Abstract
Objective:
The research sought to determine the effect of a clinical medical librarian (CML) on outcomes of in-patients on the internal medicine service.
Methods:
A prospective study was performed with two internal medicine in-patient teams. Team 1 included a CML who accompanied the team on daily rounds. The CML answered questions posed at the point of care immediately or in emails post-rounds. Patients on Team 2, which did not include a CML, as well as patients who did not require consultation by the CML on Team 1, served as the control population. Numerous clinical and library metrics were gathered on each question.
Results:
Patients on Team 1 who required an answer to a clinical question were more ill and had a longer length of stay, higher costs, and higher readmission rates compared to those in the control group. Using a matched pair analysis, we showed no difference in clinical outcomes between the intervention group and the control group.
Conclusions:
This study is the largest attempt to prospectively measure changes in patient outcomes when physicians were accompanied by a CML on rounds. This approach may serve as a model for further studies to define when and how CMLs are most effective.
Highlights.
Physicians have more queries for a clinical medical librarian (CML) when the patient has more complex medical problems.
The research provides a detailed description of how a CML can function in a medical team and identifies team members most likely to ask questions that require a CML's searching abilities.
The most frequently used resources to answer clinical questions were PubMed, followed by Access Medicine and MD Consult.
No difference was found in clinical outcomes between the intervention group and the control group.
Implications.
A CML can be most effective by rounding with those physicians who see the more complex medical problems (severe diseases and high number of secondary diagnoses).
It is difficult to compare the effects of CML intervention, because so many variables outside the CML's control are involved. These include the physician's utilization of the literature, the physician's level of competence, the uniqueness of each patient, and the practice setting.
Although difficult to implement, further research addressing the impact of a CML on patient outcomes would likely benefit from a more sophisticated study design compared to the case-control study undertaken here.
INTRODUCTION
Physicians have long been aware of the need to optimize care of their patients by searching the medical literature. At one time, doctors searched for publications addressing a specific clinical question through the laborious review of the monthly issues and yearly volumes of the Index Medicus. Yet, computerization of the searching process in 1970 brought new challenges 1. Although many physicians knew the question that they wanted answered, they were now required to first become computer literate and then learn computer search methods. In addition, research by Ely et al. has shown that some clinicians fail to pursue the answers to their own questions that may make a difference in providing better patient care 2, 3.
In the mid-1970s, the clinical medical librarian (CML) emerged to help clinicians quickly find information for the care of their patients 4–8. Physicians who worked with a CML recognized that the CML could help them find the information that they wanted, increase their knowledge of medical advances, and save them time 9. In the 1990s, libraries became fully computerized. CML services grew as the need for computer skills increased and the relevance of evidence-based medicine (EBM) and evidence-based practice (EBP) became increasingly recognized 10, 11. During this decade, it is the authors' perspective that the prevalence of CMLs expanded due to two educational initiatives. First, the Association of American Medical Colleges (AAMC) formally recognized that physicians must engage in lifelong learning 12. Second, the Accreditation Council for Graduate Medical Education (ACGME) developed the competency, “practice based learning and improvement,” for all physicians in training 13. As opposed to the time when the Index Medicus was in use, librarians now typically organize educational programs and serve as key teachers for medical students in computerized searching, EBM, and often critical analysis. In the literature, the CML has been recognized by residents and physicians as an expert in searching for clinical answers using electronic resources 14–17.
In spite of the presumed benefit to physicians and students of a CML, the evidence for the effects of the presence of a CML on patient care outcomes is not clear. A 2004 systematic review noted that studies involving CML services rarely addressed specific outcomes such as readmission rates, hospital or physician costs, mortality, or length of stay 18. A more recent systematic review determined that very few studies have even collected survey data on the impact of CML services 19. The first prospective study of CMLs to utilize outcomes as a measurement was reported in 1994. It showed that a literature search conducted early in the hospitalization of a relatively small population of patients resulted, on average, in lower charges and a shorter mean length of stay 20. A second report published in 2007 measured the effects of the CML in providing information on a series of patients presented in a department of medicine's morning report 21. Immediately following the presentation of a newly admitted patient, a librarian, along with the department chair or chief resident, conducted a search of the medical literature to address questions regarding the care of the patient. The information was then provided to the house officers providing care. This study concluded that “presentation of a case at morning report, followed by the timely dissemination of the results of an online literature review, resulted in a shortened length of stay and lower hospital charges compared with controls” 21. Yet, one of the recognized limitations of that report was the limited number of matched patients.
Seeking to provide further insight into the value of a CML working with physicians providing in-patient care, the Louisiana State University (LSU) Health Shreveport Departments of Medical Library Science and Medicine began a study to determine whether having a CML embedded in the ward team to answer questions posed by care providers affected the length of stay, cost of care, or readmission rate of the hospitalized patients.
METHODS
Hospital setting
LSU Health Shreveport is an urban medical campus serving northwest Louisiana. The hospital has 459 beds with more than 125,300 annual in-patient days. The patient population is primarily indigent and underprivileged. The Medical Library is an academic department in the School of Medicine and serves as the principal information resource for the School of Medicine, the University Hospital, the School of Graduate Studies, and the School of Allied Health Professions. In 2004, the Medical Library collaborated with the Department of Medicine to implement a morning report program 21. This collaboration led to the hiring of a full-time CML, funded through and based in the Department of Medical Library Science. A major role of the CML was to help address the Department of Medicine's informational needs.
Prior to beginning this current study, the library had fifteen faculty positions and operated on a traditional model with departments such as reference, user education, technical services, and information technology. The position of CML was filled in October 2007. The hired CML had more than twelve years of experience as a librarian, four of these as a hospital librarian serving on multidisciplinary teams addressing trauma, neurology, and cardiovascular information needs. The CML fully participated in morning rounds Monday through Friday, alternating between those two (of five) internal medicine (IM) teams (referred to as Team 1 and Team 2, below) that included American Board of Internal Medicine certified physicians. A possibly unique feature of this CML's position was access to the electronic medical records of the patients seen by the teams. Because the CML was involved in “health care operations activities” and part of the “related services” in the health care team, the policy of the Office of Civil Rights in the Department of Health and Human Services allowed access to medical information of the patients hospitalized on the ward team 22. The CML reviewed patient records prior to rounds and brought new patient information to the team for discussion.
Each team conducting rounds with the CML was typically composed of a faculty attending physician, a second- or third-year resident, and 2 interns. Often, 1 to 2 medical students joined the team for 2 weeks at a time, and sometimes, at the discretion of the Pharmacy School, a pharmacist, pharmacy fellows, or pharmacy students joined the team for 1 or 2 weeks. Rounds were made daily and involved the presentation of patient care information by a house officer or medical student to the attending faculty member, usually followed by the examination of the patient. The initial presentation typically included an assessment of the clinical symptoms that prompted the patient's arrival at the hospital, the patient's medical history and physical findings, basic management needs for the care of the patient (medications, etc.), and diagnostic tests to be scheduled. Daily, or more often as needed, the faculty member reviewed the recent events in the care of the patient, clinically assessed the patient, and acted on the collected information to develop a plan for care. Rounds usually began around 9:00 a.m. and ended by noon.
Experimental design
A 2-armed prospective interventional study was designed to evaluate the effect of intervention by the CML on patient outcomes within a single institution. The required number of study patients in the population was based on projections of primary outcome (i.e., difference in length of stay between the comparison and intervention groups). A sample size of 253 patients in each group was estimated to have 80% power to detect a difference in means for length of stay of 1.5 days or of a 20% change (the difference between a comparison group mean of 7.5 days and an intervention group mean of 6.0 days), assuming that the common standard deviation was 6.0, using a 2-group t-test with a 0.050 2-sided significance level.
The proposal, “The Effect of a Clinical Medical Librarian on Internal Medicine at Louisiana State University Health Sciences Center [LSUHSC],” received institutional review board approval (LSUHSC-Shreveport H11-040) in May 2008. Patient enrollment occurred over 78 weeks, beginning in June 2008 and ending in November 2009. While the final question was asked in November 2009, data could not be collected from the electronic medical record system until the last patient was discharged. As a result, data collection did not take place until 2010. For matching, we matched each case in the intervention group with a maximum of 4 control patients who were hospitalized for at least 1 day on the IM service from June 1, 2005, to May 31, 2010. The 5-year time span was chosen to provide a sufficient number of matched cases.
Clinical medical librarian intervention
Many questions occur during rounds, and while many are answered by the attending or other members of the team, some need further information. The CML was embedded only in Team 1 throughout the seventy-eight weeks of the study, so only Team 1 patients were eligible for the intervention group. Patients from Team 1 entered the study as members of the intervention group whenever a care provider asked the CML a question regarding the care of that patient. If no query to the CML was made regarding patients hospitalized on Team 1 throughout their stay, they joined all of the patients in Team 2 as members of the control population. Demographic information such as medical record number, patient number, and attending physician and library metrics such as date of question, search time, and resources used were documented by the CML on the data collection form (Appendix, online only). Whenever possible, the CML answered specific questions posed by team members during rounds using online medical information resources, in the same manner as was done prior to initiating the study. More detailed answers and answers to more complex questions were supplied via email after rounds. Email messages would summarize the answer to the question posed, refer to the citation, and provide full-text of the cited articles, when available. Instruction by the librarian on search techniques and possible resources to use was limited to reduce the number of intrusions on the clinical team.
In addition to the access to the CML provided to Team 1, all members of both Team 1 and Team 2 could use information resources that are always available to them. These included, but were not limited to, using hospital computers (linked to full library resources) on each ward, using their personal smart phones and pocket handbooks of medicine, or going to the library and speaking to an available librarian (not the CML).
Statistical analysis
A number of aspects of the statistical analysis of our previous work was incorporated into this report 21. We performed three analyses in this study. The first compared outcome variables between the intervention group and control group. The second compared clinical results for intervention cases with the clinical results for up to four matched controls. The third compared the outcome variables of readmission and mortality rates for pairs formed by intervention cases and their first matched control.
The first analysis compared outcome variables between the intervention group patients and the control population. Demographic information, primary diagnostic code, and number of concomitant diagnostic codes (secondary diagnoses) as well as hospital length of stay, hospital cost, and readmission rate within 30 days were determined for the 252 cases (23% of the patients on Team 1) forming the intervention group and the 1,948 members of the control group (the remainder of the patients on Team 1 and the patients on Team 2). To evaluate whether the presence of the CML influenced length of stay, all patients were required to be hospitalized for at least 1 day to be included in the analysis. We used the Wilcoxon 2-sample test to test for statistical differences between medians or the Student's t-test to test for differences between the means of the 2 populations, depending upon the distribution of the outcome variables.
The second analysis was a matched case-control analysis. This analysis was based on the intervention group and the control group of all patients admitted for more than 24 hours to the IM service from June 1, 2005, to May 31, 2010. Matching criteria included an identical primary diagnosis (International Classification of Diseases, ninth revision [ICD-9], code with decimal), age (+/−5 years), and secondary diagnoses (+/−3). For this matched analysis, the non-parametric Wilcoxon signed rank test was used because of the non-normal distribution of data. The average value of the outcome measure (e.g., length of stay) for up to 4 control patients per matched intervention case was used to compute the difference.
For the third analysis, the paired analysis, we compared in-hospital mortality between the matched groups of the cases with their closest matched control (i.e., usually the first of several controls identified during the matching process), using McNemar's test. The closest match was defined as the match with the smallest absolute value of the total difference where the total difference = |age difference|+|difference in the number of secondary diagnoses|. In case of ties, matches were chosen randomly. Matching of cases and controls and all statistical data analyses were performed using SAS system 9.2 for Windows (SAS Institute, Gary, NC). All 2-sided P-values were reported, and P<0.05 was considered statistically significant.
RESULTS
Two thousand two hundred six patients were hospitalized on the 2 IM teams and were eligible to be enrolled between June 2008 and November 2009. The CML answered 334 questions on 258 unique patients (13% of the patients) (Table 1). Because the study protocol required patients to have a length of stay of at least 1 day, 6 patients were eliminated from analysis. The remaining 252 patients became the intervention group.
Table 1.
Characteristics of questions posed to clinical medical librarian (CML)
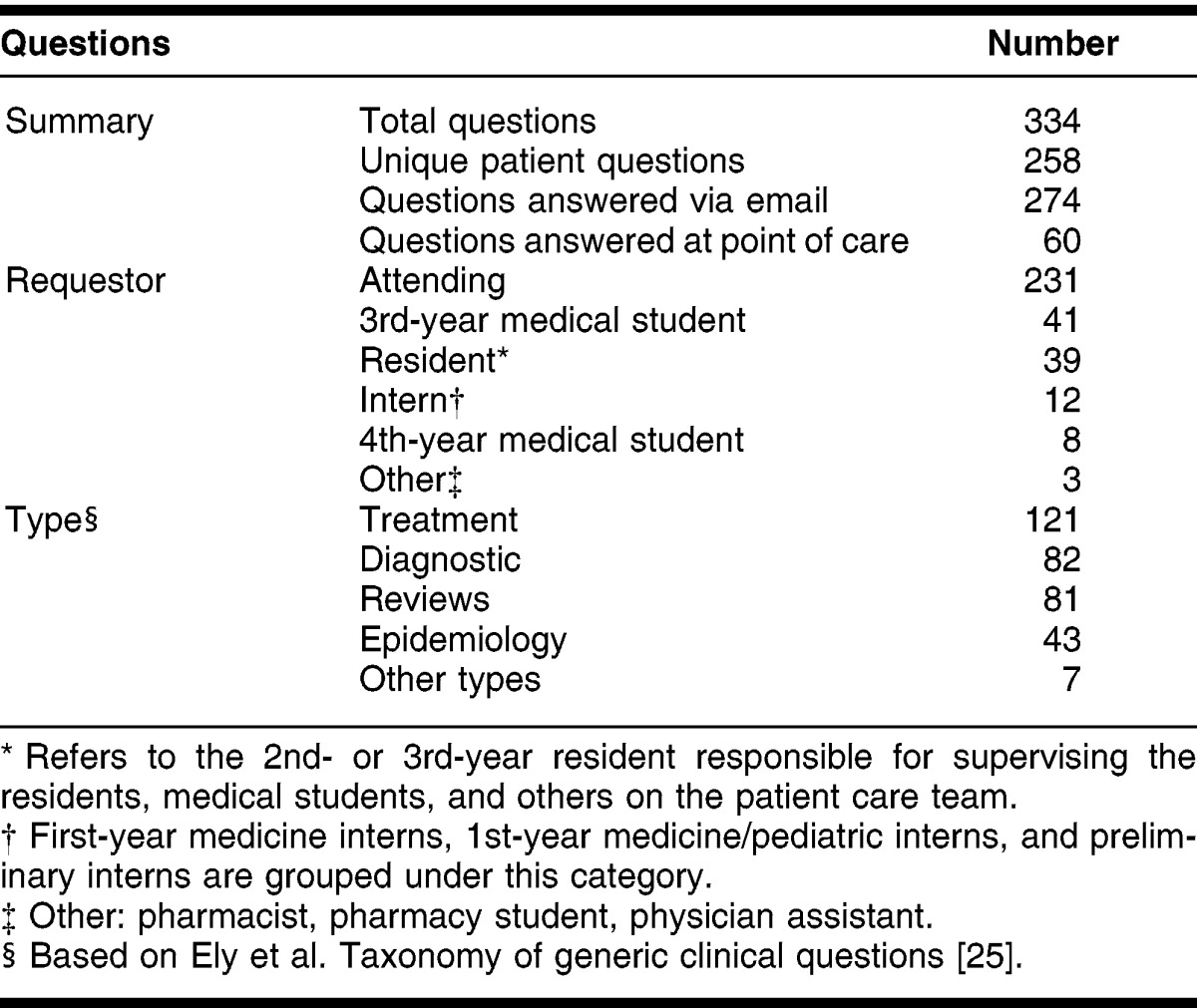
The most frequent requestor of information was the attending physician, followed by third-year medical students on the team (Table 1). Treatment and diagnostic questions dominated the information needs of the IM team, but they also frequently requested general overviews to expand their knowledge. The CML worked over 636 hours, with almost 123 hours dedicated to researching clinical questions (Table 2). Of the 636 CML hours, more than 347 hours were at the bedside of patients and 128 hours were meeting with the patient care team and discussing patients. The most frequent resources searched to answer questions were PubMed, followed by AccessMedicine and MD Consult. PubMed and AccessMedicine were the resources with highest number of relevant citations; however, many times the attending asked for a document from a specific website. For example, 2 of the specific websites with the most requested resources were the New England Journal of Medicine and the Infectious Diseases Society of America. When considering resources used in the study, it is important to note that LSU Health did not have access to DynaMed at the time of the study.
Table 2.
Resources used by time and number of citations retrieved
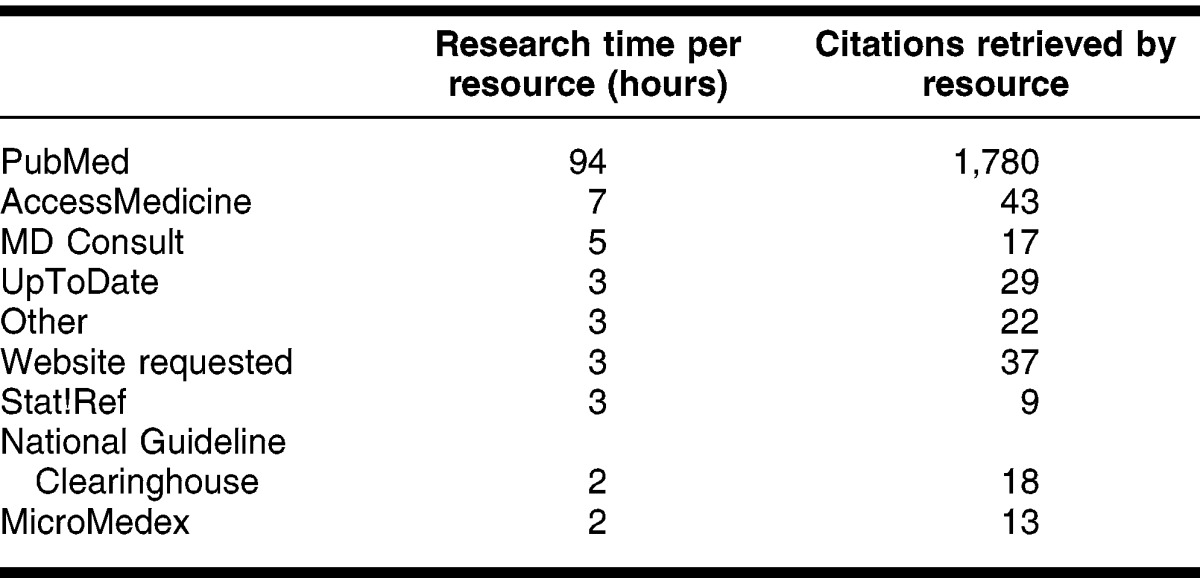
Table 3 shows demographic and comparative results for the 252 cases forming the intervention group and the 1,948 control cases. Although the intervention group was younger, there was no difference in gender or race between the 2 groups.
Table 3.
Comparison of demographic data between the intervention and control groups
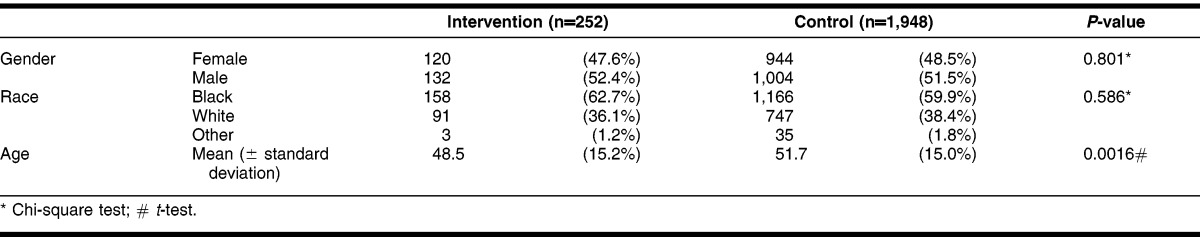
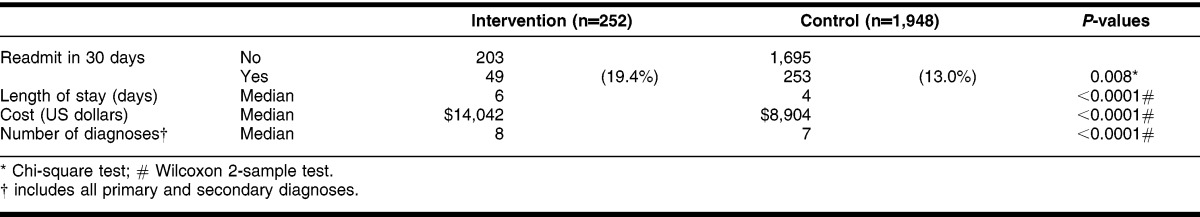
Table 4 shows the differences in the intervention and control groups. The median patient length of stay in the hospital, median patient costs, the number of diagnostic codes, and readmission rates within thirty days are shown. Compared to the study population, those patients with questions answered by the CML had significantly higher thirty-day readmission rates, longer lengths of stay, higher costs, and more diagnoses.
Table 4.
Comparison of clinical results between intervention and control patients
Matches were made for 132 of the 252 intervention cases. Fifty cases had 4 matches; 26 cases had 3 matches; 23 cases had 2 matches; and 33 cases had 1 match. Table 5 shows the comparability of the matches in the paired analysis. In this table, negative numbers mean that the values were greater in the comparison group, while positive numbers mean the values were greater in the intervention group. The median age of the control group was older in the paired analysis. No statistically significant differences between the intervention and control groups were found for median difference in the total number of diagnostic codes, length of stay, or hospital cost.
Table 5.
Comparison of clinical results between 132 pairs of intervention and matched case-control patients*
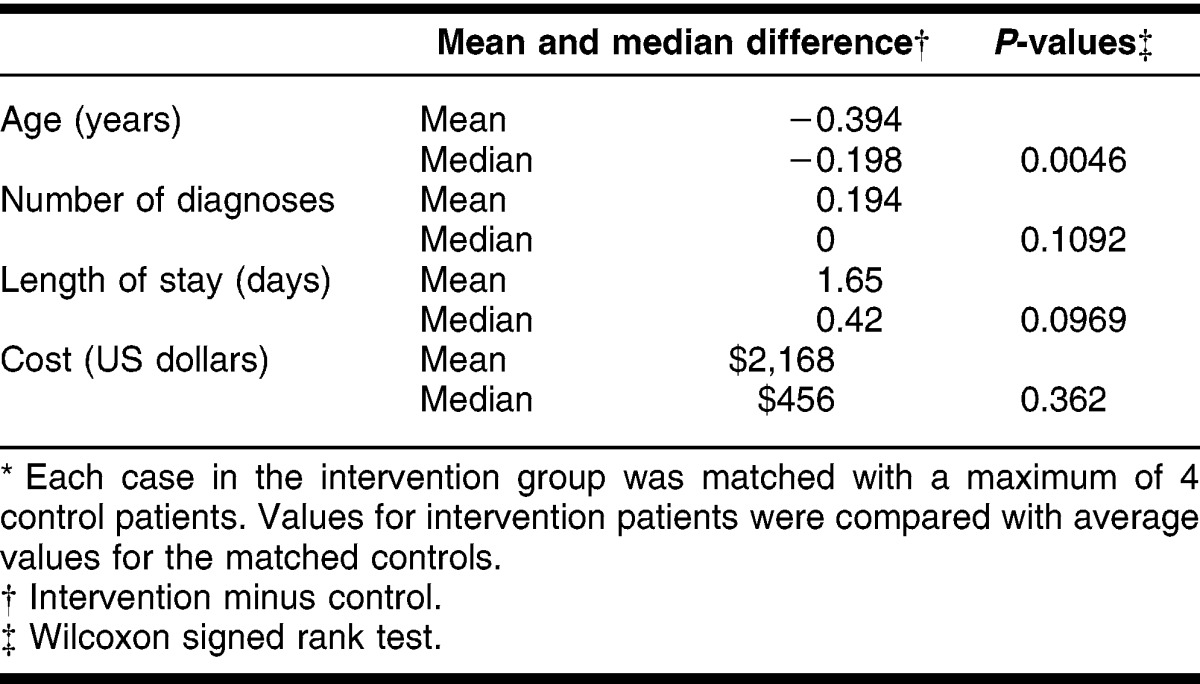
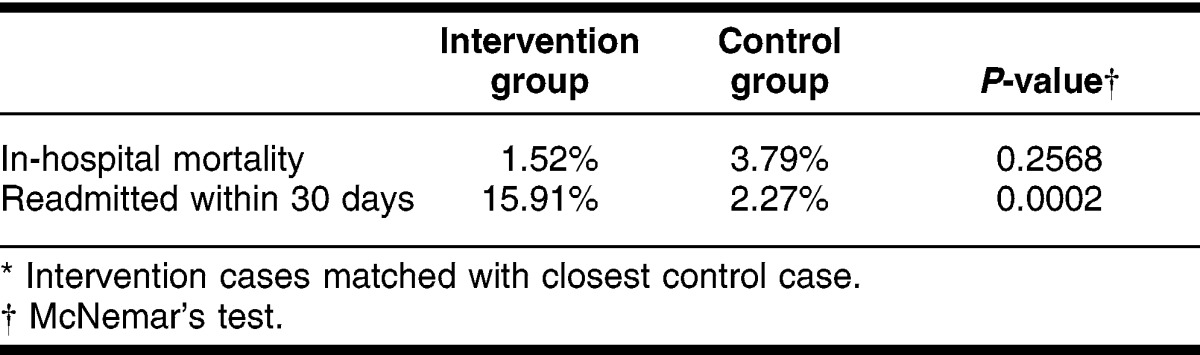
Table 6 measured the in-hospital mortality and readmission rate within 30 days for the 132 matched pairs. Mortality was 3.8% for the control group and 1.5% for the intervention group. This difference was not statistically significant (P = 0.25). Despite matching, the intervention group had a dramatically greater readmission rate within 30 days (P = 0.0002).
Table 6.
Comparison of intervention and control group readmission and mortality rates for paired analysis* (n = 132)
Finally, there were no differences (data not shown) in gender, race, or readmission rates when comparing the matched and unmatched members of the intervention group; however, mortality was marginally greater in the unmatched members (6.67% vs. 1.52%, P = 0.051).
DISCUSSION
Our intention was to compare the outcomes of patients: the “intervention group,” who benefited from the addition of a CML who provided point-of-care information, with the control population, for whom a CML did not answer questions. However, the comparison was complicated by differences between the intervention group and their controls. Using parameters that are commonly recognized to measure the effect of an intervention in hospitalized patients, we found that the intervention group was more ill than the controls. The intervention group had longer lengths of stay, higher cost, greater number of diagnoses, and higher readmission rate, despite their younger age, than the controls (Table 4). When a matched pair analysis was performed to minimize the effect of disease heterogeneity, which could affect the parameters measured in this research, the differences of the median length of stay, hospital cost, and mortality rates between intervention patients and their controls were not statistically significantly except for a dramatic difference in readmission rates within 30 days between the 2 groups (Table 6). The reasons for this difference are not clear. Comparison of matched to unmatched patients in the intervention group indicated that 132 matched patients in the paired analysis were similar to 120 unmatched patients, except for a marginal increase in mortality rate among the unmatched patients. The increase in readmission rates, too, is not easily understandable. Overall, using the intervention and the approach to statistical analysis described above, we concluded that we did not improve patient outcomes by this intervention.
Two previous reports suggest that when a search was done earlier in the patient's stay, differences in outcome occurred 20, 21. In this report, 249 of the 252 clinical queries referred to the CML were made within the first day of the patient's hospitalization.
We recognize several limitations of this report. First, this project was undertaken with a single CML at a single academic medical center. Second, we did not attempt a randomized controlled study design because responding to all questions during attending faculty rounds was a part of the regular job duties of the CML. We could not answer queries on some patients and refuse to answer queries on others. Third, we considered a larger population but thought it impractical as the likelihood in recognizing a difference of 15% (not 20% as we chose) between the 2 groups would have required 443 interventions and an extended time frame. Fourth, the IM team was not required to review the information provided by the CML in an attempt to answer the clinical question. In other cited clinical studies, it was a condition that clinicians review the clinical information and address the usefulness of the information by either including or rejecting this information in the care of the patient or by addressing the usefulness of the information in a follow-up survey 20, 21. Finally, the care was provided in a safety-net hospital. Although matching was done, patients with complex problems might remain hospitalized for prolonged times as options for long-term acute care hospitals or rehabilitation centers may not be available due to insurance status. This might have biased the outcomes as those who were more ill were more likely to remain in the hospital. This would directly impact the length of stay and the hospital costs. In addition, a recent publication indicates that readmission rates may be beyond the control of a medical team; therefore, its value as an outcome measure may be diluted 23. With these limitations, it is not surprising that little work has been done to measure the impact of the interventions by the CML on patient care outcomes.
The intervention group was very different from the control population. As a group, they were more ill, as evidenced by their hospital stay duration; had a higher cost of care; and had a greater readmission rate within thirty days of discharge. It is not surprising that physicians would have more queries regarding those with more complex medical problems.
To evaluate the effects of intervention, the degree of heterogeneity of disease, the severity of disease, and the number of concomitant conditions (secondary diagnoses) were minimized by matching the potential control patients by ICD-9 codes, age, and total number of diagnostic codes to the members of the intervention group. Although commonly used and considered reasonable, these match criteria might not be optimal. Propensity score matching was tried in an attempt to overcome the intervention and control group differences. The heterogeneity of diagnostic codes would not allow a reasonable propensity score projection 24. This problem could be addressed in future studies by focusing on single (common) disease groups with less heterogeneity in severity and comorbidities.
A recent review addressed the intrinsic difficulties in studying the field of clinical librarianship 19. Using the population, intervention, comparator, and outcome (PICO) model to explain the complexities, that review sheds light on the issues of possible bias in team selection, the difficulty in defining the role of a clinical librarian, and the complexity of evaluation. The authors understand that the designs of intervention studies in clinical settings are complex and the influences on results may be subtle and difficult to measure. The educational dynamics associated with patient care in a ward team with an embedded CML can be complicated by the personalities of the members of the team, the academic interests of team members, and the leadership and level of competence and experience of the attending physician. Similarly, comparing the quality of patient care between providers on different teams is difficult. Furthermore, the knowledge and experiences of the CML may affect the interactions within the team, as well as the appropriateness of the results of the literature search. Hidden factors such as acceptance of the CML by the care providers as well as the CML's ability to work with the members of the ward team; the relevance of the questions to the patient's outcome; the utilization of the material provided to the faculty, residents, and students; the availability of resources (i.e. new drugs, procedures) to adopt a modified care plan; and the presence of literature providing a definitive evidence-based answer can obscure or amplify the effect of CML services. All of these variables can be magnified by studies of short duration or situations where there is relatively rapid turnover of the care providers on the ward team.
CONCLUSIONS
This report is the largest study published to date to prospectively measure the use of “hands-on” librarian interactions with physicians in delivering patient care and not solely assess patient care outcomes by questionnaire. Can the same outcomes be expected in all settings? Future research, perhaps in the context of a randomized controlled study, could evaluate the effectiveness of a CML at the point of care among care providers in other (i.e., nonprofit, for-profit) hospitals. Are there differences between the outcomes of a CML integrated into patient care in IM and the results gleaned from implementing such a program in the department of pediatrics, the trauma department, or a setting, such as the military, where a considerable amount of care is provided by physician assistants or nurse practitioners? Clinicians may conclude that their smart phones or the patient care handbooks in the pockets of their white coats sufficiently address all of their clinical questions on a day-to-day basis. Yet, do physician attitudes stand in the way of accepting the full benefit of work done by the CML? As librarians advocate for EBM and EBP, they need to reach beyond surveys of satisfaction and continue to directly address the impact of their services on patient outcomes.
Electronic Content
Footnotes
Based on presentations at the 2010 South Central Chapter, Medical Library Association, Annual Meeting, October 19, 2010, Austin, TX; MLA '10, 110th Annual Meeting of the Medical Library Association, Washington, DC, May 26, 2010; and 2008 South Central Chapter, Medical Library Association, Annual Meeting, October 14, 2008, Dallas, TX.
A supplemental appendix is available with the online version of this journal.
REFERENCES
- 1.National Library of Medicine. A brief history of NLM [Internet] The Library; 2012 [updated 3 Jan 2012; cited 12 Jun 2012]. < http://www.nlm.nih.gov/about/briefhistory.html>. [Google Scholar]
- 2.Ely JW, Osheroff JA, Ebell MH, Chambliss ML, Vinson DC, Stevermer JJ, Pifer EA. Obstacles to answering doctors' questions about patient care with evidence: qualitative study. BMJ. 2002 Mar 23;324(7339):710–3. doi: 10.1136/bmj.324.7339.710. DOI: http://dx.doi.org/10.1136/bmj.324.7339.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graber MA, Randles BD, Ely JW, Monnahan J. Answering clinical questions in the ED. Am J Emerg Med. 2008 Feb;26(2):144–7. doi: 10.1016/j.ajem.2007.03.031. DOI: http://dx.doi.org/10.1016/j.ajem.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 4.Algermissen V. Biomedical librarians in a patient care setting at the University of Missouri–Kansas City School of Medicine. Bull Med Lib Assoc. 1974 Oct;62(4):354–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Colaianni LA. Clinical medical librarians in a private teaching-hospital setting. Bull Med Lib Assoc. 1975 Oct;63(4):410–1. [PMC free article] [PubMed] [Google Scholar]
- 6.Lamb G. Bridging the information gap. Hosp Lib. 1976 Nov 15;1(10):2–4. [PubMed] [Google Scholar]
- 7.Schnall JG, Wilson JW. Evaluation of a clinical medical librarianship program at a university health sciences library. Bull Med Lib Assoc. 1976 Jul;64(3):278–83. [PMC free article] [PubMed] [Google Scholar]
- 8.Staudt C, Halbrook B, Brodman E. A clinical librarians' program—an attempt at evaluation. Bull Med Lib Assoc. 1976 Apr;64(2):236–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg B, Battison S, Kolisch M, Leredu M. Evaluation of a clinical medical librarian program at the Yale Medical Library. Bull Med Lib Assoc. 1978 Jul;66(3):319–26. [PMC free article] [PubMed] [Google Scholar]
- 10.Lipscomb CE. Clinical librarianship [historical notes] Bull Med Lib Assoc. 2000 Oct;88(4):393–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Scherrer CS, Dorsch JL. The evolving role of the librarian in evidence-based medicine. Bull Med Lib Assoc. 1999 Jul;87(3):322–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Learning objectives for medical student education—guidelines for medical schools: report I of the Medical School Objectives Project. Acad Med. 1999 Jan;74(1):13–8. doi: 10.1097/00001888-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Graduate Medical Education. 1 Jul 2009 [cited 21 Mar 2011]. ACGME program requirements for graduate medical education in internal medicine [Internet] The Council; < http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/140_EIP_PR205.pdf>. [Google Scholar]
- 14.Urquhart C, Turner J, Durbin J, Ryan J. Changes in information behavior in clinical teams after introduction of a clinical librarian service. J Med Lib Assoc. 2007 Jan;95(1):14–22. [PMC free article] [PubMed] [Google Scholar]
- 15.Vaughn CJ. Evaluation of a new clinical librarian service. Med Ref Serv Q. 2009 Summer;28(2):143–53. doi: 10.1080/02763860902816750. DOI: http://dx.doi.org/10.1080/02763860902816750. [DOI] [PubMed] [Google Scholar]
- 16.Mulvaney SA, Bickman L, Giuse NB, Lambert EW, Sathe NA, Jerome RN. A randomized effectiveness trial of a clinical informatics consult service: impact on evidence-based decision-making and knowledge implementation. J Am Med Inform Assoc. 2008 Mar–Apr;15(2):203–11. doi: 10.1197/jamia.M2461. DOI: http://dx.doi.org/10.1197/jamia.M2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greco E, Englesakis M, Faulkner A, Trojan B, Rotstein LE, Urbach DR. Clinical librarian attendance at general surgery quality of care rounds (morbidity and mortality conference) Surg Innov. 2009 Sep;16(3):266–9. doi: 10.1177/1553350609345487. DOI: http://dx.doi.org/10.1177/1553350609345487. [DOI] [PubMed] [Google Scholar]
- 18.Wagner KC, Byrd GD. Evaluating the effectiveness of clinical medical librarian programs: a systematic review of the literature. J Med Lib Assoc. 2004 Jan;92(1):14–33. [PMC free article] [PubMed] [Google Scholar]
- 19.Brettle A, Maden-Jenkins M, Anderson L, McNally R, Pratchett T, Tancock J, Thornton D, Webb A. Evaluating clinical librarian services: a systematic review. Health Info Lib J. 2011 Mar;28(1):3–22. doi: 10.1111/j.1471-1842.2010.00925.x. DOI: http://dx.doi.org/10.1111/j.1471-1842.2010.00925.x. [DOI] [PubMed] [Google Scholar]
- 20.Klein MS, Ross FV, Adams DL, Gilbert CM. Effect of online literature searching on length of stay and patient care costs. Acad Med. 1994 Jun;69(6):489–95. doi: 10.1097/00001888-199406000-00017. [DOI] [PubMed] [Google Scholar]
- 21.Banks DE, Shi R, Timm DF, Christopher KA, Duggar DC, Comegys M, McLarty J. Decreased hospital length of stay associated with presentation of cases at morning report with librarian support. J Med Lib Assoc. 2007 Oct;95(4):381–7. doi: 10.3163/1536-5050.95.4.381. DOI: http://dx.doi.org/10.3163/1536-5050.95.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Office for Civil Rights (US) OCR privacy brief summary of the HIPAA privacy rule: HIPAA compliance assistance [Internet] Bethesda, (MD): Department of Health and Human Services (US); 2003 [cited 16 Oct 2012]. < http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/privacysummary.pdf>. [Google Scholar]
- 23.Joynt KE, Jha AK. Thirty-day readmissions—truth and consequences. N Engl J Med. 2012 Apr 12;366(15):1366–9. doi: 10.1056/NEJMp1201598. DOI: http://dx.doi.org/10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 24.D'Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998 Oct 15;17(19):2265–81. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. DOI: http://dx.doi.org/10.1002/(SICI)1097-0258(19981015)17:19<2265::AID-SIM918>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 25.Ely JW, Osheroff JA, Gorman PN, Ebell MH, Chambliss ML, Pifer EA, Stavri PZ. A taxonomy of generic clinical questions: classification study. BMJ. 2000 Aug 12;321(7258):429–32. doi: 10.1136/bmj.321.7258.429. DOI: http://dx.doi.org/10.1136/bmj.321.7258.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


