Abstract
In May 2009, one of the earliest outbreaks of 2009 pandemic influenza A virus (pH1N1) infection resulted in the closure of a semi-rural Pennsylvania elementary school. Two sequential telephone surveys were administered to 1345 students (85% of the students enrolled in the school) and household members in 313 households to collect data on influenza-like illness (ILI). A total of 167 persons (12.4%) among those in the surveyed households, including 93 (24.0%) of the School A students, reported ILI. Students were 3.1 times more likely than were other household members to develop ILI (95% confidence interval [CI], 2.3–4.1). Fourth-grade students were more likely to be affected than were students in other grades (relative risk, 2.2; 95% CI, 1.2–3.9). pH1N1 was confirmed in 26 (72.2%) of the individuals tested by real-time reverse-transcriptase polymerase chain reaction. The outbreak did not resume upon the reopening of the school after the 7-day closure. This investigation found that pH1N1 outbreaks at schools can have substantial attack rates; however, grades and classrooms are affected variably. Additioanl study is warranted to determine the effectiveness of school closure during outbreaks.
Since 2009 pandemic influenza A virus (pH1N1) was identified in April 2009, prevention and control of disease in educational settings has been a major concern. The first identified cases of illness caused by this virus occurred in school-age children in California and Texas, and the highest incidence of pH1N1 disease in the United States has been in the 5–19-year-old age group [1, 2]. Because schools are well-known settings for the transmission of influenza [3–9], concerns were raised that they could serve as sites for enhanced spread of pH1N1, not only among attendees but also among their families and the community. Some of these concerns were confirmed when extensive transmission was documented among students at a New York City private school [10].
On 28 April 2009, the Centers for Disease Control and Prevention (CDC) issued interim guidance to prevent and control pH1N1 in schools, recommending that communities with suspected or probable cases of pH1N1 infection among students enrolled in kindergarten (grade K) through grade 12 consider school dismissal for 7 days to reduce the spread of influenza to students, their families, and staff [11]. On 1 May 2009, the guidance was revised to extend the duration of dismissal to 14 days, to increase the likelihood of interrupting transmission among students [12]. As pH1N1 spread in the US and as data became available that suggested that most of the cases were relatively mild, these recommendations proved to be controversial, because large numbers of schools serving thousands of students were closed, which raised concerns about potential social disruption caused by parental work loss and inadequately supervised children. On 5 May 2009, the CDC revised the guidance and recommended that only sick students and staff stay home but that schools should retain the option of closure on the basis of their specific circumstances, such as high absenteeism [13]. The evolving recommendations reflect the many unanswered questions about the best approach to prevention and control of pH1N1 in the school setting.
In early May 2009, an outbreak caused by pH1N1 was reported to the Pennsylvania Department of Health (PADOH) in a semi-rural Pennsylvania elementary school, which prompted a 7-day (Thursday–Wednesday) closure. In comparison to most of the other school outbreaks identified during the initial phase of the pandemic, the Pennsylvania outbreak had several unique features. First, it occurred in a location where there was little evidence of disease in the surrounding community. Second, it was in a semi-rural area and not in an urban or suburban location [1]. Third, the involved age group (children enrolled in kindergarten through grade 4) was younger than the age groups seen in most other published school outbreaks from the initial wave of the pandemic [4, 10, 14, 15]. Because of these unique features, this school-associated outbreak was intensively investigated by the PADOH and the CDC to describe the characteristics of illness and the patterns of spread of influenza among the school children and their families before and during the school closure.
METHODS AND MATERIALS
Setting
When pH1N1 was first recognized, all schools in Pennsylvania were instructed to contact the health department if increased absenteeism was observed and to contact ill students’ homes to identify the cause. The School A outbreak was recognized on Monday, 11 May 2009, when the overall school absenteeism rate was found to be 11.4%, which was higher than the 3%–4% baseline at this school. Calls to the homes of absent students revealed that many had respiratory illness and that 1 fourth-grader who had sought care the preceding weekend had test results that were positive for influenza A virus with a rapid influenza diagnostic assay. This student’s specimen was subsequently confirmed to contain pH1N1 at the PADOH's Bureau of Laboratories (BOL) on 12 May, the same day that absenteeism increased to 15.4%. School A was closed on 14 May in an effort to limit further transmission.
School A is 1 of 4 public schools in a district with a single high school (grades 9–12), a single middle school (grades 5–8), and 2 elementary schools (grades K–4). The district is located in a semi-rural area of southeastern Pennsylvania and serves a population of 7306 persons. School A has a student population of 456 students from 364 households, along with 69 teachers and support staff. The students spend most of the day in 1 of 23 homerooms, except for special classes held outside of the homeroom, including physical education, art, music, computer, and library. The school also has a cafeteria that is used during lunch.
Definitions
Influenza-like illness (ILI) was defined as subjective fever with cough and/or sore throat in a School A student or their household members during the period 1 May–2 June 2009. Acute respiratory infection (ARI) was defined as having at least 2 symptoms, including fever, cough, sore throat, or runny nose, in a School A student or their household members during the period 1 May–2 June 2009. CDC definitions for confirmed, probable, and suspected cases of infection due to pH1N1 were used [16]. A confirmed case patient was an individual with ILI and laboratory evidence of pH1N1 by virus culture or real-time reverse-transcriptase polymerase chain reaction (rRT-PCR). A probable case patient was an individual with ILI and influenza A infection by rRT-PCR with a virus that could not be subtyped as seasonal influenza A/H1N1 or H3N2. Suspected case patients had ILI with no other known cause of illness but did not have laboratory testing performed for the presence of influenza virus.
Laboratory Testing
Field staff collected nasopharyngeal (NP) swabs from 16 School A students and 20 household members who had ILI onset within 7 days of interview. All specimens were sent to BOL and tested by rRT-PCR using the CDC pH1N1 rRT-PCR protocol that had been approved under an Emergency Use Authorization [17]. Other School A students and their household members had specimens collected by their own physicians or other clinician. Positive results from such testing were reported to Pennsylvania's National Electronic Disease Surveillance System (PA-NEDSS).
Data Collection
This investigation was part of the emergency public health practice response to the pandemic and was reviewed by a human subjects coordinator at the CDC and deemed not to be research in accordance with the federal human subjects protection regulations at 45 Code of Federal Regulations 46.101c and 46.102d and the CDC Guidelines for Defining Public Health Research and Public Health Non-Research. A list of School A students and their parents or guardians (including contact information) was obtained from the school administration, and to establish a baseline, absenteeism data were obtained for the period 1 April–13 May (13 May being the day prior to school closure). Once school reopened, absenteeism rates were monitored until the end of the school year.
An initial telephone survey was conducted during the period 16–21 May among parents or guardians of School A students using a structured questionnaire. Respondents were asked about household composition and demographic characteristics, as well as the presence and onset date of ILI among any household member after 1 May. The survey also asked whether ill individuals sought medical care, whether they were tested for influenza, and whether they were treated with medications, including antiviral agents.
A second structured questionnaire was administered by telephone from 26 May through 2 June to parents and guardians of School A students. The objective of this survey was to capture data on any individuals who may have become ill since the first survey and to collect information from households that did not participate in the first questionnaire. Questions about ILI that were similar to questions in the first survey were included, as were questions about clinical details of illness (symptoms, hospitalization, influenza testing, and medication), student participation in a variety of activities during and after school, underlying health conditions, 2008–2009 seasonal vaccination status, and travel history. To assess the occurrence of pH1N1 in the surrounding community, patients with pH1N1 in the county in which School A is located were identified using PA-NEDSS.
Statistical Analysis
Databases were created and maintained using Microsoft Access 2003 software and analyzed using SAS software, version 9.1 (SAS Institute) and STATA, version 10 (Stata). Data from the 2 surveys were merged for the analysis. Onset dates and clinical information from the first survey were used for persons who participated only in this survey and for those whose ILI onset occurred on or before the first survey was conducted. Onset dates and clinical information from the second survey were used for individuals who participated only in the second survey, as well as those who became ill after the first survey. Information that was only asked on the second survey (eg, underlying conditions, vaccination status, and travel history) was also merged into the unified database.
Univariable analyses were performed, and relative risks (RR) and 95% confidence intervals (CIs) of developing ILI between groups were calculated. Illness events were unreported if individuals developed ILI during the study period but after their last interview. Such censoring of the data might lead to underestimating ILI incidence. To evaluate the robustness of our findings to censoring, survival analyses were also performed to examine the time to the event (ie, developing ILI) from 1 May 2009 to the time of the last interview. The Kaplan–Meier method was used to estimate survival functions. Findings from the survival analyses were compared with the univariable analyses to determine their similarity.
RESULTS
A total of 41 confirmed cases of pH1N1 influenza were associated with the School A outbreak. Of these, 26 (72.2%) (13 in students and 13 in household members) were identified through the 36 specimens collected as part of the investigation, whereas 15 (4 in students and 11 in household members) were collected as part of the clinical care of the patients and were reported through PA-NEDSS. No teachers or staff members reported ILI or were confirmed with pH1N1 infection during the outbreak period. Among the 3 other schools in the district, none exhibited patterns of absenteeism similar to that in School A.
At least 1 of the 2 surveys was completed for 313 (86.0%) School A student households. The mean household size (± standard deviation) was 4.3 ± 1.4 individuals. Individual symptom questionnaires were completed for a total of 1345 persons, including 388 (85.1%) of the 456 students at School A (Tables 1 and 2). Response rates were similar among different grades at the school (Table 2). Among the surveyed households, 167 persons (12.4%) reported ILI. Among the 388 School A students who were surveyed, 93 (24.0%) reported ILI (Table 1). A total of 123 (31.7%) of the students and 143 (14.9%) of the household members were reported to have acute respiratory infection. Survival analyses estimated that 13.3% of surveyed individuals developed ILI; this figure was statistically similar to the 12.4% ILI rate found in the survey.
Table 1.
Relative Risk (RR) and 95% Confidence Intervals (CIs) for Influenza-like Illness (ILI) by Demographic Characteristics, Pennsylvania, May 2009
| ILI, no. (%) of respondents |
|||
| Demographic characteristic | Yes | No | RR (95% CI) |
| Respondent group | |||
| School A students (n = 388) | 93 (24.0) | 295 (76.0) | 3.1 (2.3–4.1) |
| Household members (n = 957) | 74 (7.7) | 883 (92.3) | Referent |
| Sex | |||
| Male (n = 658) | 82 (12.5) | 576 (87.5) | 1.0 (0.8–1.4) |
| Female (n = 667) | 81 (12.1) | 586 (87.9) | Referent |
| Agea | |||
| 0–4 Years (n = 103) | 11 (10.7) | 92 (89.3) | 2.0 (1.0–3.9) |
| 5–10 Years (n = 408) | 100 (24.5) | 308 (75.5) | 4.6 (3.1–6.8) |
| 11–18 Years (n = 188) | 25 (13.3) | 163 (86.7) | 2.5 (1.5–4.1) |
| 19–54 Years (n = 563) | 30 (5.3) | 533 (94.7) | Referent |
| 55–81 Years (n = 37) | 0 | 37 (100) | 0 |
Age data was not reported for 46 individuals.
Table 2.
Student Response Rates and Frequency of Influenza-like Illness (ILI) by Grade and by Fourth Grade Homeroom, Elementary School A, Pennsylvania, May 2009
| Grade (no. of all students) | No. (%) who responded | No. (%) with ILI | RR (95% CI) |
| K (n = 80) | 65 (81.3) | 12 (18.5) | Referent |
| 1 (n = 95) | 77 (81.1) | 16 (20.8) | 1.1 (0.6–2.2) |
| 2 (n = 90) | 83 (92.2) | 16 (19.3) | 1.0 (0.5–2.1) |
| 3 (n = 91) | 79 (86.8) | 15 (19.0) | 1.0 (0.5–2.0) |
| 4 (n = 100) | 84 (84.0) | 34 (40.5) | 2.2 (1.2–3.9) |
| Homeroom 1 (n = 24) | 23 (95.8) | 14 (60.9) | 2.9 (1.1–7.3) |
| Homeroom 2 (n = 24) | 19 (79.2) | 4 (21.1) | Referent |
| Homeroom 3 (n = 26) | 22 (84.6) | 6 (27.3) | 1.3 (0.4–3.9) |
| Homeroom 4 (n = 26) | 20 (76.9) | 10 (50.0) | 2.4 (0.9–6.3) |
| Total (n = 456) | 388 (85.1) | 93 (24.0) |
NOTE. CI, confidence interval; K, kindergarten; RR, relative risk
Children 5–10 years of age were >4 times as likely as those 19–54 years of age to develop ILI (RR, 4.6; 95% CI, 3.1–6.8) (Table 1). School A students were 3 times more likely than other household members to develop ILI (RR, 3.1; 95% CI, 2.3–4.1) (Table 1). There was no difference in ILI incidence by sex.
ILI onset for School A students and their household members occurred over the same time period (Figure 1), but ILI in the School A students generally occurred earlier. Among those with ILI, it occurred during the first 10 days of May in 67.0% of the students but in only 33.0% of household members (P < .01).
Figure 1.
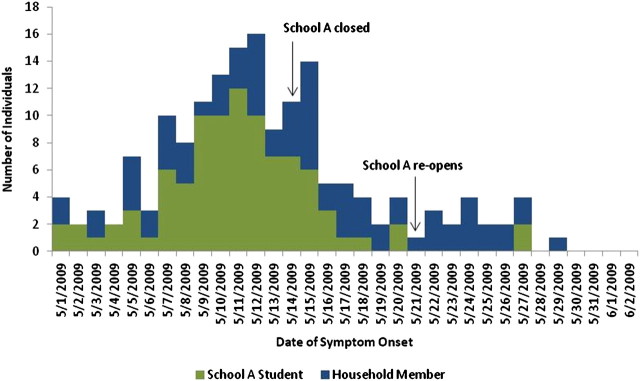
Onset of symptoms in individuals with influenza-like illness (ILI) stratified by students and household members. Pennsylvania, 1 May–2 June 2009.
Almost one-half (40.5%) of fourth-graders developed ILI, which was a significantly higher proportion than that among kindergarten students (who were selected as the reference group) at School A (RR, 2.2; 95% CI, 1.2–3.9) (Table 2). Among the 4 homerooms in the fourth grade, 2 were disproportionately affected, accounting for 70.6% of all illness in the fourth grade. Onset dates were similar across all grades (Figure 2).
Figure 2.
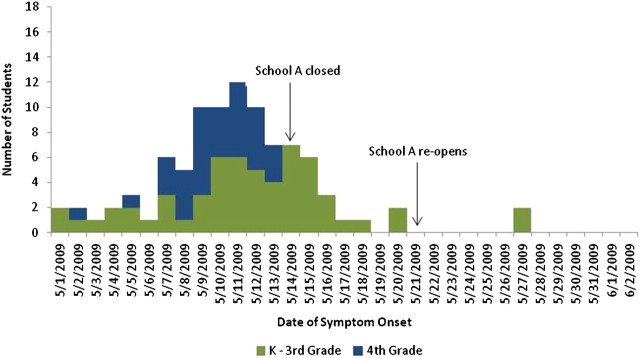
Onset of symptoms in School A students stratified by grade, Pennsylvania, 1 May–2 June 2009. K, kindergarten.
Among those with ILI, features of illness were generally similar across different age strata (Table 3). Children under 11 years of age were more likely to report cough (χ2, 9.6; P < .001) and less likely to report muscle aches than were older individuals (χ2, 16.3; P < .001). In contrast, diarrhea was more common among adults than among children (χ2, 9.7; P < .001)
Table 3.
Symptoms Reported by Individuals with Influenza-like Illness (ILI) by Age Group, Pennsylvania, May 2009
| Symptom | Age <5 years (n = 11) | Age 5–10 years (n = 100) | Age 11–18 years (n = 25) | Age 19–54 years (n = 30) | Totalb (n = 166) | χ2 (P) |
| Cough | 11/11 (100) c | 86/100 (86.0) | 18/25 (72.0) | 20/30 (66.7) | 135/166 (81.3) | 9.6 (<.001) |
| Sore throat | 5/10 (50.0) | 71/100 (71.0) | 17/25 (68.0) | 23/30 (76.7) | 116/165 (70.3) | 2.6 (.5) |
| Runny nose | 8/11 (72.7) | 51/100 (51.0) | 11/25 (44.0) | 16/30 (53.3) | 86/166 (51.8) | 2.6 (.5) |
| Vomiting | 3/11 (27.3) | 17/100 (17.0) | 4/25 (16.0) | 3/30 (10.0) | 27/166 (16.2) | 1.9 (.6) |
| Diarrhea | 1/11 (9.1) | 23/100 (23.0) | 1/25 (4.0) | 11/30 (36.7) | 36/166 (21.7) | 9.7 (<.001) |
| Vomiting and/or Diarrhea | 4/11 (36.4) | 31/100 (31.0) | 5/25 (20) | 11/30 (36.7) | 51/166 (30.7) | 2.0 (.6) |
| Muscle Aches | 1/10 (10.0) | 34/99 (34.3) | 11/25 (44.0) | 21/30 (70.0) | 67/164 (40.9) | 16.3 (<.001) |
NOTE. All individuals reporting ILI had fever, because this was a criterion of the case definition. A total of 167 cases of ILI were reported.
One individual with ILI did not report age.
Number of individuals with the specified symptom as a proportion of the number of individuals who responded to the symptom question.
A total of 95 persons with ILI (59.4%) reported visiting a health care provider for their illness. One person was hospitalized with pH1N1 infection and subsequently died. This 55-year-old individual was a household member of a School A student and had several underlying health conditions that are known to increase the risk of complications from influenza. Of those with ILI, 28 (16.8%) were prescribed antibiotics, 22 (13.2%) were prescribed a neuraminidase inhibitor (antiviral agent), and 4 (2.4%) received both types of drugs (Table 4). Among those who were prescribed neuraminidase inhibitors, 14 (63.6%) were School A students, and of those who received antibiotics, 22 (78.6%) were School A students. The 4 patients who received both a neuraminidase inhibitor and an antibiotic were also School A students. No one received neuraminidase inhibitors for prophylaxis.
Table 4.
Health Care Provider Visits and Prescribed Medication for Those with Influenza-like Illness (ILI) by Respondent, Pennsylvania, May 2009
| No. (%) of respondents with ILI |
|||
| Risk factor | School A students (n = 93) | Household members (n = 74) | Total (n = 167) |
| Visited health care providera | |||
| Yes | 61 (66.3) | 34 (50) | 95 (59.4) |
| No | 31 (33.7) | 34 (50) | 65 (40.6) |
| Received neuraminidase inhibitors | |||
| Yes | 14 (15.1) | 8 (10.8) | 22 (13.2) |
| No | 79 (84.9) | 66 (89.2) | 145 (86.8) |
| Received antibiotics | |||
| Yes | 22 (23.7) | 6 (8.1) | 28 (16.8) |
| No | 71 (76.3) | 68 (91.9) | 139 (83.2) |
| Received both neuraminidase inhibitors and antibiotics | |||
| Yes | 4 (4.3) | 0 | 4 (2.4) |
| No | 89 (95.7) | 74 (100) | 163 (97.6) |
One school A student and 6 household members with ILI did not report health care provider data.
A total of 230 individuals(17.1%) reported receiving influenza vaccine for the 2008–2009 influenza season; 35 (15.2%) developed ILI. After adjusting for age, those who received seasonal influenza vaccine were not statistically more likely to develop ILI than were those who did not receive the vaccine (RR, 1.0; 95% CI, 0.9–1.1). Among School A students, the risk of developing ILI was no different between vaccinated and unvaccinated students (RR, 0.9; 95% CI, 0.8–1.1).
During the period 1 May–2 June 2009, a total of 47 confirmed cases of pH1N1 were identified in School A's county, in addition to the 41 cases associated with School A. The first confirmed case of pH1N1 infection in the county that was not among School A students or household members did not occur until 17 May, 3 days after the school closed.
Of the 167 individuals with ILI, 12 (4 students and 8 household members) reported traveling (defined as out of county travel) during the week before onset of ILI. Most travel was within Pennsylvania, although 2 individuals reported travel to New York City during a time when pH1N1 was known to be circulating there.
When School A reopened on 21 May, absenteeism was reported to be 8.1%. Absenteeism then decreased, and by the following week, it had returned to pre-outbreak levels of 3%–4% during the week.
DISCUSSION
After it was recognized in the United States in mid-April 2009, pH1N1 spread rapidly throughout the country, and the first confirmed case in Pennsylvania had onset on 29 April, 2 weeks before the School A outbreak was first recognized on 11 May. The School A outbreak was quickly recognized, because the state Departments of Health and Education had recently recommended that all schools in Pennsylvania monitor their absenteeism rates and promptly report any increases to public health authorities. School A officials complied with this recommendation, expediting timely investigation of the outbreak and public health interventions to limit the extent of illness.
This investigation highlights the wide range of illness rates within a single community and school. Almost one-quarter of surveyed School A students experienced ILI. However, disease was unevenly distributed by grade, with significantly more illness in the fourth grade, which was the grade with the initial confirmed case. Even within the fourth grade, certain classrooms were more heavily affected than were others. Consistently increased rates of ILI or absenteeism at the other schools in the district were not observed during the same time period. Factors that may have contributed to this variability include the fact that students spend most of their day in a single homeroom, that the different grades were housed in different wings of the school, and that opportunities for mixing between grades were limited. It is also noteworthy that, despite significant levels of illness among the students, there was no reported ILI in any teacher or staff member at School A.
Despite the heightened awareness and guidance provided by PADOH regarding pH1N1 at the time of the outbreak, the diagnosis of influenza was not uniformly considered by clinicians in the area. Anecdotally, several parents reported that their children received diagnoses with streptococcal throat infection, and more children were prescribed antibiotics than were prescribed neuraminidase inhibitors. It is possible that local clinicians may not have considered the diagnosis of pH1N1 infection, because it had not been identified locally before the outbreak, and a significant proportion of those who were ill noted diarrhea in addition to the more typical influenza symptoms.
This outbreak afforded an opportunity to examine whether prior seasonal influenza vaccination altered the risk of pH1N1 infection. Reports related to this question have yielded conflicting findings. Some studies have demonstrated no impact of seasonal vaccination or have found a protective role for seasonal vaccine [18–20], whereas others have suggested that there is little cross-protection between immunity to the seasonal influenza strains and immunity to pH1N1 [21]. In the School A outbreak, vaccination did not protect against development of ILI. Limitations to this analysis include that vaccination status was not verified, that the outcome was ILI and not laboratory-confirmed influenza, and that it was not possible to adjust for underlying conditions. Nevertheless, our findings do not support a benefit of seasonal influenza vaccination in decreasing the risk for pH1N1 infection.
The rapidly escalating rates of absenteeism at School A and the presumptive identification of pH1N1 in 1 of the students prompted school officials to close the school for 7 days. The impact of the closure on the course and extent of the outbreak among School A students is uncertain; however, it is noteworthy that the outbreak did not resume among the students once school reopened and that absenteeism rates rapidly returned to baseline levels. Students with pH1N1 infection were not permitted to come back to school for a minimum period of 7 days or until they no longer had symptoms for at least 24 h, which may have contributed to limiting further spread. Also, some parents may have kept their children at home for additional days after school reopened to reduce their child's risk of exposure to pH1N1 at school. However, absenteeism levels may have returned to baseline even if the school had remained open, because of natural waning of the outbreak. At the time that the school was closed, almost three-quarters of the students had not experienced ILI, suggesting that there were many students who were likely still susceptible, although additional students may have had mild or asymptomatic infections. This uncertainty reinforces the need to better understand the effectiveness of school closure as a pH1N1 outbreak control measure, along with the optimal closure duration. Because pH1N1 continues to produce significant disease in school-aged children, such information is vitally needed to provide control recommendations.
It is possible that school closure may simply shift transmission from the school setting to the home or community setting. There is no evidence to suggest this occurred during the School A outbreak. Relatively few family members reported illness during the closure period. Increases in influenza in the community around School A mirrored similar increases seen throughout Pennsylvania.
This investigation is subject to limitations. First, the survey data were self-reported and could not be verified through other means. The main caregiver, who was usually a parent or guardian, provided the information for all members of the household. This may have over- or under-estimated the number of reported cases of ILI. Second, although the surveys were sequential, they may not have fully captured the scope and scale of the outbreak. It is possible that additional individuals in the cohort became ill after the surveys were done, especially because pH1N1 activity increased significantly in Pennsylvania in June 2009. The survival analysis was done to adjust for this possibility. However, it did not significantly alter the overall findings. Third, a small proportion (14%) of School A households were not interviewed. However, it is unlikely that such a low non-response rate would greatly impact the major findings of the investigation. Fourth, non-ILI acute respiratory illness was not assessed. Fifth, because most persons with reported ILI did not undergo diagnostic testing, it is unknown what proportion of ILI was actually due to pH1N1. However, among those tested by rRT-PCR, the proportion found to have pH1N1 was high (72.2%), and there was little seasonal influenza activity in Pennsylvania at the time of the outbreak or activity due to other respiratory viruses. Finally, survey responses may have been biased by media reports related to pH1N1. This was the first reported pH1N1 outbreak in Pennsylvania, and it attracted media attention in the area. The school district was also in daily communication with the families of the students of School A, and the families and students were likely in communication with each other. It is not possible to know how that may have influenced the responses that were given.
In summary, an outbreak of pH1N1 infection that primarily affected school-aged children at a single elementary school was the first outbreak to be detected in a small semi-rural community in Pennsylvania. The impact within the community varied substantially between schools and within the main school affected. A 7-day closure of the school was followed by few additional cases in the community or in the school. Although the impact of the closure as a control measure is unknown, attendance returned to normal upon resumption of classes 1 week later. The outbreak highlights the need to carefully study the effectiveness of school closure in reducing school and community transmission of influenza.
MEMBERS OF THE PENNSYLVANIA STUDY GROUP
Alicia Fry, Martin I. Meltzer, Paul J. Edelson, Amanda McWhorter, Charlotte Kent, Michelle Davis, John Beltrami, James Lute, Tracy Ayers, and Lyn Finelli.
Acknowledgments
We thank the Conrad Weiser Area School District, for their help and cooperation during the outbreak investigation, and Harrell Chesson, who assisted with survey design.
Financial support. Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement U60/CCU007277 (to T.L.M.).
Supplement sponsorship. Published as part of a supplement entitled “The 2009 H1N1 Influenza Pandemic: Field and Epidemiologic Investigations,” sponsored by the Centers for Disease Control and Prevention.
Potential conflicts of interest. S.C. has received consulting fees from Sanofi Pasteur for advising them on modelling the spread of varicella and varicella herpes zoster. All other authors: no conflicts.
References
- 1.Centers for Disease Control and Prevention (CDC) Swine influenza A (H1N1) infection in two children–Southern California, March–April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:437–439. [PubMed] [Google Scholar]
- 2.Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–2615. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 3.Zhao H, Joseph C, Phin N. Outbreaks of influenza influenza-like illness in schools in England and Wales, 2005/06. Euro Surveill. 2007;12 doi: 10.2807/esm.12.05.00705-en. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Smith A, Coles S, Johnson S, Saldana L, Ihekweazu C, O'Moore E. An outbreak of influenza A(H1N1)v in a boarding school in South East England, May-June 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.27.19263-en. pii: 19263. [DOI] [PubMed] [Google Scholar]
- 5.Health Protection Agency West Midlands H1N1v Investigation Team. Preliminary descriptive epidemiology of a large school outbreak of influenza A (H1N1)v in the West Midlands, United Kingdom, May 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.27.19264-en. pii: 19264. [DOI] [PubMed] [Google Scholar]
- 6.Kar-Purkayastha I, Ingram C, Maguire H, Roche A. The importance of school and social activities in the transmission of influenza A(H1N1)v: England, April–June 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.33.19311-en. pii: 19311. [DOI] [PubMed] [Google Scholar]
- 7.Glass LM, Glass RJ. Social contact networks for the spread of pandemic influenza in children and teenagers. BMC Public Health. 2008;8:61. doi: 10.1186/1471-2458-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mikolajczyk RT, Akmatov MK, Rastin S, Kretzschmar M. Social contacts of school and children the transmission of respiratory-spread pathogens. Epidemiol Infect. 2008;136:813–822. doi: 10.1017/S0950268807009181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cauchemez S, Valleron AJ, Boëlle PY, Flahault A, Ferguson NM. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452:750–754. doi: 10.1038/nature06732. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Swine-Origin influenza A (H1N1) virus infections in a school–New York City, April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:470–472. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Interim CDC guidance for nonpharmaceutical community mitigation in response to human infections with swine influenza (H1N1) virus. Available at: http://www.thebody.com/content/news/art51596.html. Updated 28 April 2009. Accessed 23 December 2009. [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Update on school (K-12) dismissal and childcare facilities: Interim CDC guidance in response to human infections with the 2009 influenza A H1N1 virus. Available at: http://www.cdc.gov/h1n1flu/K12_dismissal.htm. Updated 1 May 2009. Accessed 1 May 2009. [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Update on school (K-12) dismissal and childcare facilities: Interim CDC guidance in response to human infections with the 2009 influenza A H1N1 virus. 2009. Available at: http://www.capregboces.org/swineflu/PDFs/CDC%20Updated%20Interim%20Guidance%20on%20School%20K-12%20and%20Childcare%20Facilities%2005.05.09.pdf. Updated May 5, 2009. Accessed 23 December 2009. [Google Scholar]
- 14.Iuliano DA, Reed C, Guh A, et al. Notes from the field: outbreak of 2009 pandemic influenza A (H1N1) virus at a large public university in Delaware, April—May 2009. Clin Infect Dis. 2009;49:1811–1820. doi: 10.1086/649555. [DOI] [PubMed] [Google Scholar]
- 15.Calatayud L, Kurkela S, Neave PE, et al. Pandemic (H1N1) 2009 virus outbreak in a school in London, April—May 2009: An observational study. Epidemiol Infect. 2010;138:183–91. doi: 10.1017/S0950268809991191. Epub 20 Nov 2009. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) Interim guidance on case definitions to be used for investigations of novel influenza A (H1N1) cases. Available at: http://www.cdc.gov/h1n1flu/casedef.htm. Accessed 9 September 2009. [Google Scholar]
- 17.Emergency use authorization of rRT-PCR swine flu panel 2009. Available at: http://www.cdc.gov/h1n1flu/eua/testkit.htm. Accessed 8 January 2010. [Google Scholar]
- 18.Garcia-Garcia L, Valdespino-Gomez JL, Lazcano-Ponce E, et al. Partial protection of seasonal trivalent inactivated vaccine against novel pandemic influenza A/H1N1 2009: Case-control study in Mexico City. BMJ. 2009;339:b3928. doi: 10.1136/bmj.b3928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Effectiveness of 2008-09 trivalent influenza vaccine against 2009 pandemic influenza A (H1N1)–-United states, May—June 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1241–1245. [PubMed] [Google Scholar]
- 20.Kelly H, Grant K. Interim analysis of pandemic influenza (H1N1) 2009 in Australia: Surveillance trends, age of infection and effectiveness of seasonal vaccination. Euro Surveill. 2009;14 doi: 10.2807/ese.14.31.19288-en. pii: 19288. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC) Serum cross-Reactive Antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009;58:521–524. [PubMed] [Google Scholar]


