | Baseline | Time 1 | Time 2 | |||||||
| % | (SE) | % | (SE) | % | (SE) | % | (SE) | % | (SE) | % | (SE) | |
|
|
|
|
|
|
|
|
||||||
| Any Disorderc | 65.3 | (2.8) | 42.9 | (2.3) | 29.0 | (2.1) | 74.4 | (2.4) | 52.5 | (2.3) | 40.8 | (2.5) |
| Any Disorder, Except Behavioralc | 62.9 | (3.5) | 38.6 | (2.3) | 25.3 | (2.0) | 69.7 | (2.6) | 45.7 | (2.3) | 32.1 | (2.1) |
| Schizophreniad | --- | --- | 0.2 | (0.2) | 0.0 | --- | --- | --- | 0.2 | (0.2) | 0.0 | --- |
| Any Mood Disorder | 22.8 | (2.1) | 17.0 | (1.6) | 11.9 | (1.4) | 27.7 | (2.1) | 19.5 | (1.7) | 12.5 | (1.4) |
| Any Major Mood Disorder | 19.9 | (2.1) | 13.2 | (1.4) | 10.4 | (1.3) | 23.0 | (2.1) | 15.2 | (1.5) | 10.8 | (1.3) |
| Mania | 1.2 | (0.4) | 1.6 | (0.5) | 1.5 | (0.5) | 1.8 | (0.5) | 2.3 | (0.6) | 1.7 | (0.5) |
| Major depression | 18.9 | (2.1) | 12.7 | (1.4) | 10.2 | (1.3) | 21.6 | (2.1) | 14.6 | (1.5) | 10.4 | (1.3) |
| Hypomaniae | 0.3 | (0.2) | 4.1 | (0.8) | 0.8 | (0.4) | 0.3 | (0.2) | 4.1 | (0.8) | 0.8 | (0.4) |
| Dysthymia | 12.5 | (1.3) | 1.5 | (0.5) | 0.7 | (0.3) | 15.8 | (1.4) | 1.9 | (0.6) | 0.9 | (0.4) |
| Any Anxiety Disorderc | 18.9 | (3.4) | 12.4 | (1.5) | 8.1 | (1.2) | 24.1 | (3.4) | 14.1 | (1.5) | 8.7 | (1.3) |
| Generalized anxiety disorder | 5.1 | (0.9) | 3.3 | (0.8) | 2.1 | (0.6) | 7.3 | (1.0) | 3.3 | (0.8) | 2.1 | (0.6) |
| Panic disorder | 1.0 | (0.4) | 2.3 | (0.6) | 0.9 | (0.4) | 1.5 | (0.4) | 3.0 | (0.7) | 1.1 | (0.5) |
| Post-traumatic stress disorderc | 14.6 | (3.4) | 7.9 | (1.1) | 5.8 | (1.0) | 17.7 | (3.4) | 9.3 | (1.2) | 6.4 | (1.0) |
| Attention-deficit/hyperactivity disorder (< 18 y)f | 16.4 | (1.5) | 9.7 | (2.6) | 0.0 | --- | 21.4 | (1.6) | 11.1 | (2.7) | 0.0 | --- |
| Any Disruptive Behavior Disorderg | 34.6 | (2.1) | 16.6 | (2.1) | 7.3 | (1.1) | 45.7 | (2.1) | 24.6 | (2.2) | 15.4 | (2.5) |
| Conduct disorder (< 18 y)f | 28.5 | (2.1) | 13.5 | (3.0) | --- | --- | 40.6 | (2.1) | 20.9 | (3.5) | 18.8 | (8.6) |
| Oppositional defiant disorder (< 18 y)f | 15.1 | (1.4) | 9.1 | (2.4) | 4.0 | (3.9) | 17.5 | (1.5) | 12.9 | (2.9) | 8.1 | (5.6) |
| Antisocial personality disorder (>= 18 y)h | NA | NA | 15.4 | (2.6) | 7.2 | (1.2) | NA | NA | 23.1 | (2.6) | 15.1 | (2.6) |
| Any Substance Use Disorder | 41.7 | (2.3) | 18.0 | (2.1) | 13.5 | (1.5) | 46.8 | (2.2) | 24.7 | (2.1) | 20.4 | (1.7) |
| Alcohol use disorder | 20.0 | (2.1) | 7.8 | (1.1) | 6.0 | (1.0) | 26.5 | (2.1) | 10.6 | (1.2) | 8.5 | (1.2) |
| Drug use disorder | 38.4 | (2.4) | 12.7 | (2.0) | 9.2 | (1.2) | 42.6 | (2.3) | 18.5 | (2.1) | 15.3 | (1.5) |
SE = Standard error; y = years; NA = Not applicable
Descriptive statistics are weighted to adjust for sampling design and reflect the demographic characteristics of the Cook County Juvenile Temporary Detention Center.
Because some participants were interviewed more often than others, we used a subset of interviews to summarize prevalence rates at 3 time points: baseline (Time 0), Time 1 and Time 2. The sample consisted of n = 657, 605, and 568 females at baseline, Time 1, and Time 2, respectively.
Assessed at baseline for participants who were interviewed after the DISC-IV post-traumatic stress disorder module became available (n = 374 females).
Not assessed at baseline.
Because there are no impairment criteria for a diagnosis of hypomania, prevalence rates of hypomania with and without impairment are the same.
Assessed for participants younger than 18 years old (n = 657, 148, and 21 females at baseline, Time 1, and Time 2, respectively). We do not estimate prevalence for cells with fewer than 20 participants.
For participants younger than 18, Any Disruptive Behavior disorder is defined as having conduct disorder or oppositional defiant disorder. For participants 18 and older, it is defined as having antisocial personality disorder.
Assessed for participants 18 and older at Time 1 and Time 2 (n = 457 and 547 females, respectively). Not assessed at baseline because the sample consisted of juveniles.
eTable 2 and eTable 3 show prevalence rates of disorder by race/ethnicity for males and females. Among males, 44% of African Americans, 50% of Hispanics, and 64% of non-Hispanic whites had any disorder at Time 2. More than one-quarter of African American females and more than one-third of Hispanic and non-Hispanic white females had any disorder.
Mood Disorders
Other than mania, prevalence rates decreased as participants aged. For every additional year of age, there was an approximate 10% decrease in the odds of any mood disorder (adjusted odds ratio [AOR], 0.91; 95% CI, 0.85–0.97) and its subcategories: any major mood disorder (AOR, 0.89; 95% CI, 0.82–0.96) and major depression (AOR, 0.91; 95% CI, 0.84–0.98). The prevalence of dysthymia also decreased with age (AOR, 0.57; 95% CI, 0.46–0.70).
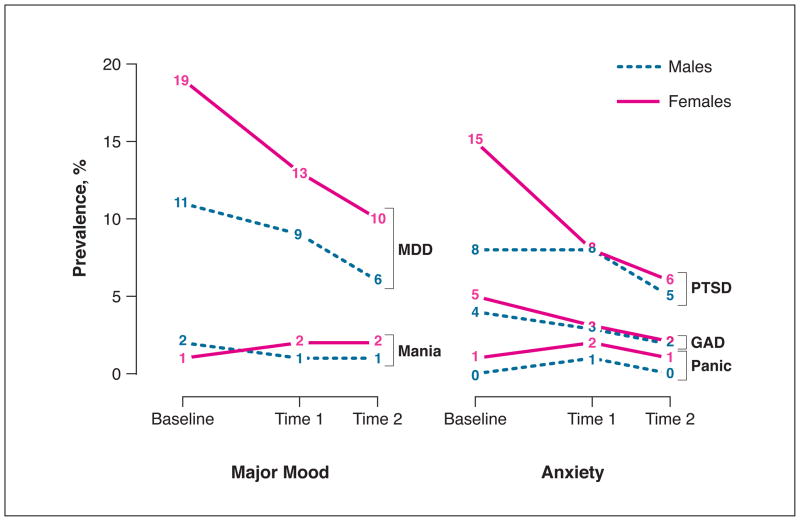
Sex Differences. Over time, females had higher rates of any mood disorder (AOR, 1.33; 95% CI, 1.05–1.68) and its subcategories: any major mood disorder (AOR, 1.54; 95% CI, 1.19–2.00) and major depression (AOR, 1.59; 95% CI, 1.22–2.08). Figure 1 illustrates prevalence rates of major mood disorders over time by sex.
Racial/Ethnic Differences. The only significant racial/ethnic difference was for mania, which was more prevalent among minorities over time (African American [AA] vs non-Hispanic white [W]: AOR, 6.92; 95% CI, 1.78–26.88; Hispanic [H] vs W: AOR, 8.01; 95% CI, 2.05–31.38).
Figure 1.
Past year prevalence of major mood disorders (major depression [MDD], mania) and anxiety disorders (post-traumatic stress disorder [PTSD], generalized anxiety disorder [GAD], and panic disorder) by sex.
Anxiety Disorders
The prevalence of panic disorder increased slightly overall (AOR, 1.30 per year; 95% CI, 1.03–1.65).
Sex Differences. Figure 1 shows changes in prevalence rates over time by sex. Females had higher rates of any anxiety disorder (AOR, 1.42; 95% CI, 1.06–1.91). Although rates of PTSD appeared to decrease, especially for females, this trend was not statistically significant (AOR, 0.93; 95% CI, 0.81–1.05).
Racial/Ethnic Differences. Compared with non-Hispanic whites, Hispanics had more than twice the odds of any anxiety disorder (AOR, 2.18; 95% CI, 1.37–3.49) and its subcategory PTSD (AOR, 2.82; 95% CI, 1.66–4.80). Compared with African Americans, Hispanics had 3.82 times the odds of panic disorder (95% CI, 1.54–9.47) and 1.54 times the odds of PTSD (95% CI, 1.01–2.34). In addition, African Americans were more likely than non-Hispanic whites to have PTSD (AOR, 1.84; 95% CI, 1.10–3.07), while non-Hispanic whites were more likely than African Americans to have panic disorder (AOR, 3.56; 95% CI, 1.28–9.94).
Disruptive Behavior Disorders
The prevalence of any disruptive behavior disorder decreased over time, but the rate of decrease depended on sex.
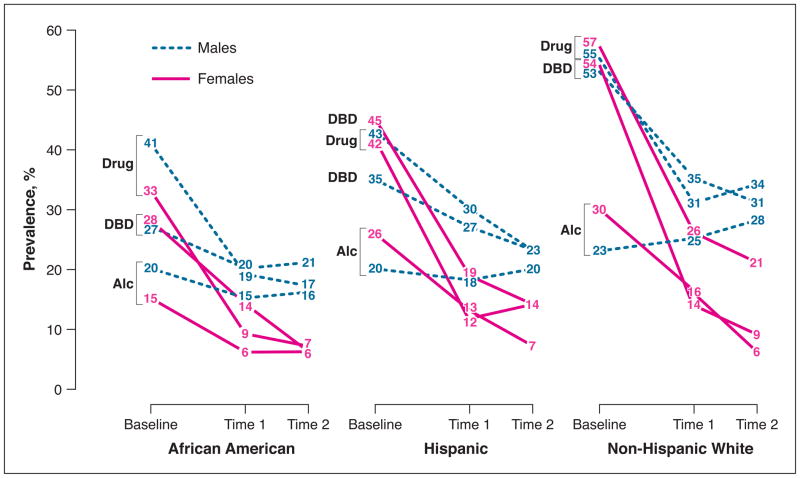
Sex Differences. Males and females did not have significantly different rates of any disruptive behavior disorder at baseline, but prevalence decreased faster among females than among males. Figure 2 illustrates these sex differences over time. Three years after baseline, males had 1.82 times the odds of any disruptive behavior disorder (95% CI, 1.46–2.26) compared with females ; five years after baseline, males had 2.95 times the odds (95% CI, 2.16–4.02).
Racial/Ethnic Differences. As illustrated in Figure 2, non-Hispanic whites had the highest rates of any disruptive behavior disorder over time (W vs AA: AOR, 2.34; 95% CI, 1.80–3.04; W vs H: AOR, 1.56; 95% CI, 1.16–2.11), followed by Hispanics (H vs AA: AOR, 1.50; 95% CI, 1.10–2.04).
Figure 2.
Past year prevalence of substance use disorders (alcohol disorder [Alc], drug disorder) and any disruptive behavior disorder (DBD) by sex and race/ethnicity.
Substance Use Disorders
Substance use disorders were the most prevalent disorders in our sample. The prevalence of substance use disorders generally decreased over time, but the rate of decrease depended on sex. Figure 2 illustrates sex and racial/ethnic differences over time.
Sex Differences. At baseline, compared with females, males had about one-third greater odds of any substance use disorder (AOR, 1.34; 95% CI, 1.05–1.71) and its subcategory, drug use disorder (AOR, 1.37; 95% CI, 1.07–1.75); rates of alcohol use disorder were not significantly different. By the follow-up interviews, however, the disparities between males and females increased substantially because prevalence rates decreased faster for females than for males. Three years after baseline, compared with females, males had approximately twice the odds of any substance use disorder (AOR, 2.00; 95% CI, 1.64–2.43) and its subcategories, drug use disorder (AOR, 2.01; 95% CI, 1.62–2.49) and alcohol use disorder (AOR, 1.97; 95% CI, 1.53–2.53). Five years after baseline, males had more than 2.5 times the odds of these disorders compared with females (respectively, AOR, 2.61; 95% CI, 1.96–3.47; AOR, 2.60; 95% CI, 1.88–3.58; AOR, 2.87; 95% CI, 2.00–4.13). Although the prevalence rates of most disorders decreased for males and females (Figure 2), three years after baseline, rates of alcohol disorder were no longer decreasing among males (AOR, 1.03 per year; 95% CI, 0.96–1.11).
Racial/Ethnic Differences. Even after adjusting for time spent in correctional facilities, substance use disorders were more common among non-Hispanic whites and Hispanics than African Americans (Figure 2). Compared with African Americans, non -Hispanic whites had nearly twice the odds of any substance use disorder and its subcategory, drug use disorder (respectively, AOR, 1.96; 95% CI, 1.54–2.49; AOR, 1.91; 95% CI, 1.50–2.43), and 1.57 times the odds of alcohol disorder (95% CI, 1.15–2.13). Hispanics had about 1.5 times the odds of any substance use disorder and its subcategory, drug use disorder, compared with African Americans (respectively, AOR, 1.59; 95% CI, 1.24–2.30; AOR, 1.46; 95% CI, 1.12–1.92).
We also analyzed substance use disorders without impairment criteria, an approach used by recent studies of the general population.50, 58 Results were substantially similar (available from the authors).
Substance Use Disorders Among Participants Living in the Community at Time 2
Because substance use is restricted in jails and prisons, we also examined rates of substance use disorders only among participants who had lived in the community the entire year prior to Time 2 (345 males and 479 females). These prevalence rates – and the demographic differences – were substantially similar to those in the entire sample (eTable 4).
Persistence
Table 3 shows the persistence of disorders: among participants who had the disorder at baseline, the proportion who still had the disorder at Time 1 or Time 2. For most disorders, rates of persistence were higher at Time 1 than at Time 2.
Sex Differences
Regardless of sex, about 1 in 5 participants had a mood disorder that persisted to Time 2. Substance use disorders were among the most persistent disorders for both males and females, but were significantly more likely to persist among males than females. Any disruptive behavior disorder was also among the most persistent disorders in males, and at Time 2 was significantly more likely to persist in males than in females.
Racial/Ethnic Differences
Among males, there were no significant racial/ethnic differences in the persistence of disorders (eTable 5). Among females, there were several significant differences (eTable 6). Compared with African Americans, non-Hispanic whites had about 3 times the odds of persisting at Time 1 with any substance use disorder and its subcategory, alcohol use disorder, and at Time 2 of persisting with drug disorder. Hispanics were also more likely than African Americans to persist at Time 1 with substance use disorder and its subcategory alcohol disorder.
COMMENT
Although prevalence rates of most psychiatric disorders declined over time, a substantial proportion of delinquent youth continue to have disorders as they age. For some youth, detention may coincide with a period of crisis that subsequently abates. Many youth, however, continue to struggle: five years after detention, when participants were ages 14 to 24 years, nearly half of males and nearly 30% of females had one or more psychiatric disorders with associated impairment.
Substance use and disruptive behavior disorders continued to be the most common disorders. For many delinquent youth – especially males – externalizing disorders were not limited to adolescence. Five years after baseline, males had 2 to 3 times the odds of having substance use and disruptive behavior disorders compared with females. Furthermore, the disparity between males and females increased over time. Males were also more likely than females to persist with substance use disorders and disruptive behavior disorder.
The observed sex differences in externalizing disorders are consistent with those in the general population, where males are up to ten times more likely than females to persist in antisocial behavior from childhood to adulthood.93 Why might males fare worse than females? First, delinquent males are less likely to receive services than females.94 Second, delinquent males may have fewer opportunities to assume age-appropriate social roles—jobs, post-secondary schooling—turning points that might reduce problem behaviors.95 Finally, precocious transition to adult social roles, such as parenthood, may be associated with worse outcomes for males than for females.96–98
As in the general population,99 females had higher rates of internalizing disorders than males. The persistence of mood disorders, about 20%, was similar in males and females.
Rates of substance use disorders and disruptive behavior disorders were lower in African Americans than non-Hispanic whites. These findings may reflect underlying racial/ethnic disparities in the legal system, 71, 100–102 and the different pathways by which non -Hispanic whites and racial/ethnic minorities enter the system. We found racial/ethnic differences in substance use disorders even after taking into account that African Americans spend more time in correctional facilities—where access to alcohol and drugs is restricted.100, 101 Our findings add to the growing debate about how the “War on Drugs” has affected the disproportionate incarceration of African Americans. Many investigators suggest that disproportionate minority confinement for drug offenses is due, in part, to disparate enforcement of drug laws in African American communities, rather than higher rates of use or dealing.103–106 Our findings appear consistent with this view.
It is difficult to compare specific prevalence rates in our sample with those in the general population because differences in instrumentation and sample demographics limit meaningful comparisons. The National Comorbidity Survey Replication (NCS-R) provides the most comparable data to our Time 2 interview. Although the NCS-R used different, and often less stringent, impairment criteria and did not assess the same disorders (such as antisocial personality disorder), it provides DSM-IV diagnoses for a similarly aged sample (18–24 years).107, 108 The most marked discrepancies between our findings and NCS-R were for drug use disorders, regardless of sex and race/ethnicity. For example, we found about 20% of males had a drug use disorder, compared with about 7% in the NCS-R; nearly 14% of Hispanic females and nearly one-quarter of Hispanic males had a drug use disorder, compared with less than 5% of Hispanics in the NCS-R.99
Changes in prevalence over time mirror those in the general population for most disorders. As summarized in the recent literature review by Costello et al,109 many disorders in the general population decrease from adolescence to young adulthood, with the exception of panic disorders and substance use disorders, which increase;48, 110–115 findings on depression have been equivocal.48, 110–115 Again, our sample is most notably different than the general population in substance use disorders: our rates decreased over time. Perhaps substance abuse peaks earlier in delinquent youth, coinciding with the general course of delinquent behavior.116, 117 In contrast, general population youth may experience events that increase the likelihood of substance abuse as they age118, 119-- living in college dormitories, freedom from social controls, delays in assuming adult responsibilities such as parenting –events less likely to be experienced by delinquent youth.120
In terms of persistence, the most recent comparable investigation48 that was conducted in the United States using a sample of similar age and DSM-based criteria (albeit different measures) found lower rates of persistence of depression and disruptive behavior disorders than in our sample. (Persistence of substance use disorders are not comparable because definitions differed; Copeland et al48 used more liberal impairment criteria and included nicotine.)
Limitations
Our data are subject to the limitations of self-report. Moreover, it was not feasible to study more than one jurisdiction; because the prevalence of psychiatric disorders may vary across jurisdictions,14, 121, 122 generalizability may be limited. We cannot know if psychiatric disorders increase the likelihood of arrest and detention or vice versa. Findings might have been marginally different had we been able to use identical measures and time frames at the baseline and follow-up interviews. Rates would likely have been higher had caretakers been available to provide independent reports at baseline.15 At the follow-up interviews, many participants were not eligible to have caretakers interviewed because the participants were older than 17 years or did not live with a caretaker. Although retention rates were high, participants who missed interviews might be more likely to have had disorders than those who were found. Our findings do not take into account mental health services that might have been provided. Despite these limitations, our findings have implications for future research and mental health policy.
Directions for Future Research
Retain incarcerated persons in longitudinal studies of psychiatric disorders. Most large-scale longitudinal studies of the general population do not retain persons who become incarcerated by follow-up (such as the National Epidemiologic Survey on Alcohol and Related Conditions123) or reinterview too few to analyze (the Epidemiologic Catchment Area Study 124). Thus, these samples are biased: they systematically exclude persons who, as our study suggests, are likely to have psychiatric disorders and poor outcomes. Excluding incarcerated persons biases prevalence rates, especially for African American males. At any given time, nearly 1 in 9 African American males, ages 25 to 34 years, are incarcerated.71 To address health disparities, we must include correctional populations, which have increased from approximately 2 million in 2000 to nearly 2.4 million in 2008.71, 125
Add variables on incarceration history to general population studies. Although many studies examine the prevalence of psychiatric disorders in incarcerated populations,13–16, 74, 121, 126–128 few focus on the effect of incarceration on psychiatric disorders. We suggest that general population epidemiologic surveys add the following variables: number of incarcerations, age at time of incarceration, length of incarcerations, and experiences in “community corrections” (parole, probation, and community supervision). This strategy would generate necessary information on how disproportionate confinement of racial/ethnic minorities affects health disparities in psychiatric disorders and related outcomes.
Include females in longitudinal studies of delinquents. The observed sex differences underscore that findings for males may not generalize to females. Yet, most longitudinal studies of delinquents exclude females or sample too few to analyze sex differences. (Summary tables are available from the authors.) Future studies must include females and collect data on pregnancy, childbirth, and child-rearing. We will then have the requisite empirical foundation to improve sex-specific mental health services, especially needed now that females comprise an increasing proportion (now 30%129) of juvenile arrests.
Examine variables that affect trajectories of disorder in high-risk youth. Few studies of high-risk youth examine trajectories of disorder; fewer still examine how potentially modifiable risk and protective factors predict trajectories of disorder. Future studies should investigate how social, cognitive, and biological factors interact to affect trajectories. For example, advances in neuroscience research provide unique opportunities to investigate how developmental differences in emotion regulation interact with “turning points” to alter trajectories.130–132
Implications for Mental Health Policy
Focus on delinquent males. In recent years, innovative programs funded by the Office of Juvenile Justice and Delinquency Prevention133—such as Girl Talk,134 and Girl Scouts in Detention Centers—addressed the needs of delinquent females.135–137 The mental health system must now improve services for males, who comprise 70% of juvenile arrests and 85% of youth in correctional facilities.17, 129 Our findings demonstrate that interventions for substance use and disruptive behavior disorders are especially needed. Comprehensive interventions, such as functional family therapy,138 multidimensional treatment foster care,139 and multisystemic therapy, 140 can be effective. Continued development and dissemination of these programs can further reduce illegal behaviors and provide cost-effective alternatives to incarceration.141
Assess and treat substance use disorders in correctional facilities and after release. Irrespective of sex or race/ethnicity, alcohol and drug use disorders were among the most common and persistent disorders. Yet, the need for services far exceeds their availability. About one-half of youth in juvenile correctional facilities142, 143 and about three -quarters of youth in adult jails and prisons who need substance abuse treatment do not receive it.142 Incarcerated adults fare much worse: summarizing Department of Justice statistics,144, 145 a recent study published in JAMA concluded that 80% to 85% of adult prisoners who needed treatment for drug abuse did not receive it.146 After release back to the community, services may be difficult to obtain. SAMHSA reports, for example, that fewer than 10% of juveniles147 and adults 148 with an “alcohol use problem” received specialty services in the past year.
Despite the promise of health care reform, service provision is not likely to improve mental health services for persons like our participants, who may frequently cycle through correctional facilities. Incarceration disrupts community treatment. Moreover, the expansion of Medicaid provides no benefit to prisoners because federal law prohibits Medicaid payments for individuals—juvenile or adult—who are inmates of public institutions (20 CFR §416.211). Health Care Reform also does not improve the deteriorating public health infrastructure (“safety-net programs”), where many impoverished persons would receive treatment149, 150 after they are released. We must improve services in corrections and in the community, where virtually all detained juveniles and incarcerated adults will eventually return.
Supplementary Material
Acknowledgments
This work was supported by National Institute on Drug Abuse grants R01DA019380, R01DA022953, and R01DA028763, National Institute of Mental Health grants R01MH54197 and R01MH59463 (Division of Services and Intervention Research and Center for Mental Health Research on AIDS) and grants 1999-JE-FX-1001, 2005-JL-FX-0288 and 2008-JF-FX-0068 from the Office of Juvenile Justice and Delinquency Prevention. Major funding was also provided by the National Institute on Alcohol Abuse and Alcoholism, the NIH Office of Behavioral and Social Sciences Research, Substance Abuse and Mental Health Services Administration (Center for Mental Health Services, Center for Substance Abuse Prevention, Center for Substance Abuse Treatment), the NIH Center on Minority Health and Health Disparities, the Centers for Disease Control and Prevention (National Center for Injury Prevention and Control and National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention), the NIH Office of Research on Women’s Health, the NIH Office of Rare Diseases, Department of Labor, Department of Housing and Urban Development, The William T. Grant Foundation, and The Robert Wood Johnson Foundation. Additional funds were provided by The John D. and Catherine T. MacArthur Foundation, The Open Society Institute, and The Chicago Community Trust.
This work could not have been accomplished without the advice of Celia Fisher, Ph.D. We thank our participants for their time and willingness to participate, our talented project staff, especially Elena Bassett, MS, Lynda Carey, MA, Jennifer Heil, MA, Kathryn Jacoby, BA, and Nichole Olson, BS, as well as the Cook County and State of Illinois systems for their cooperation. We also thank the anonymous reviewers, who provided insightful and incisive comments on earlier drafts.
Footnotes
Dr. Teplin had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All other authors had full access to all study data.
Financial Disclosure: Dr. Dulcan receives book royalties from American Psychiatric Publishing, Inc. She sat on the ADHD/RD and Strattera Advisory Boards of Eli Lilly Company, most recently in 2009. She is a consultant for Care Management Technologies, Inc. All other authors have no relevant financial interests to disclose.
References
- 1.Davis DL, Bean GJ, Schumacher JE, Stringer TL. Prevalence of emotional disorders in a juvenile justice institutional population. American Journal of Forensic Psychology. 1991;9(1):5–17. [Google Scholar]
- 2.Forehand R, Wierson M, Frame C, Kempton T, Armistead L. Juvenile delinquency entry and persistence: do attention problems contribute to conduct problems? Journal of Behavior Therapy and Experimental Psychiatry. 1991;22(4):261–264. doi: 10.1016/0005-7916(91)90042-4. [DOI] [PubMed] [Google Scholar]
- 3.Eppright TD, Kashani JH, Robison BD, Reid JC. Comorbidity of conduct disorder and personality disorders in an incarcerated juvenile population. American Journal of Psychiatry. 1993;150(8):1233–1236. doi: 10.1176/ajp.150.8.1233. [DOI] [PubMed] [Google Scholar]
- 4.Rohde P, Mace DE, Seeley JR. The association of psychiatric disorders with suicide attempts in a juvenile delinquent sample. Criminal Behavior and Mental Health. 1997;7:187–200. [Google Scholar]
- 5.Steiner H, Garcia IG, Mathews Z. Posttraumatic stress disorder in incarcerated juvenile delinquents. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(3):357–365. doi: 10.1097/00004583-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Timmons-Mitchell J, Brown C, Schulz SC, Webster SE, Underwood LA, Semple WE. Comparing the mental health needs of female and male incarcerated juvenile delinquents. Behavioral Sciences and the Law. 1997;15:195–202. doi: 10.1002/(sici)1099-0798(199721)15:2<195::aid-bsl269>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 7.Cauffman E, Feldman S, Waterman J, Steiner H. Posttraumatic stress disorder among female juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(11):1209–1216. [PubMed] [Google Scholar]
- 8.Duclos CW, Beals J, Novins DK, Martin C, Jewett CS, Manson SM. Prevalence of common psychiatric disorders among American Indian adolescent detainees. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(8):866–873. doi: 10.1097/00004583-199808000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Erwin BA, Newman E, McMackin RA, Morrissey C, Kaloupek DG. PTSD, malevolent environment, and criminality among criminally involved male adolescents. Criminal Justice and Behavior. 2000;27(2):196–215. [Google Scholar]
- 10.Pliszka SR, Sherman JO, Barrow MV, Irick S. Affective disorder in juvenile offenders: a preliminary study. American Journal of Psychiatry. 2000;157(1):130–132. doi: 10.1176/ajp.157.1.130. [DOI] [PubMed] [Google Scholar]
- 11.Shelton D. Emotional disorders in young offenders. Image -the Journal of Nursing Scholarship. 2001;33(3):259–263. doi: 10.1111/j.1547-5069.2001.00259.x. [DOI] [PubMed] [Google Scholar]
- 12.Wasserman GA, McReynolds LS, Lucas CP, Fisher P, Santos L. The voice DISC-IV with incarcerated male youths: prevalence of disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(3):314–321. doi: 10.1097/00004583-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Domalanta DD, Risser WL, Roberts RE, Risser WL. Prevalence of depression and other psychiatric disorders among incarcerated youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(4):477–484. doi: 10.1097/01.CHI.0000046819.95464.0B. [DOI] [PubMed] [Google Scholar]
- 14.Fazel S, Doll H, Långström N. Mental disorders among adolescents in juvenile detention and correctional facilities: A systematic review and metaregression analysis of 25 surveys. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(9):1010–1019. doi: 10.1097/CHI.ObO13e31817eecf3. [DOI] [PubMed] [Google Scholar]
- 15.Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59(12):1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karnik NS, Soller M, Redlich A, Silverman M, Kraemer HC, Haapanen R, Steiner H. Prevalence of and gender differences in psychiatric disorders among juvenile delinquents incarcerated for nine months. Psychiatric Services. 2009;60(6):838–841. doi: 10.1176/ps.2009.60.6.838. [DOI] [PubMed] [Google Scholar]
- 17.Sickmund M, Sladky TJ, Kang W. [Accessed November 25, 2008];Census of Juveniles in Residential Placement Databook. http://www.ojjdp.ncjrs.org/ojstatbb/cjrp/
- 18.Wareham J, Dembo R. A Longitudinal Study of Psychological Functioning Among Juvenile Offenders: A Latent Growth Model Analysis. Criminal Justice and Behavior. 2007;34(2):259–273. [Google Scholar]
- 19.Dixon A, Howie P, Starling J. Psychopathology in female juvenile offenders. Journal of Child Psychology & Psychiatry. 2004;45(6):1150–1158. doi: 10.1111/j.1469-7610.2004.00307.x. [DOI] [PubMed] [Google Scholar]
- 20.Gover AR. Childhood sexual abuse, gender, and depression among incarcerated youth. International Journal of Offender Therapy and Comparative Criminology. 2004;48(6):683–696. doi: 10.1177/0306624X04264459. [DOI] [PubMed] [Google Scholar]
- 21.Dembo R, Jainchill N, Turner C, Chunki F, Farkas S, Childs K. Levels of psychopathy and its correlates: A study of incarcerated youths in three states. Behavioral Sciences & the Law. 2007;25(5):717–738. doi: 10.1002/bsl.784. [DOI] [PubMed] [Google Scholar]
- 22.Perron BE, Howard MO. Prevalence and correlates of traumatic brain injury among delinquent youths. Criminal Behaviour and Mental Health. 2008;18(4):243–255. doi: 10.1002/cbm.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hiscoke UL, Langstrom N, Ottosson H, Grann M. Self-reported personality traits and disorders (DSM-IV) and risk of criminal recidivism: A prospective study. Journal of Personality Disorders. 2003;17(4):293–305. doi: 10.1521/pedi.17.4.293.23966. [DOI] [PubMed] [Google Scholar]
- 24.Vermeiren R, Schwab-Stone M, Ruchkin V, De Clippele A, Deboutte D. Predicting recidivism in delinquent adolescents from psychological and psychiatric assessment. Comprehensive Psychiatry. 2002;43(2):142–149. doi: 10.1053/comp.2002.30809. [DOI] [PubMed] [Google Scholar]
- 25.Randall J, Henggeler SW, Pickrel SG, Brondino MJ. Psychiatric comorbidity and the 16-month trajectory of substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(9):1118–1124. doi: 10.1097/00004583-199909000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Douglas KS, Epstein ME, Poythress NG. Criminal recidivism among juvenile offenders: Testing the incremental and predictive validity of three measures of psychopathic features. Law and Human Behavior. 2008;32(5):423–438. doi: 10.1007/s10979-007-9114-8. [DOI] [PubMed] [Google Scholar]
- 27.Harrington RC, Kroll L, Rothwell J, McCarthy K, Bradley D, Bailey S. Psychosocial needs of boys in secure care for serious or persistent offending. Journal of Child Psychology and Psychiatry. 2005;46(8):859–866. doi: 10.1111/j.1469-7610.2004.00388.x. [DOI] [PubMed] [Google Scholar]
- 28.Craig TKJ, Hodson S. Homeless youth in London: II. Accommodation, employment and health outcomes at 1 year. Psychological Medicine. 2000;30(1):187–194. doi: 10.1017/s0033291799001488. [DOI] [PubMed] [Google Scholar]
- 29.Meyer SE, Carlson GA, Youngstrom E, Ronsaville DS, Martinez PE, Gold PW, Hakak R, Radke-Yarrow M. Long-term outcomes of youth who manifested the CBCL-Pediatric Bipolar Disorder phenotype during childhood and/or adolescence. Journal of Affective Disorders. 2009;113(3):227–235. doi: 10.1016/j.jad.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 30.Mason WA, Kosterman R, Hawkins JD, Herrenkohl TI, Lengua LJ, McCauley E. Predicting depression, social phobia, and violence in early adulthood from childhood behavior problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(3):307–315. doi: 10.1097/00004583-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Cohen P, Chen H, Crawford TN, Brook JS, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug and Alcohol Dependence. 2007;88:S71–s84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fothergill KE, Ensminger ME. Childhood and adolescent antecedents of drug and alcohol problems: A longitudinal study. Drug and Alcohol Dependence. 2006;82(1):61–76. doi: 10.1016/j.drugalcdep.2005.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fothergill KE, Ensminger ME, Green KM, Crum RM, Robertson J, Juon H-S. The impact of early school behavior and educational achievement on adult drug use disorders: A prospective study. Drug and Alcohol Dependence. 2008;92(1):191–199. doi: 10.1016/j.drugalcdep.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crum RM, Juon H-S, Green KM, Robertson J, Fothergill K, Ensminger M. Educational achievement and early school behavior as predictors of alcohol-use disorders: 35-year follow-up of the Woodlawn Study. Journal of Studies on Alcohol. 2006;67(1):75–85. doi: 10.15288/jsa.2006.67.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Egeland JA, Shaw JA, Endicott J, Pauls DL, Allen CR, Hostetter AM, Sussex JN. Prospective study of prodromal features for bipolarity in well Amish children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(7):786–796. doi: 10.1097/01.CHI.0000046878.27264.12. [DOI] [PubMed] [Google Scholar]
- 36.Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents: 10 years later. Archives of General Psychiatry. 1997;54:932–940. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- 37.Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: A survival analysis. Journal of Clinical Child Psychology. 1999;28(3):333–341. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- 38.Barnow S, Schuckit M, Smith T, Freyberger HJ. Predictors of attention problems for the period from pre-teen to early teen years. Psychopathology. 2006;39:227–235. doi: 10.1159/000093923. [DOI] [PubMed] [Google Scholar]
- 39.King KM, Chassin L. A Prospective Study of the Effects of Age of Initiation of Alcohol and Drug Use on Young Adult Substance Dependence. Journal of Studies on Alcohol and Drugs. 2007;68(2):256–265. doi: 10.15288/jsad.2007.68.256. [DOI] [PubMed] [Google Scholar]
- 40.King KM, Chassin L. Adolescent stressors, psychopathology, and young adult substance dependence: A prospective study. Journal of Studies on Alcohol and Drugs. 2008;69(5):629–638. doi: 10.15288/jsad.2008.69.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kirisci L, Tarter RE, Reynolds M, Vanyukov M. Individual differences in childhood neurobehavior disinhibition predict decision to desist substance use during adolescence and substance use disorder in young adulthood: A prospective study. Addictive Behaviors. 2006;31(4):686–696. doi: 10.1016/j.addbeh.2005.05.049. [DOI] [PubMed] [Google Scholar]
- 42.Kirisci L, Tarter R, Mezzich A, Vanyukov M. Developmental trajectory classes in substance use disorder etiology. Psychology of Addictive Behaviors. 2007;21(3):287–296. doi: 10.1037/0893-164X.21.3.287. [DOI] [PubMed] [Google Scholar]
- 43.Nigg J, Wong M, Martel M, Jester J, Puttler L, Glass J, Adams K, Fitzgerald H, Zucker R. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(4):468–475. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- 44.Buu A, DiPiazza C, Wang J, Puttler LI, Fitzgerald HE, Zucker RA. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. Journal of Studies on Alcohol and Drugs. 2009;70(4):489–498. doi: 10.15288/jsad.2009.70.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reynolds MD, Tarter R, Kirisci L, Kirillova G, Brown S, Clark DB, Gavaler J. Testosterone levels and sexual maturation predict substance use disorders in adolescent boys: A prospective study. Biological Psychiatry. 2007;61(11):1223–1227. doi: 10.1016/j.biopsych.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 46.Trim RS, Meehan BT, King KM, Chassin L. The relation between adolescent substance use and young adult internalizing symptoms: Findings from a high-risk longitudinal sample. Psychology of Addictive Behaviors. 2007;21(1):97–107. doi: 10.1037/0893-164X.21.1.97. [DOI] [PubMed] [Google Scholar]
- 47.Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of Youth: Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53(12):1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 48.Copeland WE, Shanahan L, Costello J, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 50.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Merikangas K, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MCD, Compton WC, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 53.Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(1):56–63. doi: 10.1097/00004583-199901000-00020. [DOI] [PubMed] [Google Scholar]
- 54.Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry. 2000;157(10):1584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- 55.Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. Mahwah, NJ US: Lawrence Erlbaum Associates Publishers; 1998. [Google Scholar]
- 56.Briggs-Gowan MJ, Owens PL, Schwab-Stone ME, Leventhal JM, Leaf PJ, Horowitz SM. Persistence of psychiatric disorders in pediatric settings. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(11):1360–1369. doi: 10.1097/01.CHI.0000084834.67701.8a. [DOI] [PubMed] [Google Scholar]
- 57.Costello EJ, Angold A, Keeler GP. Adolescent outcomes of childhood disorders: The consequences of severity and impairment. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(2):121–128. doi: 10.1097/00004583-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 58.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 59.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 60.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 61.Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S-M, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and Alcohol Dependence. 2007;88:S38–s49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR. Longitudinal associations between depressive and anxiety disorders: A comparison of two trait models. Psychological Medicine. 2008;38(3):353–363. doi: 10.1017/S0033291707001341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wiesner M. A longitudinal latent variable analysis of reciprocal relations between depressive symptoms and delinquency during adolescence. Journal of Abnormal Psychology. 2003;112(4):633–645. doi: 10.1037/0021-843X.112.4.633. [DOI] [PubMed] [Google Scholar]
- 65.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 66.Office of Human Research Protections. OHRP Guidance on the Involvement of Prisoners in Research. Bethesda, MD: Department of Health and Human Services; 2003. [Google Scholar]
- 67.Snyder HN, Sickmund M. Juvenile Offenders and Victims: 1999 National Report. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 1999. NCJ 178257. [Google Scholar]
- 68.US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 69.U.S. Department of Health and Human Services. [Accessed December, 2010];Healthy People 2020. http://www.healthypeople.gov/
- 70.Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC US: Institute of Medicine of the National Academies; 2003. [PubMed] [Google Scholar]
- 71.West HC. Prison Inmates at Midyear 2009 -Statistical Tables. Washington, D.C: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2010. [Google Scholar]
- 72.US Census Bureau. Resident Population by Race, Hispanic Origin, and Single Years of Age: 2009. Table 20. [Accessed March 18, 2011];Monthly Resident Population Estimates by Age, Sex, Race and Hispanic Origin for the United States: April 1, 2000 to December 1, 2010. 2011 [ http://www.census.gov/popest/national/asrh/2009-nat-res.html.
- 73.Abram KM, Teplin LA, Charles DR, Longworth SL, McClelland GM, Dulcan MK. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;661:403–410. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abram KM, Teplin LA, McClelland GM, Dulcan MK. Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2003;60(11):1097–1108. doi: 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Federal Policy for the Protection of Human Subjects: Notices and Rules. Part 2. Federal Register. 1991 Jun 18;56(117):28002–32. (56 FR 28002) [PubMed] [Google Scholar]
- 76.Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, Lahey BB, Bourdon K, Jensen PS, Bird HR, Canino G, Regier DA. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the Meca Study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 77.Fisher PW, Shaffer D, Piacentini J, Lapkin J, Kafantaris V, Leonard H, Herzog D. Sensitivity of the Diagnostic Interview Schedule for Children, 2nd edition (DISC-2.1) for specific diagnoses of children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):666–673. doi: 10.1097/00004583-199305000-00026. [DOI] [PubMed] [Google Scholar]
- 78.Piacentini J, Shaffer D, Fisher PW, Schwab-Stone M, Davies M, Gioia E. The Diagnostic Interview Schedule for Children--Revised Version (DISC--R): III. Concurrent criterion validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):658–665. doi: 10.1097/00004583-199305000-00025. [DOI] [PubMed] [Google Scholar]
- 79.Schwab-Stone M, Fisher PW, Piacentini J, Shaffer D, Davies M, Briggs M. The Diagnostic Interview Schedule for Children--Revised version (DISC--R): II. Test-retest reliability. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):651–657. doi: 10.1097/00004583-199305000-00024. [DOI] [PubMed] [Google Scholar]
- 80.Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Goodman SH, Lahey BB, Lichtman JH, Canino G, Rubio-Stipec M, Rae DS. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(7):878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- 81.Shaffer D, Schwab-Stone M, Fisher PW, Cohen P, Piacentini J, Davies M, Conners C, Reiger D. The Diagnostic Interview Schedule for Children--Revised version (DISC--R): I. Preparation, field testing, interrater reliability, and acceptability. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):643–650. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- 82.Shaffer D, Fisher P, Lucas C. The Diagnostic Interview Schedule for Children (DISC) In: Hilsenroth MJ, Segal DL, editors. Comprehensive Handbook of Psychological Assessment. Vol. 2. Hoboken, NJ: John Wiley & Sons; 2003. pp. 256–270. [Google Scholar]
- 83.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 84.Canino G, Shrout PE, Rubio-Stipec M, Bird HR, Bravo M, Ramirez R, Chavez L, Alegria M, Bauermeister JJ, Hohmann A, Ribera J, Garcia P, Martinez-Taboas A. The DSM-IV rates of child and adolescent disorders in Puerto Rico. Archives of General Psychiatry. 2004;61:85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- 85.Robins LN, Cottler LB, Bucholz KK, Compton WM. Diagnostic Interview Schedule for DSM-IV (DIS-IV) St. Louis, MO: Washington University; 1995. [Google Scholar]
- 86.Compton WM, Cottler LB. The Diagnostic Interview Schedule (DIS) In: Hilsenroth M, Segal DL, editors. Comprehensive Handbook of Psychological Assessment. Vol. 2. Hoboken, NJ: John Wiley & Sons; 2004. pp. 153–162. [Google Scholar]
- 87.Korn E, Graubard B. Analysis of Health Surveys. New York: Wiley; 1999. [Google Scholar]
- 88.Cochran WG. Sampling Techniques. New York, NY: John Wiley & Sons; 1977. [Google Scholar]
- 89.Levy PS, Lemeshow S. Sampling of Populations: Methods and Applications. New York, NY: John Wiley & Sons; 1999. [Google Scholar]
- 90.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 91.Molenberghs G, Verbeke G. Models for Discrete Longitudinal Data. Springer; 2006. [Google Scholar]
- 92.Stata Stastical Software: Release 11 [computer program]. Version. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 93.Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Development and Psychopathology. 2002;14(1):179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- 94.Teplin LA, Abram KM, McClelland GM, Washburn JJ, Pikus AK. Detecting mental disorder in juvenile detainees: Who receives services. American Journal of Public Health. 2005;95(10):1773–1780. doi: 10.2105/AJPH.2005.067819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sampson RJ, Laub JH. Crime and deviance in the life course. Annual Review of Sociology. 1992;18:63–84. [Google Scholar]
- 96.Kreager DA, Matsueda RL, Erosheva EA. Motherhood and Criminal Desistance in Disadvantaged Neighborhoods. Criminology. 2010;48(1):221–258. [Google Scholar]
- 97.Hope TL, Wilder EI, Watt TT. The relationships among adolescent pregnancy, pregnancy resolution, and juvenile delinquency. The Sociological Quarterly. 2003;44(4) [Google Scholar]
- 98.Thornberry TP, Wei EH, Stouthamer-Loeber M, Van Dyke J. Teenage Fatherhood and Delinquent Behavior. Washington, D. C: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2000. [Google Scholar]
- 99.NCS-R dataset. [Accessed March 15, 2011];Collaborative Psychiatric Epidemiology Surveys Web site. http://www.icpsr.umich.edu/CPES.
- 100.Puzzanchera C, Kang W. Easy Access to Juvenile Court Statistics: 1985–2008. http://www.ojjdp.gov/ojstatbb/ezajcs/
- 101.Sickmund M, Sladky TJ, Kang W. Census of Juveniles in Residential Placement Databook. http://www.ojjdp.gov/ojstatbb/ezacjrp/
- 102.Minton TD. Jail Inmates at Midyear 2010 -Statistical Tables. Washington, DC: US Department of Justice; 2011. [Google Scholar]
- 103.Beckett K, Nyrop K, Pfingst L. Race, drugs, and policing: Understanding disparities in drug delivery arrests. Criminology. 2006;44(1):105–137. [Google Scholar]
- 104.Beckett K, Nyrop K, Pfingst L, Bowen M. Drug use, drug possession arrests, and the question of race: Lessons from Seattle. Social Problems. 2005;52(3):419–441. [Google Scholar]
- 105.Moore LD, Elkavich A. Who’s using and who’s doing time: Incarceration, the War on Drugs, and public health. American Journal of Public Health. 2008;98:782–786. doi: 10.2105/AJPH.2007.126284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gorvin I. Targeting Blacks: Drug Law Enforcement and Race in the United States. New York: Human Rights Watch; 2008. [Google Scholar]
- 107.National Comorbidity Survey. [Accessed March 16, 2011];Harvard School of Medicine Web site. http://www.hcp.med.harvard.edu/ncs/diagnosis.php.
- 108.NCS and NCS-R Data. [Accessed March 16, 2011];Harvard School of Medicine Web site. http://www.hcp.med.harvard.edu/ncs/ncs_data.php.
- 109.Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry. 2011;52(10):1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychological Medicine. 1998;28(1):109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- 111.Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of General Psychiatry. 2002;59(3):215–222. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- 112.Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, Connell F. A longitudinal evaluation of adolescent depression and adult obesity. Archives of Pediatrics & Adolescent Medicine. 2003;157(8):739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 113.Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of General Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 114.Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from ages 11–21. Journal of Consulting and Clinical Psychology. 1996;64(3):552–562. [PubMed] [Google Scholar]
- 115.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depression and Anxiety. 1998;7(1):3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 116.Hirschi T, Gottfredson M. Age and the explanation of crime. American Journal of Sociology. 1983;89(3) [Google Scholar]
- 117.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. 1993;100(4):674–701. [PubMed] [Google Scholar]
- 118.Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35:235–253. [Google Scholar]
- 119.White HR, Jackson K. Social and psychological influences on emerging adult drinking behavior. Alcohol Research & Health. 2004–2005;28(4):182–190. [Google Scholar]
- 120.Berzin SC, De Marco AC. Understanding the impact of poverty on critical events in emerging adulthood. Youth & Society. 2010;42(2):278–300. [Google Scholar]
- 121.Fazel S, Danesh J. Serious mental disorder in 23,000 prisoners: A systematic review of 62 surveys. The Lancet. 2002;359(9306):545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- 122.Wasserman GA, McReynolds LS, Craig SS, Keating JM, Jones SA. Psychiatric disorder, comorbidity, and suicidal behavior in juvenile justice youth. Criminal Justice and Behavior. 2010;37(12):1361–1376. [Google Scholar]
- 123.Grant B. e-mail communication. Aug 13, 2010.
- 124.Eaton W. oral communication. Aug 11, 2010.
- 125.Sickmund M. Juvenilesin Residential Placement, 1997–2008. Office of Juvenile Justice and Delinquency Prevention, US Department of Justice; 2010. [Google Scholar]
- 126.Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women: Pretrial jail detainees. Archives of General Psychiatry. 1996;53(6):505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- 127.Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women: Convicted felons entering prison. Archives of General Psychiatry. 1996;53(6):513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- 128.Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatric Services. 2009;60(6):761–765. doi: 10.1176/ps.2009.60.6.761. [DOI] [PubMed] [Google Scholar]
- 129.Puzzanchera C. Juvenile Arrests 2008. US Departemnt of Justice, Office of Juvenile Justice and Delinquency Prevention; 2009. NCJ 228479. [Google Scholar]
- 130.Feder A, Nestler EJ, Charney DS. Psychobiology and molecular genetics of resilience. Nature Reviews Neuroscience. 2009;10(6):446–457. doi: 10.1038/nrn2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Drabant EM, McRae K, Manuck SB, Hariri AR, Gross JJ. Individual differences in typical reappraisal use predict amygdala and prefrontal responses. Biological Psychiatry. 2009;65(5):367–373. doi: 10.1016/j.biopsych.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN. Prefrontal-Subcortical Pathways Mediating Successful Emotion Regulation. Neuron. 2008;59(6):1037–1050. doi: 10.1016/j.neuron.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.US Department of Justice. Correctional Populations in the United States, 1998. Washington, DC: US Department of Justice; 2001. NCJ 192929. [Google Scholar]
- 134.Shaffner L. A study of GIRLS LINK collaborative; part one: The evaluation of the GIRLS LINK collaborative. Chicago, IL: Cook County Bureau of Public Safety and Judicial Coordination; 2002. [Google Scholar]
- 135.Slowikowski J. In Focus: Girls’ Delinquency. Washington, DC: US Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2010. [Google Scholar]
- 136.Greene Peters and Associates. [Accessed March, 22, 2005];Guiding principles for promising female programming: An inventory of best practices. http://www.ojjdp.ncjrs.org/pubs/principles/contents.html.
- 137.Sherman FT. Pathways to Juvenile Detention Reform: Detention Reform and Girls. Baltimore, MD: The Annie E. Casey Foundation; 2005. [Google Scholar]
- 138.Gordon DA, Arbuthnot J, Gustafson KE, McGreen P. Home-based behavioral-systems family therapy with disadvantaged juvenile delinquents. American Journal of Family Therapy. 1988;16(3):243–255. [Google Scholar]
- 139.Chamberlain P, Leve LD, DeGarmo DS. Multidimensional treatment foster care for girls in the juvenile justice system: Two year follow-up of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2007;75(1):187–193. doi: 10.1037/0022-006X.75.1.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Henggeler SW, Clingempeel WG, Brondino MJ, Pickerel SG. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(7):868–874. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- 141.Aos S, Phillips P, Barnoski B, Lieb R. The Comparative Costs and Benefits of Programs to Reduce Crime. Olympia, WA: Washington State Institute for Public Policy; 2001. [Google Scholar]
- 142.Mulvey EP, Schubert CA, Chung H. Service use after court involvement in a sample of serious adolescent offenders. Children and Youth Services Review. 2007;29:518–544. doi: 10.1016/j.childyouth.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sedlak AJ, McPherson KS. Youth’s Needs and Services: Findings from the Survey of Youth in Residential Placement. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2010. [Google Scholar]
- 144.Karberg JC, James DJ. Substance Dependence, Abuse, and Treatment of Jail Inmates, 2002. U.S. Department of Justice; 2005. [Google Scholar]
- 145.Mumola CJ, Karberg JC. Drug Use and Dependence, State and Federal Prisoners, 2004. U.S. Department of Justice; 2006. [Google Scholar]
- 146.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: Imporving public health and safety. Journal of the American Medical Association. 2009;301(2):183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. [Google Scholar]
- 148. [Accessed October 4, 2010];2009 National Survey on Drug Use and Health: Detailed Tables. http://oas.samhsa.gov/NSDUH/2k9NSDUH/tabs/LOTSect5pe.htm#TopOfPage.
- 149.Jacobson PD, Gostin LO. Restoring health to health reform. Journal of the American Medical Association. 2010;304(1):85–86. doi: 10.1001/jama.2010.917. [DOI] [PubMed] [Google Scholar]
- 150.Katz MH. Future of the safety net under health reform. Journal of the American Medical Association. 2010;304(6):679–680. doi: 10.1001/jama.2010.1126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.