Abstract
The purpose of this study was to determine if six weeks of folic acid supplementation would improve brachial artery endothelial-dependent flow-mediated dilation in eumenorrheic female runners with previously normal serum folate levels. This was a prospective, double-blinded, randomized pilot study with convenience sampling. Sixteen eumenorrheic subjects who were not taking birth control pills and who ran at least 20 miles/week were randomly assigned to 10 mg/day of folic acid supplementation or placebo for at least 6 weeks. Serum folate levels and brachial artery measurements were made during the early follicular phase of the menstrual cycle, in a sedentary state, following an 8 hour fast; a standard ultrasound technique was used. The brachial artery vasodilator response to reactive hyperemia was similar between the folic acid (6.6% ± 0.8%, mean ± SE) and placebo groups (6.5% ± 0.7%) at baseline. After six weeks, there was a significantly higher change in flow-mediated dilation for the folic acid group (3.5% ± 0.6%) compared to the placebo group (0.1% ± 0.2%) (p = 0.01). Serum folate levels also increased significantly in the folic acid group following six weeks of folic acid supplementation. This study demonstrates that brachial artery flow-mediated dilation improves significantly in eumenorrheic female runners with previously normal serum folate levels after 6 weeks of supplementation with folic acid.
Key points.
Folic acid improves FMD in eumenorrheic runners.
Folic acid improves FMD in women runners.
Key words: Premenopause, regular menstruation, endothelial function, folate, flow-mediated vasodilation
Introduction
Cardiovascular disease is the number one cause of death in women, with risk of the disease increasing significantly after menopause when estrogen levels drop. Impaired endothelial function has gained acceptance as the sentinel atherogenic event (Celermajer, 1997; Ganz et al., 2003; Ross, 1999) in cardiovascular disease; it is seen as early as seven days after ovariectomy in premenopausal women (Ohmichi et al., 2003) and three months after menopause (Lieberman et al., 1994). Flow-mediated dilation (FMD) can be used as a tangible marker in order to quantify endothelial cell function and thus assess cardiovascular risk. Researchers (Rickenlund et al., 2005a; Rickenlund et al., 2005b) have recently demonstrated that young female runners with athletic-associated amenorrhea show reduced endothelial-dependent FMD of the brachial artery compared to eumenorrheic runners. The magnitude of endothelial dysfunction in these young women (age 21.9 ± 1.2 yrs, mean ± SE) was alarming: with an FMD of 1.10% ± 0.96% which is similar to significantly older women (age 60.0 ± 2. 0 yrs) with established cardiovascular disease (Celermajer et al., 1992). Additionally, researchers discovered that the eumenorrheic and oligomenorrheic runners in this study had endothelial function at the low end of normal despite no apparent risk factors for cardiovascular disease (Hoch et al., 2003). The clinical consequences of this observation in the eumenorrheic and oligomenorrheic groups are unclear. However, it deserves further evaluation in regards to etiology, treatment, and future consequences since these findings suggest the potential for an increased cardiovascular risk. Previous studies have shown that estrogen will increase FMD. However, in light of the recent findings from the Women’s Health Initiative (Rossouw et al., 2002) which revealed an added cardiovascular risk with estrogen treatment, alternative therapy must be considered.
Folic acid has recently become popular because of its potential benefits with regards to cardiovascular parameters such as endothelial function, arterial stiffness, blood pressure and thrombotic activity (Chambers et al., 2000; Deol et al., 2004; Mangoni et al., 2001; 2002; 2003; 2005; Schutte et al., 2004; Undas et al., 1999; van Dijk et al., 2001). Several mechanisms exist to explain the effectiveness of folate therapy. Folates are alleged to participate in the endogenous regeneration of tetrahydrobiopterin (Wever et al., 1997), an essential cofactor for endothelial nitric oxide synthase (eNOS) production of nitric oxide; such a role may therefore result in increased NO production after supplementation. Additionally, the well-known homocysteine-lowering effect of folic acid could contribute to improvements in endothelial function (Pancharuniti et al., 1994; van den et al., 1995); however, this hypothesis has recently been challenged as some studies have shown that folic acid improves endothelial function without producing significant changes in homocysteine concentration (Mangoni et al., 2002; 2005; Verhaar et al., 1998). Finally, recent in vitro data suggest that folic acid may have a direct antioxidant effect in the vasculature, thus increasing NO bioavailability and improving FMD (Bonetti et al., 2003).
Previous studies indicate that there is no significant difference in endothelium-independent vasodilation between amenorrheic, oligomenorrheic and eumenorrheic women (Hoch et al., 2003); thus, we focused solely on the differences in endothelial-dependent FMD. The purpose of this study was to determine if 6 weeks of high-dose folic acid supplementation (10 mg·day-1) would improve brachial artery FMD in eumenorrheic runners with normal serum folate levels and borderline endothelial function.
Methods
Subjects and experimental design
Subjects were recruited from track and cross country teams at a local university. Inclusion criteria were as follows: eumenorrheic females between the ages of 18-30, healthy with no medical conditions, and running at least 20 miles/week for the last 12 months. Eumenorrheic was defined as menstrual bleeding every 28 - 32 days for at least twelve months; ovulation during regular cycles was not determined. Subjects were excluded from the study if they were pregnant, hypertensive (systolic > 160 mmHg and diastolic > 90 mmHg), on birth control pills or hormone replacement therapy, smokers, oligomenorrheic or amenorrheic. Subjects were also excluded if they had a known pituitary tumor, thyroid disorder, chromosomal abnormality, hypercoagulable state, or history of cardiovascular disease. Subjects were not excluded on the basis of race; however all were Caucasian ethnicity.
Sixteen women gave written informed consent in accordance with our Institutional Review Board. Three subjects dropped out from the placebo group prior to initial testing due to time constraints. All subjects filled out questionnaires about their health and menstrual status and reported miles run per week. No subjects had a family history of cardiovascular disease or reported taking multivitamins. Subjects were randomly assigned with a blocking technique to receive either 10 mg/day of folic acid (n = 8) or placebo (n = 5) in blinded fashion. We used 10mg of folic acid because others have used this dosage and found it to be safe and improve flow-mediated dilation (Moens et al., 2007; Title et al., 2006; US Food and Drug Administration, 2008; Wilmink et al., 2000; Woo et al., 1999). They were instructed to take the medication for at least six weeks. All subjects were studied in the morning after an overnight fast. They were also studied during the follicular phase of their menstrual cycle (days 4-8) since it is known that FMD varies during the menstrual cycle in relation to both estrogen and progesterone levels (Hashimoto et al., 1995; Mather et al., 2000; Williams et al., 2001). For standardization purposes, subjects were instructed to take their supplements in the morning with food.
Serum folic acid levels
Fasting whole serum folate levels were measured by the Bayer ADVIA Centaur before and after supplementation with folic acid or placebo. This assay is a competitive immunoassay using direct chemiluminescent technology. The inter-assay coefficient of variation was 5-7%, the intra-assay coefficient of variation was 4-8%, and the lower limit of sensitivity was 0.35 ng·mL-1.
Endothelial function
Thirteen subjects underwent brachial artery endothelial function testing at baseline and after at least six weeks of treatment with 10 mg/day folic acid or placebo, using FMD as a quantifiable measure of endothelial-dependent vascular function. All subjects were tested in the morning after an eight hour fast, and during the early follicular phase of their menstrual cycle (days 4-8), since it is known that FMD varies during the menstrual cycle in relation to both estrogen and progesterone levels (Hashimoto et al., 1995; Mather et al., 2000; Williams et al., 2001). Brachial artery FMD was measured using the same ultrasound technique as previous studies in this lab and those done by Celermajer (Celermajer et al., 1992; Celermajer, 1997); this brachial artery technique was found to have a reproducibility coefficient of variation of 1.4% and a repeatability coefficient of variation of 2.3%. Subjects were instrumented for continuous recording of ECG (lead II), heart rate, capillary oxygen saturation, and intermittent blood pressure using an automated cuff. FMD was measured as follows: in the supine position with the non-dominant arm in a comfortable position, a sphygmomanometric cuff was placed around the forearm distal to the antecubital fossa (Corretti et al., 2002; Doshi et al., 2001b). An ultrasound machine, using a 10 MHz linear array small footprint probe (intraoperative), was secured over the brachial artery. Images of the brachial artery were made along the longitudinal axis after identifying a >5 cm segment where the near and far endothelial borders were clearly delineated. The ultrasound probe can be used to measure both vessel diameter and blood flow velocity using the pulsed Doppler mode. The ECG recorded simultaneously with the ultrasound image in order to gate events in the cardiac cycle. At least 15 seconds of stable diameter recordings were assessed at each point where data was acquired. All brachial artery images were recorded on a super VHS videotape for subsequent analysis. Image analysis was performed on a dedicated Pentium III computer using a Matrox millennium card for A/D conversion of analog images at high resolution. Diameter was measured from digitized images using an automated edge detection program (Brachial Analyzer and Brachial Imager) from Medical Imaging Systems (Iowa City, Iowa). Ten images were obtained each second for 10 seconds and the average minimum diameter for each cardiac cycle was used for analysis. To minimize variation, one experienced operator performed all investigations (AS); the operator was also blinded to treatment vs. control (placebo) status.
Endothelial-dependent FMD was quantified as the peak percent change in diameter of the brachial artery from resting baseline (at end-diastole) to reactive hyperemia, where measurements were made at 30 seconds, one minute, and two minutes after release of a 4.5 minute forearm occlusion (cuff inflation to 40 mmHg above systolic pressure). Brachial artery blood flow velocity was measured as the peak systolic velocity from the pulsed-wave velocity signal, which was corrected for probe angulations with respect to the vessel. The hyperemic response was measured as the percent change from baseline to the point of maximal reactive hyperemia following release of the forearm cuff occlusion.
Statistical analysis
Descriptive statistics are presented as means and standard errors for each measure at baseline and at 6 weeks for this pilot study with convenience sampling. Because of our concern that the data is not normally distributed, non-parametric Wilcoxon tests were used to compare the folic acid and placebo groups at baseline, at 6 weeks and to compare the 6 week changes between the folic acid and placebo groups. The primary outcome of interest for this pilot study was comparing the 6 week change in brachial artery vasodilator response to reactive hyperemia between the folic acid and placebo groups. For this outcome, an analysis of covariance (ANCOVA) was also performed to adjust for significantly different baseline characteristics between the two groups. An alpha level of 0.05 was used throughout to denote statistical significance.
Results
Baseline characteristics of the folic acid and placebo groups are presented in Table 1. There were no significant differences between the groups in age, height, age of menarche, or miles run per week. It should be noted that 8 subjects were initially enrolled for the placebo group; however, three subjects dropped out prior to initial testing, leaving only five individuals available for analysis. The folic acid group had a lower weight (p < 0.01) and BMI (p = 0.02) at baseline.
Table 1.
Subjects characteristics. Data are means (± SE).
| Folic Acid Group (n = 8) |
Placebo Group (n = 5) |
|
|---|---|---|
| Age (yr) | 25.0 (1.4) | 22.4 (.9) |
| Height (m) | 1.70 (1.00) | 1.70 (.09) |
| Weight (kg) | 58.1 (3.8) | 67.6 (5.8) ** |
| Body Mass Index (kg·m-2) | 20.7 (.6) | 24.4 (1.2) * |
| Age of Menarche (yr) | 13.9 (3.2) | 13.0 (.8) |
| Miles run·week-1 | 30.3 (3.2) | 29.5 (4.1) |
* and ** denote p < 0.05 and 0.01 respectivelyaccording to Exact Wilcoxon Rank-Sum Test.
Baseline brachial artery diameters were similar between the folic acid and placebo groups (p = 0.44), while the peak change in blood flow velocity during reperfusion was slightly higher in the placebo group compared to the folic acid group, although the difference was not statistically significant (p = 0.12) (Table 2). The 6 week change in brachial artery vasodilator response to reactive hyperemia was significantly greater (p < 0.01) in eumenorrheic runners with folic acid supplementation (3.5% ± 0.6%) compared to the placebo group (0.1% ± 0.2%) (Figure 1 and Table 3). This difference persisted even after adjusting for the effect on baseline BMI using ANCOVA (p = 0.03).
Table 2.
Brachial artery studies before supplementation. Data are means (± SE).
| Folic Acid Group (n = 8) |
Placebo Group (n = 5) |
|
|---|---|---|
| Heart rate (min) | 71 (5) | 55 (3) * |
| Mean arterial pressure | ||
| Systolic (mmHg) | 105.3 (2.8) | 106.4 (1.8) |
| Diastolic (mmHg) | 64.9 (2.8) | 60.8 (2.3) |
| Temperature (°C) | 22.8 (.3) | 23.2 (.5) |
| Humidity | 33.8 (1.8) | 42.0 (1.3) * |
| Baseline brachial artery diameter (mm) |
3.1 (.1) | 3.4 (.2) |
| Peak brachial artery diameter (mm) |
3.3 (.1) | 3.6 (.2) |
| Flow-mediated dilation (%) | 6.6 (.8 ) | 6.5 (.7) |
| Peak change in flow velocity (%) | 93.2 (9.4 ) | 121.0 (5.5) |
* denotes p < 0.05 according to Exact Wilcoxon Rank-Sum Test.
Figure 1.
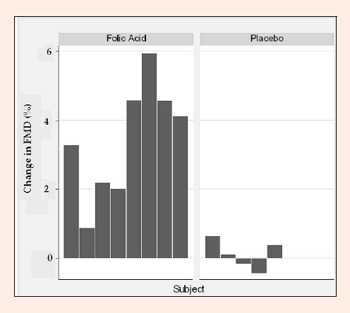
Six week change in brachial artery dilation after folic acid or placebo supplementation in eumenorrheic runners.
Table 3.
Six week changes in brachial artery measures after supplementation. Data are means (± SE).
| Folic Acid Group (n = 8) |
Placebo Group (n = 5) |
|
|---|---|---|
| Heart rate (min) | -9.9 (7.6) | -.8 (1.2) |
| Mean arterial pressure | ||
| Systolic (mmHg) | -2.8 (3.5) | -2.0 (2.5) |
| Diastolic (mmHg) | .4 (2.7) | .2 (2.9) |
| Temperature (°C) | .3 (.8) | 1.8 (.5) |
| Humidity | 8.4 (3.6) | 4.4 ± 0.6 |
| Baseline brachial artery diameter (mm) | .02 (.1) | .2 (.2 ) |
| Peak brachial artery diameter (mm) | .1 (.1 ) | .2 (.2) |
| Flow-mediated dilation (%) | 3.5 (.6) | .11 (.2) ** |
| Peak change in flow velocity (%) | 7.0 (8.0) | -10.6 (12.2) |
** denotes p < 0.01 according to Exact Wilcoxon Rank-Sum Test.
Additional post-supplementation values are listed in Table 4, while the changes from baseline in brachial artery parameters are described in Table 3. There was no difference in serum folate levels prior to supplementation between the two groups (p = 0.64); after supplementation, the folic acid group had significantly higher levels (p < 0.01) (Table 5), with every member of the folic acid group having a serum folate level of >24 ng·mL-1. The folic acid group had at least a 28.1% increase in folic acid levels and the placebo group had a 0.6% increase ( = 0.09). Caution should be used when interpreting this as our lab reports a value of “>24 ”for all values greater than 24 (i.e. 26, 28, 30, 100). Therefore, the percent increase may actually be much higher.
Table 4.
Brachial artery studies after supplementation. Data are means (± SE).
| Folic Acid Group (n = 8) |
Placebo Group (n = 5) |
|
|---|---|---|
| Heart rate (min) | 61 (6) | 54 (4) |
| Mean arterial pressure | ||
| Systolic (mmHg) | 102.5 (1.1 ) | 104.4 (3.0) |
| Diastolic (mmHg) | 65.3 (1.6) | 61.0 (4.0 ) |
| Temperature (°C) | 23.1 (.8) | 25.0 (.0) * |
| Humidity | 42.2 (2.5) | 46.4 (.9) |
| Baseline brachial artery diameter (mm) | 3.1 (.1 ) | 3.52 (.1) ** |
| Peak brachial artery diameter (mm) | 3.4 (.1) | 3.8 (.1) * |
| Flow-mediated dilation (%) | 10.0 (.9) | 6.65 (.7) * |
| Peak change in flow velocity (%) | 100.2 (10.0 ) | 110.4 (8.9) |
* and ** denote p < 0.05 and 0.01 respectivelyaccording to Exact Wilcoxon Rank-Sum Test.
Table 5.
Folic acid levels. Data are means (± SE).
| Folic Acid Group (n = 8) |
Placebo Group (n = 5) |
|
|---|---|---|
| Before Supplementation | 19.9 (1.7) | 18.4 (2.1) |
| After Supplementation | 24.0 (.0) | 17.3 (.9) ** |
** denotes p < 0.01 according to Exact Wilcoxon Rank-Sum Test.
Discussion
In this randomized, double-blinded, placebo-controlled pilot study with convenience sampling, we found that six weeks of folic acid therapy improved brachial artery FMD in eumenorrheic female runners with previously normal serum folate levels and borderline FMD. Folic acid supplementation has already been shown in several studies to improve endothelial function in various disease states, including hypercholesterolemia (Verhaar et al., 1998; 1999), hypertension (van Dijk et al., 2001), diabetes (van Etten et al., 2002) and coronary artery disease (Doshi et al., 2001a; 2002). These data suggest that higher folic acid intake by specific populations may have vasculoprotective effects. Before eumenorrheic female runners with borderline FMD can be added to this group, a large cohort study needs to be performed.
It is well known that hypoestrogenism has deleterious effects on endothelial function and cardiovascular health in postmenopausal women (Lieberman et al., 1994; Mijatovic et al., 1998; Moreau et al., 2003; Ridker et al., 2000; Rosenson et al., 1998; Stevenson et al., 1993; Yen et al., 2001; Yildirir et al., 2002); it is also theorized to contribute at least partially to endothelial dysfunction in young amenorrheic runners (Hoch et al., 2003; Rickenlund et al., 2005b). Estrogen plays an important regulatory role in vascular function through its effects on vascular endothelial cells and smooth muscle cells, both of which express the two known estrogen receptors. Importantly, it has both fast vasodilatory effects and slower, longer-term actions which inhibit the response to vascular injury and thus help prevent atherosclerosis. Estrogen increases both production of endothelial-derived nitric oxide, leading to vasodilation (Cid et al., 2002; Mendelsohn, 2002; Schnaper et al., 2000), and stimulates longer-term genomic effects, resulting in increased eNOS synthesis and activity (Mendelsohn, 2002). Less is known about the role that progesterone plays in endothelial-dependent vascular responses such as FMD, especially in premenopausal women.
When comparing chronic estrogen suppression in amenorrheic athletes to the cyclical fluctuation of estrogen in eumenorrheic athletes, it is more accurate to assess estrogen status and ovulation with daily urinary analysis of estrogen metabolites throughout the menstrual cycle (O'Donnell et al., 2004). The runners in this study reported in both an interview and questionnaire that they were having normal menstrual periods every 28-32 days; however, it was beyond the scope of this study to measure serum estrogen levels or daily urinary estrogen metabolites. It is important to understand that menstrual dysfunction occurs along a continuum: women with anovulatory cycles may still have menstrual bleeding, and thus appear eumenorrheic, but their overall estrogen levels will be lower than women with true ovulatory eumenorrhea. This theory may begin to explain the borderline endothelial function seen in studies of oligomenorrheics and self-reported eumenorrheic athletes (Hoch et al., 2003). It is beyond the scope of this study to measure estrogen levels and determine ovulation. This requires measuring daily urinary metabolites for 28 - 30 days.
Consequently, there may exist a critical level of estrogen exposure which affects endothelial function independent of the presence or absence of menstrual bleeding. In support of this, Rickenlund et al., 2005b has recently shown that there was no difference in estrogen levels between amenorrheic (29 pg·mL-1) and eumenorrheic (30 pg/mL) runners with similar training schedules. Control sedentary women, on the other hand, had significantly higher estrogen levels (38 pg·mL-1) than either of the runner groups. Further, it was shown that oral contraceptive administration (30 μg ethinyl estradiol and 150 μg levonorgestrel) significantly improved brachial artery FMD in young amenorrheic runners (Rickenlund et al., 2005b); other researchers have also demonstrated similar findings (Hoch et al., 2005). Therefore, from a clinical perspective, it would seem logical that if flow-mediated dilation was determined to be low clinicians could potentially recommend folic acid on a daily basis. However, the optimal dose is still to be determined.
There have been no reported side effects of folic acid at 10 mg·day-1 (Moens et al., 2007; Title et al., 2006; US Food and Drug Administration, 2008; Wilmink et al., 2000; Woo et al., 1999). Higher doses > 15 mg·day-1 can cause side effects such as upset stomach, sleep disturbances and skin problems. The RDA for folate for women ages 19-50 is 400 μg·day-1 and the tolerable upper intake level (UL) is 1 g·day-1. For women with risk factors for neural tube defects, 4 mg is recommended. It is important to recognize that the upper intake level refers to the amount of synthetic folate (folic acid) being consumed per day from fortified foods and/or supplements. There is no health risk and no UL for natural sources of folate found in food. The risk of toxicity from folic acid intake from supplements and/or fortified foods is low (Hathcock, 1997). It is a water soluble vitamin that is regularly eliminated in the urine. There is some evidence that high levels of folic acid can provoke seizures in patients taking anti-convulsant medications (Herbert, 1999). None of our subjects had a known seizure disorder.
The National Institutes of Health (National Institutes of Health, 2008) also states, under supplementation with folic acid, caution should be used in patients with a vitamin B12 deficiency as this may hide the deficiency and silently exacerbate the condition.
Finally, in the current study there was a difference in blood flow velocity change during reperfusion between the folic acid (93%) and placebo (121%) groups. This may be secondary to the higher temperature and relative humidity at time of follow-up testing in this group. However, this acts to amplify our findings since the folic acid group still had a significantly greater increase in FMD.
Although these results are significant, we do concede that there are several limitations in the current study. Both the folic acid and placebo groups were small and so these observations should be investigated in a larger cohort of individuals. Further, despite not obtaining extensive dietary histories, the fact that serum folate levels were significantly higher in the folic acid group and unchanged in the placebo group after 6 weeks likely confirms our assumption that the 10 mg·day-1 supplementation was the major factor influencing the amount of serum folate. Finally, weight and BMI were significantly lower in the folic acid group at the start of the study; it is unclear if this played a role in FMD when both groups were in the “normal ”range for BMI (National Heart, 2007) as well as within 5 kg·m-2 of each other (Benjamin et al., 2004). Although the observed effect on FMD still persisted after adjusting for baseline BMI, this and similar covariate imbalance could still have the potential to confound our results.
Conclusion
Our data indicate that oral folic acid treatment may provide a safe and inexpensive tool to improve endothelial function in eumenorrheic female runners with borderline FMD and thus potentially reduce future cardiovascular risk. The present observation may have important clinical implications particularly for athletes opposed to estrogen supplementation. High-dose folic acid (10 mg/day) for at least six weeks improves brachial artery FMD in eumenorrheic runners with previously normal serum folate levels; further research is needed to clarify the exact mechanism by which this occurs. Additionally, future studies may help determine the precise level of folic acid supplementation which confers significant vascular benefits.
Acknowledgement
The authors of this study would like to acknowledge the Cardiovascular Center at the Medical College of Wisconsin for their continued support of our research. We would also like to thank Michael Widlansky, MD for reviewing this manuscript. This study was partially funded by the Cardiovascular Center at the Medical College of Wisconsin, Milwaukee. This study was also funded in part by NIH Grant 5-M01-RR00058-39.
Biographies

Anne Z. Hoch
Employment
Associate Professor, Medical College of Wisconsin.
Degree
DO
Research interests
Sports medicine, female athletes, Female Athlete Triad, cardiovascular dysfunction.
E-mail: azeni@mcw.edu
Nicholas M. Pajewski
Employment
Postdoctoral Fellow, Medical College of Wisconsin.
Degree
PhD.
Research interests
tatistical genetics, bayesian statistics.
E-mail: npajewsk@mcw.edu

Jane E. Schimke
Employment
Clinical Research Coordinator, Medical College of Wisconsin.
Degree
AAS
Research interests
Sports medicine, female athletes.
E-mail: jschimke@mcw.edu

David D. Gutterman
Employment
Sr. Associate Dean for Research, Office of Research, Medical College of Wisconsin.
Degree
MD
Research interests
Vascular biology, endothelial function, oxidative stress, coronary circulation.
E-mail: dgutt@mcw.edu
References
- Benjamin E.J., Larson M.G., Keyes M.J., Mitchell G.F., Vasan R.S., Keaney J.F., Jr., Lehman B.T., Fan S., Osypiuk E., Vita J.A. (2004) Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation 109, 613-619 [DOI] [PubMed] [Google Scholar]
- Bonetti P.O., Lerman L.O., Lerman A. (2003) Endothelial dysfunction: a marker of atherosclerotic risk. Arteriosclerosis, Thrombosis, and Vascular Biology 223, 168-175 [DOI] [PubMed] [Google Scholar]
- Celermajer D.S. (1997) Endothelial dysfunction: does it matter?. Is it reversible? Journal of the American College of Cardiology 330, 325-333 [DOI] [PubMed] [Google Scholar]
- Celermajer D.S., Sorensen K.E., Gooch V.M., Spiegelhalter D.J., Miller O.I., Sullivan I.D., Lloyd J.K., Deanfield J.E. (1992) Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340, 1111-1115 [DOI] [PubMed] [Google Scholar]
- Chambers J.C., Ueland P.M., Obeid O.A., Wrigley J., Refsum H., Kooner J.S. (2000) Improved vascular endothelial function after oral B vitamins: An effect mediated through reduced concentrations of free plasma homocysteine. Circulation 102, 2479-2483 [DOI] [PubMed] [Google Scholar]
- Cid M.C., Schnaper H., Kleinman H.K. (2002) Estrogens and the vascular endothelium. Annals of the New York Academy of Sciences 966, 143-157 [DOI] [PubMed] [Google Scholar]
- Corretti M.C., Anderson T.J., Benjamin E.J., Celermajer D., Charbonneau F., Creager M.A., Deanfield J., Drexler H., Gerhard-Herman M., Herrington D., Vallance P., Vita J., Vogel R. (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. Journal of the American College of Cardiology 339, 257-265 [DOI] [PubMed] [Google Scholar]
- Deol P.S., Barnes T.A., Dampier K., John P.K., Oppenheimer C., Pavord S.R. (2004) The effects of folic acid supplements on coagulation status in pregnancy. British Journal of Haematology 127, 204-208 [DOI] [PubMed] [Google Scholar]
- Doshi S.N., McDowell I.F., Moat S.J., Lang D., Newcombe R.G., Kredan M.B., Lewis M.J., Goodfellow J. (2001a) Folate improves endothelial function in coronary artery disease: an effect mediated by reduction of intracellular superoxide? Arteriosclerosis, Thrombosis, and Vascular Biology 221, 1196-1202 [DOI] [PubMed] [Google Scholar]
- Doshi S.N., McDowell I.F., Moat S.J., Payne N., Durrant H.J., Lewis M.J., Goodfellow J. (2002) Folic acid improves endothelial function in coronary artery disease via mechanisms largely independent of homocysteine lowering. Circulation 105, 22-26 [DOI] [PubMed] [Google Scholar]
- Doshi S.N., Naka K.K., Payne N., Jones C.J., Ashton M., Lewis M.J., Goodfellow J. (2001b) Flow-mediated dilatation following wrist and upper arm occlusion in humans: the contribution of nitric oxide. Clinical Science (London) 101, 629-635 [PubMed] [Google Scholar]
- Ganz P., Vita J.A. (2003) Testing endothelial vasomotor function: nitric oxide, a multipotent molecule. Circulation 108, 2049-2053 [DOI] [PubMed] [Google Scholar]
- Hashimoto M., Akishita M., Eto M., Ishikawa M., Kozaki K., Toba K., Sagara Y., Taketani Y., Orimo H., Ouchi Y. (1995) Modulation of endothelium-dependent flow-mediated dilatation of the brachial artery by sex and menstrual cycle. Circulation 992, 3431-3435 [DOI] [PubMed] [Google Scholar]
- Hathcock J.N. (1997) Vitamins and minerals: efficacy and safety. Americian Journal of Clinical Nutrition 666, 427-437 [DOI] [PubMed] [Google Scholar]
- Herbert V. (1999) Folic acid. In: Modern nutrition in health and disease. Eds: Shils M., Olson J., Shike M., Ross AC. Baltimore: Williams & Wilkins; 433-466 [Google Scholar]
- Hoch A.Z., Adams B., Syed A.Q., Syed A.Y., Clifford P.S., Gutterman D. (2005) Folic acid supplementation improves endothelial function in eumenorrheic runners. Medicine & Science in Sports & Exercise 337, S52, 2005 [Google Scholar]
- Hoch A.Z., Dempsey R.L., Carrera G.F., Wilson C.R., Chen E.H., Barnabei V.M., Sandford P.R., Ryan T.A., Gutterman D.D. (2003) Is there an association between athletic amenorrhea and endothelial cell dysfunction? Medicine & Science in Sports & Exercise 335, 377-383 [DOI] [PubMed] [Google Scholar]
- Lieberman E.H., Gerhard M.D., Uehata A., Walsh B.W., Selwyn A.P., Ganz P., Yeung A.C., Creager M.A. (1994) Estrogen improves endothelium-dependent, flow-mediated vasodilation in postmenopausal women. Annals of Internal Medicine 121, 936-941 [DOI] [PubMed] [Google Scholar]
- Mangoni A.A., Arya R., Ford E., Asonganyi B., Sherwood R.A., Ouldred E., Swift C.G., Jackson S.H. (2003) Effects of folic acid supplementation on inflammatory and thrombogenic markers in chronic smokers. A randomised controlled trial. Thrombosis Research 110, 13-17 [DOI] [PubMed] [Google Scholar]
- Mangoni A.A., Ouldred E., Swif C.G., Jackson S.H., Draper R.P., Sherwood R.A., Lambert-Hammill M., Wierzbicki A.S. (2001) Vascular and blood pressure effects of folic acid in older patients with cardiovascular disease. Journal of the American Geriatrics Society 449, 1003-1004 [DOI] [PubMed] [Google Scholar]
- Mangoni A.A., Sherwood R.A., Asonganyi B., Swift C.G., Thomas S., Jackson S.H. (2005) Short-term oral folic acid supplementation enhances endothelial function in patients with type 2 diabetes. American Journal of Hypertension 118, 220-226 [DOI] [PubMed] [Google Scholar]
- Mangoni A.A., Sherwood R.A., Swift C.G., Jackson S.H. (2002) Folic acid enhances endothelial function and reduces blood pressure in smokers: a randomized controlled trial. Journal of Internal Medicine 252, 497-503 [DOI] [PubMed] [Google Scholar]
- Mather K.J., Norman E.G., Prior J.C., Elliott T.G. (2000) Preserved forearm endothelial responses with acute exposure to progesterone: A randomized cross-over trial of 17-beta estradiol, progesterone, and 17-beta estradiol with progesterone in healthy menopausal women. Journal of Clinical Endocrinology & Metabolism 85, 4644-4649 [DOI] [PubMed] [Google Scholar]
- Mendelsohn M.E. (2002) Protective effects of estrogen on the cardiovascular system. American Journal of Cardiology 889, 12E-17E [DOI] [PubMed] [Google Scholar]
- Mijatovic V., Kenemans P., Jakobs C., van Baal W.M., Peters-Muller E.R., van der Mooren M.J. (1998) A randomized controlled study of the effects of 17beta-estradiol-dydrogesterone on plasma homocysteine in postmenopausal women. Obstetrics & Gynecology 991, 432-436 [DOI] [PubMed] [Google Scholar]
- Moens A.L., Claeys M.J., Wuyts F.L., Goovaerts I., Van Hertbruggen E., Wendelen L.C., Van Hoof V.O., Vrints C.J. (2007) Effect of folic acid on endothelial function following acute myocardial infarction. American Journal of Cardiology 999, 476-481 [DOI] [PubMed] [Google Scholar]
- Moreau K.L., Donato A.J., Tanaka H., Jones P.P., Gates P.E., Seals D.R. (2003) Basal leg blood flow in healthy women is related to age and hormone replacement therapy status. Journal of Physiology 547, 309-316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Heart (2007) Calculate your body mass index. Available from URL: http://www.nhlbisupport.com/bmi/. Retrieved November 1, 2008
- National Institutes of Health (2008) Office of dietary supplements. Dietary supplement fact sheet: Folate. Published online. Available from URL: http://ods.od.nih.gov/factsheets/folate.asp#en10 Retrieved November 13, 2008
- O'Donnell E., De Souza M. J. (2004) The cardiovascular effects of chronic hypoestrogenism in amenorrhoeic athletes: a critical review. Sports Medicine 334, 601-627 [DOI] [PubMed] [Google Scholar]
- Ohmichi M., Kanda Y., Hisamoto K., Morishige K., Takahashi K., Sawada K., Minekawa R., Tasaka K., Murata Y. (2003) Rapid changes of flow-mediated dilatation after surgical menopause. Maturitas 444, 125-131 [DOI] [PubMed] [Google Scholar]
- Pancharuniti N., Lewis C.A., Sauberlich H.E., Perkins L.L., Go R.C., Alvarez J.O., Macaluso M., Acton R.T., Copeland R.B., Cousins A.L. (1994) Plasma homocyst(e)ine, folate, and vitamin B-12 concentrations and risk for early-onset coronary artery disease. American Journal of Clinical Nutrition 559, 940-948 [DOI] [PubMed] [Google Scholar]
- Rickenlund A., Eriksson M.J., Schenck-Gustafsson K., Hirschberg A.L. (2005a) Amenorrhea in female athletes is associated with endothelial dysfunction and unfavorable lipid profile. Journal of Clinical Endocrinology & Metabolism 990, 1354-1359 [DOI] [PubMed] [Google Scholar]
- Rickenlund A., Eriksson M.J., Schenck-Gustafsson K., Hirschberg A.L. (2005b) Oral contraceptives improve endothelial function in amenorrheic athletes. Journal of Clinical Endocrinology & Metabolism 990, 3162-3167 [DOI] [PubMed] [Google Scholar]
- Ridker P.M., Hennekens C.H., Buring J.E., Rifai N. (2000) C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. New England Journal of Medicine 342, 836-843 [DOI] [PubMed] [Google Scholar]
- Rosenson R.S., Tangney C.C., Mosca L.J. (1998) Hormone replacement therapy improves cardiovascular risk by lowering plasma viscosity in postmenopausal women. Arteriosclerosis, Thrombosis, and Vascular Biology 118, 1902-1905 [DOI] [PubMed] [Google Scholar]
- Ross R. (1999) Atherosclerosis--an inflammatory disease. New England Journal of Medicine 340, 115-126 [DOI] [PubMed] [Google Scholar]
- Rossouw J.E., Anderson G.L., Prentice R.L., LaCroix A.Z., Kooperberg C., Stefanick M.L., Jackson R.D., Beresford S.A., Howard B.V., Johnson K.C., Kotchen J.M., Ockene J. (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. Journal of the American Medical Association 288, 321-333 [DOI] [PubMed] [Google Scholar]
- Schnaper H.W., McGuire J., Runyan C., Hubchak S.C. (2000) Sex steroids and the endothelium. Current Medicinal Chemistry 77, 519-531 [DOI] [PubMed] [Google Scholar]
- Schutte A.E., Huisman H.W., Oosthuizen W., van Rooyen J.M., Jerling J.C. (2004) Cardiovascular effects of oral Supplementation of vitamin C, E and folic acid in young healthy males. International Journal for Vitamin and Nutrition Research 774, 285-293 [DOI] [PubMed] [Google Scholar]
- Stevenson J.C., Crook D., Godsland I.F. (1993) Influence of age and menopause on serum lipids and lipoproteins in healthy women. Atherosclerosis 998, 83-90 [DOI] [PubMed] [Google Scholar]
- Title L.M., Ur E., Giddens K., McQueen M.J., Nassar B.A. (2006) Folic acid improves endothelial dysfunction in type 2 diabetes--an effect independent of homocysteine-lowering. Vascular Medicine 111, 101-109 [DOI] [PubMed] [Google Scholar]
- Undas A., Domagala T.B., Jankowski M., Szczeklik A. (1999) Treatment of hyperhomocysteinemia with folic acid and vitamins B12 and B6 attenuates thrombin generation. Thrombosis Research 995, 281-288 [DOI] [PubMed] [Google Scholar]
- US Food and Drug Administration (2008) The FDA safety information and adverse event reporting program: Medical product safety information. Available from URL: http://www.fda.gov/medwatch/ SAFETY.htm. Retrieved December 8, 2008
- van den B.M., Boers G.H., Franken D.G., Blom H.J., Van Kamp G.J., Jakobs C., Rauwerda J.A., Kluft C., Stehouwert C.D. (1995) Hyperhomocysteinaemia and endothelial dysfunction in young patients with peripheral arterial occlusive disease. European Journal of Clinical Investigation 225, 176-181 [DOI] [PubMed] [Google Scholar]
- van Dijk R.A., Rauwerda J.A., Steyn M., Twisk J.W., Stehouwer C.D. (2001) Long-term homocysteine-lowering treatment with folic acid plus pyridoxine is associated with decreased blood pressure but not with improved brachial artery endothelium-dependent vasodilation or carotid artery stiffness: a 2-year, randomized, placebo-controlled trial. Arteriosclerosis, Thrombosis, and Vascular Biology 221, 2072-2079 [DOI] [PubMed] [Google Scholar]
- van Etten R.W., de Koning E.J., Verhaar M.C., Gaillard C.A., Rabelink T.J. (2002) Impaired NO-dependent vasodilation in patients with Type II (non-insulin-dependent) diabetes mellitus is restored by acute administration of folate. Diabetologia 445, 1004-1010 [DOI] [PubMed] [Google Scholar]
- Verhaar M.C., Wever R.M., Kastelein J.J., van Dam T., Koomans H.A., Rabelink T.J. (1998) 5-methyltetrahydrofolate, the active form of folic acid, restores endothelial function in familial hypercholesterolemia. Circulation 997, 237-241 [DOI] [PubMed] [Google Scholar]
- Verhaar M.C., Wever R.M., Kastelein J.J., van Loon D., Milstien S., Koomans H.A., Rabelink T.J. (1999) Effects of oral folic acid supplementation on endothelial function in familial hypercholesterolemia: A randomized placebo-controlled trial [In Process Citation]. Circulation 100, 335-338 [DOI] [PubMed] [Google Scholar]
- Wever R.M., van Dam T., van Rijn H.J., de Groot F., Rabelink T.J. (1997) Tetrahydrobiopterin regulates superoxide and nitric oxide generation by recombinant endothelial nitric oxide synthase. Biochemical and Biophysical Research Communications 237, 340-344 [DOI] [PubMed] [Google Scholar]
- Williams M.R., Westerman R.A., Kingwell B.A., Paige J., Blombery P.A., Sudhir K., Komesaroff P.A. (2001) Variations in endothelial function and arterial compliance during the menstrual cycle. Journal of Clinical Endocrinology & Metabolism 886, 5389-5395 [DOI] [PubMed] [Google Scholar]
- Wilmink H.W., Stroes E.S., Erkelens W.D., Gerritsen W.B., Wever R., Banga J.D., Rabelink T.J. (2000) Influence of folic acid on postprandial endothelial dysfunction. Arteriosclerosis, Thrombosis, and Vascular Biology 220, 185-188 [DOI] [PubMed] [Google Scholar]
- Woo K.S., Chook P., Lolin Y.I., Sanderson J.E., Metreweli C., Celermajer D.S. (1999) Folic acid improves arterial endothelial function in adults with hyperhomocystinemia. Journal of the American College of Cardiology 34, 2002-2006 [DOI] [PubMed] [Google Scholar]
- Yen C.H., Hsieh C.C., Chou S.Y., Lau Y.T. (2001) 17Beta-estradiol inhibits oxidized low density lipoprotein-induced generation of reactive oxygen species in endothelial cells. Life Sciences 770, 403-413 [DOI] [PubMed] [Google Scholar]
- Yildirir A., Aybar F., Tokgozoglu L., Yarali H., Kabakci G., Bukulmez O., Sinici I., Oto A. (2002) Effects of hormone replacement therapy on plasma homocysteine and C-reactive protein levels. Gynecologic and Obstetric Investigation 553, 54-58 [DOI] [PubMed] [Google Scholar]


