Abstract
Objective
To assess the effectiveness of interventions to improve the mental health of women in the perinatal period and to evaluate any effect on the health, growth and development of their offspring, in low- and middle-income (LAMI) countries.
Methods
Seven electronic bibliographic databases were systematically searched for papers published up to May 2012 describing controlled trials of interventions designed to improve mental health outcomes in women who were pregnant or had recently given birth. The main outcomes of interest were rates of common perinatal mental disorders (CPMDs), primarily postpartum depression or anxiety; measures of the quality of the mother–infant relationship; and measures of infant or child health, growth and cognitive development. Meta-analysis was conducted to obtain a summary measure of the clinical effectiveness of the interventions.
Findings
Thirteen trials representing 20 092 participants were identified. In all studies, supervised, non-specialist health and community workers delivered the interventions, which proved more beneficial than routine care for both mothers and children. The pooled effect size for maternal depression was −0.38 (95% confidence interval: −0.56 to −0.21; I2 = 79.9%). Where assessed, benefits to the child included improved mother–infant interaction, better cognitive development and growth, reduced diarrhoeal episodes and increased immunization rates.
Conclusion
In LAMI countries, the burden of CPMDs can be reduced through mental health interventions delivered by supervised non-specialists. Such interventions benefit both women and their children, but further studies are needed to understand how they can be scaled up in the highly diverse settings that exist in LAMI countries.
Résumé
Objectif
Estimer l'efficacité des interventions visant à améliorer la santé mentale des femmes dans la période périnatale et évaluer tout effet sur la santé, la croissance et le développement de leur progéniture, dans les pays à faible et moyen revenus (PFMR).
Méthodes
On a étudié de manière systématique sept bases de données bibliographiques électroniques pour y trouver les articles, publiés jusqu'en mai 2012, décrivant les essais contrôlés d'interventions visant à améliorer la santé mentale des femmes enceintes ou ayant récemment accouché. Les principaux résultats intéressants étaient les taux des troubles mentaux périnataux communs (TMPC), la dépression ou l'anxiété, essentiellement après l'accouchement, les mesures de la qualité de la relation mère-nourrisson, ainsi que la mesure de la santé, de la croissance et du développement cognitif du nourrisson ou de l'enfant. Une méta-analyse a été effectuée pour obtenir une mesure synthétique de l'efficacité clinique des interventions.
Résultats
On a identifié treize essais représentant 20 092 participants. Dans toutes les études, des agents de la santé et des travailleurs communautaires non spécialistes supervisés ont effectué les interventions qui se sont avérées plus bénéfiques que les soins de routine pour les mères et les enfants. La taille de l'effet groupé de la dépression maternelle était de −0,38 (intervalle de confiance de 95%: −0,56 à −0,21; I2 = 79,9%). Dans les cas où ils étaient évalués, les avantages pour l'enfant comprenaient une meilleure interaction mère-enfant, un meilleur développement cognitif, une croissance supérieure, des épisodes diarrhéiques réduits et des taux accrus de vaccination.
Conclusion
Dans les PFMR, la charge des TMPC peut être réduite par des interventions de santé mentale prises en charge par des non-spécialistes supervisés. Ces interventions bénéficient à la fois aux femmes et à leurs enfants, mais d'autres études sont nécessaires pour comprendre comment elles peuvent être élargies aux paramètres très divers qui existent dans les PFMR.
Resumen
Objetivo
Determinar la efectividad de las intervenciones destinadas a mejorar la salud mental de las mujeres en el periodo perinatal y evaluar los efectos en la salud, el crecimiento y el desarrollo de sus hijos en los países de ingresos bajos y medios (PIBM).
Métodos
Se realizaron búsquedas sistemáticas en siete bases de datos bibliográficas electrónicas a fin de hallar trabajos, publicados antes de mayo de 2012, que describieran ensayos controlados de intervenciones diseñadas para mejorar el estado de salud mental de mujeres embarazadas o que habían dado a luz recientemente. Los resultados de mayor interés fueron: las tasas de trastornos mentales perinatales frecuentes (TMPF); la depresión o la ansiedad principalmente después del parto; las medidas de la calidad de la relación madre–hijo; así como la medida de la salud, el crecimiento y el desarrollo cognitivo de bebés y niños. Se realizó un metaanálisis para obtener una medida sinóptica sobre la efectividad clínica de las intervenciones.
Resultados
Se identificaron trece ensayos que representaron a un total de 20 092 participantes. En todos los estudios, las intervenciones se llevaron a cabo por personal de salud no especializado y por trabajadores comunitarios bajo supervisión, lo cual resultó ser más beneficioso que la atención rutinaria para madres y niños. El tamaño del efecto combinado de la depresión materna fue −0,38 (intervalo de confianza del 95 %: −0,56 a −0,21; l 2 = 79,9 %). En las zonas donde se realizó la evaluación, los beneficios para el niño incluían una mejora en la interacción madre-hijo, en el desarrollo cognitivo y el crecimiento, una reducción en los episodios de diarrea, así como un aumento en las tasas de inmunización.
Conclusión
En países de ingresos bajos o medios es posible reducir la carga por los trastornos mentales perinatales frecuentes mediante intervenciones de salud mental prestadas por personal no especializado bajo supervisión. Estas intervenciones benefician tanto a las mujeres como a sus hijos, pero se necesitan más estudios para averiguar cómo pueden ampliarse dentro de la gran diversidad de los países de ingresos bajos y medios.
ملخص
الغرض
تقييم فعالية التدخلات من أجل تحسين الصحة النفسية للنساء في الفترة المحيطة بالولادة وتقييم أي تأثير على صحة أطفالهن ونموهم وتطورهم، في البلدان المنخفضة والمتوسطة الدخل.
الطريقة
تم إجراء بحث في سبع قواعد بيانات بيبليوغرافية إلكترونية على نحو منهجي للحصول على الأبحاث المنشورة حتى أيار/ مايو 2012 التي تصف التجارب التي أجريت في بيئة خاضعة للمراقبة خاصة بالتدخلات المصممة لتحسين حصائل الصحة النفسية لدى النساء اللاتي حملن أو ولدن مؤخراً. وكانت الحصائل المهمة الرئيسية هي معدلات الاضطرابات النفسية الشائعة في الفترة المحيطة بالولادة، أو اكتئاب أو قلق ما بعد الولادة؛ وقياسات جودة العلاقة بين الأم والرضيع؛ وقياس صحة الرضيع أو الطفل والنمو والنمو الإدراكي. وتم إجراء تحليل وصفي للحصول على قياس موجز للفعالية السريرية للتدخلات.
النتائج
تم تحديد 13 تجربة تمثل 20092 مشاركاً. وفي جميع الدراسات، قام العاملون الصحيون والمجتمعيون غير المتخصصين الذين يعملون تحت الإشراف بإيتاء التدخلات، التي أثبتت فائدتها عن الرعاية الروتينية لكل من الأمهات والأطفال. وكان حجم الأثر المجمع لاكتئاب الأم -0.38 (فاصل الثقة 95 %: من -0.56 إلى -00.21؛ I 2 = 79.9 %). شملت الفوائد التي تعود على الطفل، عند تقييمها، تحسين تفاعل الأم مع الرضيع وتحسين النمو والنمو الإدراكي وتقليل نوبات الإسهال وازدياد معدلات التمنيع.
الاستنتاج
في البلدان المنخفضة والمتوسطة الدخل، يمكن تقليل عبء الاضطرابات النفسية الشائعة في الفترة المحيطة الولادة من خلال تدخلات الصحة النفسية التي يقدمها عاملون غير متخصصين يعملون تحت إشراف. وتفيد هذه التدخلات كلاً من النساء وأطفالهن، ولكن لابد من إجراء مزيد من الدراسات لفهم الكيفية التي يمكن من خلالها دعم هذه التدخلات في البيئات شديدة التنوع، التي توجد في البلدان المنخفضة والمتوسطة الدخل.
摘要
目的
评估中低收入(LAMI)国家旨在改善围产期妇女心理健康状况的干预措施的有效性,并评估对其后代的健康、成长和发育的任何影响。
方法
对七个电子文献数据库进行系统检索,查找描述旨在改善怀孕或者刚刚分娩的妇女精神健康效果的干预措施对照试验的论文,发表时间截至2012 年5 月。 关注的主要成果是围产期常见精神障碍(CPMD)率,主要是产后抑郁症或焦虑;母婴关系质量的衡量;以及婴儿或儿童健康、成长和认知发展的衡量。执行元分析获得干预措施临床效果的总体衡量。
结果
确定了十三个代表20092 名参与者的试验。在所有研究中,受监督的非专业卫生和社区工作者提供了干预措施,经证明这些措施比常规护理更有利于母亲和儿童。孕产妇抑郁症汇总效应大小是-0.38(95%置信区间:-0.56 至-0.21;I2 = 79.9%)。评估方面,对孩子的益处包括改善母婴互动、更好的认知发展和成长、更低的腹泻发作率和更高的免疫率。
结论
在LAMI国家,可通过由受监督的非专业人员提供精神健康干预措施,降低CPMD负担。这种干预措施对妇女及其孩子都有益处,但是要理解如何在LAMI国家高度多样化的环境中推广这些措施还需要进一步的研究。
Резюме
Цель
Оценить эффективность вмешательств для улучшения психического здоровья женщин в перинатальный период и оценить влияние на здоровье, рост и развитие их плода в странах с низким и средним уровнем доходов.
Методы
По семи электронным библиографическим базам данных проводился систематический поиск работ, опубликованных до мая 2012 года, в которых описывались контролируемые испытания вмешательств, направленных на улучшение психического здоровья беременных или недавно родивших женщин. Главными результатами исследования являлись уровни общих перинатальных психических расстройств (ОППР) (в основном послеродовой депрессии или беспокойства), оценки качества отношений между матерью и младенцем и оценка здоровья, роста и когнитивного развития младенцев и детей. Проводился мета-анализ для получения итоговой оценки клинической эффективности вмешательств.
Результаты
Было исследовано 13 испытаний, представляющих 20 092 участников. Во всех исследованиях вмешательства проводились контролируемыми медико-санитарными работниками-неспециалистами и они оказались более благотворными, чем система регулярного ухода как за матерями, так и за детьми. Общая величина эффекта при материнской депрессии составила −0,38 (доверительный интервал: от −0,56 до −0,21; I2 = 79,9%). Там, где проводилась оценка, благотворные воздействия на ребенка включали улучшение взаимодействия матери и младенца, лучшее когнитивное развитие и рост, уменьшенную частоту развития диареи и повышенный уровень иммунизации.
Вывод
В странах с низким и средним уровнем доходов бремя ОППР может быть уменьшено посредством проводимых контролируемыми неспециалистами вмешательств в области психического здоровья. Подобные вмешательства оказывают благотворное воздействие как на женщин, так и на детей, однако необходимо проведение дальнейших исследований для понимания того, как они могут быть увеличены в весьма различных условиях, имеющихся в странах с низким и средним уровнем доходов.
Introduction
Perinatal mental health problems are common worldwide.1 In high-income countries, about 10% of pregnant women and 13% of women who have just given birth experience a mental disorder, primarily depression or anxiety.2,3 A recent systematic review showed higher rates of common perinatal mental disorders (CPMDs) among women from low- and lower-middle-income countries, where the weighted mean prevalence of these disorders was found to be 15.6% (95% confidence interval, CI: 15.4–15.9) in pregnant women and 19.8% (95% CI: 19.5–20.0) in women who had recently given birth.4 The review identified several risk factors for CPMDs among women: having a partner lacking in empathy or openly antagonistic; being a victim of gender-based violence; having belligerent in-laws; being socially disadvantaged; having no reproductive autonomy; having an unintended or unwanted pregnancy; having pregnancy-related illness or disability; receiving neither emotional nor practical support from one’s mother, and giving birth to a female infant.4 The day-to-day interactions between neonates and their primary caregivers influence neurological, cognitive, emotional and social development throughout childhood. Maternal mental health problems are not only detrimental to a woman’s health; they have also been linked to reduced sensitivity and responsiveness in caregiving and to higher rates of behavioural problems in young children. There is growing evidence that, in low- and middle-income (LAMI) countries, the negative effects of maternal mental disorders on the growth and development of infants and young children are independent of the influence of poverty, malnutrition and chronic social adversity.5,6 In low-income settings, maternal depression has been linked directly to low birth weight and undernutrition during the first year of life, as well as to higher rates of diarrhoeal diseases, incomplete immunization and poor cognitive development in young children.7–10
In some high-income countries, including England and Australia, the detection and treatment of CPMDs are prioritized.11 However, this is not so in most LAMI countries, where many other health problems compete for attention.4 Psycho-educational interventions that promote problem solving and a sense of personal agency and help to reframe unhelpful thinking patterns, including cognitive behaviour therapy and interpersonal therapy, have consistently proven effective in the management of CPMDs.12,13 Although few LAMI countries have sufficient mental health professionals to meet their populations’ mental health needs,14 several have tried to deliver acceptable, feasible and affordable interventions based on evidence generated locally.15 The aims of this study were to investigate systematically the evidence surrounding the impact of such interventions on women and their infants and on the mother–infant relationship, and to understand the feasibility of applying them in LAMI countries.
Methods
Search strategy
We conducted a systematic search, without language restrictions, of seven electronic bibliographic databases: MEDLINE, EMBASE, CINAHL, PsycINFO, the British Nursing Index, the Allied and Complementary Medicine database and the Cochrane Central Register. The search terms were: depression, maternal depression, perinatal depression, postnatal depression, postpartum depression, common mental disorders, mental health and postpartum psychosis. These terms were individually combined with the terms randomized controlled trial, controlled clinical trial, clinical trials, evaluation studies, cross over studies AND with the names of countries classified as LAMI countries by the World Bank.16 China is a middle-income country. Despite ambiguity in its economic status, we included Taiwan, China, in the middle-income category. We hand-searched the reference lists of all included articles. When necessary, we also approached experts to identify unpublished studies.
We included all controlled trials from LAMI countries, published up to May 2012,17 that involved structured mental health interventions targeting women during pregnancy and after childbirth, or that measured maternal mental health outcomes up to 36 months postpartum. Two reviewers scanned the abstracts of all identified sources to determine eligibility independently. Disagreements were resolved consensually. Using a standard form, we extracted information on the following for all eligible studies: study design, study setting, sample characteristics, recruitment strategies, measures of mental health, main outcomes of interest and follow-up intervals. We also summarized the details of each intervention, including its acceptability to patients and providers, if assessed.
Data analysis
We undertook a meta-analysis of selected outcomes. We translated continuous outcomes to a standardized effect size (mean of intervention group minus mean of control group, divided by the pooled standard deviation); we translated dichotomous outcomes to a standardized effect size using conventional procedures.18 To maximize consistency, we chose the outcomes reported in the review a priori according to an algorithm. Thus, in studies that had more than one follow-up assessment, we chose the outcome for the assessment closest to 6 months after the intervention. If both categorical and continuous data were reported, we used the continuous data for the meta-analysis. To adjust for the precision of cluster trials, we used the methods recommended by the Cochrane Collaboration19 and assumed an intra-class correlation of 0.02. We conducted meta-analysis using random effects modelling to assess the pooled effect of maternal mental health interventions. The I2 statistic was used to quantify heterogeneity.20 To assess possible publication bias, we conducted the Egger test and generated a funnel plot.
Studies were heterogeneous in terms of the setting, nature and content of the interventions, as well as outcomes and outcome measures, so we also undertook a realist review using Pawson et al.’s method.21 With this method, similarities and differences between studies are considered on the basis of study design, methodological quality, intervention characteristics and delivery, presumed mode of action, fidelity of implementation, acceptability to participants, recognition of the sociocultural context and appropriateness of the outcome measures for the particular setting.
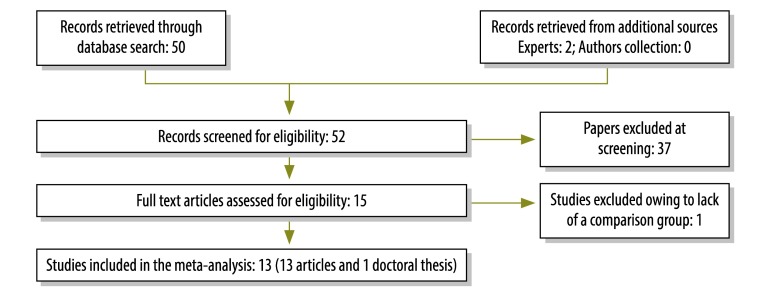
Results
Of the 52 records we retrieved, we retained 15 after screening. We excluded one study because it lacked a comparison group. The 13 eligible trials, described in 13 papers and a thesis, represented 20 092 participants. Their findings were used for the meta-analysis (Fig. 1).22–35 China contributed three trials; India, Pakistan and South Africa contributed two trials each, and Chile, Jamaica, Mexico and Uganda contributed one each. Twelve studies were controlled and randomized either at the individual or the cluster level and one study28 used a historical matched control from another epidemiological study. The main outcomes assessed were maternal mental health, the mother–infant relationship, and infant or child cognitive development and health.
Fig. 1.
Flowchart showing selection of studies on interventions for common perinatal mental disorders among women in low- and middle-income countries
Study characteristics and quality
In the trials, outcomes were assessed at one or more points from 3 weeks to 3 years after childbirth. The following self-reported symptom checklists were used in the different studies to assess maternal depression: the World Health Organization’s 20-item Self-reporting Questionnaire (SRQ-20),36 the Edinburgh Postnatal Depression Scale (EPDS),37 the 12-item General Health Questionnaire (GHQ-12),38 the nine-item Patient Health Questionnaire (PHQ-9),39 the Centre for Epidemiologic Studies Depression Scale (CES-D),40 the interviewer-administered Structured Clinical Interview for DSM-IV Axis 1 Disorders (SCID-I),41 the Mini International Neuropsychiatric Interview (MINI),42 the Hamilton Depression Rating Scale (HDRS),43 the Revised Clinical Interview Schedule (CIS-R),44 the 10-item Kessler Psychological Distress Scale (K10),45 the Short Form (36) Health Survey (SF-36),46 the Symptom Checklist-90-R (SCL-90-R)47 and the Beck Depression Inventory–II (BDI-II).48 In nine studies, the self-report measure was supplemented by a psychiatric interview (Table 1, available at: http://www.who.int/bulletin/volumes/91/8/12-109819).
Table 1. Design, methods and main findings of 13 trials of interventions for common perinatal mental disorders in women in low- and middle-income countries.
| Study | Location | Design | Inclusion/exclusion criteria, recruitment and retention | Baseline assessment and outcome measures | Main findings |
|---|---|---|---|---|---|
| Cooper et al., 200228 | Khayelitsha, a periurban settlement outside Cape Town, South Africa | Pilot investigation to inform a controlled trial, with comparison between two non-systematically recruited groups consisting of mother–infant pairs |
Inclusion criteria: intervention group, 40 women-infant pairs; comparison group, 32 mother–infant pairs, group-matched with survey participants in an adjacent area on at least two of maternal age, parity and marital status; Recruitment: strategy not specified; Retention: 32 of 40 (80%) mothers in intervention group followed up to the end of the project. No attrition in control group was reported. |
Baseline: No assessment. Outcomes (assessed at 6 months postpartum): – maternal mood – SCID-I for major depression in mothers; – mother–infant interaction – coded ratings of 5–10 minute video recordings of mother and infant during free play and feeding; – infant growth – infant weight, length and head circumference. |
Maternal mood: – major depression 19% (6/32) in intervention group; 28% (9/32) in comparison group; Mother-infant interaction: – after controlling for age and education, mothers in the intervention group were more sensitive in play (P = 0.02) and tended to show more positive affect during feeding (P = 0.08). Infant growth – infants in the intervention group were heavier (P = 0.01) and taller (P = 0.02), but no differences in head circumference or weight-to-height ratio were noted. |
| Baker-Henningham et al., 200522 | Nutrition clinics in Jamaica | Comparison between mother–infant pairs recruited from government clinics. Clinics were stratified by size of client population and randomly assigned to intervention (11) and control (7) arms |
Inclusion criteria: singleton infants aged 9 to 30 months; weight-for-age Z-score ≤ –1.5 at time of assessment and ≤ –2 in 3 most recent months; birth weight > 1.8 kg; absence of chronic disease or disability; Exclusion criteria: none stated; Recruitment: 70 of 76 (92%) eligible mother–infant pairs recruited for intervention arm; 69 of 70 (99%) eligible pairs recruited for control arm; Retention: 64 of 70 (91%) mother–infant pairs in intervention group and 61 of 69 (88%) pairs in control group were followed up to the end of the study. |
Baseline: parental sociodemographic characteristics, housing quality, maternal vocabulary on PPVT-R. Outcomes (assessed 1 year after recruitment): – maternal mood – culturally modified version of the CES-D to assess maternal depression; – child development – subscales of the Griffiths Mental Development Scale assessing: locomotor development, hearing and speech, hand–eye coordination and performance development to give a global developmental quotient (DQ); – child anthropometry – height-for-age, weight-for-height, and weight-for-age Z-scores of the NCHS growth reference. |
Maternal mood: – decline in depressive symptoms seen in intervention group but not in control group (β = –0.98; 95% CI: –1.53 to –0.41); – mothers receiving 40–50 home visits had greatest decline in depressive symptoms (β = −1.84; 95% CI: –2.97 to –0.72); – mothers receiving 25–39 home visits had lesser decline in depressive symptoms (β = −1.06; 95% CI: –2.02 to –0.11); – mothers receiving 0–24 home visits did not differ from control group (β = −0.09; 95% CI: –1.11 to 1.13). Child development – final maternal depression and final DQ correlated in boys (P < 0.05) but not in girls. |
| Rojas et al., 200723 | Primary care clinics in Santiago, Chile | Comparison between participants randomized to multi-component intervention or to regular primary health care |
Inclusion criteria: having a child aged ≤ 1 year old; being enrolled in one of the clinics; EPDS score ≥ 10 on two occasions 2 weeks apart; MINI diagnosis of major depression; Exclusion criteria: any treatment for depression since giving birth; pregnancy; psychotic symptoms; suicidal behaviour; history of mania or alcohol or substance abuse; Recruitment: of 313, 67 met at least one exclusion criterion and 16 refused; 230 of 246 (93%) recruited; Retention: in intervention group, 101 of 114 (89%) at 3 months and 106 of 114 (93%) at 6 months; in control group, 108 of 116 (93%) at 3 months and 102 of 116 (88%) at 6 months. |
Baseline: maternal age, marital status, occupation, parity, interval since giving birth and history of depression (EPDS, SF-36, MINI). Outcomes (assessed blindly 3 and 6 months after the intervention): – maternal mood – primary outcome: EPDS score; secondary outcomes: mental health, emotional role, social functioning and vitality dimensions of the SF-36 and clinical improvement. |
Maternal mood: – EPDS scores improved in multi-component intervention at 3 months (–4.5 difference in mean scores between groups [95% CI: –6.3 to –2.7; P < 0.0001]); – EPDS scores were at least 3 points lower (95% CI: 3–29) at 6 months than at baseline in 73% of the intervention group and 57% of the usual care group. |
| Rahman et al., 200825 | Union Council clusters in two sub-districts: Gujar Khan and Kallar Syedan in rural Pakistan | Comparison between women living in 40 union councils that had been randomized independently to intervention (20) and control (20) groups |
Inclusion criteria: being married; being 16 to 45 years old; being, in the third trimester of pregnancy; meeting SCID-I criteria for major depressive episode; Exclusion criteria: serious medical condition or pregnancy-related illness; significant learning or intellectual disability; postpartum or other psychosis; Recruitment: inclusion criteria were met by 463 of 1787 (26%) women in intervention councils and by 440 of 1731 (25%) women in control councils; Retention: in intervention group, 418 of 463 (90%) mothers at 6 months and 412 of 463 (89%) at 12 months; in control group, 400 of 412 (91%) mothers at 6 months and 386 of 412 (88%) at 12 months; in intervention group, 368 (79%) infants at 6 months and 360 (78%) at 12 months; in control group, 359 (82%) at 6 months and 345 (78%) at 12 months. |
Baseline: maternal age, education, family structure, parity, socioeconomic status and financial empowerment; HDRS, Brief Disability Questionnaire, Global Assessment of Functioning, self-assessment of adequacy of social support. Outcomes (assessed blindly): – maternal mood – psychiatrist-administered HDRS and SCID-I at 6 and 12 months postpartum to assess maternal depression; – infant health and development – infant weight and length; number of diarrhoeal episodes in previous fortnight and infant immunization status; – family health and functioning – maternal reports of exclusive breastfeeding, use of contraception and time dedicated to infant play. |
Maternal mood – after adjusting for covariates women in the intervention group: – were less likely to be depressed at 6 months postpartum (23% vs 53%; aOR: 0.22; 95% CI: 0.14–0.36; P < 0.0001); – were less likely to be depressed at 12 months postpartum (27% vs 59%; aOR 0.23; 95% CI: 0.15–0.36; P < 0.0001); – were less disabled at 6 months (aMD: −1.80; 95% CI –2.48 to –1.12; P < 0.0001) and at 12 months (aMD: –2.88; 95% CI –3.66 to –2.10; P < 0.0001); – had better global functioning at 6 months (aMD: 6.85; 95% CI: 4.73–8.96; P < 0.0001) and at 12 months (aMD: 8.27; 95% CI: 6.23–10.31; P < 0.0001); – had better perceived social support at 6 months (aMD: 6.71; 95% CI: 3.93–9.48; P < 0.0001) and at 12 months (aMD: 7.85; 95% CI: 5.43–10.27; P < 0.0001). Infant health and development: – no difference between groups in infant stunting or malnutrition; – infants of intervention group mothers had fewer episodes of diarrhoea at 12 months (aOR: 0.6; 95% CI: 0.39–0.98; P = 0.04) and were more likely to be fully immunized (aOR: 2.5; 95% CI: 1.47–4.72; P = 0.001). Family health and functioning: – intervention group more likely to be using contraception at 12 months (aOR: 1.6; 95% CI: 1.20–2.27; P = 0.002); – both parents dedicated time to playing with the infant (aOR for mothers: 2.4; 95% CI: 2.07–4.01; P < 0.0001; aOR for fathers: 1.9; 95% CI: 1.59–4.15; P = 0.0001). |
| Rahman et al., 200924 | Kallar Syedan, a Union Council district of 60 villages in a rural area south-east of Rawalpindi, Pakistan | 48 of 60 villages accessible by road. Comparison between mothers and infants living in villages randomly assigned to the intervention (24) or to usual care (24) |
Inclusion criteria: being married; being 17–40 years old; being in the third trimester of pregnancy; being registered with a lay health worker; Exclusion criteria: serious medical condition or complication of pregnancy; Recruitment: of 367 women, 334 met inclusion criteria and agreed to participate: 177 of 194 (91%) in intervention villages and 157 of 173 (90%) in control villages; Retention: 163 of 177 (92%) women in intervention group and 146 of 157 (93%) women in control group. |
Baseline: – maternal age, education and parity and family income and structure; – maternal knowledge and attitudes about infant development in the first 8 weeks of life using an original infant development questionnaire; – maternal emotional distress using the SRQ-20, locally field-tested and validated. Outcomes (assessed blindly at 3 months postpartum): – maternal knowledge about infant development; – infant development questionnaire; – maternal emotional distress SRQ-20. |
Maternal knowledge about infant development – intervention group had significantly higher increase in questionnaire scores than control group at 3 months postpartum (aOR: 4.28; 95% CI: 3.68–4.89; P < 0.0001); Maternal emotional distress – no difference in SRQ-20 scores between intervention and control groups. |
| Cooper et al., 200926 | Khayelitsha, South Africa | Comparison between women, identified systematically during pregnancy via home visits and randomly assigned to intervention or standard care using minimization procedures to control for antenatal depression and unintended pregnancy |
Inclusion criteria: living in one of the two study areas; being in the third trimester of pregnancy; Exclusion criteria: none; Recruitment: 449 of 452 eligible women recruited: 220 assigned to intervention group and 229 to control group; Retention: 354 of 449 (78.8%) at 6 months; 346 of 449 (77%) at 12 months and 342 of 449 (76%) at 18 months. Retention lower among younger women than among older women (P < 0.05). |
Baseline: No assessment. Outcomes (assessed in a purposely-built accessible facility with a one-way mirror and video-recorders): – mother–infant interaction – at infant age of 6 months, video tapes of 10 minutes of free play independently scored to assess maternal sensitivity and intrusiveness; at infant age of 1 year, observations of maternal ability to facilitate play; – infant attachment – at infant age of 18 months, the Strange Situation Procedure; – maternal depression – at 6 months postpartum, SCID-I interviews, which incorporated the EPDS, administered in Xhosa by a trained research worker, taped and then scored with a clinical psychologist. |
Mother-infant interaction – intervention group significantly more sensitive and less intrusive in interactions with infants at both 6 and 12 months (all P < 0.05); Infant attachment: – more securely attached infants in intervention group than in control group (OR: 1.70; P < 0.029); – higher rates of anxious–avoidant attachment in control than intervention group. Maternal depression: – lower prevalence of depression in intervention than control group at 6 and 12 months postpartum, but differences not significant; – EPDS scores lower in intervention than control group at both assessment points, but difference only significant (P = 0.04) at 6 months; – depression ratings unrelated to maternal sensitivity or intrusiveness. |
| Ho et al., 200933 | Taipei and Taiwan, China | Comparison between primiparous women assigned alternatively on day one postpartum to intervention or control group. Women in shared wards were assigned as a group |
Inclusion criteria: being married; being primiparous; being 20–25 years old; having had a spontaneous vaginal delivery; having had a singleton, at-term infant weighing ≥ 2500 g and with an APGAR score > 8; Exclusion criteria: postnatal complications or psychiatric history; Recruitment: numbers meeting eligibility criteria not reported. Of 240 invited, 200 were recruited and 100 were assigned to each arm; Retention: 83 of 100 (83%) women in intervention group and 80 of 100 (80%) women in control group were followed up to the end of the project. |
Baseline: no baseline assessment; sociodemographic characteristics assessed at 6 weeks. Outcomes: – maternal mood – EPDS score and “experience of postnatal depression” assessed at 6 and 12 weeks postpartum. |
Maternal mood: – no differences between groups in sociodemographic factors or “postnatal experiences”; – no difference between groups in EPDS score > 9 at 6 weeks (21% intervention versus 30% control, P = 0.2) or at 3 months (11% intervention versus 16% control, P = 0.3) postpartum; – both groups experienced improvement in mood over time. |
| Gao et al., 201029 & 201230 | A regional teaching hospital in southern mainland China | Comparison between groups randomly assigned to intervention and control arms |
Inclusion criteria: being married; being nulliparous; being < 36 years old; being > 28 weeks pregnant; Exclusion criteria: having a complicated pregnancy or a psychiatric history; Recruitment: 194 of 262 (74%) eligible women recruited: 96 assigned to intervention group and 98 to control group; Retention: 87 of 96 (90%) women in intervention group and 88 of 98 (89%) women in control group. |
Baseline: Sociodemographic characteristics, EPDS, GHQ-12, SWIRS. Outcomes (assessed at 6 and 12 weeks postpartum): – maternal mood – EPDS, GHQ-12, and SWIRS completed at obstetric clinic visits. |
Maternal mood: – intervention group significantly lower EPDS (95% CI: –3.48 to –1.09); GHQ-12 (95% CI: –1.29 to 0.33) and SWIRS mean scores (95% CI: 0.31–1.25) than control group at 6 weeks postpartum; – difference in proportion with EPDS scores > 12 in intervention (9.38%) and control (17.35%) not significant (P = 0.1) at 6 weeks postpartum; – intervention group significantly lower mean scores on EPDS (5.61 vs 6.87; P < 0.01) and GHQ-12 (1.44 vs 1.71; P < 0.01) at 3 months postpartum. |
| Tripathy et al., 201034 | Saraikela Kharswan, West Singhbhum and Keonjjhar districts in Jharkand and Orissa states, India | Comparison between women living in control and intervention communities from July 2005 to July 2008. Clusters stratified by whether or not women’s groups were available, then allocated to intervention and control groups by a transparent number-drawing process on site |
Inclusion criteria: being 15–49 years old; being pregnant and giving birth during the study period; being a resident of a study district; Exclusion criteria: none, but data from women who migrated out of the study area were excluded from intention-to-treat analyses. |
Baseline: no assessment of individual women. Outcomes: – neonatal mortality rate – maternal and neonatal deaths assessed by key informant (usually a traditional birth attendant) surveillance system and verbal autopsies; – maternal mood – structured interviews about sociodemographic characteristics, antepartum, intrapartum and postpartum health and health care and the K10 in 2nd and 3rd years of the study. |
Neonatal mortality ratio – 55.6, 37.1 and 36.3 per 1000 births in intervention clusters vs 53.4, 59.6 and 64.3 in control clusters in the 3 years of the study. Overall, 32% lower in intervention than in control clusters (aOR: 0.68; 95% CI: 0.59–0.78); 45% lower in years 2 and 3 (aOR: 0.55; 95% CI: 0.46–0.66); Maternal mood – no significant differences between groups overall, but moderate depression (K10: 16–30) 5% in intervention and 10% in control group in year 3 of the study (aOR 0.43; 95% CI: 0.23–0.80); Infant care – clean birth care practices and rates of exclusive breastfeeding at 6 weeks higher in intervention than control groups. |
| Lara et al., 201031 | Mexico City, Mexico | Comparison of depression rates at 3 and 6 weeks and at 4 to 6 months postpartum in women randomly assigned to intervention and to regular antenatal care |
Inclusion criteria: ≥ 18 years old; ≤ 26 weeks pregnant; completed primary school; Exclusion criteria: substance abuse or bipolar conditions; reported suicide attempts during the last six months; Recruitment: from the waiting rooms of: (i) a hospital providing intensive care for women with high-risk pregnancies; (ii) a women's clinic for partners and/or wives of men in the armed forces; and (iii) a community health-care centre. Intervention group: 117 pregnant women; comparison group: 250 pregnant women; Recruitment rate: 70.2%; Retention: 27.2% women in intervention group and 53.6% in control group. |
Baseline: demographic and obstetric data; SCID-I; BDI-II, SCL-90-R. Outcomes: – maternal mood; – major depression: SCID-I interviews for DSM-IV diagnoses of major depression in mothers; – depressive symptoms: BDI-II, cut-off point of 14; – anxiety symptoms: SCL-90-R, cut-off point of 18. |
Maternal mood: – cumulative incidence of major depression over three time periods was 10.7% in intervention and 25% in control group (P < 0.05); – significant reduction of BDI-II score in both groups, but no significant treatment effect; – most participants who completed the intervention reported that it had a moderate to large influence on their well-being, mood, ability to cope with problems, role as mothers and relationship with their infants. |
| Mao et al., 201232 | First Hospital of Hangzhou, Zhejiang, China | Comparison of depression rates at 6 weeks postpartum in pregnant women randomly assigned to an emotional self-management training programme or to standard antenatal care |
Inclusion criteria: being healthy and nulliparous; having a single pregnancy; Exclusion criteria: “puerpera of old age” (age not specified); pregnancy complications; personal or family history of psychiatric disorder; Recruitment: 240 of 532 (45.1%) eligible women recruited and randomized to intervention (120) and control (120) groups; Retention: 113 of 120 (94%) women in intervention group and 108 of 120 (90%) women in control group. |
Baseline: socio-demographic characteristics, PHQ-9. Outcomes: – maternal mood – depression: PHQ-9 score ≥ 10, EPDS, SCID-I, interviewed by the first author who was blind to group allocation. |
Maternal mood: – at 6 weeks postpartum, intervention group had significantly lower mean PHQ-9 (P < 0.01) and EPDS scores (P = 0.04) than control group; – fewer in intervention group with SCID-I diagnosis of major depression (OR = 0.29; 95% CI: 0.21–1.01). |
| Hughes, 200927 | Goa, India | Pregnant women identified through 138 anganwadi centres and randomly assigned to intervention or standard care arms |
Inclusion criteria: being in the third trimester of pregnancy; being able to speak English or Konkani; scoring ≥ 5 on GHQ-12, or having an unplanned pregnancy, or having a “male child fixation”; Exclusion criteria: having a severe health condition; intending to leave area during study period; having frequent thoughts of harming self; Recruitment: of 1320 pregnant women, 62 were ineligible and 76 did not attend the screening interview. Of the 1173 women screened, 565 (48.1%) met inclusion criteria, 142 (25.1%) met at least one exclusion criterion and 1 declined. Remaining 422 women at “high risk of postnatal depression” randomly assigned to intervention group (212) or standard care (210); Retention: 187 of 212 (88.2%) women in intervention group and 181 of 210 (86.2%) women in control group. |
Baseline: – socioeconomic factors; parity, gestational age; feelings about the pregnancy and past psychiatric history; – maternal mood assessed by locally validated EPDS and CIS-R. Outcomes (assessed blindly): – maternal mood – EPDS score and meeting CIS-R assessed ICD diagnostic criteria for depression at 3 months postpartum; – infant development – DAS-II mental development quotient ; maternal report of infant birth weight; infant weight at 12 and 26 weeks postpartum. |
Maternal mood (with control for between-group differences in sociodemographic factors) – no difference between groups in EPDS score > 12 (7.7% vs 7.8%; uOR: 1.01; 95% CI: 0.51–2.01). Infant development – no difference between groups in DQ < 85 (12.1% vs 10.0%; uRR: 0.82; 95% CI: 0.45–1.49); no differences in mean infant weight between intervention and control groups. |
| Morris et al., 201235 | Camps for internally displaced people in Kitgum district, Northern Uganda | Comparison between women attending three Kitgum emergency feeding centres (intervention group) and women attending two other centres (control group) |
Inclusion criteria: having a moderately or severely malnourished infant aged 6 to 30 months; being enrolled in a feeding centre; Exclusion criterion: infant requiring inpatient care; Recruitment: all 132 eligible women agreed to participate in the intervention; 105 were in control group; Retention: 106 of 132 (80.3%) women in intervention group and 52 of 105 (49.5%) in control group. |
Baseline: sociodemographic characteristics and years in camp. Outcomes: – maternal knowledge of child development – 10-item Knowledge, Attitudes and Practice test; – mother–infant relationship – Acholi adaptation of the HOME Inventory to assess maternal involvement, variety, punishment, play materials, emotional and verbal responsiveness, acceptance and organization; – maternal mood –study-specific, culturally appropriate Kitgum Maternal Mood Scale developed through multiple methods to assess sadness, irritability and somatic complaints. |
Maternal knowledge about child development – no effect of the intervention and the measure found to have poor internal consistency. Mother–infant relationship – mothers in intervention group more emotionally responsive (OR: 2.97; 95% CI: 0.71–5.23) and used more play materials (OR: 2.16; 95% CI: 1.22–3.10) than those in the control group. Maternal mood – no differences between groups when interview location controlled. |
aMD, adjusted mean difference; aOR, adjusted odds ratio; BDI-II, Beck Depression Inventory II; CES-D, Center for Epidemiologic Studies Depression Scale; CI, confidence interval; CIS-R, Revised Clinical Interview Schedule; DASII, Development Assessment Scales for Indian Infants; DQ, developmental quotient; EPDS, Edinburgh Postnatal Depression Scale; GHQ-12, 12-item General Health Questionnaire; HDRS, Hamilton Depression Rating Scale; HOME, Home Observation and Measurement of the Environment; ICD, International Classification of Diseases; K10, 10-item Kessler Psychological Distress Scale; MINI, Mini International Neuropsychiatric Interview; NCHS, National Center for Health Statistics; OR, odds ratio; PHQ-9, nine-item Patient Health Questionnaire; PPVT-R, Peabody Picture Vocabulary Test – revised; SCID-I, Structured Clinical Interview for DSM-IV Diagnoses; SCL-90-R, Symptom Checklist-90-R; SF-36, Short Form (36) Health Survey; SRQ-20, 20-item Self-Reporting Questionnaire; SWIRS, Satisfaction with Interpersonal Relationships Scale; uOR, unadjusted odds ratio; uRR, unadjusted relative risk.
Intervention characteristics
The interventions varied in content and structure, mode of implementation and method of assessing acceptability to providers and participants (Table 2, available at: http://www.who.int/bulletin/volumes/91/8/12-109819). Four studies addressed maternal depression directly. Rahman et al.’s25 multimodal approach in the Thinking Healthy Programme (THP) included specific cognitive behaviour therapy methods to identify and modify maladaptive thinking styles – e.g. fatalism, inability to act, superstitious explanations and somatization – and replace them with more adaptive ways of thinking.49 It aimed to improve women’s social status by using the family’s shared commitment to the infant’s well-being as an entry point. Mao et al.32 also used a culturally adapted approach based on cognitive behaviour therapy to teach emotional self-management, including problem-solving and cognitive re-framing, in a facilitated group programme. Rojas et al.23 sought to maximize the uptake of antidepressant pharmacotherapy and treatment compliance. Their intervention also involved professionally-led, structured psycho-educational groups that focused on symptom recognition and management, including problem-solving and behavioural strategies. Hughes et al.27 focused on a specific social determinant that had been identified in their study site, namely, the “male child fixation” in pregnant women whose older children were all female.50 This problem was addressed through specific education about sex determination and strategies to empower women to challenge ill-informed reactions devaluing the birth of a female child.
Table 2. Nature of interventions for common perinatal mental disorders in low- and middle-income countries and acceptability to consumers and providers.
| Study | Nature of intervention | Recipient and provider perceptions |
|---|---|---|
| Cooper et al., 200228 | Adaptation of the Health Visitor Intervention Programme by incorporating principles of WHO’s Improving the Psychosocial Development of Children programme to: – enhance emotional support for the mother – promote sensitivity in interacting with infant – use items from the NBAS to sensitize mother to infant’s abilities – provide specific practical advice about management of infant sleep, crying and feeding. Home visits to mothers were made twice antenatally, twice weekly during first month after birth; weekly for next 8 weeks; fortnightly for next month and monthly for next 2 months (a total of 20 visits). |
Recipients: moderate to strong agreement among recipients on four-point fixed choice questionnaire items: – 94% said provider “made me feel supported”; “‘was on my side”; “I could trust and talk openly to her” – 90% said provider “really understood how I felt” – 100% said provider “‘made me appreciate the things my baby can do”’ – 90% said provider “‘helped me to solve problems I was having with my baby”; “helped me understand my child’s needs”; “showed me how to respond to what my child was doing”. |
| Baker-Henningham et al., 200522 | Weekly home visits lasting half an hour to: – improve mothers’ knowledge of child-rearing practices and parenting self-esteem – use homemade toys, books and household items to demonstrate age-appropriate activities for the child by involving mother and child in play – provide experiences of mastery and success for mother and child; – emphasize the importance of praise, responsiveness, nutrition, appropriate discipline and play and learning; – friendly, empathic approach, but no specific focus on problem solving or on addressing maternal concerns – standard health and nutrition care offered at clinics. |
No data about recipient or provider perceptions reported. |
| Rojas et al., 200723 | A multi-component intervention that included: – eight weekly structured psycho-educational groups to convey information about symptoms and treatments and to teach problem solving and behavioural activation strategies and cognitive techniques using examples illustrative of the postnatal period – structured cost-free pharmacotherapy protocol of fluoxetine (20–40 mg per day) or sertraline (50–100 mg per day) for women who did not respond to fluoxetine or were lactating – medical appointments at weeks two and four and thereafter monthly for 6 months to monitor clinical progress and treatment compliance. |
No data about recipient or provider perceptions reported. |
| Rahman et al., 200825 | Thinking Healthy Programme (THP), a manualized intervention incorporating cognitive and behavioural techniques of active listening and collaboration with family; non-threatening enquiry into the family’s health beliefs, a challenging of wrong beliefs, and substitution of these with alternative information when required; and inter-session practice activities. It is designed to be integrated into existing maternal and child health education home visits. Intervention group received: one THP session per week for the last month of pregnancy, three sessions in the first postpartum month and one session per month for the subsequent nine months (a total of 16 sessions). |
Providers: LHWs trained in THP reported that the intervention was relevant to their work and did not constitute an extra workload. |
| Rahman et al., 200924 | Learning Through Play (LTP) programme, developed for use by lay home visitors in Canada and adapted for use in low-income countries. It includes images demonstrating infant development, parent–child play activities and skilled parenting practices conducive to normal cognitive, social and emotional development in the child. The images are accompanied by simple text for groups with low literacy and are presented together as a calendar demonstrating developmental progress. A training manual for providers with additional information about child development is used as a supplement, together with group sessions or one-to-one sessions with parents. Intervention group received a half-day session on LTP in late pregnancy, with a calendar for home use. Mothers were subsequently visited for 15–20 minutes once a fortnight to discuss their infants’ development, using the calendar as a reference point, until infants turned 12 weeks old. Participants were encouraged to meet informally in groups to apply the techniques in the calendar and provide mutual support to each other. |
LHW (n = 24) feedback on the LTP training showed that: – 87.5% agreed fully or partially that the intervention was relevant to their work – 84% said that it was easy to integrate into their routine tasks – 100% felt that the concepts were understandable – 84% felt they could communicate the concepts to mothers in their care. |
| Cooper et al., 200926 | Same adaptation of the Health Visitor Intervention Programme incorporating principles of WHO’s Improving the Psychosocial Development of Children programme, as used in Cooper et al. (2002)28 to: – enhance maternal sensitivity and responsiveness towards infants and mother–infant interaction – use items from the NBAS to sensitize mothers to their infants’ abilities and needs – hour-long home visits to mothers made twice antenatally, weekly for the first 8 weeks after birth, fortnightly for the next 2 months and monthly for another 2 months (a total of 16 visits, finishing at infant age of 5 months) – standard health care, which included a fortnightly home visit from a community health worker who assessed maternal and infant health and encouraged mothers to attend the local clinic for infant immunization and weight checks. |
Strong support from the local community for the health workers and the project. Low dropout rates, suggesting that the assessments were acceptable to participants. |
| Ho et al., 200933 | The education programme included a printed three-page booklet containing the incidence, symptoms, causes and management information about the postpartum depression. Women in the experimental group received the booklet and discussed it with primary care nurses on the second day after delivery. | No data about recipient or provider perceptions reported. |
| Gao et al., 201029 & 201230 | Intervention embedded in the antenatal childbirth psycho-education programme. In addition to routine antenatal care (two 90-minute classes), the intervention group received two “interpersonal psychotherapy-oriented” classes lasting two hours each and a postpartum follow-up telephone call to reinforce principles. Classes included information-giving, clarification, role playing and brainstorming about new roles and strategies to manage relationships with husbands and mothers-in-law, supplemented by written material. | Women in the study group completed the classes with an attendance rate of 95.8%. |
| Tripathy et al., 201034 | Monthly intervention consisting of facilitated women’s group meetings in intervention clusters. The groups involved a participatory action cycle with a focus on maternal and neonatal health: clean births and care seeking. Contextually appropriate case studies used to identify and prioritize perinatal health problems, select strategies to address them (including prevention, home-care support and consultations), implement the strategies and assess results. Maternal depression not a direct focus of the intervention but potentially improved by social support of the group and acquisition of problem-solving skills. | No data about recipient or provider perceptions reported. |
| Lara et al., 201031 | Eight weekly sessions lasting 2 hours each and with no more than 15 participants per group. Intervention programme that included: (i) information about the “normal” perinatal period and risk factors for postpartum depression; (ii) a psychological component, aimed at reducing depression through various strategies (e.g. increasing positive thinking and pleasant activities, improving self-esteem and self-care), and (iii) a group component designed to create an atmosphere of trust and support. Control participants received the usual care provided by their institutions, and both groups received copies of a self-help book on depression especially designed for women with limited reading abilities. The book included a directory of community mental health services in the area. |
High proportion of participants reported the impact of the intervention on their depression as having been moderate (60%) or major (23%). |
| Mao et al., 201232 | Emotional Self-Management Group Training (ESMGT) programme comprising 4 weekly group sessions and one individual counselling session. Each group session lasted for 90 minutes. Group session topics included self-management, effective problem solving, positive communication, relaxation, cognitive restructuring and improving self-confidence. On completion of group training, one individual counselling session was arranged to address personal problems. Control group received standard antenatal education at the study venue. This consisted of four 90-minute sessions conducted by obstetrics nurses. The content of the programme focused on preparation for childbirth. |
All participants completed the 4-week ESMGT programme. |
| Hughes, 200927 | Home visits lasting 45 minutes made twice antenatally and three times postnatally (at 4, 7 and 10 weeks, for a total of 5 visits). Visits involved supportive, empathic listening and education intended to: – provide information within a relationship of trust – focus on gender determination to help women overcome the notion that infant sex is maternally determined – conduct client-centred postpartum discussions, including demonstrations of infant massage. |
No data about recipient or provider perceptions reported. |
| Morris et al., 201235 | The intervention, derived from the LTP Play programme, was in addition to intensive feeding and included: – culturally appropriate psycho-education about early childhood development – given in mother–infant group sessions, which also provided opportunities to share experiences and discuss the new information – supplemented by home visits – there were six mother–infant groups at weekly intervals, with an unspecified number of home visits. |
No data about recipient or provider perceptions reported. However, nine women who had received the intervention initiated groups spontaneously in their own locations to assist other mothers, which suggests that they experienced the intervention as being worthwhile. |
LHW, lay health worker; NBAS, Neonatal Behavioural Assessment Scale; THP, Thinking Health Programme; WHO, World Health Organization.
Two studies in China29,33 and one in Mexico31 addressed adjustment to motherhood through programmes integrated into existing hospital-based antenatal education or postpartum health care. These studies also took a psycho-educational approach, with structured content provided in a psychologically supportive context. Gao et al.’s programme29 was derived from interpersonal therapy and used learning activities and the social support of a group process to promote a problem-solving approach, including ways to manage interpersonal conflict in intimate relationships. Ho et al.33 and Lara et al.31 provided information about the symptoms and causes of postpartum depression in an information booklet and supplemented this with either supportive discussion with a primary care nurse to encourage early help-seeking behaviour,33 or participation in a series of group discussions facilitated by professionals.31
Five studies22,24,26,28,35 did not address maternal mental health directly. However, the researchers hypothesized that individual parenting education provided by a supportive home visitor or within the context of a mother’s group might also improve maternal depression and improve infant health and development. In South Africa, Cooper et al.26,28 demonstrated what neonates could do using a neonatal assessment scale. In a study conducted by Baker-Henningham et al.22 in Jamaica and in the adapted Learning Through Play (LTP) programmes implemented in Pakistan24 and northern Uganda,35 mothers were shown age-appropriate play activities and how to craft toys out of affordable, accessible materials to stimulate infant cognitive development. In broad terms, the theoretical rationale underpinning these approaches was that optimal child development requires maternal caregiving that attends explicitly to development in the physical, social, emotional and cognitive domains. The interventions carried out in these five studies aimed to enhance mothers’ knowledge about normal child development, improve maternal sensitivity and responsiveness towards infants and, through group programmes,24,35 reduce social isolation and improve maternal mood by means of peer support.
Tripathy et al.’s intervention34 also addressed maternal depression indirectly. It focused on educating mothers about pregnancy, birth, neonatal health and health-care seeking through locally designed illustrative case studies and stories. With the help of a trained local woman, community participatory action groups devised local interventions designed to reduce maternal and neonatal morbidity, with potential flow-on benefits for maternal mental health.
All studies except those from China and Mexico were conducted with participants of low socioeconomic status who experienced difficulties that could have contributed to their mental health problems. In these studies, the social determinants of perinatal depression in women were either reported as relevant by participants or explicitly recognized on a theoretical level.24–28,35 Such determinants include, for example, living in poor and overcrowded housing, suffering social exclusion as a result of illiteracy and unemployment, being a victim of the gender stereotypes that restrict women’s social participation or underpin hostility towards women, and experiencing social instability and neighbourhood violence.22 No study addressed these determinants directly.
All the studies drew on evidence generated in high-income countries. However, authors acknowledged that such evidence could not be transferred directly to resource-constrained settings and that, before being adopted, the interventions had to be supported by local evidence about effectiveness, affordability, acceptability and cultural appropriateness. The study interventions were all assessed in settings with very few specialists in mental health. Chile, China and Mexico were the only countries where the interventions were implemented by mental health professionals.23,29,31,33 In all other studies they were implemented by local trained community health workers under professional supervision. In seven interventions involving individual home visits,22,24–28,35 the therapeutic relationship between the health worker and the study participant was regarded as an important determinant of improvements in mental health. In this relationship, trust was of utmost importance. Equally important was the selection of local health workers who understood their clients’ sociocultural circumstances and who possessed basic psychological counselling skills, including knowing how to listen and to be non-judgmental, empathic and supportive. In settings where many women lived in multigenerational households, members of the extended family were engaged during home visits to reduce women’s reticence and encourage long-term behaviour change.22,24
Effects on maternal mental health
Psychiatric labels and the conceptualization of illness differed widely among studies. In Rojas et al.’s intervention,23 participants were assessed for depression and received education about symptom recognition and the importance of compliance with psychotropic medication. Some interventions were applied to women in the general community;22,24,29,34,35 others were applied only to women who were attending programmes not specifically dealing with mental health.29,33 In these interventions, mental health was assessed by means of symptom checklists rather than diagnoses or psychiatric assessment. Although all participants in the THP met the diagnostic criteria for depression, the intervention was positioned as a maternal and child health promotion strategy in which the use of psychopathological labelling was likely to have increased stigma and reduced compliance.25
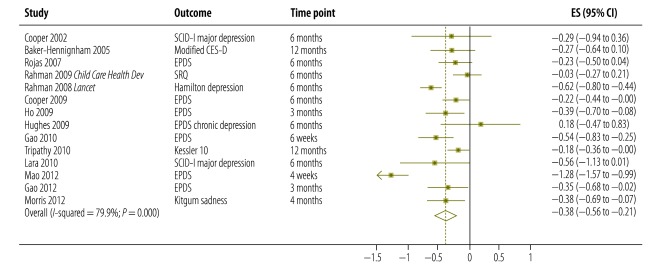
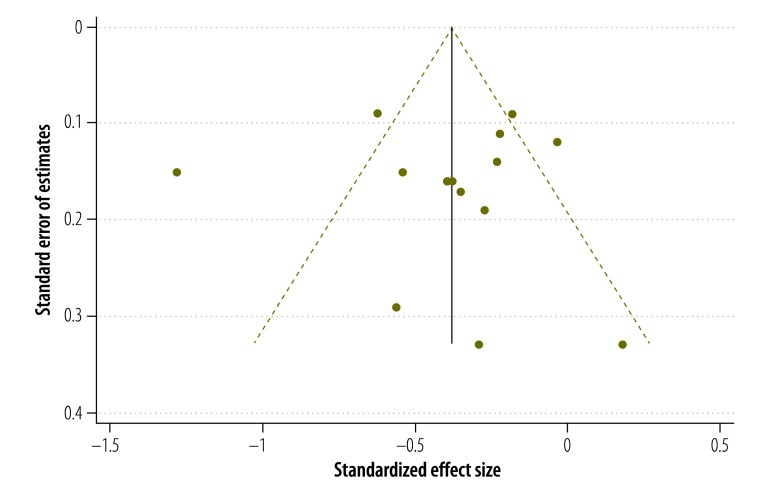
All 13 studies reported outcome data on maternal depression that was sufficiently detailed to be included in a meta-analysis. The resulting pooled effect size was −0.38 (95% CI: –0.56 to −0.21; I2 = 79.9%) (Fig. 2). The funnel plots were symmetrical (Fig. 3). Egger test statistics confirmed the lack of asymmetry indicative of publication bias (P = 0.97).
Fig. 2.
Forest plot presenting the standardized effect size (and 95% confidence intervals, CI) for 13 interventions for common perinatal mental disorders among women in low- and middle-income countries
CES-D, Center for Epidemiologic Studies Depression Scale; EPDS, Edinburgh Postnatal Depression Scale; ES, effect size; SRQ-20, 20-item Self-Reporting Questionnaire; SCID-I, Structured Clinical Interview for DSM-IV Axis 1 Disorders.
Note: Weights are from random effects analysis.
Fig. 3.
Funnel plot showing the standardized effect sizea and pseudo 95% confidence limits for 13 interventions for common perinatal mental disorders among women in low- and middle-income countries
a Mean of intervention group minus mean of control group, divided by the pooled standard deviation.
Two trials assessed secondary maternal psychological outcomes. Rojas et al.23 reported that women who received multi-component group therapy were more compliant with their antidepressant drug schedules, attended primary care more frequently and had better functioning, as measured by the SF-36, than those in the usual care group. Women in the THP intervention clusters in Pakistan25 had less disability, better overall functioning and greater perceived social support at their two follow-up assessments than women in the control group.
Child health and development
Direct, between-study comparisons of the effects of the various interventions on infant health and development are limited by differences in design, intervention content, the age at which outcomes were measured and the parameters that were assessed. Six of the 13 interventions22,24,25,27,28,34 aimed specifically to enhance infant health and development either by improving maternal knowledge, sensitivity, responsiveness or caregiving skills, or, less directly, by improving maternal mood (Table 2).
In three studies that focused specifically on child health and development, information on the benefits of age-appropriate activities for stimulating cognitive capacity and of structured parent–infant play was provided during home visits by community health workers.22,24,35 Women who participated in the LTP programme in Pakistan showed significantly better knowledge about their infants’ needs and development than those who had received standard care.24 Even under crisis conditions in Uganda, there was a notable improvement in mothers’ use of play materials to stimulate their infants in the Acholi adaptation of the LTP programme.35 In a Jamaican programme, mothers were shown how to engage their infants’ interest with affordable toys, picture books and household materials,22 and the results showed a negative association between the development quotient in boys – not girls – and the number of depressive symptoms found in the mother. None of these studies reported specifically on child health or physical development.
In an intervention conducted by Hughes,27 anganwadi workers explained to mothers, using dolls, how massaging their infants could improve child development. No differences were noted in child health and development outcomes, but average weight was significantly lower in infants whose mothers were at high risk of becoming depressed. The THP study aimed to improve child health by reducing maternal depression. Although infant stunting and low weight were not improved, infants experienced fewer episodes of diarrhoea and rates of completion of the recommended immunization schedule improved.25
The mother–infant relationship
Six interventions sought to improve the relationship between mother and infant as a primary26,28,35 or subsidiary22,25 goal (Table 1). The pooled effect size of the corresponding interventions was 0.36 (95% CI: 0.22–0.51).
In Cooper et al.’s studies,26,28 which focused on the mother–infant relationship, behavioural assessment items were used to show mothers what their infants could do (e.g. tracking objects with their eyes or imitating others’ facial expressions) and the reciprocal influence of the infant–child interaction. In one of the two studies, mothers were given direct, tailored advice about how to recognize and respond to normal infant needs in a manner intended to make the mother–infant interaction more gratifying and to enhance maternal competence and self-confidence.28 The pilot intervention led to improved infant weight and length.28 Cooper et al.’s studies were the only ones that assessed the quality of the mother–infant relationship through independent scoring of videotaped interactions. Mothers’ sensitivity and expressions of affection towards their infants improved, and, in one trial, rates of secure infant–mother attachment increased.26
The interventions conducted by Baker-Henningham et al.22 were manifold. They included demonstrations of activities for stimulating infants’ cognitive development; praise for mothers who showed sensitivity and imagination in their interactions with their infants, and facilitator-initiated discussions about infant nutrition. A less direct but explicit approach was used in two Pakistani studies that focused specifically on the mother–infant relationship. In these studies,25 the THP sought to help mothers become more aware of their infants’ needs and replace “unhealthy” thoughts about their infants with more productive thinking based on improved knowledge. In LTP programmes in Pakistan and Northern Uganda, as a way to stimulate discussion mothers were shown educational images illustrating activities that they could engage in with their infants.24,35
In the two Pakistani studies, the interventions’ beneficial effect on maternal depression and on the mother–infant relationship was assumed to be attributable to a common pathway: that improving maternal knowledge, caregiving skills, sensitivity and responsiveness towards infants enhances the mother–infant interaction and maternal self-efficacy and satisfaction. Mood lifting effects were demonstrated to some degree. Morris et al.35 found no improvement in maternal sadness or irritability when they controlled for the effects of interview site and baseline scores, but Baker-Henningham et al.22 and Rahman et al.25 did note improvements in maternal depression. In Rahman et al.’s study, knowledge about infant care improved not just among mothers, but also among fathers; as a result of the THP, both parents became more playful with their infants, with potential flow-on benefits in terms of the parent–infant relationship and the infants’ cognitive, social and emotional development.25 Overall the interventions had significant positive effects on growth, development and rates of infectious diseases among infants, and they resulted in lower neonatal mortality (Table 3).
Table 3. Outcomes of interest, effect measures and effect sizes from studies of interventions for common perinatal mental disorders among women in low- and middle-income countries .
| Outcome of interest | No. of trials | No. of participants | Effect measure | Effect size |
|---|---|---|---|---|
| Maternal depression | 13a | 15 429 | SMD (95% CI) | –0.38 (–0.56 to –0.21) |
| At 3 or 4 months postpartum | 5 | 943 | SMD (95% CI) | –0.59 (–0.95 to –0.24) |
| At 6 months postpartum | 7 | 1945 | SMD (95% CI) | –0.27 (–0.50 to –0.05) |
| At 12 months postpartum | 2 | 12 541 | SMD (95% CI) | –0.19 (–0.36 to –0.04) |
| Infant health and development | 6b | 14 029 | SMD (95% CI) | Separate dimensions onlyc |
| Infant growth | 3 | 1125 | SMD (95% CI) | 0.19 (0.07 to 0.31) |
| Infant development | 2 | 473 | SMD (95% CI) | 1.57 (0.28 to 2.85) |
| Infant infectious disease rate | 1 | 705 | OR (95% CI) | 0.60 (0.39 to 0.98) |
| Neonatal mortality rate | 1 | 12 431 | OR (95% CI) | 0.68 (0.59 to 0.78) |
| Mother–infant relationship | 4 | 1123 | SMD (95% CI) | 0.36 (0.22 to 0.51) |
CI, confidence interval; OR, odds ratio; SMD, standardized mean difference.
a There are 14 outcomes because among trials in which maternal depression was an outcome of interest, one collected data at two time points, each reported in separate papers.
b There are seven outcomes because among trials presenting infant health and development outcomes, one reported two outcomes.
c Since diverse infant outcomes were assessed, they cannot be combined and are reported separately.
Discussion
This is the first systematic review of the evidence surrounding interventions for the relief of CPMDs. Its findings show that such interventions can be effectively implemented in LAMI countries by trained and supervised health workers in primary care and community settings. The results are concordant with the findings of meta-analyses of psychological and psychosocial intervention studies for perinatal depression from high-income countries, which report a summary relative risk of 0.70 (95% CI: 0.60–0.81) for women in the intervention arm versus controls receiving standard care.13
There was substantial heterogeneity in estimated treatment effects, but the small number of studies precludes a meaningful assessment of the reasons for the variation. The psychotherapeutic content of the interventions, the number of therapy sessions, and staff training and supervision practices may have differed across studies. This is true of the THP in Pakistan25 and of the anganwadi intervention in India conducted by Hughes et al.,27 which had the largest and the smallest impact, respectively. The THP in Pakistan was based on cognitive behaviour therapy combined with active listening, measures for strengthening the mother–infant relationship and mobilization of family support. The anganwadi intervention, on the other hand, was based on a more general supportive psycho-educational approach. The interventions also differed in intensity: 1625 sessions as opposed to 5, respectively.27 Although the THP had a shorter training period (3 days compared with 1 month for the anganwadi workers), the Lady Health Workers in Pakistan had monthly half-day supervision throughout the intervention. This suggests that continuous supervision is more effective than one-off training.
Our findings suggest that the relationship between maternal mood and infant health and development is not unidirectional. Interventions in which mothers are taught about infant development and are shown how to engage and stimulate their infants and to be more responsive and affectionate towards them appear to improve maternal mood, in addition to strengthening the mother–infant relationship and leading to better infant health and development outcomes. Similarly, interventions expressly designed to improve maternal mental health have a positive impact on infant health and development. An intervention’s effect on infant health and development appears to be stronger when the maternal and infant components are integrated and infant health is a direct, rather than an incidental focus of the intervention.
Collectively, the studies in this review provide important lessons in terms of service development. First, approaches that are culturally adapted and grounded in cognitive, problem-solving and educational techniques can be applied effectively to groups or individuals. Most of the interventions described in the studies targeted mothers and infants and were conducted in women’s homes. In settings where women live in multigenerational households, this approach makes it possible to engage the whole family in the common pursuit of caring for the new infant. In all the studies, except for Lara et al.’s in Mexico, the interventions were delivered by supervised, non-specialist health and community workers without any training in mental health care. Thus, the studies provide evidence of the feasibility of training such workers to deliver mental health interventions effectively in a relatively short time. For low-income countries, where mental health professionals are scarce and tend to concentrate in big cities, this has important implications.51,52
A second lesson learnt is that the psychological and educational components of the interventions must be adapted to the circumstances in which women in LAMI countries live. In places where women live in densely populated communities and crowded households, involving the entire family and community in their care tends to be more beneficial than an individualistic approach. Interventions that engage the family can mitigate some important risk factors for depression in women: a poor sense of personal agency, pejorative and limiting gender stereotypes, lack of financial autonomy and intimate partner coercion and violence.
Common perinatal mental disorders are difficult to recognize. Furthermore, the fear of stigma can make women and their families reluctant to seek care. In the studies included in this review, health workers integrated the mental health interventions into their regular work activities, which may prove less stigmatizing to women. Maternal mental health and infant development interventions appear to act synergistically and the perinatal period provides an opportunity to deliver them in an integrated fashion. These data indicate that community-based approaches are beneficial and might be preferable to stand-alone vertical programmes. They may also be relevant to high-income countries, where providing equitable mental health services is becoming increasingly costly.15
No interventions targeting the more severe perinatal mental disorders, such as postpartum psychosis or suicidal behaviour, were found in this review. Future studies should address this gap. Nevertheless, our meta-analysis provides grounds for believing that the large global burden of CPMDs, particularly perinatal depression in women, can be addressed in resource-constrained settings through appropriate interventions. District-level primary care programmes providing integrated training and supervision and outcomes assessed in the general community are required to inform strategies for taking such interventions to scale.
Acknowledgements
We thank the authors of trials who provided additional information for our review and meta-analysis.
Funding:
The study was sponsored by the Department of Mental Health and Substance Abuse of the World Health Organization, the United Nations Population Fund (UNFPA) and Compass, the Women’s and Children’s Health Knowledge Hub funded by the Australian Agency for International Development (AusAID) and the Victorian Operational Infrastructure Support Programme. The views expressed in this article do not necessarily represent the decisions, policy or views of WHO, the UNPFA or AusAID. The authors had full control over the analysis and reporting of the results.
Competing interests:
None declared.
References
- 1.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 2.O'hara MW, Swain AM. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry. 1996;8:37–54. doi: 10.3109/09540269609037816. [DOI] [Google Scholar]
- 3.Hendrick V, Altshuler L, Cohen L, Stowe Z. Evaluation of mental health and depression during pregnancy: position paper. Psychopharmacol Bull. 1998;34:297–9. [PubMed] [Google Scholar]
- 4.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139G–49G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart RC. Maternal depression and infant growth: a review of recent evidence. Matern Child Nutr. 2007;3:94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engle PL. Maternal mental health: program and policy implications. Am J Clin Nutr. 2009;89:963S–6S. doi: 10.3945/ajcn.2008.26692G. [DOI] [PubMed] [Google Scholar]
- 7.Patel V, DeSouza N, Rodrigues M. Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Arch Dis Child. 2003;88:34–7. doi: 10.1136/adc.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry. 2004;61:946–52. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 9.Rahman A, Lovel H, Bunn J, Iqbal Z, Harrington R. Mothers’ mental health and infant growth: a case-control study from Rawalpindi, Pakistan. Child Care Health Dev. 2004;30:21–7. doi: 10.1111/j.1365-2214.2004.00382.x. [DOI] [PubMed] [Google Scholar]
- 10.Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrhoeal illness: a cohort study. Arch Dis Child. 2007;92:24–8. doi: 10.1136/adc.2005.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Australian Government Department of Health and Ageing [Internet]. National Perinatal Depression Initiative. Canberra: AGDHA; 2013. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/mental-perinat [accessed 11 May 2013].
- 12.National Collaborating Centre for Mental Health. Antenatal and postnatal mental health: the NICE guideline on clinical management and service guidance London: The British Psychological Society & The Royal College of Psychiatrists; 2007. [PubMed] [Google Scholar]
- 13.Dennis C, Hodnett E. Psychosocial and psychological interventions for treating postpartum depression (review) London: JohnWiley & Sons Ltd; 2009. [DOI] [PubMed] [Google Scholar]
- 14.Mental health atlas. Geneva: WHO Department of Mental Health and Substance Abuse; 2005. [Google Scholar]
- 15.Patel V, Kirkwood B. Perinatal depression treated by community health workers. Lancet. 2008;372:868–9. doi: 10.1016/S0140-6736(08)61374-4. [DOI] [PubMed] [Google Scholar]
- 16.World Bank [Internet]. World Bank development indicators. Washington: World Bank; 2005. Available from: http://data.worldbank.org/about/country-classifications/country-and-lending-groups [accessed 15 May 2013].
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lipsey MW, Wilson DB. Practical meta-analysis Thousand Oaks: Sage Publications; 2001. [Google Scholar]
- 19.Alderson P, Bero L, Eccles M. Effective Practice and Organisation of Care Group (Cochrane Collaborative Review Groups). London: John Wiley and Sons; 2005. [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review–a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(Suppl 1):21–34. doi: 10.1258/1355819054308530. [DOI] [PubMed] [Google Scholar]
- 22.Baker-Henningham H, Powell C, Walker S, Grantham-McGregor S. The effect of early stimulation on maternal depression: a cluster randomised controlled trial. Arch Dis Child. 2005;90:1230–4. doi: 10.1136/adc.2005.073015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, González M, et al. Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet. 2007;370:1629–37. doi: 10.1016/S0140-6736(07)61685-7. [DOI] [PubMed] [Google Scholar]
- 24.Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child Care Health Dev. 2009;35:56–62. doi: 10.1111/j.1365-2214.2008.00897.x. [DOI] [PubMed] [Google Scholar]
- 25.Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. 2008;372:902–9. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, et al. Improving quality of mother–infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ. 2009;338:b974. doi: 10.1136/bmj.b974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hughes MWA. Randomised, controlled trial of a perinatal psycho-social intervention for postnatal depression in Goa, India [thesis]. London: University of London & King's College London Institute of Psychiatry; 2009. [Google Scholar]
- 28.Cooper PJ, Landman M, Tomlinson M, Molteno C, Swartz L, Murray L. Impact of a mother-infant intervention in an indigent peri-urban South African context: pilot study. Br J Psychiatry. 2002;180:76–81. doi: 10.1192/bjp.180.1.76. [DOI] [PubMed] [Google Scholar]
- 29.Gao LL, Chan SW, Li X, Chen S, Hao Y. Evaluation of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women: a randomised controlled trial. Int J Nurs Stud. 2010;47:1208–16. doi: 10.1016/j.ijnurstu.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Gao LL, Chan SW, Sun K. Effects of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women at 3-month follow up: randomised controlled trial. Int J Nurs Stud. 2012;49:274–81. doi: 10.1016/j.ijnurstu.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 31.Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: a randomized control trial. J Affect Disord. 2010;122:109–17. doi: 10.1016/j.jad.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 32.Mao HJ, Li HJ, Chiu H, Chan WC, Chen SL. Effectiveness of antenatal emotional self-management training program in prevention of postnatal depression in Chinese women. Perspect Psychiatr Care. 2012;48:218–24. doi: 10.1111/j.1744-6163.2012.00331.x. [DOI] [PubMed] [Google Scholar]
- 33.Ho SM, Heh SS, Jevitt CM, Huang LH, Fu YY, Wang LL. Effectiveness of a discharge education program in reducing the severity of postpartum depression: a randomized controlled evaluation study. Patient Educ Couns. 2009;77:68–71. doi: 10.1016/j.pec.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 34.Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375:1182–92. doi: 10.1016/S0140-6736(09)62042-0. [DOI] [PubMed] [Google Scholar]
- 35.Morris J, Jones L, Berrino A, Jordans MJ, Okema L, Crow C. Does combining infant stimulation with emergency feeding improve psychosocial outcomes for displaced mothers and babies? A controlled evaluation from northern Uganda. Am J Orthopsychiatry. 2012;82:349–57. doi: 10.1111/j.1939-0025.2012.01168.x. [DOI] [PubMed] [Google Scholar]
- 36.A user's guide to the Self Reporting Questionnaire (SRQ). Geneva: World Health Organization; 1994. [Google Scholar]
- 37.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 38.Goldberg D, Williams P. A user's guide to the General Health Questionnaire. Oxford: NFER-Nelson Publishing Company Ltd; 1988. [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 41.First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for Axis I DSM-IV disorders New York: Biometrics Research; 1994. [Google Scholar]
- 42.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33,quiz 34-57. [PubMed] [Google Scholar]
- 43.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med. 1992;22:465–86. doi: 10.1017/S0033291700030415. [DOI] [PubMed] [Google Scholar]
- 45.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–76. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 46.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): conceptual framework and item selection. Med Care. 1992;30:473–83. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Derogatis LR. SCL-90-R: Symptom Checklist-90-R: administration, scoring, and procedures manual Bloomington: NCS Pearson, Inc.; 1996.
- 48.Beck A, Steer R, Brown G. Manual for beck depression inventory II (BDI-II) San Antonio: Psychology Corporation; 1996. [Google Scholar]
- 49.Rahman A. Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan–a multi-method study. Arch Womens Ment Health. 2007;10:211–9. doi: 10.1007/s00737-007-0193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159:43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 51.Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, et al. Mental health systems in countries: where are we now? Lancet. 2007;370:1061–77. doi: 10.1016/S0140-6736(07)61241-0. [DOI] [PubMed] [Google Scholar]
- 52.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–89. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]