Abstract
We investigated the response of insulin-like growth factor (IGF- I), insulin-like growth factor binding protein-3 (IGFBP-3) and some hormones, i.e., testosterone (T), growth hormone (GH), cortisol (C), and insulin (I), to maximal exercise in road cyclists with and without diagnosed left ventricular hypertrophy. M-mode and two-dimensional Doppler echocardiography was performed in 30 professional male endurance athletes and a group of 14 healthy untrained subjects using a Hewlett-Packard Image Point HX ultrasound system with standard imaging transducers. Echocardiography and an incremental physical exercise test were performed during the competitive season. Venous blood samples were drawn before and immediately after the maximal cycling exercise test for determination of somatomedin and hormonal concentrations. The basal concentration of IGF-I was statistically higher (p < 0.05) in athletes with left ventricular muscle hypertrophy (LVH) when compared to athletes with a normal upper limit of the left ventricular wall (LVN) (p < 0.05) and to the control group (CG) (p < 0.01). The IGF-I level increased significantly at maximal intensity of incremental exercise in CG (p < 0.01), LVN (p < 0.05) and LVH (p < 0.05) compared to respective values at rest. Long-term endurance training induced an increase in resting (p < 0.01) and post-exercise (p < 0.05) IGF-I/IGFBP-3 ratio in athletes with LVH compared to LVN. The testosterone (T) level was lower in LVH at rest compared to LVN and CG groups (p < 0.05). These results indicate that resting serum IGF-I concentration were higher in trained subjects with LVH compared to athletes without LVH. Serum IGF- I/IGFBP-3 elevation at rest and after exercise might suggest that IGF-I act as a potent stimulant of left ventricular hypertrophy in chronically trained endurance athletes.
Key points.
In sports training athletes engaged in the same training regimen acquired different stages of cardiac hypertrophy.
Physical exercise had a significant effect on serum insulin-like growth factor - I concentration depending on maximal oxygen uptake during endurance exercise.
Athletes with clinically diagnosed physiological left ventricular hypertrophy had higher resting serum insulin-like growth factor - I concentration compared to those without left ventricular hypertrophy and sedentary subjects.
Increased insulin-like growth factor - I release during long-term training seems to significantly contribute to sports-specific functional adaptation of the left ventricle.
Key words: Echocardiography, heart, somatomedins, anabolic hormones, endurance training.
Introduction
The heart undergoes morphological and functional changes in response to athletic training, which is known as Athletic Heart Syndrome (Rich, 2004). Athletes engaged in the same sport type for many years may acquire different stages of left ventricular hypertrophy (LVH) (Sharma, 2003), which might implicate some genetic contribution to this phenomenon (Strom et al., 2005).
Exercise induces hormonal and/or mechanical responses that are considered major LVH stimulants (Decker et al., 1997; Neri Serneri et al., 2001). The results of both in vitro and in vivo studies suggest that elevated levels of endogenous insulin- like growth factor-I (IGF-I), observed during a 2-week endurance training of laboratory animals, increases myocardial expression of IGF-I (Scheinowitz et al., 2003). Moreover, exogenous administration of IGF-I independently promotes collagen synthesis by cardiac fibroblasts, leading to cardiac hypertrophy after long-term training (Horio et al., 2005). In a human study, hemodynamic overload of the heart is associated with enhanced cardiac IGF-I formation in endurance-trained athletes (Neri Serneri et al., 2001). An increase in plasma IGF-I concentration in sedentary humans resulted in improved left ventricular inotropic function at rest (Bisi et al., 1999).
IGF-I affinity for target cells is modulated by multiple insulin growth factor binding proteins (IGFBPs) (Rosendal et al., 2002; Delafontaine et al., 2004). Of the six IGFBPs, IGF-binding protein-3 (IGFBP-3) has the highest affinity to IGF-I, and is thereby considered an important factor modulating the interaction of IGF-I with its receptors (Fischer et al., 2004; Manetta et al., 2003). It has been proposed that exercise-induced IGFBP-3 proteolysis could contribute to the anabolic effects of exercise, with more distinct changes observed in untrained subjects (Schwarz et al., 1996).
IGF secretion is under hormonal control (Kupfer et al., 1992). A number of studies have demonstrated that the interaction between growth hormone (GH) and its hepatic receptors stimulates IGF-I gene expression and IGF-I release in sedentary subjects (Kupfer et al., 1992; Manetta et al., 2002; Zanconato et al., 1994). Since endurance training is known to promote hypertrophy in cardiac myocytes (Mettauer et al., 2001), an involvement of the GH/IGF-I axis in this process can be hypothesized (Neri Serneri et al., 2001; Manetta et al., 2002). However, earlier experiments designed to test this hypothesis yielded opposite results. IGF-I concentration was found to be diminished in response to exercise in subjects participating in a short-term exercise program (up to 5 weeks), whereas an increase in serum IGF-I concentration was observed after long-term training (over 5 weeks) (Eliakim et al., 1998). Findings from several studies indicate that endurance training is associated with decreased blood testosterone (T) and increased cortisol (C) concentrations, which might potentially influence protein synthesis and degradation, thereby affecting the GH/IGF-I axis response (Mettauer et al., 2001). In line with the involvement of paracrine and endocrine factors in LVH stimulation are data obtained in patients with hypertension (Diez, 1999), and coronary heart diseases (Fischer et al., 2004; Ren et al., 1999). Diez, 1999 suggested that alterations in the synthesis, secretion, and/or bioavailability of IGF-I participated in the pathophysiology of essential hypertension. It was proposed that circulating levels of IGF-I and IGF-I to IGFBP-3 ratio increased in patients with hypertension as compared to normotensive subjects. Both IGF-I and IGF-I receptor mRNA levels in the myocardium were upregulated in an experimental angiotensin II-induced hypertension model (Brink et al., 1999) and exercise-induced physiological cardiac hypertrophy (Kim et al., 2008).
Left ventricular hypertrophy is believed to be mediated in part by circulating IGF-I (Bleumink et al., 2005; Horio et al., 2005; McMullen et al., 2004; Scheinowitz et al., 2003). If this is the case, one might suppose that exercise-induced changes in circulating IGF-I concentration in response to standard exercise would be higher in athletes with LVH compared to those who participated in the same training process within normal LV dimensions (Pelliccia et al., 1991; Sharma, 2003). Moreover, since the usage of anabolic-androgenic steroids might results in cardiac muscle cell growth independent of hemodynamic conditions, one might speculate that in athletes with LVH, hormonal response (GH, T, C) should be higher than in subjects with normal left ventricle dimension. To test this hypothesis, we investigated serum concentrations of insulin growth factor-I and insulin growth factor binding protein-3, and hormonal (testosterone, growth hormone, cortisol, and insulin) responses to graded maximal exercise in chronically endurance-trained athletes with and without diagnosed LVH.
Methods
Subjects
Thirty professional, male road cyclists volunteered to participate in the experiment (Table 1). The following inclusion criteria were used:
Table 1.
Anthropometric and physiologic characteristics of control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH). Data are means(±SD).
| VARIABLE | CG (n = 14) | LVN ( n = 15) | LVH (n = 15) |
|---|---|---|---|
| Age [yr] | 20.9 (.9) | 21.8 (2.2) | 22.5 (1.3) |
| Height [m] | 1.77 (.05) | 177.1 (4.9) | 179.7 (5.7) |
| Body mass [kg] | 72.6 (6.6) | 69.7 (5.3) | 71.0 (5.3) |
| BMI [kg·m-2] | 23.1 (2.6) | 22.9 (1.5) | 22.0 (1.1) |
| FAT [%] | 13.9 (3.6) | 11.4 (4.2) † | 6.8 (1.9) ** ## |
| TBW [kg] | 45.7 (1.1) | 46.4 (4.8) | 48.0 (3.3) |
| Hct R[%] | 46.1 (3.2) | 45.2 (2.3) | 46.3 (2.8) |
| Hct MAX [%] | 49.6 (3.5) | 48.8 (2.5) | 48.2 (2.4) |
| VO2max [ml·min-1·kg-1] | 50.3 (3.3) | 63.0 (11.0) ## | 70.3 (6.1) ***# |
| LApeak [mmol/l] | 9.9 (1.3) | 9.8 (1.1) | 9.9 (1.2) |
| Hct [%] | 46.1 (3.2) | 45.2 (2.3) | 46.3 (2.8) |
| Wmax [W] | 289 (17) | 357 (52) †† | 413 (19.2) ***## |
BMI = body mass index, FAT = percent of body fat, TBW = total body water, Hct = haematocrit, VO2max = maximal oxygen uptake,
LApeak = peak blood lactate concentration;,Wmax = power output at maximal intensity of exercise in control group (CG), athletes
with normal heart dimension (LVN ), and athletes with heart hypertrophy (LVH). *** p < 0.001 LVH vs. CG; # p < 0.05
LVH vs. LVN; ## p < 0.01 LVH vs. LVN; † p < 0.05 CG vs. LVN; †† p < 0.01 CG vs. LVN
- Group I (LVH Group) - competitive male road cyclists with clinically diagnosed left ventricular muscle hypertrophy (LVH Group),
- Group II (LVN Group) - competitive male road cyclists with a normal left ventricular muscle mass, i.e., left ventricular muscle indices (LVMI) lower than 134 g·m-2, left ventricular end diastolic posterior wall (LVPWT) < 13 mm and left ventricular end-diastolic internal diameter (LVEDd) < 55 mm (Levy et al., 1997).
All cyclists had been training for more than five years on the same cycling team. The values of relative intensity and volume of monthly road training were 1652.5 ± 109.1 and 1589.4 ± 201.9 km in Group I and II (p > 0.05), respectively. All athletes underwent medical evaluations at the same time of the pre-season training process, which included clinical history and physical examination. Echocardiography and the incremental cycling exercise test were performed at the beginning of the competitive season. Fourteen healthy but untrained men, students of the Physical Education Faculty age-matched to the study subjects, served as the control group (CG). Both the cyclists and controls were non-smokers, and none had taken any medication or anabolic steroid drugs.
The experimental procedures and possible risks were explained to all participants verbally and in writing, and the participants then gave informed written consent. The experiment was approved by the Ethics Committee of the Academy of Physical Education in Katowice and conforms to the standards set by the Declaration of Helsinki.
Study design
For three days before experiment, the subjects were on a standardized normocaloric (37kcal·kg-1·day-1) diet with 50-60% carbohydrate, 15-20% protein, and 20-30% fat. They were also obliged to abstain from strenuous exercise. No caffeine, tea, or alcohol was permitted during the 48 hours before the experiment. On the day of exercise testing, the subjects reported to the Laboratory after an overnight fast. Blood samples were taken in the morning (between 8.00 and 9.00 am) to avoid the effects of diurnal differences in hormone concentrations, from a peripheral catheter inserted into the ancubital vein. All subjects performed a graded cardiopulmonary exercise test on cycle ergometer (Ex) using Monark ergometer (Sweden). The exercise started with unloaded cycling for 5 min, and then intensity was increased by 40 W every 3 min up to maximal exercise intensity and 60-70 rpms were maintained. The Borg scale >18 was used as a criterion for maximal exercise, and/or physical exhaustion (Fletcher et al., 2001). Maximal heart rate (HRmax = 220-age) was also considered. Maximal lactate concentration (LApeak) was used for evaluation of the maximal oxygen consumption peak and relative work effort. All subjects performed incremental maximal intensity cycle exercise (over the anaerobic threshold AT), which was recognized to stimulate a higher increase in blood concentrations of IGF-I and IGFBP-3 than did low intensity exercise (below AT) (Kraemer, 2000). Pulmonary ventilation (VE), oxygen uptake (VO2), and carbon dioxide output (CO2) were measured continuously from the 6th min prior to exercise and throughout each stage of the exercise load using the Oxycon Apparatus (Jaeger, Germany). Heart rate (HR) was continuously recorded using the PE-3000 Sport-Tester (Polar Inc. Finland), and systolic and diastolic blood pressures were measured with a sphygmomanometer. Pulse pressure was calculated as systolic pressure minus diastolic pressure (PP = SBP-DBP).
After the 3 days of diet in all investigated subjects bioelectric impedance analysis under resting conditions was used to measure percent body fat and total body water. The values (mean ± SD) of age, height, body mass and body mass index content of the participants are presented in Table 1.
Procedure and echocardiography measurements
M-mode and two-dimensional Doppler-echocardiography was performed in all subjects using a Hewlett-Packard Image Point HX ultrasound system with standard imaging transducers. All analyses were made by the same investigator, using the trackball on the monitor. The intra-observer coefficients of variation were 2.5 % for measurements of LV diameters, and 3.6 % for measurements of LVEF. Left ventricular (LV) systolic function was determined by measurements of left ventricular ejection fraction (LVEF) and stroke volume (SV), and LV diastolic function was evaluated by Doppler echocardiography based on the ratio between the maximal flow velocities during the early diastolic rapid filling phase and the late diastolic atrial contraction (E/A). LV muscle mass (LVM) was derived according to Devereux et al., 1998: LVM = 1.04 [(LVEDd + IVSDd + LVPWd)3-(LVEDd)3], where LVEDd is left ventricular end-diastolic internal diameter, IVSDd is intraventricular septum thickness during diastole, and LVPWT is left ventricular posterior wall thickness. The left ventricular mass index (LVMI) was calculated with correction for body surface area. Left ventricular hypertrophy was identified when LVMI was equal to or greater than 134 g·m-2 (Levy et al., 1997).
Hormonal assays
Venous blood samples were collected at rest (approximately 15 min pre-exercise) for the assessment of serum insulin-like growth factor (IGF-I), insulin-like growth factor binding protein-3 (IGFBP-3), growth hormone (GH), testosterone (T), cortisol (C), and insulin (I) concentrations. The sampling was repeated immediately after cessation of exercise. Additionally, 0.1 mL of blood was taken from the finger tip at the end of each work load for the assessment of hematocrit and blood lactate concentration. Serum somatomedin C/IGF-I and IGFBP-3 were determined in duplicate by using a DSL ACTIVE IGF-I and IGFBP-3 immunoradiometric assay (IRMA) kit (Diagnostic System Laboratories, Webster, Texas). This is a 2-site immunoradiometric assay in which the analyte to be measured is “sandwiched” between the two antibodies. The first antibody is immobilized on the inside wall of the tubes. The other antibody is radiolabeled for detection. The analyte present in the subject samples, standards, and controls is bound by both of the antibodies to form a sandwich complex. Unbound materials are removed by decanting and washing the tubes. The detection limit is 0.01 ng/mL. The intra-assay coefficient of variation (CV) for IGF- I was determined by repetitive measurements of the blood sample and was calculated at 3.9% to 7.0%. The variance for IGFBP-3 ranges between 5.5 % and 6.5%. Serum GH was assayed with the DSL GH IRMA kit, while C, T, and I were measured by DSL RIA kits (Diagnostic System Laboratories, Webster, Texas). The procedure follows the basic principle of radioimmunoassay with competition between a radioactive and a nonradioactive antigen for a fixed number of antibody-binding sites. The separation of free and bound antigen is achieved using a double antibody system. Intra-assay CV for GH ranges from 9.1% to 10.1%. Both T and C showed variance between 5.1% and 10.0%, while I ranges from 8.3% to 10.0%. Blood lactate concentration (LA) was measured enzymatically using commercial kits (Boehringer, Manheim, Germany). The intra-assay CVs for the lactate assay was 3.2% and 8.9% for 6 and 10 assays, respectively.
Statistical analysis
Data are presented as mean and standard deviation (X ± SD). The data from three groups of subjects were analyzed by two- way ANOVA test with the use of Statistica 7.1 (StatSoft) software. When significant differences in F ratio were found, post-hoc Tukey’s test was used. Due to non-parametric data distribution, statistical significance of intra-group differences (LVH and LVN) was analyzed using Bonferroni test for independent variables. Between groups, correlation coefficients were determined with Pearson’s rank order test. Statistical significance was set at p < 0.05.
Results
Analysis of variance revealed a significant effect of endurance training on LVM p < 0.001(F = 18.3), LVMI p < 0.001 (F = 17.1), IVSDd p < 0.001 (F = 17.3) and LVPWT p < 0.01 (F = 8.7). As compared to athletes with normal heart dimensions (LVN group) and control subjects (CG), the LVMI was significantly higher in athletes with LVH (Fig.1). In subjects from the LVN group, LVMI was higher in relation to CG (p < 0.05) (Figure 1). Similarly, the intraventricular septum wall thickness (IVSDd) and LVPWT were also significantly greater in LVH athletes compared to LVN and CG groups. Left ventricular end-diastolic internal diameter (LVEDd) was lower in controls subjects compared to the athletes from the LVH group (p < 0.05). The mean intraventricular septum to left ventricular posterior wall thickness (IVS/PWT) ratio was higher in LVH athletes in relation to LVN (p < 0.05) (Table 2). In subjects from the LVH group stroke volume (SV) was elevated in relation to CG (p < 0.05) and LVN (p < 0.05) (Table 2). Athletes from the LVH group were found to have lower HRR than those from the LVN group (p < 0.05) and controls (p < 0.01) (Table 2).
Figure 1.
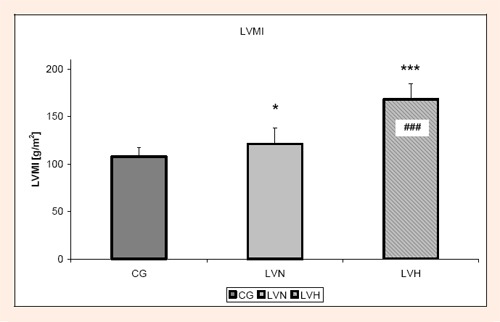
LVMI- Left Ventricular Mass Index in control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH) (mean ± SD). * p< 0.05 LVN vs. CG; *** p < 0.001 LVH vs. CG ### p < 0.001 LVH vs. LVN.
Table 2.
Echocardiographic variables in control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH). Data are means (± SD).
| VARIABLE | CG(n=14) | LVN ( n=15) | LVH (n=15) |
|---|---|---|---|
| LVM [g] | 206.4 (19.7) | 231.3 (29.6) | 325.9 (63.6) *** ### |
| LVEDd[mm] | 52.6 (3.2) | 53.1 (3.3) | 56.6 (3.0) * |
| IVSDd/LVPWT | 1.1 (.1) | 1.0 (.1) | 1.3 (.2) *# |
| LVEF % | 61.5 (8.4) | 63.4 (3.6) | 66.5 (5.3) ** |
| SV [mL] | 76.3 (10.3) | 76.6 (20.9) | 92.0 (19.5) * # |
| HRR [b/min] | 71 (6) | 66 (7) | 60 (7) **# |
| BPs [mmHg] | 183 (8) | 185 (14) | 197 (7) * |
| BPd [mmHg] | 64 (10) | 59 (7) | 57 (11) |
| PP [mmHg] | 119 (9) | 126 (13) | 139 (9) ***## |
LVM - left ventricular mass; LVEDd - end-diastolic internal diameter; IVSDd- intraventricular septum wall thickness; LVPWT - left ventricular posterior wall thickness; LVEF - left ventricular ejection fraction; SV - stroke volume; HRR - rest heart rate; BPs - systolic blood pressure; BPd - diastolic blood pressure, and PP-pulse pressure at maximal intensity of exercise
*, ** and *** indicate p < 0.05, 0.01 and 0.001, respectively, LVH vs. CG; #, ## and ### p < 0.05, 0.01 and 0.001, respectively, LVH vs. LVN.
ANOVA revealed a significant effect of basal level of IGF-I on left ventricular hypertrophy p<0.001 (F = 17.1), but no significant difference was seen in IGFBP-3 (p > 0.05).
Significant differences were found at maximal intensity of incremental exercise p < 0.01 (F = 7.6) and post-exercise p < 0.05 (F = 3.4) IGF-I concentrations in trained and sedentary subjects. The resting concentration of IGF-I was statistically higher in subjects from LVH compared to the values recorded in LVN (p < 0.05) and CG groups (p < 0.01). Compared to the resting values, the maximal incremental exercise test led to a significant increase in IGF-I level in CG (p < 0.01) and both groups of trained subjects (p < 0.05) (Figure 2). Resting serum levels of IGFBP-3 was lower in LVH group compared to CG and LVN groups (p < 0.05) (Figure 3). A significant resting and post-exercise increase in IGF-I/IGFBP-3 ratio was evidenced in LVH group in relation to CG (p < 0.01 vs. p < 0.05) and LVN (p < 0. 01 vs. p < 0.05) (Figure 4).
Figure 2.
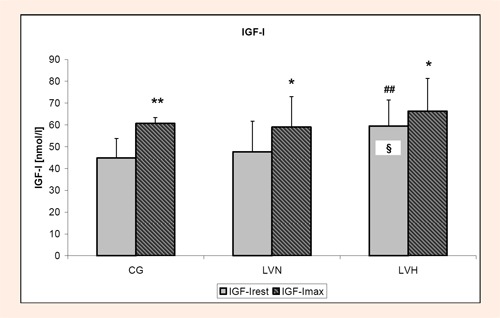
Insulin Growth Factor-I (IGF-I) concentration before (rest) and at maximal intensity of exercise (max) in control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH) (mean ± SD). * and ** indicate p < 0.05 and 0.01 respectively rest vs. max; ## indicates p < 0.01 LVH vs. CG; § indicates p < 0.05 LVH vs. LVN.
Figure 3.
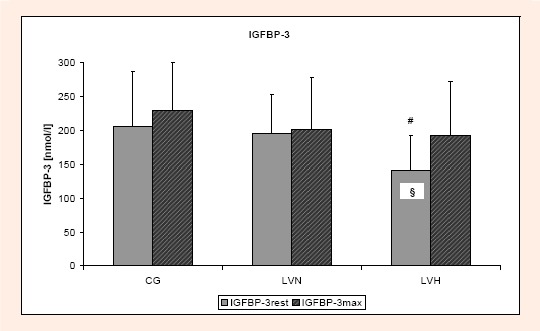
Insulin Growth Factor Binding Protein-3 (IGFBP-3) concentration before (rest) and at maximal intensity of exercise (max) in control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH) (mean ± SD). # p < 0.05 LVH vs. CG; § p < 0.05 LVH vs. LVN.
Figure 4.
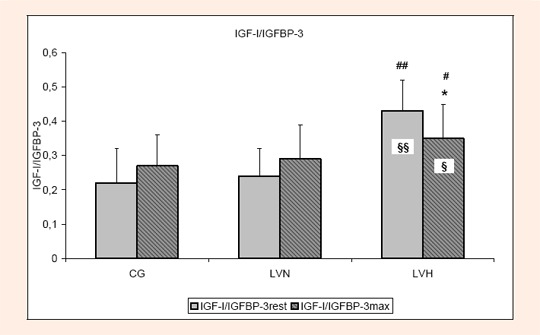
Insulin Growth Factor-I to Insulin Growth Factor Binding Protein-3 ratio (IGF-I/ IGFBP-3) before (rest) and at maximal intensity of exercise (max) in control group (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH) (mean ± SD). * p < 0.05 rest vs. max; # and ## indicates p < 0.05 and 0.01 respectively LVH vs. CG; § and §§ indicate p < 0.05 and 0.01 respectively LVH vs. LVN.
ANOVA revealed significant effects of training on resting (F = 10.1; p < 0.01) and post-exercise (F = 3.9; p < 0.05) testosterone (T) concentrations that were significantly lower in the LVH group compared to CG (p < 0.05) and LVN (Table 3). A negative correlation was found between resting T and IGF-I concentrations (r = -0.32; p < 0.05) in all subjects. No significant influence of training was observed on resting and post-exercise growth hormone (GH), or insulin (I) in any of the groups (Table 3).
Table 3.
Hormone concentration (GH - growth hormone, T- testosterone, C - cortisol, I - insulin) in control subjects (CG), athletes with normal heart dimension (LVN), and athletes with heart hypertrophy (LVH). Data are means (±SD).
| VARIABLE | CG (n = 14) | LVN ( n = 15) | LVH (n = 15) |
|---|---|---|---|
| GHR [ng·mL-1] | .3 (.2) | .6 (.5) | .5 (.4) |
| GH MAX [ng·mL-1] | 16.5 (7.4) | 15.7 (6.2) | 16.3 (6.1) |
| TR [nmol·L-1] | 14.5 (3.0) | 14.6 (5.6) | 11.1 (4.4) *# |
| T MAX [nmol·L-1] | 22.4 (7.2) | 17.1 (6.2) | 13.9 (5.4) * |
| CR [nmol·L-1] | 390.4 (119.2) | 413.2 (81.9) | 442.2 (111.6) |
| CMAX [nmol·L-1 | 513.6 (123.6) | 442.6 (188.1) | 583.5 (117.7) # |
| IR [μlU·mL-1] | 8.3 (4.3) | 8.0 (4.6) | 8.0 (3.2 ) |
| I MAX [μlU·mL-1] | 9.5 (4.9) | 13.7 (4.1) | 12.6 (6.3) |
Subscript R indicates resting values, subscript MAX indicates values reached at maximal exercise intensity.
* p < 0.05 LVH vs. CG;# p < 0.05 LVH vs. LVN.
Significant positive correlations were seen in the LVH group between the resting IGF-I concentration and LVM (r = 0.35; p < 0.05), and LVMI (r = 0.33; p < 0.05) (Figure 5). An exercise-induced increase in IGF-I concentration was found to be correlated with GH (r = 0.41; p<0.01) and post-exercise lactate (LA) (r = 36; p<0.05) concentration.
Figure 5.
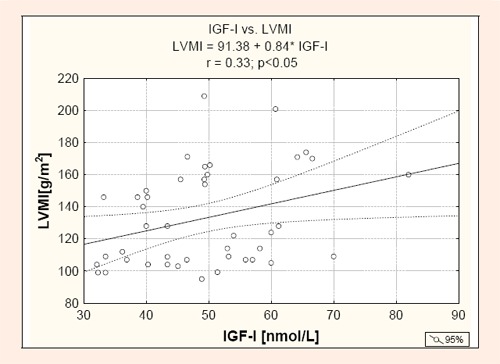
Relationship between resting Insulin-Like Growth Factor- I (IGF-I) concentration and left ventricular mass index (LVMI).
Moreover, a positive correlation between resting IGF-I and VO2max (r = 0.37; p < 0.05) (Figure 6) and a negative correlation between percent body fat and resting IGF-I (r = -0.48; p < 0.01) concentrations were found in all groups. No significant correlations between rest and post-exercise IGF-I concentrations and systolic, diastolic, and pulse blood pressure were observed (p > 0.05).
Figure 6.
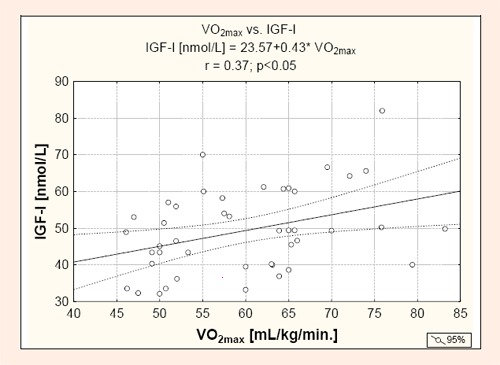
Relationship between maximal oxygen uptake (VO2max) and resting Insulin-Like Growth Factor- I (IGF-I) concentration.
Discussion
Physiological heart hypertrophy is a process of adaptation to an increased hemodynamic and/or pressure overload. The primary stimulus for cardiac hypertrophy is mechanical stress, which induces a growth response in the overloaded myocardium. The other mechanism of cardiac hypertrophy is associated with hormonal or adrenergic nervous system (Brink, et al., 1999; Hanson et al., 1993; Huang et al., 2003). It has also been documented that mechanical loading regulates intracellular signals of specific gene expression for cardiac hypertrophy without participation of humoral or neural factors (Donohue et al., 1994; Kim et al., 2008).
Our study revealed a higher exercise-induced increase in systolic blood pressure (SBP), and a tendency of diastolic blood pressure (DBP) to decrease in athletes with left ventricular hypertrophy compared to control subjects. These changes in blood pressure result in a concomitant widening of pulse pressure with a decrease in peripheral vascular resistance (Table 2). Kasikcioglu et al., 2005 observed that the peak pulse pressure during maximal exercise was closely associated with left ventricular mass index, and was predicted of LV hypertrophy. However, in our study we did not observe significant differences in systolic blood pressure response in athletes with and without cardiac hypertrophy. Thus, it cannot be excluded that, apart from hemodynamic and pressure overload, some endocrine factors may also be implicated in physiological heart hypertrophy. Also earlier experimental evidence acquired with the use of animals is in agreement with a possible role of somatomedins in stimulation of heart hypertrophy (Huang et al., 2003).
A high prevalence of left ventricular hypertrophy was documented in male athletes with a body surface area > 2.0 m2 who participated in endurance sports (Pelliccia et al., 1991; Sharma, 2003). Nishimura et al., 1980 found that left ventricular hypertrophy in cyclists was related to the type, duration, and intensity of training. Therefore, the training regimen applied to the athletes was characterized by the same relative intensity (calculated according to individual anaerobic threshold LAT) and volume of exercise (Groups I and II: 1589.4 ± 201.9 vs. 1652.5 ± 109.1 km monthly road training volume, respectively, p > 0.05). There was also no significant difference between different groups in age, body mass, and body mass index (BMI) (Table 1). Since the body mass control was a basic procedure applied by our subjects and they did not report significant changes one may suppose that they basic metabolic rate was the same. Therefore, our results might most likely reflect the training-induced effect of somatomedin and hormones on cardiac cells.
We found that athletes with LVH have significantly higher resting concentrations of circulating IGF-I than age- and training status-matched subjects with normal left ventricular dimensions. Moreover, IGF-I was significantly elevated after incremental exercise in LVH athletes in comparison to the resting values (Figure 2). The importance of this investigation is the fact that the ratio between IGF-I/IGFBP-3 was higher in LVH group compared to trained subjects without LVH (Figure 4). Since no difference in IGF-I level between LVN athletes and control subjects was detected, all the aforementioned results imply that both elevated resting level of IGF-I and increased serum IGF-I in response to repeated bouts of acute high- intensity exercise during endurance training process may act, at least partially, as a causative factor, leading to the development of physiological hypertrophy.
Athletic Heart Syndrome is associated with an increase in left ventricular mass and left ventricular wall thickness and is usually associated with a cavity dimension > 55 mm (Rich and Havens, 2004). Our results are in agreement with previous observations made in adult athletes having a left ventricular cavity > 55 mm induced by repeated volume-overloads during isotonic exercises. There are also reports that evidenced a lack of differences in left ventricular cavity dimension in endurance-trained athletes; however, in 2% of these athletes the LVPWT exceeded the upper physiological limits (Levy et al., 1997). In some cases, LVPWT was similar to that seen in patients with hypertrophic cardiomyopathy and impaired left ventricular diastolic function. It should be emphasized that diastolic function in athletes remained unchanged or even improved compared to sedentary subjects (Nishimura et al., 1980; Pluim et al., 1999; Sharma, 2003). The fact that endurance athletes showed a different level of cardiac hypertrophy prompted us to compare some hormonal and somatomedin responses to the maximal graded exercise test in athletes with left ventricular hypertrophy and normal heart dimensions. All subjects performed incremental maximal intensity cycle exercise, which was recognized to stimulate a higher increase in blood concentrations of IGF-I and IGFBP-3 than did low intensity exercise (Kraemer, 2000). However, it should be stressed that, while several authors observed an exercise intensity-related increase in serum IGF-I (Kraemer, 2000; Scheinowitz et al., 2003), some others have reported opposite effects (Eliakim et al., 1998; Rosendal et al., 2002). Findings from several studies investigating the response of IGF-I to chronic training indicate that both its intensity and duration determine the resultant IGF-I levels (Koziris et al., 1999; Manetta et al., 2002; Schwarz et al., 1996). In our study, cyclists have been training for more than five years in the same cycling team, and all of them were subjected to the same training regimen with the same relative intensity and volume.
The metabolic effects of IGF-I are mediated by multiple insulin-like binding proteins (IGFBPs), which modifying IGF-I bioavailability. IGFBP-1 and IGFBP-3 are the most important of the 6 circulating IGFBPs (Fischer et al., 2004). Although, IGFBP-1 play a role in glucoregulatory process, the level of circulating IGF-I are mediated predominantly by IGFBP-3, which may be responsible for better delivery of IGF-I to the cells in both trained and untrained subjects (Delafontaine et al., 2004; Kraemer, 2000; Rosendal et al., 2002). Application of most training protocols has resulted in stimulation of IGFBP-3 synthesis (Nguyen et al., 1998). However, there are also reports revealing a decrease in serum IGFBP-3 level following 4 weeks of training, which could be caused by enhanced IGFBP-3 proteolysis in response to intensive endurance training (Schwarz et al., 1996). The authors speculated that during acute and repeated exercise, the proteolysis of IGFBP-3 might increase the bioavailability of free IGF-I. It is worth pointing out that the elevation of resting concentration of IGF-I observed in our study was associated with a markedly increased IGF-I to IGFBP-3 ratio in LVH athletes (Figure 4).
Compared to sedentary subjects, the professional male athletes were found to have a significantly higher artery- coronary sinus concentration gradient of IGF-I, which implies greater IGF-I cardiac formations (Neri Serneri et al., 2001). IGF-I activates phosphatidyl inositol (PI), 3-kinase/Akt, and mitogen-activated protein kinase (MAPK) signaling pathways, which may induce the growth and differentiation of cardiomyocytes (Catalucci, et al. 2008; McMullen et al., 2004). Cardiac hypertrophy can be stimulated by local IGF-I synthesis (Kupfer et al., 1992; Kobayashi et al., 2004) and by an exercise-induced increase in the circulating IGF-I level (Neri Serneri et al., 2001). Our data support previous findings suggesting that circulating IGF-I may be an important cardiac growth factor (Bleumink et al., 2005; Ren et al., 1999). Although we were only able to measure serum IGF-I and IGFBP-3 concentrations, our results in human subjects support the observations derived from experiments on rat hearts, which have evidenced that exogenous IGF-I induces hypertrophic growth in rat ventricular cardiomyocytes by increasing their size, total protein synthesis, and transcription of the muscle-specific gene (Bleumink et al., 2005; Kobayashi et al., 2004; Kupfer et al., 1992).
Studies on IGF-I production and IGF-I mRNA expression in the myocardial tissue confirmed a key role of this protein in the activation of right and left ventricle growth during experimental volume overload (Modesti et al., 2004). The hypothesis of the role of IGF-I as the main paracrine/autocrine factor regulating myocyte hypertrophy in trained athletes is further supported by data on aorta-coronary sinus concentration gradients of endothelin (ET)-1 and angiotensin (Ang) II, which failed to reveal differences in these gradients between endurance athletes and the sedentary control (Neri Serneri et al., 2001). IGF-I has been found to promote cardiac growth independently on altered hemodynamics, ventricular loading conditions, and other changes in the neurohormonal pathway (Bleumink et al., 2005; Ren et al., 1999).
Testosterone and growth hormone are known to be involved in pressure-overload induced cardiac growth. Several studies have demonstrated that cardiomyocytes express androgen receptors that, when activated, modulate gene expression in the cells (Culig et al., 1995; Marsh et al., 1998). An increase in anabolic-androgenic steroid concentrations in the blood due to exogenous administration and endogenous secretion may stimulate myocardial and ventricular hypertrophy, both in training-related and pathologic conditions (Mettauer et al., 2001; Marsh et al., 1998). It worth to point out, that anabolic steroids may also decrease the physiological effect of endogenous hormones because of negative feedback. Our study revealed lower resting and post- exercise serum T concentrations in LVH compared to LVN and CG groups, suggesting that testosterone was not involved in cardiac hypertrophy in our experienced athletes with LVH. The negative correlation observed between resting T and IGF-I concentrations suggests that the hypertrophic effect observed in our athletes was solely stimulated by IGF-I. This conclusion must be treated with caution because previous data have shown that endurance training might result in up-regulation of myocardial androgen receptors, thereby increasing the effectiveness of testosterone action (Culig et al., 1995; Marsh et al., 1998).
In the present study, significantly higher resting IGF-I secretion and higher post- exercise level of IGF-I/IGFBP-3 ratio was induced by participation in longitudinal training process in experienced athletes compared to sedentary subjects (CG) and athletes without left ventricular hypertrophy (LVN). In the light of such evidence, IGF-I might be implicated as one of the most important regulatory factors involved in the development of myocardial hypertrophy in response to repeated bouts of exercise.
Conclusion
The data from this research indicate that resting circulating levels of IGF-I were higher in athletes with physiological left ventricular hypertrophy (LVH) compared to athletes with normal heart dimension and sedentary subjects. Comparable GH and C post-exercise elevations in both athlete groups and lower T concentrations in athletes with left ventricular hypertrophy exclude the essential impact of these hormones on the left ventricular dimension. We suggest that the greater exercise-related IGF-I increase in athletes with left ventricular hypertrophy might be, at least partially, a consequence of circulating free IGF-I elevation in response to IGFBP-3 proteolysis after intense endurance training.
Acknowledgments
This study was supported by the statutory activity of the Department of Physiology, Academy of Physical Education in Katowice, Poland.
We acknowledge research support from Silesian University School of Medicine in Katowice, Poland.
Biographies
Aleksandra Żebrowska
Employment
Department of Physiology, Academy of Physical Education, Katowice, Poland.
Degree
Ph. D
Research interests
Exercise physiology, Physiotherapy.
E-mail: olazebrowska@yahoo.com
Zbigniew Gąsior
Employment
Department of Cardiology, Silesian University School of Medicine, Katowice, Poland.
Degree
Prof.
Research interests
Cardiology, Echocardiography.
E-mail: zgasior@sum.edu.pl
Józef Langfort
Employment
Department of Physiology, Academy of Physical Education, Katowice, Poland
Department of Experimental Pharmacology, Polish Academy of Science, Warsaw, Poland.
Degree
Prof.
Research interests
Exercise physiology, Neurotransmiters, Antyoxidant.
E-mail: langfort@cmdik.pan.pl
References
- 1.Bisi G., Podio V., Valetto M.R., Bertuccio G., Rio G., Boghen M.F., Berti F., Muller E.E., Ghigo E. (1999) Radionuclide angiocardiographic evaluation of the cardiovascular effects of recombinant human IGF-I in normal adults. European Journal of Endocrinology 140, 322-327 [DOI] [PubMed] [Google Scholar]
- 2.Brink M., Chrast J., Mitch W.E., Delafontaine P. (1999) Angiotensin II stimulates gene expression of cardiac insulin-like growth factor 1 and its receptor through effects on blood pressure and food intake. Hypertension 334, 1053-1059 [DOI] [PubMed] [Google Scholar]
- 3.Bleumink G.S., Schut A.F., Sturkenboom MC.J.M., Janssen J.A.M.J.L., Witteman J.C.M., van Duijn C.M., Hofman A., Stricker B.H.Ch. (2005) A promoter polymorphism of the insulin-like growth factor-I gene is associated with left ventricular hypertrophy. Heart 91, 239-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catalucci D., Latronico M.V., Ellingsen O., Condorelli G. (2008) Physiological myocardial hypertrophy: how and why? Frontiers in Bioscience 1(13), 312-324 [DOI] [PubMed] [Google Scholar]
- 5.Culig Z., Hobisch A., Cronauer M., Hittmair A., Radmayer C., Bartsch G., Klocker H. (1995) Activation of androgen receptor by polypeptide growth factors and cellular regulators. World Journal of Urology, 13, 285-289 [DOI] [PubMed] [Google Scholar]
- 6.Decker M.L., Janes D.M., Barclay M.M., Harger L., Decker R.S. (1997) Regulation of adult cardiocyte growth: Effects of active and passive mechanical loading. American. Journal of Physiology 272, H2902-H2918 [DOI] [PubMed] [Google Scholar]
- 7.Delafontaine P., Yao-Hua S., Yangxin L. (2004) Expression, Regulation, and function of IGF-1, IGF-1R, and IGF-1 binding proteins in blood vessels. Arteriosclerosis Thrombosis and Vascular Biology 24, 435-444 [DOI] [PubMed] [Google Scholar]
- 8.Devereux R.B., Alonso R., Lutas R., Gottlieb G., Campo E., Sachs I., Reiche K.N. (1998) Echocardiogrphic assessment of left ventricular hypertrophy: comparison to necropsy finding. American Journal of Cardiology 157, 450-458 [DOI] [PubMed] [Google Scholar]
- 9.Diez J. (1999) Insulin growth factor I in essential hypertension. Kidney International 55, 744-759 [DOI] [PubMed] [Google Scholar]
- 10.Donohue T.J., Dworkin L.D., Lango M.N., Fliegner K., Lango R.P., Benstein J.A., Slater W.R., Catanese V.M. (1994) Induction of myocardial insulin-like growth factor-I gene expression in left ventricular hypertrophy. CCirculation 889, 799-809 [DOI] [PubMed] [Google Scholar]
- 11.Eliakim A., Brasel J.A., Mohan S., Wong W.L., Cooper D.M. (1998) Increased physical activity and the growth hormone-IGF-I axis in adolescent males. American Journal of Physiology Regulatory, Integrative and Comparative Physiology 275, R308-R314 [DOI] [PubMed] [Google Scholar]
- 12.Fischer F., Schulte H., Mohan S., Tataru M., Köhler E., Assmann G., Eckardstein A. (2004) Association of insulin-like growth factors, insulin growth factor binding proteins and acid-labile subunit with coronary heart disease. Clinical Endocrinology 61, 595-602 [DOI] [PubMed] [Google Scholar]
- 13.Fletcher G.F. Balady G.J., Amsterdam E.A. Chaitman B., Eckel R. Fleg J., Froelicher V.F. Leon A. Piña I.L., Rodney R. Simons-Morton D.A., Williams M.A. Bazzarre T. (2001) Exercise standards for testing and training. A statement for healthcare professionals from the America Heart Association. Circulation 104, 1694-1740 [DOI] [PubMed] [Google Scholar]
- 14.Hanson M.C., Fath K.A., Alexander R.W., Delafontaine P. (1993) Induction of cardiac insulin-like growth factor I gene expression in pressure overload hypertrophy. American Journal of Medicine and Science 306(2), 69-74 [DOI] [PubMed] [Google Scholar]
- 15.Horio T., Maki T., Kishimoto I., Okumura H., Yoshihara F., Suga S., Takeo S., Kawano Y., Kangawa K. (2005) Production and autocrine/paracrine effects of endogenous insulin-like growth factor-1 in rat cardiac fibroblasts. Regulatory Peptides 124, 65-72 [DOI] [PubMed] [Google Scholar]
- 16.Huang Ch., Buchanan D.L., Gordon R.L., Scherman M.J., Razzaq J., White K., Buetow D.E. (2003) Increased insulin-like growth factor-I gene expression precedes left ventricular cardiomyocytes hypertrophy in rapidly-hypertrophying rat model system. Cell Biochemistry and Function 221, 355-361 [DOI] [PubMed] [Google Scholar]
- 17.Kasikcioglu E., Oflaz H., Akhan H., Kayserilioglu A., Umman B. (2005) Peak pulse pressure during exercise and left ventricular hypertrophy in athletes. AAnatolian Journal of Cardiology, 5, 64-65 [PubMed] [Google Scholar]
- 18.Kim J., Wende A.R., Sena S., Theobald H.A., Soto J., Sloan C., Wayment B.E., Litwin S.E., Holzenberger M., LeRoith D., Abel E.D. (2008) Insulin-like growth factor I receptor signaling is required for exercise-induced cardiac hypertrophy. Molecular Endocrinology 22(11), 2531-2543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kobayashi S., Kawashma S., Sakoda T., Ueyama T., Hirase T., Kawai M., Toh R., Iwai K., Yokoyama M. (2004) Glycogen Synthase Kinase-3 is involved in the process of myocardial hypertrophy stimulated by insulin-like growth factor-1. Circulation Journal 68, 247-253 [DOI] [PubMed] [Google Scholar]
- 20.Koziris L.P., Hickson R.C., Chatterton R.T., Groseth R.T., Christie I.M., Goldflies D.G., Unterman T.G. (1999) Serum levels of total and free IGF-I and IGFBP-3 are increased and maintained in long-term training. Journal Applied Physiology 86, 1436-1442 [DOI] [PubMed] [Google Scholar]
- 21.Kraemer W.J. (2000) Effects of exercise and alkalosis on serum insulin-like growth factor I and IGF-binding protein-3. Canadian Journal of Applied Physiology 25, 127-138 [DOI] [PubMed] [Google Scholar]
- 22.Kupfer I.M., Rubin S.A. (1992) Differential regulation of insulin-like growth factor I by growth hormone and thyroid hormone in the heart of juvenile hypophysectomized rats. Journal of Molecular and Cellular Cardiology 224, 631-639 [DOI] [PubMed] [Google Scholar]
- 23.Levy D., Savage D.D., Garrisonn R.J., Anderson K.M., Kannell W.B., Casterlli W.P. (1997) Echocardiographic criteria for left ventricular hypertrophy: the Framingham heart study. American Journal of Cardiology 59, 656-960 [DOI] [PubMed] [Google Scholar]
- 24.Manetta J., Brun J.F., Fedou C., Maïmoun L., Prefaut C., Mercier J. (2003) Serum levels of insulin-like growth factor-I (IGF-I), and IGF-binding proteins-1 and-3 in middle-aged and young athletes versus sedentary men: relationship with glucose disposal. Metabolism 52, 821-826 [DOI] [PubMed] [Google Scholar]
- 25.Manetta J., Brun J.F., Maïmoun L., Callis A., Prefaut C., Mercier J. (2002) Effect of training on the GH/IGF-I axis during exercise in middle-aged men: relationship to glucose homeostasis. American Journal of Physiology and Endocrinology 283, 929-936 [DOI] [PubMed] [Google Scholar]
- 26.Marsh J.D., Lehmann M.H., Ritchie R.H., Gwathmey J.K., Green G.E., Schiebinger R.J. (1998) Androgen receptors mediated hypertrophy in cardiac myocytes. Circulation, 98, 256-261 [DOI] [PubMed] [Google Scholar]
- 27.McMullen J.R., Shioi T., Huang W.Y., Zhang L., Tarnavski O., Bisping E., Schinke M., Kong S., Sherwood MC., Brown J., Rigi L., Kang P.M., Izumo S. (2004) The insulin like growth factor 1 receptor induces physiological heart growth via the phosphoinositide 3-kinase (p110alpha) pathway. Journal of Biological Chemistry 279, 4782-4793 [DOI] [PubMed] [Google Scholar]
- 28.Mettauer B., Geny B., Landsdorf-Wolf E., Charloux A., Zhao Q.M., Heitz-Naegelen B., Epailly E., Lampert E., Levy F. (2001) Exercise training with a heart device: a hemodynamic, metabolic, and hormonal study. Medicine and Science Sports and Exercise 33, 2-9 [DOI] [PubMed] [Google Scholar]
- 29.Modesti P.A., Vanni S., Bertolozzi I., Cecioni I., Lumachi C., Perna A.M., Boddi M., Gensini G.F. (2004) Different growth factor in the right and left ventricles in experimental volume overload. Hypertension 43, 110-108 [DOI] [PubMed] [Google Scholar]
- 30.Neri Serneri G., Boddi M., Modesti P., Cecioni I. Coppo M., Padeletti L. Michelucci A., Colella A. Galanti G. (2001) Increased cardiac sympathetic activity and insulin-like growth factor-I formation are associated with physiological hypertrophy in athletes. Circulation Research 89, 977-982 [DOI] [PubMed] [Google Scholar]
- 31.Nguyen U.N., Mougin F., Simon-Rigaud M.L., Rouillon I.D., Marguel P., Regnard J. (1998) Influence of exercise duration on serum insulin-like growth factor and its binding proteins in athletes. European Journal of Applied Physiology and Occupational Physiology 78, 533-537 [DOI] [PubMed] [Google Scholar]
- 32.Nishimura T., Yamada Y., Kawai C. (1980) Echocardiographic evaluation of long-term effects of exercise on left ventricular hypertrophy and function in professional bicyclists. Circulation 10, 540-547 [DOI] [PubMed] [Google Scholar]
- 33.Pelliccia A., Maron B.J., Spataro A., Proschan M., Spirito P. (1991) The upper limits of physiological hypertrophy in highly trained athletes. The New England Journal of Medicine 324, 295-301 [DOI] [PubMed] [Google Scholar]
- 34.Pluim B.M., Zwinderman A.H., van der Laarse A., van der Wall E.E. (1999) The athlete’s heart: a meta-analysis of cardiac structure and function. Circulation 100, 336-344 [DOI] [PubMed] [Google Scholar]
- 35.Ren J., Samson W.K., Sowers J.R. (1999) Insulin-like growth factor I as a cardiac hormone: physiological and pathophysiological implications in heart disease. Journal of Molecular and Cellular Cardiology 31, 2049-2061 [DOI] [PubMed] [Google Scholar]
- 36.Rich B.S., Havens S.A. (2004) The athletic heart syndrome. Current Sports Medicine Reports 33, 84-88 [DOI] [PubMed] [Google Scholar]
- 37.Rosendal L., Langberg H., Flyvbjerg A., Frystyk J., Ørskov H., Kjær M. (2002) Physical capacity influences the response of insulin-like growth factor and its binding proteins to training. Journal of Applied Physiology 93, 1669-1675 [DOI] [PubMed] [Google Scholar]
- 38.Scheinowitz M., Kessler-Icekson G., Freimann S., Zimmermann R., Schaper W., Golomb E., Savion N., Eldar M. (2003) Short-and long-term swimming exercise training increase myocardial insulin-like growth factor-I gene expression. Growth Hormone and IGF Research 13, 19-25 [DOI] [PubMed] [Google Scholar]
- 39.Schwarz A.J., Brasel J., Hintz R.L., Mohan S., Cooper D.M. (1996) Acute effect of brief low-and high-intensity exercise on circulating insulin-like growth factor (IGF) I, II and IGH-binding protein-3 and its proteolysis in young healthy men. Journal of Clinical Endocrinology and Metabolism 881, 3492-3497 [DOI] [PubMed] [Google Scholar]
- 40.Sharma S. (2003) Athlete’s heart-effect of age, sex, ethnicity and sporting discipline. Experimental Physiology 88, 665-669 [DOI] [PubMed] [Google Scholar]
- 41.Strøm C.C., Aplin M., Ploug T., Christofferson T.E., Langfort J., Viese M., Galbo H., Haunso S., Sheikh S.P. (2005) Expression profiling reveals differences in metabolic gene expression between exercise-induced cardiac effects and maladaptive cardiac hypertrophy. FEBS Journal 272, 2684-2695 [DOI] [PubMed] [Google Scholar]
- 42.Zanconato S., Moromisato D.Y., Moromisato M.Y., Woods J., Brasel J.A., LeRoith D., Roberts C.T., Cooper D.M. (1994) Effect of training and growth hormone suppression on insulin-like growth factor-I mRNA in young rats. Journal of Applied Physiology 76, 2204-2209 [DOI] [PubMed] [Google Scholar]


