Abstract
Objectives: Influenza viruses constitute one of the most common pathogens that cause acute respiratory disease in children. The aim of this study is to present the contribution of influenza viruses to influenza-like illness (ILI) in children (aged<10 years old) in Northern Greece during six influenza seasons (2004-2010).
Materials and Methods: 1,242 pharyngeal swabs or/and washes from children younger than 10 years old, presented as ILI infections during the last six influenza seasons (2004-2005, 2005-2006, 2006-2007, 2007-2008, 2008-2009 and 2009-2010) were examined for influenza A and B by Real-time one step RT-PCR.
Results: Influenza viruses were detected in 431 (34.7%) of the 1,242 specimens. In a total of 372 specimens were positive for influenza A and 58 for influenza B. The majority of the infected young patients were 6-10 years old (51.9%).
Conclusion: Our results show that in N. Greece, influenza viruses type A and B contribute to ILI presenting infections at a rate of 34.7 % in children younger than 10 years old.
Keywords: Influenza viruses, children, North Greece
Introduction
Influenza A and B viruses cause winter-seasonal epidemics of respiratory illness, with reports of paediatric attack rates between 20% and 35%1. The rates of influenza infection are higher in children than adults, while the elderly have the highest mortality rate2. In addition, influenza is responsible for a significant number of hospitalizations among infants and children. As a result, the case of Influenza infection attracts great medical interest and research perspectives.
During April 2009, a novel H1N1 virus was detected in epidemiologically unrelated cases of influenza-like illness in California and was recognized to be the cause of a major outbreak of respiratory disease in Mexico. The virus was found to be an H1N1 virus that was antigenically and genetically unrelated to human seasonal influenza viruses and genetically related to viruses known to circulate in swine3.
In the beginning of April 2009, H1N1 influenza spread across the world. The World Health Organization (WHO) declared it a global pandemic, caused by the novel influenza virus. Over 213 countries and territories reported laboratory confirmed cases of pandemic (H1N1) 2009 with more than 16,813 deaths as of March 21, 20104.
The National Influenza Centre for northern Greece, which is located in the 2nd Microbiology Department of Medical School of Aristotle University of Thessaloniki, is one of the two National Influenza Centers in Greece, and it has been responsible for ILI surveillance in Greece since December 1999. In response to the health emergency declared by WHO, Greece set up an enhanced surveillance system for pandemic H1N1 2009 by the 30th of April 20095.
The purpose of this study is to report the influenza surveillance data in northern Greece between 2004 and 2010 influenza seasons in children aged 0-10 years old. For specific research purposes, the clinical symptomatology of the patients was taken under consideration.
Materials and methods
During 2004-2010 influenza seasons, pharyngeal swabs and/or washes were collected from a total of 1,242 paediatric patients (653 males and 588 females), younger than 10 years old from northern Greece, who were identified by clinicians as patients with ILI during the above influenza seasons. The specimens were collected within three days from the onset of symptoms and they were transported to the laboratory in sucrose phosphate medium within 24 hours at the temperature of 4° C. All specimens were sent to the National Influenza Centre for North Greece, accompanied by a Standard Form, presenting the necessary demographic data, date of illness onset, date of specimen collection, particular ILI symptoms and medical history of every case.
RNA extractions were performed using the Qiagen Viral RNA mini kit according to manufacturer’s instructions. The existence of influenza virus and its subtype (H1 or H3) was checked by real-time one step RT-PCR with specific primers and probes for matrix protein, nucleoprotein and haemaglutinin respectively, using the CDC influenza real-time RT-PCR kit, following WHO recommendations6.
All results were registered and kept as a record file for the National Influenza Centre for northern Greece and they were sent additionally to the Hellenic Centre for Disease Control and Prevention (HCIDC), following the determined guidelines.
Statistical analysis
Statistical analysis of the results was performed using the SPSS (version 16.0) software. For the different age groups and the infection rates were estimated by means of descriptive statistics. The chi-square test was used to compare the infections rates for influenza among different age groups.
Results
The patients were stratified into two age groups (0-5 years and 6-10 years old), by gender and geographical origin (Table 1). From November 2004 to May 2010, 1,242 specimens were sent for virus screening, while influenza viruses were detected in 431 of them (34.7%) (Table1). In total, 373 specimens were positive for influenza A and 58 for influenza B, while the seasonally distribution of the influenza virus infections are shown in Table 1.
Table 1. Influenza viruses infections in ILI cases in children <10 years old, Northern Greece, 2004-2010.
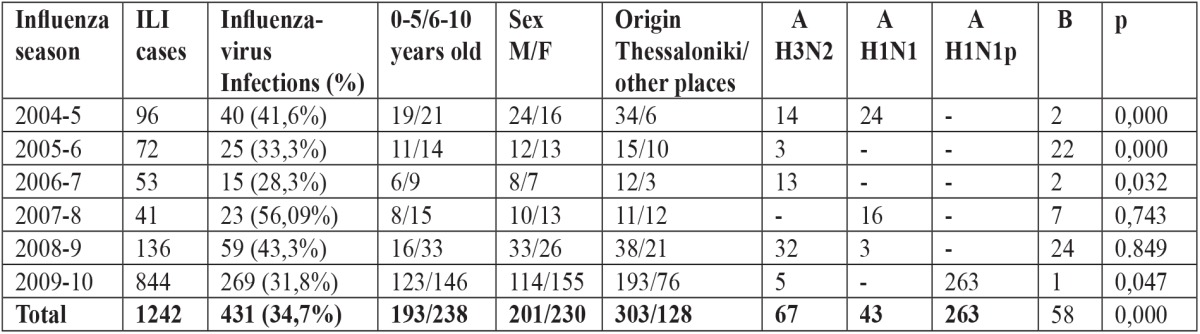
ILI: influenza-like illness.
The most common clinical findings in patients infected with influenza viruses were fever, rhinorrhoea and wheezing. Especially, for the 2009-2010 season, 66.91% of influenza infected patients developed mostly low temperature fever; still, 37 influenza positive patients developed fever > 40°C. Furthermore, in the same season, 180 ILI patients developed pneumonia, while 30 of them (16.6%) were positive for influenza A(H1pandemic), as determined by real-time RT-PCR. The majority of these patients belonged to the age group of 6-10 years old (16 patients). In addition, three patients developed myositis and three developed encephalitis, which were all infected by influenza A (H1 pandemic). Conjunctivitis was observed in 19 influenza positive patients during all seasons, while most of them (63%) were positive for influenza virus, type B.
Type A influenza viruses were predominant in five of the six seasons, while type B only in 2005-2006 season. Influenza viruses of the A(H3N2) subtype were recorded in 2006-2007 and 2008-2009 season, while in 2004-2005, 2007-2008 and 2009-2010 seasons most of the isolates belonged to the influenza A(H1N1) subtype (Table 1). The data indicate that the strains of influenza viruses that circulated in northern Greece in each season were similar to those circulating worldwide.
Age and geographical distribution of confirmed influenza viruses infections, as well as gender information are included in Table 1. According to the age distribution the majority (n=458, 36.8%) of the patients were 6-10 years old. The incidence of influenza infection was slightly higher in the age group of 6-10 years old, as 238 of 458 influenza-infected patients (51.9%) belonged to this group.
Statistical analysis of the results demonstrated that there was a statistically significant difference between the age groups and influenza infection in 2004-2005, 2005-2006 and 2006-2007 seasons. During those seasons, influenza virus positivity was higher in older children (6-10 yrs old). This trend was observed during the pandemic period (2009-2010) as well, but not such a statistical difference was found during the 2007-2008 and 2008-2009 seasons (Table 1).
Additionally, no statistically significant difference was observed in influenza positive infections regarding sex for each season and in total.
Discussion
Influenza viruses are the main pathogens which are associated with mild infections from upper respiratory system to severe pneumonia, especially in children.
The aim of the present study was to report the influenza surveillance data in Northern Greece, between years 2004 and 2010, in children younger than 10 years old. According to our results, influenza viruses contributed to respiratory infections at a rate of 34.7% (30.7% in males and 39% in females). Children aged 0-5 years old were influenza positive at a rate of 24.7%, while 51.9% of the 6-10 years old children were positive. The European Paediatric Influenza Analysis project, which was created in order to collect and analyze data regarding the paediatric influenza burden in European countries, presented the results from a study conducted in Netherlands during 2002-2008. Influenza positivity rates in children 0-4 years and 5-14 years old with respiratory infection were 47% and 62% respectively, while in Spain, influenza viruses were responsible for 80% of the respiratory infections in children 0-4 years old and 83% in children 5-14 years old7.
The influenza season 2009-2010, due to 2009 H1N1 influenza pandemic, started earlier (June 2009) than the previous years. In addition, the number of specimens which were examined was greater. The total number of the specimens examined was 884, while 269 of them were positive for influenza viruses, 97.3% of which belonged to subtype A (H1 pandemic). In a similar study conducted in Canada, during 2009-2010 season, the pandemic AH1N1 influenza virus was identified in 98.5% of the reported cases8.
Additionally, none of the children tested developed pneumonia until 2009-2010 season, in which 180 children with pneumonia were found and 30 (16.6%) of them were positive for influenza viruses, specifically A (H1 pandemic). This finding is probably due to an increased and extended surveillance during the 2009-2010 season. In a study conducted in the United States of America during 2003-2008, 36% of the children had influenza-associated pneumonia9. Furthermore, in a similar study in Bangladesh during 2004-2007 seasons, influenza infection was associated with 10% of all childhood pneumonia10. Our data report that the most common symptoms were fever, cough, catarrh, sore throat, fatigue, headache and muscle pain, which means that most cases of pandemic H1N1 2009 currently seem to have mild, uncomplicated clinical features. Influenza pneumonia which was not seen until the pandemic season was probably due to an extended surveillance during that period and not due to a potential increased pathogenicity of pandemic H1N1. This finding is consistent with reports from other countries11-13. In contrast, a previous study in United Kingdom demonstrates that H1N1/09 influenza is associated with more severe diseases than those with previous years’ Influenza A subtypes14.
Our data indicate that influenza viruses play an important role as a pathogen in respiratory infections in children. These infections are mostly associated with symptoms from the upper respiratory system. Older children, 6-10 years old, are most likely to be infected, while the incidence of influenza infection is slightly lower in younger children.
Finally, we must support the importance of surveillance activities in order to monitor the influenza epidemics each season and guide public health by collecting data on epidemiological parameters and mechanisms of virus transmission on the community. This data will also provide some of the scientific back up that will help support decisions regarding influenza vaccination recommendations for children in the country.
Conflict of Interest
The authors confirm that there is no conflict of interest associated with this publication and there has been no financial support for this work that could have influenced its outcome.
References
- 1.Aymard M, Valette M, Luciani J. Burden of influenza in children: preliminary data from a pilot survey network on community diseases. Pediatr Infect Dis J. 2003;22:S211–S214. doi: 10.1097/01.inf.0000092189.42748.cc. [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 3.Garten RJ, Davis CT, Russel CS, Shu B, Lindstrom S, Balish A, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Weekly virological surveillance update. Pandemic (H1N1) 2009-update 92, 2010. Available from: http://www.who.int/csr/disease/swineflu/en/index.html.
- 5.Panagiotopoulos T, Bonovas S, Danis K, Iliopoulos D, Dedoukou X, Pavli A, et al. Cluster of new influenza A(H1N1) cases in travellers returning from Scotland to Greece - community transmission within the European Union? Euro Surveill. 2009;14:19226. doi: 10.2807/ese.14.21.19226-en. [DOI] [PubMed] [Google Scholar]
- 6.CDC Real-time RT-PCR protocol for detection and characterization of swine influenza (version 2009) Centre of Disease Control. CDC ref: #I-007-05 [Google Scholar]
- 7.Paget WJ, Baldestron C, Casa I, Donker RGE, Edelman L, Flemong D, et al. Assessing the burden of paediatric influenza in Europe: the European Paediatric Influenza Analysis (EPIA) project. Eur J of Pediatr. 2010;169:997–1008. doi: 10.1007/s00431-010-1164-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bettinger JA, Sauvé LJ, Scheifele DW, Moore D, Vaudry W, Tran D, et al. Pandemic influenza in Canadian children: a summary of hospitalized pediatric cases. Vaccine. 2010;28:3180–3184. doi: 10.1016/j.vaccine.2010.02.044. [DOI] [PubMed] [Google Scholar]
- 9.Dawood FS, Fiore A, Kamimoto L, Nowell M, Reingold A, Gershman K, et al. Influenza-associated pneumonia in children hospitalized with laboratory-confirmed influenza, 2003-2008. Pediatr Infect Dis J. 2010;29:585–589. doi: 10.1097/inf.0b013e3181d411c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks WA, Goswami D, Rahman M, Nahar K, Fry AM, Balish A, et al. Influenza is a major contributor to childhood pneumonia in a tropical developing country. Pediatr Infect Dis J. 2010;29:216–221. doi: 10.1097/INF.0b013e3181bc23fd. [DOI] [PubMed] [Google Scholar]
- 11.Ciblak MA, Albayrak N, Odabas Y, Basak Atlas A, Kanturvardar M, Hasoksuz M, et al. Cases of influenza A(H1N1)v reported in Turkey, May-July 2009. Euro Surveill. 2009;14:19313. [PubMed] [Google Scholar]
- 12.European Centre for Disease Prevention and Control (ECDC) Surveillance Report. Pandemic (H1N1) 2009: Analysis of individual case reports in EU and EEA countries. Available from: http://ecdc.europa.eu/en/health-topics/Documents/090810_Influenza_A(H1N1)_Analysis_of individual_data_EU_EEA_EFTA.PDF.
- 13.Gioula G, Exindari M, Melidou A, Chatzidimitriou D, Chatzopoulou E, Malisiovas N. Epidemiological Surveillance of Pandemic H1N1 2009 infections in Northern Greece. Eur J Gen Med. 2010;7:240–244. [Google Scholar]
- 14.Herberg JA, Jones KD, Paulus S, Gomley S, Muir D, Cooper M, et al. Comparison of pandemic and seasonal influenza reveals higher mortality and increased prevalence of shock in children with severe H1N1/09 infection. Pediatr Infect Dis J. 2011;30:438–440. doi: 10.1097/INF.0b013e3182040c90. [DOI] [PubMed] [Google Scholar]


