Abstract
Platelet-rich plasma (PRP) to increase levels of platelets and growth factors has been used for the treatment of sports injuries suggesting to improve healing and regeneration. This method offers some potential especially for elite athletes. However, the insulin like growth factor-1 (IGF-1) is prohibited by the World Anti Doping Agency and, in addition, there may be a possible link between increased levels of IGF-1 and cancer risk. Aim of the study was to evaluate a systemic increase of IGF-1 after local intramuscular administration of PRP in young healthy moderately trained male subjects. Blood samples were drawn and PRP preparation was performed by means of centrifugation. Enriched plasma was injected into the gluteus muscle. Venous blood was collected and serum prepared before as well as after 0.5, 3 and 24 hours after PRP administration. IGF-1 analysis was performed applying an ELISA test kit. No significant systemic increase of mean IGF-1 was found after the PRP injection. Only one subject showed an increase after 24 h, but all IGF-1 values were found within reference limits. We conclude that a single intramuscular application of PRP does not significantly increase systemic IGF-1 levels. Therefore, a single application of PRP is safe with respect to systemic IGF-1 response and cancer risk and this should be allowed for treatment of muscle injuries in elite athletes.
Key points.
There is no increase of systemic IGF-1 levels after a single local intramuscular administration of PRP.
Professional athletes and non-athletes alike can benefit from such a treatment option for muscle injuries and related sports injuries without an increased risk of cancer.
More studies are warranted to provide definitive evidence to guide surgeon’s decision making regarding the appropriate use for PRP products.
Key words: Platelet rich plasma, intramuscular application, IGF-1, cancer risk, doping.
Introduction
Recently, an increased trend has emerged in the use of autologous blood products in an effort to promote healing in a variety of applications such as muscle injuries, chronic tendinopathies and cartilage degeneration (Baltzer et al., 2009; Banfi et al., 2006; Castricini et al., 2011; Creaney and Hamilton, 2008, Volpi et al., 2010). The potentially beneficial method described is the homologous local application of concentrated platelets (Baltzer et al., 2009; Banfi et al., 2006; Mishra and Pavelko, 2006) also known as platelet rich plasma (PRP) (Foster et al., 2009). Several preliminary studies showed possible benefits of this therapeutic PRP application (Banfi et al., 2006; Baltzer et al., 2009, Mishra and Pavelko, 2006; Sánchez et al., 2009). However, the evidence is not supported yet (Arnoczky et al., 2009). The method may be very attractive for athletes but there are serious contradictions with respect to doping issues and the World Anti Doping Agency (WADA) code which have rarely been investigated to date (WADA, 2011)
The PRP method and its application
PRP can be defined as plasma containing a concentration of platelets that is above the concentration found in whole blood. Platelet-rich plasma, with a platelet concentration of at least 109 platelets·l-1, is very likely associated with the enhancement of healing (Marx, 2004). Platelet-rich plasma contains up to 4 times the concentration of platelets found in whole blood. The basic bioactive factors identified in platelets are the transforming growth factor-β (TGF-β), the platelet-derived growth factor (PDGF), the insulin-like growth factors (IGF-1, IGF-2), the fibroblast growth factor (FGF), the epidermal growth factor, the vascular endothelial growth factor (VEGF), and the endothelial growth factor (EGF). These cytokines play important roles in cell proliferation, chemotaxis, cell differentiation, and angiogenesis (Foster et al., 2009).
Although debate continues regarding the potential benefit of PRP to improve bone healing (Griffin et al., 2009; Ranly et al., 2007) a growing body of laboratory evidence supports the use of PRP injections for the treatment of muscle and tendon injuries (Sánchez et al., 2007, 2009b; Wright-Carpenter et al., 2004). However, a recent randomized controlled study by Castricini et al., 2011 did not support the use of autologous platelet-rich fibrin matrix in the treatment of rotator cuff injury.
Sports injuries to muscle tissue are very frequent due to a direct blow or tearing of the muscle. Early recovery is crucial for athletes and therefore therapies pushing the healing process are very attractive (Lopez-Vidriero et al., 2010). As in other parts of the body, healing is dependent upon the vascularity of the tissue (Yokota et al., 2008). The speed of recovery depends on the severity of the injury, the post injury treatment, and the patient’s inherent ability to heal soft tissue injuries. Several techniques have been employed in an effort to shorten return to play intervals. Platelet-rich plasma has been suggested as a potential intervention for athletes with acute muscular injuries (Lopez-Vidriero et al., 2010). One in vitro study suggests that growth factors may influence muscle regeneration after injury (Kasemkijwattana et al., 2000). Platelet-rich plasma treatment after an acute muscular injury may benefit the athlete by decreasing the time of recovery; however, there are no randomized controlled human studies regarding the use of PRP for muscle injuries.
Beside possible beneficial effects of PRP, several concerns have been raised about undesireable side effects. Particular attention is focused on IGF-1 because of its potential doping (Tentori and Graziani, 2007) and carcinogenetic affect (Grimberg and Cohen, 2000; Grimberg, 2003, LeRoith and Roberts, 2003; Lann and LeRoith, 2008; Rowlands et al., 2009).
Banfi et al., 2006 already investigated the systemic response of several growth factors after a single PRP application, however, these authors did not investigate IGF-1.
IGF-1
IGF-1 has at least three isoforms, whereof the isoform IGF-1Ea is known to stimulate terminal differentiation of muscle cells into myotubes and promote stem cell-mediated muscle regeneration, whereas MGF (isoform IGF-1Ec) is damage sensitive, controls local tissue repair and is more potent than IGF-1Ea at causing hypertrophy. MGF is rapidly degraded in the serum (Philippou et al., 2007).
Serum IGF-1 levels vary greatly among individuals and depend on genetic influences and nutritional status. Typical mean values of 299 μg·l-1 (reference range 158(-2 SD) -497(+2SD) μg·l-1) and 230 μg·l-1 (range 112 (-2SD) -402 (+2SD) μg·l-1) has been described for 20 and 25 years old males, respectively (Brabant et al., 2003).
IGF-1 and carcinogenesis
In reference to carcinogenesis, Creaney and Hamilton, 2008 and Marx, 2004 suggested that growth factors act on cell surface receptors, do not enter the cell, and do not cause DNA mutation. Therefore, from their point of view, no plausible mechanism can be described by which growth factors result in neoplastic development. Despite no direct evidence published so far, there are some indications that elevated IGF-1 may have some relationship to cancer development. Grimberg and Cohen, 2000 and Grimberg, 2003 concluded in their review papers that multiple large case-control studies have reported positive associations between high circulating levels of IGF-1 and risk for different types of cancer and they critically mentioned that this hypothesis is worth for further examinations through mechanistic studies. A systematic review and meta-regression analysis by Renehan et al., 2004 showed that concentrations of circulating IGF-1 and IGFBP-3 (an IGF binding protein) were associated with an increased risk of common cancers, but associations were modest and varied between sites.
IGF-1 and doping issues
The latest statement of the WADA 2011 has deleted the prohibition of intramuscular injection of platelet-derived preparations (e.g. PRP, “blood spinning”) (WADA, 2011). All routes of administration require a declaration of use in accordance with the International Standard for Therapeutic Use Exemptions (TUE).
The fact that IGF-1 is a prohibited substance in the prohibited S2 section by the WADA is an important concern which has provoked discussions among orthopaedic sports medicine practitioners. A detailed analysis of the prohibited S2 section reveals that besides IGF-1 several growth factors affecting muscle, tendon or ligament protein synthesis/degradation, vascularization, energy utilization, regenerative capacity or fibre type switching are prohibited with the exception of platelet-rich therapies applied intramuscularly (WADA, 2011) (Engebretsen et al., 2010).
Overall, basic scientific research supports the opinion that PRP is unlikely to provide a potent ergogenic aid for the following reasons:
The doses of IGF-1 in PRP are subtherapeutic in terms of producing systemic anabolic actions by a factor of 500 (300 ng versus 160 μg) (Creaney and Hamilton, 2008). Several commercial PRP systems such as ACP, GPS, and PRGF have been shown not to increase IGF-1 over normal circulating blood levels (Conway et al., 2006; Eppley et al., 2004; Buhr and Siekmann, 2009; Sánchez et al., 2007; Anitua et al., 2005).
The availability of most IGF-1 is modulated by a binding protein (IGFBP-3) and only 1% of the total IGF-1 released from the PRGF is unbound, and therefore biologically available and active, ready to bind to receptors (IGF-IRs) inducing biological outcomes. In addition, the unbound IGF-1 has too short a half-life to be able to exert systemic effects (10 min versus 16 h for the bound form) (Foster et al., 2009).
The isoform IGF-1Ea found in PRP is not the isoform principally responsible for skeletal muscle hypertrophy (IGF-1Ec/MGF) and may not have the same performance-enhancing effects as skeletal muscle-derived IGF-1Ec (MGF) (Creaney and Hamilton, 2008).
Although it is unlikely that a single PRP injection systematically increases IGF-1, this important growth factor has, to our knowledge, not been investigated yet in this regard.
The aim of the study was to investigate possible systemic effects of intramuscularly applied PRP on serum IGF-1 levels in healthy subjects to exclude potential (cancer) risks and to clarify doping issues. In line with the literature we hypothesized no systemic IGF-1 effect after one single PRP injection. This might be of relevance for top level athletes and non-athletes alike, as neither the increased risk of cancer promotion nor the risk for a positive doping test by a distinct systemic increase of IGF-1 would exist.
Methods
Ten 23 ± 1.5 years old healthy trained male subjects (VO2max: 52.0 ± 11.1 ml·kg-1·min-1; body mass: 78.7 ± 9.3 kg, height 1.84 ± 0.08 m) were investigated. Written informed consent was obtained from all subjects and the study was approved by the local ethics committee (No.: 21-160ex 09/10).
Prior to taking blood, 1 ml of ACD-A (Anticoagulant Citrate Dextrose Solution, NoClot 400TM, Cytosol Laboratories, INC) was withdrawn into the outer syringe of an ACP Doublesyringe system (Arthrex®). Then 9 ml of venous blood was withdrawn with a butterfly cannula of the cubital vein. The blood was processed at 1500 rpm for 5 minutes within a centrifuge (Hettich Rotofix 32A) to separate plasma from erythrocytes and leukocytes and the plasma transferred to the smaller syringe by pulling the according (small) plunger. Thereafter, 2.5 ml of autologous conditioned plasma (ACP) was injected into the right gluteus maximus of each subject.
According to the manufacturer’s reference the ACP product consists of a 1.6 fold increase of platelets (unpublished white paper, Arthrex®), a 2-6 fold increase in the growth factors EGF, VEGF, TGF-β1, TGF-β2, PDGF-AB, PDGF-BB, as well as a 10% increase in IGF-1 (Engebretesen et al. 2010)
Venous blood samples were drawn from the same cubital vein and serum was prepared to determine IGF-1 levels before ACP administration, after 30 minutes, 3 hours and 24 hours, respectively. Samples were stored at -20°C until further processing. All subjects were requested to abstain from any exercise at least two days prior to testing and during the observation period.
Serum IGF-1 was measured in duplicate using the R&D Quantikine ELISA testkit for human IGF-1 (Biomedica, Vienna, Austria) following the manufacturer’s instructions. Intra-assay precision was found within the limits described by the manufacturer to be between 3.5 and 4.3 % (Human IGF-1 immunoassay, Quantikine, R&D Systems).
The actual number of platelets was not directly measured but the manufacturer’s specification suggest a 1.6 fold increase of platelets compared to whole blood (unpublished white paper, Arthrex®)
Statistical analysis
Measures are reported as means (±SD) and data were tested as being normally distributed (Kolmogorov-Smirnov-test; Winstat, Calmia Corp., USA). Comparisons between pre and post IGF-1 levels were performed by means of repeated measures ANOVA. A p-value < 0.05 was considered to be significant. The required sample size of 10 subjects was calculated a-priori by G*Power analysis (Faul et al., 2007) (using an assumed large effect size of 0.4 (Cohen, 1988), an α-level of 0.05 and a power of 0.8) to simulate a meaningful elevation of IGF-1 above mean values for this age group (Brabant et al., 2003).
Results
Mean pre application values of IGF-1 were found at the lower limit of age related norms (161 ± 27 μg·l-1) as shown by Brabant et al., 2003. The application of ACP did not influence mean IGF-1 values after 30 minutes (157 ± 29 μg·l-1), 3 (159 ± 25 μg·l-1) and 24 hours (161 ± 38 μg·l-1), receptively. There was no significant difference detectable between groups (repeated measures ANOVA p-value > 0.05). The individual time courses of IGF-1 were essentially the same in all subjects except one (Figure 1), who presented an increase of IGF-1 from 171 pre ACP conditions up to 220 μg·l-1 after 24 hours post PRP application. All single values were within the age related means for IGF-1 in this age group.
Figure 1.
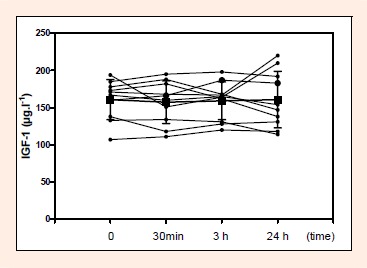
Individual time course of systemic IGF-1 levels after ACP administration in young healthy trained subjects
Discussion
A single intramuscular ACP administration in young healthy trained subjects had no effect on circulating IGF-1 values. Only one subject showed an increase from pre ACP conditions to post ACP injection after 24 hours. However, this change was within reference limits for this age group (Brabant et al., 2003).
Several studies have suggested that PRP may be advantageous in sports medicine, but there are little data aside from small case series to support this hypothesis. The majority of performed human studies are level 4 and 5 studies, which demonstrated the efficacy of PRP in treating tendinopathies (Arnoczky et al., 2009; Foster et al., 2009; Mishra and Pavelko, 2006; Sánchez et al., 2009a, 2009b). There is a need for prospective, randomized controlled double-blind studies that meet the requirements for properly powered studies. Despite this fact the authors believe this technology may see new exciting developments in the next decades.
IGF-1 and carcinogenesis
One concern may be a potential carcinogenic effect of IGF-1 provided that PRP application results in a sustained increase in IGF-1 levels above normal. Several authors concluded positive associations between high circulating levels of IGF-I and risk for different types of cancer (Grimberg and Cohen, 2000; Grimberg, 2003, LeRoith and Roberts, 2003; Lann and LeRoith, 2008; Rowlands et al., 2009; Chen et al., 2009). A single intramuscular PRP administration however, did not show an increase in circulating IGF-1 levels after 30 minutes and 3 and 24 hours post application. From this point of view, a single PRP injection is suggested to be a safe method of treatment at least as applied in our study. Although multiple injections were not specifically examined in this study, the lack of increase in IGF-1 seen in the 10 subjects combined with the fact that most PRP systems do not concentrate IGF-1 (Anitua et al., 2005; Buhr and Siekmann, 2009; Conway et al., 2006; Eppley et al., 2004; Sánchez et al., 2007) would not raise additional concerns regarding carcinogenic effects of IGF-1 increase as a result of multiple injections.
IGF-1 and doping issues
An important issue is the fact that administration of PRP in sports medicine was critically discussed to by the WADA, particularly because of concerns regarding the IGF-1 content of such preparations and its potential for abuse as performance-enhancing agents. It has been shown recently that PRP products are unlikely to increase IGF-1 levels systemically, although not experimentally proven (Creaney and Hamilton, 2008). Still, it has to be clearly stated that exogenous IGF-1 administration apart from PRP as performance enhancing growth hormone is still banned by the WADA anti-doping code (section S2). Growth hormones have gained popularity in the last two decades due to the availability of the recombinant forms and are now largely used in the sports world (Saugy et al., 2006; Sonkens, 2001; Stay et al., 2004). Nowadays, athletes such as cyclists, swimmers, power lifters and body builders are suspected to use recombinant GH or IGF-1 for desired anabolic effects (Stay et al., 2004; Saugy et al., 2006; Sonkens, 2001).
The current study has shown that the standardized method of one single intramuscular PRP administration does not increase systemic IGF-1 levels and is therefore suggested as an ineffective means to gain systemic effects. This is in line with Creaney and Hamilton, 2008 who stated that PRP is unlikely to be a potent ergogenic aid because the unbound IGF-1 has too short a half-life to be able to exert systemic effects and the doses of IGF-1 in PRP are subtherapeutic in terms of producing systemic anabolic actions even without a delay in growth factor release as used in our study. Similarly, Volpi et al., 2010 concluded from their study, that PRP-based local therapy could influence systemic homeostasis and antidoping evaluations, but, in their opinion, does not represent a doping substance itself.
A limit of the study may be the small sample size and the use of IGF-1 measures only instead of various growth factors (Banfi et al., 2006). An additional limit may be the fact that the actual content of IGF-1 was not measured in our applied ACP product. Previous studies confirmed a 2-3 fold increased platelet concentration and increased growth factors including IFG-1 in the ACP product (unpublished white paper - Athrex®). Additionally, from our data it cannot be ruled out that a different metabolization may be evident in injured muscle tissue.
Conclusion
Several concerns regarding IGF-1 application such as a possible carcinogenetic effect and more importantly doping issues in athletes do exist. The PRP method offers some interesting aspects for the treatment of injured athletes to promote and accelerate the physiological healing process and functional recovery and effective from January 2011 a local intramuscular application is allowed by the WADA code.
Our data showed no increase of systemic IGF-1 levels after one single local intramuscular administration of PRP. Therefore, professional athletes and non-athletes alike can benefit from such a treatment option for muscle injuries and related sports injuries without an increased risk of cancer. However, more studies are warranted to provide definitive evidence to guide surgeon’s decision making regarding the appropriate use for PRP products.
Acknowledgements
The authors would like acknowledge the assistance of Julia Kröpfl for her statistic analysis.
Competing interests: Each author certifies that he has no commercial associations (e.g. consultancies, stock ownership, equity interest, patient/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted paper.
Funding: This study was supported by Arthrex® which is a company that markets a system for preparing PRP (ACP®) for therapeutic use.
Biographies

Gert Schippinger
Employment
Professor at Human Performance Research Graz, University and Medical University Graz, Private practice for trauma and orthopaedic surgery “Sportchirurgieplus”
Degree
MD, PhD
Research interest
oxidative stress, sports injury and biological treatment options, arthroscopic surgery
E-mail: gert.schippinger@uni-graz.at
Karl Oettl
Employment
Associate professor for physiological chemistry at the Institute for Physiological Chemistry, Medical University of Graz
Degree
Dr. rer.nat.
Research interest
Oxidative stress in exercise and disease, Albumin chemistry and function in liver disease, Analytics of physiologically and clinically relevant compounds
E-mail: karl.oettl@medunigraz.at

Florian Fankhauser
Employment
Private practice for trauma and orthopaedic surgery “Sportchirurgieplus” Lecturer for physiotherapy at FH Joanneum Graz
Degree
MD, PhD
Research interest
Oxidative stress, sports injury, arthroscopic surgery
E-mail: florian.fankhauser@sportchirurgieplus.at

Stefan Spirk
Employment
Student Assistant at Human Performance Research Graz, University Graz, Student of Sport Science, Institute of Sport Science University of Graz
Research interest
Sports injury, performance diagnostics and training
E-mail: s.spirk@uni-graz.at

Wolfgang Domej
Employment
Professor for Sport medicine at Human Performance Research Graz, University and Medical University Graz and Pulmonologist Clinical Department of Pulmonology
Degree
MD
Research interest
High-altitude physiology and medicine, hypoxic chamber technology, respiration at moderate to high altitude, high-altitudetolerance and intolerance, ergometry in hypoxic conditions, prae-acclimatisation and training under hypoxic conditions, chronic disease states and altitude exposure, expeditions medicine high-altitude pulmonary hypertension, hypoxic ventilatory and vascular response, chronic hypoxic vascular remodelling.
E-mail: wolfgang.domej@medunigraz.at

Peter Hofmann
Employment
Professor at Human Performance Research Graz, University and Medical University Graz and Institute of Sports Science, University of Graz
Degree
Dr. rer. nat.
Research interest
Exercise testing and performance diagnostics, exercise prescription and training
E-mail: peter.hofmann@uni-graz.at
References
- Anitua E., Andía I., Sanchez M., Azofra J., del Mar Zalduendo M., de la Fuente M., Nurden P., Nurden AT. (2005) Autologous preparations rich in growth factors promote proliferation and induce VEGF and HGF production by human tendon cells in culture. Journal of Orthopaedic Research 23(2), 281-286 [DOI] [PubMed] [Google Scholar]
- Arnoczky S.P., Anderson L., Fanelli G., Ho S., Mishra A., Scgalione N. (2009) The role of platelet-rich plasma in connective tissue repair. Orthopaedics Today 226, 29 [Google Scholar]
- Baltzer A.W., Moser C., Jansen S.A., Krauspe R. (2009) Autologous conditioned serum (Orthokine) is an effective treatment for knee osteoarthritis. Osteoarthritis and Cartilage 17, 152-160 [DOI] [PubMed] [Google Scholar]
- Banfi G., Corsi M.M., Volpi P. (2006) Could platelet rich plasma have effects on systemic circulating growth factors and cytokine release in orthopaedic applications? British Journal of Sports Medicine 40, 816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brabant G., von zur Mühlen A., Wüster C., Ranke M.B., Kratzsch J., Kiess W., Ketelslegers J.M., Wilhelmsen L., Hulthén L., Saller B., Mattsson A., Wilde J., Schemer R., Kann P. (2003) Serum insulin like Growth Factor 1 Reference Values for an Automated Chemiluminescence Immunoassay System: Results from a Multicenter Study. Hormone Research 60, 53-60 [DOI] [PubMed] [Google Scholar]
- Buhr M., Siekmann W. (2009) Intra-articular Injection of Platelet Rich Plasma for cartilage repair. Orthopädische Praxis 45(1), 10-16 [Google Scholar]
- Castricini R., Longo U.G., De Benedetto M., Panfoli N., Pirani P., Zini R., Maffulli N., Denaro V. (2011) Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. The American Journal of Sports Medicine 39, 258-265 [DOI] [PubMed] [Google Scholar]
- Chen B., Liu S., Xu W., Wang X., Zhao W., Wu J. (2009) IGF-1 and IGFBP-3 and the risk of lung cancer: A meta-analysis based on nested case-control studies. Journal of Experimental & Clinical Cancer Research 28, 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical power analysis for the behavioral sciences. 2ndedition Lawrence Erlbaum Associates [Google Scholar]
- Conway K., Price P., Harding K.G., Jiang W.G. (2006) The molecular and clinical impact of hepatocyte growth factor, its receptors, activators, and inhibitors in wound healing. Wound Repair and Regeneration 14, 2-10 [DOI] [PubMed] [Google Scholar]
- Creaney L., Hamilton B. (2008) Growth factor delivery methods in the management of sports injuries: the state of play. British journal of Sports Medicine 42, 314-320 [DOI] [PubMed] [Google Scholar]
- Engebretsen L., Steffen K., Alsousou J., Anitua E., Bachl N., Devilee R., Everts P., Hamilton B., Huard J., Jenoure P., Kelberine F., Kon E., Maffulli N., Matheson G., Mei-Dan O., Menetrey J., Philippon M., Randelli P., Schamasch P., Schwellnus M., Vernec A., Verrall G. (2010) IOC consensus paper on the use of platelet-rich plasma in sports medicine. British journal of Sports Medicine 44, 1072-1081 [DOI] [PubMed] [Google Scholar]
- Eppley B.L., Woodell J.E., Higgins J. (2004) Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plastic and Reconstructive Surgery 114(6), 1502-1508 [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A-G., Buchner A. (2007) G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39, 175-191 [DOI] [PubMed] [Google Scholar]
- Foster T.E., Puskas B.L., Mandelbaum B.R., Gerhardt M.B., Rodeo S.A. (2009) Platelet-rich plasma: from basic science to clinical applications. The American Journal of Sports Medicine 37, 2259-2272 [DOI] [PubMed] [Google Scholar]
- Griffin X.L., Smith C.M., Costa M.L. (2009) The clinical use of platelet rich plasma in the promotion of bone healing: A systematic review. Injury 40, 158-162 [DOI] [PubMed] [Google Scholar]
- Grimberg A., Cohen P. (2000) Role of insulin-like growth factors and their binding proteins in growth control and carcinogenesis. Journal of Cellular Physiology 183, 1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimberg A. (2003) Mechanisms by which IGF-1 may promote cancer. Cancer Biology & Therapy 2, 630-635 [PMC free article] [PubMed] [Google Scholar]
- Kasemkijwattana C., Menetrey J., Bosch P., Somogyi G., Moreland MS., Fu F.H., Buranapanitkit B., Watkins S.S., Huard J. (2000) Use of growth factors to improve muscle healing after strain injury. Clinical Orthopaedics and Related Research 370, 272-285 [DOI] [PubMed] [Google Scholar]
- Lann D., LeRoith D. (2008) The role of endocrine insulin-like growth factor-1 and insulin in breast cancer. Journal of Mammary Gland Biology and Neoplasia 13, 371-379 [DOI] [PubMed] [Google Scholar]
- LeRoith D., Roberts C.T. (2003) The Insulin-like growth factor system and cancer. Cancer Letters 195, 127-137 [DOI] [PubMed] [Google Scholar]
- Lopez-Vidriero E., Goulding K.A., Simon D.A., Sanchez M., Johnson D.H. (2010) The use of platelet-rich plasma in arthroscopy and sports medicine: optimizing the healing environment. Arthroscopy 26, 269-278 [DOI] [PubMed] [Google Scholar]
- Marx R.E. (2004) Platelet-rich plasma: evidence to support its use. J Oral and Maxillofacial Surgery 62, 489-496 [DOI] [PubMed] [Google Scholar]
- Mishra A., Pavelko T. (2006) Treatment of chronic elbow tendinosis with buffered platetelet-rich plasma. The American Journal of Sports Medicine 34, 1774-1778 [DOI] [PubMed] [Google Scholar]
- Philippou A., Maridaki M., Halapas A., Koutsilieris M. (2007) The role of insulin-like growth factor 1(IGF-1) in skeletal muscle physiology. In Vivo 21, 45-54 [PubMed] [Google Scholar]
- Ranly D.M., Lohmann C.H., Andreacchio D., Boyan BD., Schwartz Z. (2007) Platelet rich plasma inhibits demineralized bone matrix-induced bone formation in nude mice. The Journal of Bone And Joint Surgery. American Volume 89, 139-146 [DOI] [PubMed] [Google Scholar]
- Renehan A.G., Zwahlen M., Minder C., O’Dwyer S.T., Shalet S.M., Egger M. (2004) Insulin-like growth factor (IGF)-1, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 363, 1346-1353 [DOI] [PubMed] [Google Scholar]
- Rowlands M.A., Gunnell D., Harris R., Vatten L.J., Holly J.M., Martin R.M. (2009) Circulating insulin-like growth factor peptides and prostate cancer risk: a systematic review and meta-analysis. International Journal of Cancer 124, 2416-2429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez M., Anitua E., Azofra J., Andía I., Padilla S., Mujika I. (2007) Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. The American Journal of Sports Medicine 35, 245-251 [DOI] [PubMed] [Google Scholar]
- Sanchez M., Anitua E., Cugat R., Azofra J., Guadilla J., Seijas R., Andia I. (2009a) Nonunions treated with autologous preparation rich in growth factors. Journal of Orthopaedic Trauma 23, 52-59 [DOI] [PubMed] [Google Scholar]
- Sánchez M., Anitua E., Orive G., Mujika I., Andia I. (2009b) Platelet-rich therapies in the treatment of orthopaedic sport injuries. Sports medicine 39, 345-354 [DOI] [PubMed] [Google Scholar]
- Saugy M., Robinson N., Saudan C., Baume N., Avois L., Mangin P. (2006) Human growth hormone doping in sport. British Journal of Sports Medicine 40, 35-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonksen P.H. (2001) Insulin, growth hormone and sport. The Journal of endocrinology 170, 13-25 [DOI] [PubMed] [Google Scholar]
- Stay J.J., Terrell T.R., Armsey T.D. (2004) Ergogenic aids: human growth hormone. Current Sports Medicine Reports 3, 229-233 [DOI] [PubMed] [Google Scholar]
- Tentori L., Graziani G. (2007) Doping with growth hormone/IGF-1, anabolic steroids or erythropoietin: is there a risk? Pharmacological Research 55, 359-369 [DOI] [PubMed] [Google Scholar]
- WADA (2011) The 2011 Prohibited List World Anti-Doping Code. Available from URLhttp://www.wada-ama.org/Documents/ World_Anti-Doping_Program/WADP-Prohibited-list/To_be_ effective/WADA_Prohibited_List_2011_EN.pdf
- WADA (2008) World Anti-Doping Agency. Available from URL: http://www.wada-ama.org(accessed 2008 Mar 16).
- Volpi P., Quaglia A., Schoenhuber H., Melegati G., Corsi M.M., Banfi G., de Girolamo L. (2010) Growth factors in the management of sport-induced tendinopathies: results after 24 months from treatment. A pilot study. The Journal of Sports Medicine and Physical Fitness 50, 494-500 [PubMed] [Google Scholar]
- Wright-Carpenter T., Opolon P., Appell H.J., Meijer H., Wehling P., Mir LM. (2004) Treatment of muscle injuries by local administration of autologous conditioned serum: animal experiments using a muscle contusion model. International Journal of Sports Medicine 25, 582-587 [DOI] [PubMed] [Google Scholar]
- Yokota K., Ishida O., Sunagawa T., Suzuki O., Nakamae A., Ochi M. (2008) Platelet-rich plasma accelerated surgical angiogenesis in vascular implanted necrotic bone: an experimental study in rabbits. Acta Orthopaedica 79, 106-110 [DOI] [PubMed] [Google Scholar]


