Abstract
Objectives
Occupational noise-induced hearing loss (NIHL) is prevalent, yet evidence on the effectiveness of preventive interventions is lacking. The effectiveness of a new technology allowing workers to monitor daily at-ear noise exposure was analysed.
Methods
Workers in the hearing conservation program of an aluminium smelter were recruited because of accelerated rates of hearing loss. The intervention consisted of daily monitoring of at-ear noise exposure and regular feedback on exposures from supervisors. The annual rate of change in high frequency hearing average at 2, 3 and 4 KHz before intervention (2000–2004) and 4 years after intervention (2006–2009) was determined. Annual rates of loss were compared between 78 intervention subjects and 234 controls in other company smelters matched for age, gender and high frequency hearing threshold level in 2005.
Results
Individuals monitoring daily noise exposure experienced on average no further worsening of high frequency hearing (average rate of hearing change at 2, 3 and 4 KHz=–0.5 dB/year). Matched controls also showed decelerating hearing loss, the difference in rates between the two groups being significant (p<0.0001). Analysis of a subset of intervention subjects matched to controls for initial rate of hearing loss showed a similar trend but the difference was not statistically significant (p=0.06).
Conclusion
Monitoring daily occupational noise exposure inside hearing protection with ongoing administrative feedback apparently reduces the risk of occupational NIHL in industrial workers. Longer follow-up of these workers will help determine the significance of the intervention effect. Intervention studies for the prevention of NIHL need to include appropriate control groups.
BACKGROUND
Noise is one of the most prevalent occupational hazards, and noise-induced hearing loss (NIHL) is one of the most common occupational diseases.1 Despite widespread implementation of hearing conservation programs in workplaces over recent decades, NIHL continues to occur in noise-exposed workforces. The 1983 Occupational Safety and Health Administration (OSHA) occupational noise standard requires that employers enrol workers in hearing conservation programs when ambient noise exposures are at or above 85 dBA (8 h time weighted average (TWA)).2 Such programs consist of administrative controls, engineering controls, training, annual audiometry and the personal use of hearing protection devices.3
Despite the existence of mandated hearing conservation programs, there is a lack of evidence that interventions to prevent occupational NIHL are effective.4 One of the challenges to effective hearing conservation is that the actual attenuation provided by hearing protectors in real world settings varies greatly between individuals and may not correlate well with manufacturer’s listed noise reduction ratings.5 In addition, there is evidence that in many noise exposure situations, hearing protection devices are under-used.6 Recent studies in industry have shown that hearing loss rates in areas of moderate noise may be higher than in areas of higher ambient noise, suggesting a differential use of hearing protectors between the two environments.7 Therefore, the actual noise dose that workers are receiving on a daily basis is not known, and many cases of NIHL are only detected after significant loss has already occurred.
Recent advances in hearing protector technology include the development of a device to monitor noise exposures inside hearing protectors, and to record such noise data on a daily basis (K Michael, personal communication, 2009). However, whether daily monitoring of noise exposure is an effective means of preventing occupational hearing loss remains unclear.
We report on an analysis of the hearing loss experience of a cohort of industrial workers who are enrolled in a mandatory program to perform daily noise exposure monitoring inside their hearing protection devices. The purpose of the analysis was to determine whether the users of the devices were experiencing less hearing loss than control workers not enrolled in the mandatory program.
METHODS
Alcoa Inc. is a worldwide producer of aluminium and other industrial products. In Alcoa locations in the USA, hearing conservation programs have been in place since the late 1970s or earlier. Research collaboration agreements between Alcoa, Yale University School of Medicine and Stanford School of Medicine have resulted in ongoing analysis of audiometric data collected for hearing conservation purposes that has been previously described.8 Research protocols to analyse these audiometric data have been reviewed and approved by Yale University School of Medicine Human Investigations Committee as well as the Institutional Review Board of Stanford School of Medicine. In 2005, an Alcoa smelter located in the USA initiated a mandatory program requiring workers who were demonstrating excessive hearing loss in the audiometric monitoring program to wear hearing protection devices fitted with a dosimeter attached to a microphone capable of measuring noise exposures inside the hearing protection. The program’s definition of excessive loss was an audiometric shift from baseline of at least 5 dB in the average of hearing thresholds at 2, 3 and 4 KHz in either ear, after age correction. Each worker enrolled in this program was expected to use the dosimetry device to monitor noise exposure on a daily basis. The dosimeter can be fitted into either earplugs or earmuffs. In order to record daily noise ‘dose’, the dosimeters were set to a 5 dB exchange rate, slow response, 100% dose of 90 dBA and 80 dBA noise floor. At the end of the work shift, the worker placed the dosimeter in the cradle of an infrared reading device connected to a computer terminal that would store the time-weighted daily noise dose (as a percentage of the 90 dBA permissible exposure limit (PEL)) and also display the dose result on a computer screen available to the worker. Since Alcoa policy specifies 85 dBA as the corporate occupational exposure level for Alcoa workers, workers were instructed to keep recorded doses to less than 50% dose (85 dBA). In addition, each dosimeter was equipped with a visual warning signal that turns yellow when daily cumulative dose exceeds 45% dose (84 dBA), flashes red when short term exposures are over 85 dBA, and remains a constant red when daily cumulative dose exceeds 100% (90 dBA). In addition to the worker receiving feedback about daily noise exposures, the worker’s supervisor regularly reviews both the recorded noise exposures as well as the completeness of recording of the noise data, with a goal of 100% compliance. Since the workers using the devices are enrolled in the hearing conservation program, they receive annual surveillance audiometry. We performed a retrospective analysis of the hearing loss experience of these individuals before and after being enrolled in this mandatory noise exposure monitoring program. SAS v 9.01 was used for all statistical analyses including the matching of intervention subjects and controls.
Selection of intervention subjects
Using the Alcoa audiometric database for the location where the intervention took place, we selected for this analysis workers at the smelter facility who began use of the daily noise exposure monitor device in 2005, and who had at least three audiometric tests in the surveillance database in 2000–2004 and at least three audiometric tests in 2006–2009. In 2005, 138 workers were fitted with the daily exposure monitoring devices. Eighty of these workers met the above criteria for analysing their hearing loss experience.
Selection of controls
Controls were selected from workers among seven other Alcoa smelter locations who had audiograms as part of the hearing conservation program during the same historical period. Controls were not selected from the same facility as the intervention subjects to avoid facility-wide effects of the monitoring programs. The control selection process involved searching the Alcoa audiometric database for the records of individuals included in the hearing conservation programs of these smelters during the same time period. For each intervention subject we selected three control subjects who matched on age (within 5 years), gender and high frequency hearing threshold level (binaural average of 2, 3 and 4 KHz) (within 5 dB) in 2005. Through this process we were able to match 78 of the subjects to 234 controls.
To assess any possible effect of regression to the mean occurring in subjects who had been selected due to high initial rates of hearing loss, we performed two additional analyses. The first was to determine, within the 80 intervention subjects, whether the annual rate of hearing loss (annual rate of change in the binaural average of 2, 3 and 4 KHz, in dB/year) during the pre-intervention period was a significant predictor of subsequent rate of hearing loss in the post-intervention period. In a multivariate regression controlling for age, hearing level and gender, no significant association was found between rate of hearing loss during the pre-intervention period and post-intervention rate of hearing loss (p=0.74). As an additional check for possible regression to the mean effect, we performed a sub-analysis matching on initial rate of hearing loss during the pre-intervention period. This was done by dividing the initial rates into quintiles and matching each intervention subject to a control with an initial hearing loss rate from the same quintile, matching as well on age, gender and hearing level as before. With these criteria we were able to match 46 of the intervention subjects to 138 controls. We performed subsequent analyses using both the larger group of subjects and matched controls and the more highly matched subgroup.
Rates of hearing loss
For each audiogram performed on intervention subjects and controls, we calculated the average binaural high frequency hearing levels at the noise-sensitive frequencies that are tracked in OSHA hearing conservation programs (2, 3 and 4 KHz).9 We then calculated for each intervention subject and control individual the annual rate of hearing loss (in dB/year) by performing a linear regression of audiometric results performed over 2000–2004 and 2006–2009 for each individual. We then compared the difference between the pre-intervention rates and the post-intervention rates for both the intervention and control subjects using a difference-in-difference analysis, as shown in the following equation:
where R is the annual rate of hearing loss, I and C are the intervention subjects and controls, Post is the post-intervention time period (2006–2010), and Pre is the pre-intervention time period (2000–2004). The statistical significance of the difference between the groups was assessed using a t test.
Calculation of ambient noise exposure and noise exposure inside the hearing protection
Alcoa routinely performs noise exposure assessments for noisy areas in facilities, and these noise measurements are entered into an industrial hygiene database which allows linkage of particular job titles to noise exposures in a job exposure matrix. We used this job exposure matrix to calculate the mean TWA ambient (outside the hearing protection) noise exposure for workers in the study (both intervention subjects and controls), by calculating a work history for each worker and then assigning them an ambient noise exposure based on the job exposure matrix. These methods have been described previously.7 Median ambient noise exposures during 2001–2004 and 2006–2009 were calculated for 68 of the intervention subjects and 166 controls whose jobs could be linked to noise measurements in the company industrial hygiene database.
For the 80 intervention subjects, we used the daily noise monitoring records to calculate the median daily noise exposure over the intervention period for each individual, and then determined the median and range of noise exposures for the intervention group as a whole.
RESULTS
Demographics
Table 1 shows the demographics of the study subjects and 234 controls matched on age, 2005 hearing level and gender, as well as the overall population of smelter workers from which the controls were drawn. As can be seen, the average age and years of previous employment indicate that a number of workers had substantial prior exposure to occupational noise at the initiation of intervention. There were no significant differences between intervention subjects and controls for age, gender and duration of employment in the smelters. There was a higher percentage of Hispanic ethnicity among intervention subjects compared to controls. Controls had higher reported rates of hunting and/or shooting compared to controls. Compared to the general worker population, both the intervention subjects and the controls were slightly older and exhibited higher average hearing thresholds.
Table 1.
Characteristics of intervention subjects and controls
| Characteristic | Intervention subjects (N=78) | Workers in seven other smelters (N=2210) | Matched controls (N=234) |
|---|---|---|---|
| Age (mean, SD) | 48.7 (7.2) | 46.7 (8.2) | 48.6 (7.5) |
| Male (n, %) | 78 (100.0) | 2045 (92.5) | 234 (100.0) |
| Race (n, %) | |||
| White | 69 (88.5) | 1873 (84.8) | 224 (95.7) |
| Hispanic | 6 (7.7) | 37 (1.7) | 5 (2.1) |
| American Indian/Alaska native | 2 (2.6) | 20 (0.9) | 2 (1.0) |
| Asian | 1 (1.3) | 6 (0.3) | 0 (0.0) |
| African American | 0 (0.0) | 274 (12.4) | 3 (1.3) |
| Tenure (mean, SD) | 22.5 (9.9) | 18.5 (10.5) | 20.6 (10.4) |
| History of shooting (n, %) | 30 (38.5) | 904 (40.9) | 113 (48.3) |
| Hearing at start of intervention (mean, SD) | |||
| Average 2–4 KHz | 28.2 (13.4) | 20.5 (15.1) | 28.2 (13.6) |
Rates of hearing loss
Table 2 shows the rate of hearing loss in the binaural average hearing level at 2, 3 and 4 KHz (in dB/year) for the 80 intervention subjects. The rate of annual hearing loss declined markedly between the pre-intervention and post-intervention time periods. When the 78 intervention subjects are compared to 234 controls from similar facilities, matched on age, gender and hearing level, it can be seen that there was some deceleration in the rate of loss in both groups between the pre- and post-intervention time periods. Despite this similarity, the difference in hearing loss rates between the pre-intervention and post-intervention time periods was significantly greater for the intervention subjects (p<0.0001). For the subgroup of 46 intervention subjects and 138 controls who could be matched on age, gender, 2005 hearing level and annual rate of hearing loss during the pre-intervention time period; rates of hearing loss for both intervention subjects and controls improved during the second time period, with a trend towards greater improvement in the intervention group (p=0.06).
Table 2.
Average rate of hearing loss (dB/year) before and after initiation of daily noise exposure monitoring
| Intervention group
|
Control group
|
Difference in difference* | p Value | |||||
|---|---|---|---|---|---|---|---|---|
| No. | Before | After | No. | Before | After | |||
| All intervention subjects | 80 | 1.7 (1.3) | −0.5 (1.9) | |||||
| Matched on age, gender, baseline hearing | 78 | 1.8 (1.3) | −0.4 (1.5) | 234 | 0.4 (1.1) | −0.1 (2.1) | 1.7 | <0.0001 |
| Matched on age, gender, baseline hearing and initial rate of hearing loss | 46 | 1.4 (1.5) | −0.2 (1.6) | 138 | 1.1 (1.1) | 0.45 (1.45) | 1.0 | 0.06 |
Difference in the difference between the pre-intervention (2000–2004) and post-intervention time periods (2006–2010).
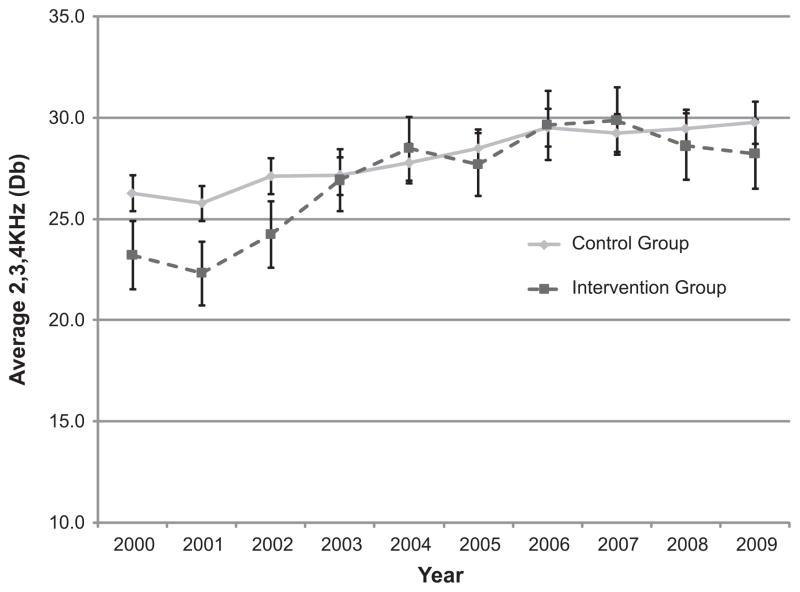
Figure 1 graphically depicts the annual median of hearing thresholds for the frequencies of 2, 3 and 4 KHz for 78 intervention subjects and 234 matched controls. The controls showed a gradual worsening of yearly average thresholds, while the intervention subjects demonstrated a levelling off of annual average thresholds after initiation of the intervention.
Figure 1.
Median high frequency hearing threshold levels for intervention subjects (N=78) and matched controls (N=234) before and after initiation of daily noise exposure monitoring.
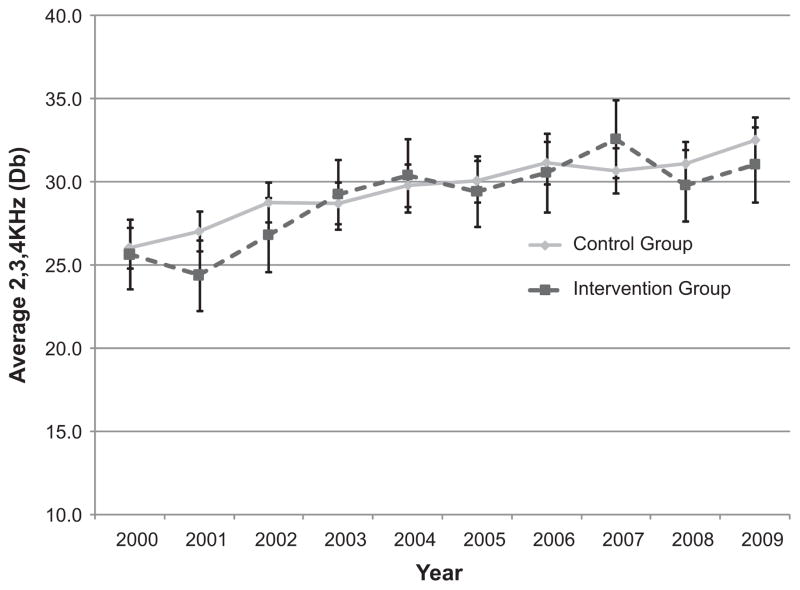
Figure 2 shows the annual median hearing thresholds for the subgroup matching on initial rate of hearing loss. Again, the controls show gradual worsening of hearing thresholds while the intervention subjects show a levelling off. The difference between the intervention group and controls appears less distinct in this matched analysis.
Figure 2.
Median high frequency hearing threshold levels for intervention subjects (N=46) and controls (N=138) matched on initial rate of hearing loss.
Calculated noise exposures
The median of ambient (ie, outside hearing protection) noise measurements for the jobs of the 68 intervention subjects who could be linked to company industrial hygiene noise exposure assessments was 86.6 dBA (IQR 75.3–88.4) during the pre-intervention period, and 86.6 dBA (IQR 74.7–88.4) during the post-intervention period. This indicates that among the post-intervention group, there was no evidence of selective out-migration from heavily exposed jobs. The pre-intervention median ambient noise levels for the 158 controls who could be linked to company industrial hygiene records was 80.9 dBA (IQR 79.1–85.1) between 2001 and 2004, and 80.6 dBA (IQR 79.2–84.9) during the post-intervention period between 2006 and 2009.
For the 80 intervention subjects, the median of individual median noise exposures (assessed on a daily basis inside hearing protection) over the intervention period was 74.7 dBA (IQR 69.7–78.0).
DISCUSSION
The results of this study indicate that daily use by industrial workers of devices that monitor noise exposure inside their hearing protection and that make the results of these daily noise dose measurements available to both workers and their supervisors may decrease occupational hearing loss risk. Since hearing loss develops gradually over time, further follow-up of this cohort can help confirm the significance of the intervention effect.
There are a number of reasons why daily noise exposure monitoring could be effective in preventing occupational hearing loss. Workers who are regularly alerted to their true occupational noise exposures can play an active role in optimising their use of hearing protection devices to reduce such exposures, such as using hearing protection more consistently and more effectively, as well as avoiding excessively loud noise sources. Making company personnel aware of employee noise exposures on a daily basis could result in such persons identifying and taking steps to reduce sources of excessive noise exposure. While our data suggest that daily noise monitoring intervention with at-ear noise exposure assessment may be effective in reducing hearing loss, there may be alternative technological ways (in addition to at-ear noise exposure monitoring) to achieve the same result, such as ambient dosimeters with warning devices worn on the shoulder to alert workers to excessive noise exposures. Further research on such approaches to determine the relative effectiveness of different program components appears warranted.
Since this study was an observational analysis, it is possible that other factors could explain the observed results. If workers who began using the daily noise exposure monitoring devices migrated to less noisy jobs, their risk of subsequent hearing loss might be expected to decrease. However, the estimated ambient noise exposures for the intervention subjects before and after the initiation of daily monitoring did not indicate substantial evidence of such out-migration from noisy jobs.
For the subjects who wore the daily noise exposure devices, the calculated average rate of hearing in the binaural average of 2, 3 and 4 KHz during the post-intervention period actually demonstrated improvement of 0.5 dB/year. Since surveillance audiograms were used to calculate these hearing rates, and such audiograms are typically performed during work shifts without allowing the ear a rest period in quiet, we believe that one likely explanation for the observed ‘improvement’ in hearing thresholds could be a reduction in the degree of temporary hearing threshold shifts due to improved consistent noise exposure reduction.
A possible explanation for the reduced rate of hearing loss during the post-intervention period (in both intervention subjects and controls) is the previously reported observation that the rate of NIHL in exposed workers is greatest in the first 10–15 years of exposure, and decelerates after that.9 The workers using the devices had a history of previous noise exposure. Therefore it is possible that some portion of the observed deceleration in yearly loss could be due to the fact that their NIHL was already slowing. This could help explain why the matched controls also demonstrated a deceleration of hearing loss rates during 2006–2009. Another possible reason for the observed reduction in hearing loss rates during 2006–2009 is that conventional interventions through their hearing conservation program, such as counselling, retraining and refitting of hearing protectors, could have been exhibiting a beneficial effect. An additional factor could be the statistical phenomenon of regression to the mean, whereby for some of the individuals selected based on their rapid rate of hearing loss, their observed hearing loss could have been due to random measurement error, and they would then be expected to regress to the mean hearing loss experience of the rest of the population with subsequent measurements. Even in the presence of these effects that could obscure a beneficial effect of the intervention, a statistically significant difference in hearing loss rates was observed between intervention subjects and controls, arguing strongly for the effectiveness of the intervention. When a subgroup of the intervention subjects was matched with controls based on the initial rate of hearing loss in the pre-intervention period, the intervention group still showed less hearing loss than controls, but the difference between the rates of hearing loss for the two groups during the subsequent time period was less distinct and did not reach statistical significance. This implies that some (but not all) of the observed difference in hearing loss rates between intervention and control groups was probably related to the statistical phenomenon of regression of the mean. This further demonstrates the need for careful selection of controls in intervention studies of this type.
Another reason for the observed difference in hearing loss rates between intervention subjects and controls could be confounding effects of other covariates, such as exposure to ototoxic chemicals or non-occupational noise. Indeed, the reported rate of hunting and/or shooting was slightly higher in the control subjects. However, when intervention subjects and controls were matched on reported hunting and shooting status (as well as age, gender and 2005 hearing loss), this matching did not affect the study results. Additionally, the fact that controls were drawn from similar industrial facilities (aluminium smelters) and were similar to intervention subjects in age, work tenure and baseline hearing level, makes such confounding less likely (although still possible). In terms of ototoxic exposures, both intervention subjects and controls worked in aluminium smelters where exposures to solvents and other ototoxic chemicals did not appear to be significant. Therefore, the weight of the evidence from this study appears to support the protective effect of the daily noise exposure monitoring intervention on rates of NIHL.
There are limits to generalising the results of this study. The workers selected for the intervention tended to be older and with worse baseline hearing than the general population of noise exposed workers, and it is possible that different effects would be seen in other populations. An important aspect of the intervention is that participation in the daily noise exposure monitoring program was mandatory at the intervention location, and that supervisors were aware of the daily noise doses of the workers. It is possible, therefore, that other factors besides use of the monitoring device could explain the impact on hearing loss risk. These factors could include greater involvement of supervisors in the hearing conservation program, and other changes in work practice associated with the program. It is furthermore difficult to generalise the effectiveness of a mandatory program to a setting where the use of such devices would be voluntary. An intervention effectiveness trial of voluntary use of the daily noise exposure monitoring devices is currently underway. If additional controlled (and ideally randomised) trials of this type confirm the promising effect of daily noise exposure monitoring seen in this observational study, it could open up important new possibilities for the prevention of NIHL.
What this paper adds.
Occupational noise-induced hearing loss is one of the most prevalent occupational conditions, yet evidence, such as controlled intervention trials, regarding the efficacy of preventive measures is lacking.
This paper analyses the effectiveness of an intervention to prevent occupational hearing loss using a novel technology allowing daily monitoring of noise exposure inside hearing protection.
Over a 4-year period, workers with progressive hearing loss who used the monitoring devices showed, as a group, no further deterioration in hearing; control subjects also showed improving rates of hearing loss, but did not improve as much as the workers using the devices.
These results from one of the first controlled intervention studies for the prevention of noise-induced hearing loss indicate that daily noise exposure monitoring inside hearing protection may prevent further progression of hearing loss in industrial workers, and also show the importance of selecting appropriate controls for such intervention studies.
Acknowledgments
The authors wish to thank Rhonda Wilkinson for her work implementing this intervention program.
Funding This work was supported by the National Institute for Occupational Safety and Health, grant no. 1 R01 OH008641-01A2.
Footnotes
Competing interests Several of the authors (PMR, DG, SRK, MDS, MRC) provide consultant services to Alcoa Inc. One author (CDE) serves as the corporate audiologist for Alcoa Inc.
Ethics approval This study was conducted with the approval of the Yale Human Investigation Committee (HIC), Yale University School of Medicine, and the Institutional Review Board of Stanford University.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Tak S, Calvert GM. Hearing difficulty attributable to employment by industry and occupation: an analysis of the National Health Interview Survey–United States, 1997 to 2003. J Occup Environ Med. 2008;50:46–56. doi: 10.1097/JOM.0b013e3181579316. [DOI] [PubMed] [Google Scholar]
- 2.Occupational Safety and Health Administration, OSHA; Labor USDo, editor. 1910.95 CFR. 48 Federal Register. 1983. Occupational Noise Exposure: Hearing Conservation Amendment (Final Rule) pp. 9738–85. [Google Scholar]
- 3.American College of Occupational and Environmental Medicine. The Role of the Professional Supervisor in the Audiometric Testing Component of Hearing Conservation Programs. Position Paper. Illinois: American College of Occupational and Environmental Medicine; 2007. [accessed 1 Jun 2010]. http://www.acoem.org/guidelines.aspx?id=3050b. [DOI] [PubMed] [Google Scholar]
- 4.Verbeek JH, Kateman E, Morata TC, et al. Interventions to prevent occupational noise induced hearing loss. Cochrane Database Syst Rev. 2009;(3):CD006396. doi: 10.1002/14651858.CD006396.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Berger EH, Franks JR, Behar A, et al. Development of a new standard laboratory protocol for estimating the field attenuation of hearing protection devices. Part III. The validity of using subject-fit data. J Acoust Soc Am. 1998;103:665–72. doi: 10.1121/1.423236. [DOI] [PubMed] [Google Scholar]
- 6.Tak S, Davis RR, Calvert GM. Exposure to hazardous workplace noise and use of hearing protection devices among US workers–NHANES, 1999–2004. Am J Ind Med. 2009;52:358–71. doi: 10.1002/ajim.20690. [DOI] [PubMed] [Google Scholar]
- 7.Rabinowitz PM, Galusha D, Dixon-Ernst C, et al. Do ambient noise exposure levels predict hearing loss in a modern industrial cohort? Occup Environ Med. 2007;64:53–9. doi: 10.1136/oem.2005.025924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabinowitz PM, Slade M, Dixon-Ernst C, et al. Impact of OSHA final rule—recording hearing loss: an analysis of an industrial audiometric dataset. J Occup Environ Med. 2003;45:1274–80. doi: 10.1097/01.jom.0000100040.45929.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Occupational and Environmental Medicine. ACOEM evidence based statement: noise-induced hearing loss. J Occup Environ Med. 2003;45:579–81. doi: 10.1097/00043764-200306000-00001. [DOI] [PubMed] [Google Scholar]