Abstract
Objective
To explore the relationship between weather phenomena and pollution levels and daily hospital admissions (as an approximation to morbidity patterns) in Hong Kong Special Administrative Region (SAR), China, in 1998–2009.
Methods
Generalized additive models and lag models were constructed with data from official sources on hospital admissions and on mean daily temperature, mean daily wind speed, mean relative humidity, daily total global solar radiation, total daily rainfall and daily pollution levels.
Findings
During the hot season, admissions increased by 4.5% for every increase of 1 °C above 29 °C; during the cold season, admissions increased by 1.4% for every decrease of 1 °C within the 8.2–26.9 °C range. In subgroup analyses, admissions for respiratory and infectious diseases increased during extreme heat and cold, but cardiovascular disease admissions increased only during cold temperatures. For every increase of 1 °C above 29 °C, admissions for unintentional injuries increased by 1.9%. During the cold season, for every decrease of 1 °C within the 8.2–26.9 °C range, admissions for cardiovascular diseases and intentional injuries rose by 2.1% and 2.4%, respectively. Admission patterns were not sensitive to sex. Admissions for respiratory diseases rose during hot and cold temperatures among children but only during cold temperatures among the elderly. In people aged 75 years or older, admissions for infectious diseases rose during both temperature extremes.
Conclusion
In Hong Kong SAR, hospitalizations rise during extreme temperatures. Public health interventions should be developed to protect children, the elderly and other vulnerable groups from excessive heat and cold.
Résumé
Objectif
Étudier la relation entre les phénomènes météorologiques, les niveaux de pollution et les hospitalisations quotidiennes (en guise d'approximation des schémas de morbidité) dans la région administrative spéciale (RAS) de Hong Kong, Chine, de 1998 à 2009.
Méthodes
Des modèles additifs généralisés et des modèles de latence ont été élaborés avec des données provenant de sources officielles relatives aux admissions hospitalières et à la température quotidienne moyenne, à la vitesse moyenne quotidienne du vent, à l'humidité relative moyenne, au rayonnement solaire global total quotidien, aux précipitations quotidiennes totales et aux niveaux de pollution quotidiens.
Résultats
Pendant la saison chaude, les admissions ont augmenté de 4,5% pour chaque augmentation de 1 ºC au-dessus de 29 ºC; pendant la saison froide, les admissions ont augmenté de 1,4% pour chaque diminution de 1 ºC entre 8,2 et 26,9 ºC. Dans les analyses des sous-groupes, les admissions pour des maladies respiratoires et infectieuses ont augmenté pendant les périodes de chaleur et de froid extrêmes, mais les admissions dues aux maladies cardiovasculaires ont seulement augmenté par temps froid. Pour chaque augmentation de 1 ºC au-dessus de 29 ºC, les admissions pour blessures involontaires ont augmenté de 1,9%. Pendant la saison froide, pour chaque baisse de 1 ºC entre 8,2 et 26,9 ºC, les admissions pour maladies cardiovasculaires et blessures intentionnelles ont augmenté de 2,1% et 2,4%, respectivement. Les schémas d'admission n'étaient pas différents selon le sexe. Les admissions pour maladies respiratoires des enfants ont augmenté avec les températures chaudes et froides, mais celles des personnes âgées seulement avec les températures froides. Chez les personnes âgées de 75 ans ou plus, les admissions pour maladies infectieuses ont augmenté durant les deux périodes de températures extrêmes.
Conclusion
À Hong Kong, les hospitalisations augmentent pendant les périodes de températures extrêmes. Des interventions de santé publique devraient être développées pour protéger de la chaleur et du froid excessifs les enfants, les personnes âgées et les autres groupes vulnérables.
Resumen
Objetivo
Explorar la relación entre los fenómenos meteorológicos, los niveles de contaminación y los ingresos hospitalarios diarios (como una aproximación a los patrones de morbilidad) en la Región Administrativa Especial de Hong Kong (RAE), China, de 1998 a 2009.
Métodos
Se diseñaron modelos aditivos generalizados y modelos de retardos con datos de fuentes oficiales sobre los ingresos hospitalarios y la temperatura diaria media, la velocidad media diaria del viento, la humedad relativa media, la radiación solar global total diaria, las precipitaciones diarias totales, así como los niveles de contaminación diaria.
Resultados
Durante la época de calor, los ingresos se incrementaron en un 4,5 % por cada aumento de 1 °C por encima de 29 °C; durante la época de frío, los ingresos aumentaron un 1,4 % por cada disminución de 1 °C en el rango de 8,2 a 26,9 °C. En los análisis de subgrupos, los ingresos por enfermedades respiratorias e infecciosas aumentaron durante las temperaturas extremas de calor y frío; sin embargo, los ingresos debidos a enfermedades cardiovasculares solo aumentaron con las temperaturas frías. Por cada aumento de 1 °C por encima de 29 °C, los ingresos por lesiones involuntarias aumentaron un 1,9 %. Durante la época de frío, por cada disminución de 1 °C en el rango de 8,2 a 26,9 °C, los ingresos por enfermedades cardiovasculares y por lesiones causadas de forma intencionada aumentaron, respectivamente, un 2,1 % y un 2,4 %. El sexo de los pacientes no se tuvo en cuenta en los patrones de admisión. Los ingresos por enfermedades respiratorias aumentaron durante las temperaturas altas y bajas entre los niños, pero solo se incrementaron en los ancianos durante las temperaturas bajas. En las personas de 75 años o más, los ingresos por enfermedades infecciosas aumentaron durante ambos extremos de temperatura.
Conclusión
En la Región Administrativa Especial de Hong Kong, el número de hospitalizaciones aumenta durante las temperaturas extremas. Es necesario desarrollar intervenciones en materia de salud pública a fin de proteger a niños, ancianos y otros grupos vulnerables frente a las temperaturas extremas de calor y frío.
ملخص
الغرض
استعراض العلاقة بين ظواهر الطقس ومستويات التلوث ودخول المستشفيات يومياً (كتقريب لأنماط المراضة) في إقليم هونغ كونغ الإداري الخاص (SAR) بالصين، في الفترة من 1998 إلى 2009.
الطريقة
تم بناء نماذج مضافة عامة ونماذج تأخر باستخدام البيانات المأخوذة من المصادر الرسمية المعنية بدخول المستشفيات وبمتوسط درجة الحرارة اليومية وبمتوسط سرعة الرياح اليومية وبمتوسط الرطوبة النسبية وبإجمالي الإشعاع الشمسي العالمي اليومي وبإجمالي سقوط المطر اليومي ومستويات التلوث اليومي.
النتائج
أثناء موسم الحر، ازداد دخول المستشفيات بنسبة 4.5 % لكل زيادة قدرها درجة واحدة مئوية فوق 29 درجة مئوية؛ وأثناء موسم البرد، ازداد دخول المستشفيات بنسبة 1.4 % لكل انخفاض قدره درجة واحدة مئوية داخل النطاق من 8.2 إلى 26.9 درجة مئوية. وفي تحليلات الفئات الفرعية، ازداد الدخول إثر الإصابة بالأمراض التنفسية والمعدية أثناء الحر والبرد الشديدين، ولكن لم يزدد الدخول بسبب الأمراض القلبية الوعائية إلا أثناء درجات الحرارة الباردة. ولكل زيادة قدرها درجة واحدة مئوية فوق 29 درجة مئوية، ازداد الدخول إثر الإصابات غير المتعمدة بنسبة 1.9 %. وأثناء موسم البرد، ارتفع الدخول إثر الإصابة بالأمراض القلبية الوعائية والإصابات غير المتعمدة بنسبة 2.1 % و2.4 %، على التوالي لكل زيادة قدرها درجة واحدة مئوية داخل النطاق من 8.2 إلى 26.9 درجة مئوية. ولم تكن أنماط الدخول إلى المستشفيات حساسة لنوع الجنس. وارتفع دخول المستشفيات إثر الإصابة بالأمراض التنفسية أثناء درجات الحرارة الساخنة والباردة بين الأطفال، ولكنه لم يرتفع إلا أثناء درجات الحرارة الباردة بين كبار السن. وفي الأشخاص الذين يبلغون 75 سنة فأكثر، ارتفع الدخول إلى المستشفيات إثر الإصابة بأمراض معدية أثناء درجات الحرارة القصوى.
الاستنتاج
في إقليم هونغ كونغ الإداري الخاص، ارتفع الإدخال إلى المستشفيات أثناء درجات الحرارة الشديدة. وينبغي تطوير تدخلات الصحة العمومية لحماية الأطفال وكبار السن وغيرهم من الفئات سريعة التأثر بالحر والبرد المفرطين.
摘要
目的
探讨1998 至2009 年中国香港特别行政区(SAR)天气现象和污染程度与每天入院人数(作为对发病率模式的近似)的关系。
方法
使用有关入院和日平均温度、日平均风速、平均相对湿度、每天全球总太阳辐射、每天总降雨量和日常污染水平的官方来源数据构建广义加法模型和滞后模型。
结果
在炎热季节,在29 °C以上温度时,温度每升高1 °C,入院人数增加4.5%;在寒冷季节,在8.2–26.9 °C温度范围内,温度每降低 1 °C,入院人数增加1.4%。在亚组分析中,在极端炎热和寒冷的天气中,呼吸和传染病入院人数增加,但心血管疾病入院数只在寒冷的天气中增加。在29 °C以上,温度每增加 1 °C,意外伤害入院数增加1.9%。在寒冷季节,在 8.2–26.9 °C温度范围内,温度每增加1 °C,心血管疾病和故意伤害入院数分别增加2.1%和2.4%。入院模式对性别不敏感。对于呼吸道疾病,儿童入院数在冷天和热天增加,老年人入院数仅在冷天增加。75 岁及以上人群在两种极端温度中的传染病入院数都会增加。
结论
在香港特别行政区,极端温度时入院数增加。应发展公共卫生干预措施保护儿童、老年人和其他脆弱人群免受极端冷热天气的伤害。
Резюме
Цель
Изучить взаимосвязь между погодными явлениями, уровнями загрязнения и числом ежедневных госпитализаций (как приближенные модели смертности) в 1998–2009 гг. в Специальном административном районе Гонконг (САР Гонконг), Китай.
Методы
Были построены обобщенные аддитивные и лаговые модели с использованием официальных данных о числе случаев госпитализации и среднесуточной температуре, среднесуточной скорости ветра, средней относительной влажности, среднесуточном суммарном солнечном излучении, общем суточном количестве осадков и уровнях ежесуточного загрязнения.
Результаты
В жаркий сезон число случаев госпитализации увеличивалось на 4,5% при повышении температуры свыше 29°C на каждый градус (°C), в холодный сезон число случаев госпитализации увеличивалось на 1,4% при понижении температуры на каждый градус (°C) в диапазоне 8,2–26,9°C. В подгрупповых анализах число случаев госпитализации по причине респираторных и инфекционных заболеваний увеличивалось при чрезвычайно высоких или низких температурах, а число случаев госпитализации по причине сердечно-сосудистых заболеваний увеличивалось только при низких температурах. При повышении температуры свыше 29°C на каждый градус (°C) число случаев госпитализации по причине непреднамеренных травм увеличивалось на 1,9%. В холодный сезон при понижении температуры на каждый градус (°C) в диапазоне 8,2–26,9°C число случаев госпитализации по причине сердечно-сосудистых заболеваний и непреднамеренных травм увеличивалось на 2,1% и 2,4% соответственно. В моделях госпитализаций учитывались данные для обоих полов. Число случаев госпитализации по причине респираторных заболеваний увеличивалось при высоких и низких температурах среди детей и только при низких температурах среди взрослых. Число случаев госпитализации по причине инфекционных заболеваний среди пожилых людей в возрасте 75 лет или старше увеличивалось при обоих экстремальных значениях температур.
Вывод
В САР Гонконг число случаев госпитализации увеличивается при экстремальных значениях температур. Следует разработать меры вмешательства в сфере общественного здравоохранения для зашиты здоровья детей, пожилых людей и других групп риска от экстремальных высоких и низких температур.
Introduction
According to the Intergovernmental Panel on Climate Change, global climate change poses major health threats and shifting temperature patterns in the 21st century are expected to substantially affect the burden of disease worldwide.1–9 Although there is evidence of an association between outdoor temperature and mortality rates, the interplay between the two remains only partially understood in Asia because of a lack of databases with comprehensive, comparable data for most urban communities in low- and middle-income settings.10,11 Evidence from European and American cities suggests that when outdoor temperatures are unusually high, there is a rise in hospital admissions10,12–15 for respiratory ailments, renal diseases,12 and infectious diseases (both vector-borne and foodborne) and cerebrovascular accidents, including subarachnoid haemorrhage13 and transient ischaemic attacks.16–22 The risk of admission appears to be higher among the critically ill,23 the very young, the very old, people of low socioeconomic status,24 people with pre-existing medical conditions,12,16 health-care workers, pregnant women25 and people who are institutionalized, live alone or have poor mobility.24
Hong Kong Special Administrative Region (SAR), China, has recorded one of the world’s highest average increases in ambient temperature.26 A study of the relationship between outdoor temperature and mortality in the city has shown a cumulative increase in mortality of 1.8% for every increase of 1 °C above 28.2 °C in mean daily outdoor temperature.26 According to another study on help-seeking behaviour in the city, elevated temperatures are associated with an increased volume of calls to an emergency hotline, particularly from women and elderly people.27 In light of these findings, the main objectives of this study were to examine whether rates of injury and disease fluctuate in relation to outdoor temperature and other environmental parameters in Hong Kong SAR by looking at hospital admissions, and to identify high-risk population subgroups. The ultimate aim is to facilitate policy to mitigate the negative health effects of changing climate patterns.
Methods
We conducted a retrospective ecological study using data on outdoor temperature, pollution levels and routine hospital admissions in Hong Kong SAR from 1 January 1998 to 31 December 2009. Meteorological variables, including mean daily temperature (MDT), mean daily relative humidity (MDRH), mean daily wind speed (MDWS), daily total global solar radiation (DTGSR) and total daily rainfall (TDR), were obtained from the Hong Kong SAR Observatory. Mean daily pollution levels were based on hourly concentrations of nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3) and particulate matter measuring ≤ 10 µm. These data were obtained from the 11 general environmental data collection stations belonging to the Environmental Protection Department.
The Hospital Authority in SAR keeps a citywide hospital database that covers all admissions to public hospitals, which represent 83% of all admissions. From this database we extracted data on routine hospital admissions by age, sex, district of residence, name of hospital, admission and discharge dates, cause of hospitalization, total length of hospital stay and discharge status. We analysed data on admissions for the following causes, as coded in the International statistical classification of diseases and related health problems, ninth revision:28 unintentional injuries (from external causes, codes 800–957; from accidents, codes E800–E949); intentional injuries (intentional self-harm, codes E950–E959; assaults, codes E960-E969); infectious diseases, codes 001–139, 320–323 and 614–616; renal failure, codes 584–586; diabetes, codes 249–250; cirrhosis, codes 571.5, 571.6, 571.8 and 571.9; cancer, codes 140–239; circulatory diseases, codes 390–459; and respiratory diseases, codes 460–519. All analyses were conducted by sex and age group (< 15 years, 15–59 years, 60–74 years and ≥ 75 years).
Statistical modelling
We developed generalized additive (Poisson) models to examine the association between changes in MDT and daily number of hospital admissions attributable to the causes described in the preceding section. Analyses were conducted separately for the hot season (June to September) and the cold season (November to March) to allow for the lag effect of temperature on hospitalization patterns. We used R version 2.10.1 (The R Foundation for Statistical Computing, Vienna, Austria) for the analyses. First we used R’s distributed lag nonlinear model (dlnm) package to determine how lagged effects should be modelled, and then proceeded to fit distributed lag models. We subsequently fit the generalized additive models with nonlinear smooth terms for MDT with a lag from day 0 (same day) to day k, where k was determined from the results of the distributed lag models. In all models, we controlled for time trend by means of a variable representing the day of the study (with values from 1 to 4383), and we controlled for season by means of another variable representing the day of the year (with values from 1 to 365). We allowed each of these variables a maximum of 4 degrees of freedom.
Results
From 1998 to 2009, temperatures ranged from 22.2 °C to 31.8 °C during the hot season; the average MDT was 28.4 °C and the average median daily temperature was 28.6 °C. During the cold season, temperatures ranged from 8.2 °C to 26.9 °C; the average mean and median daily temperatures were 18.7 °C and 19.0 °C, respectively. Table 1 shows the number of routine hospital admissions for various causes during the cold season (November to March) and the hot season (June to September). During the study period, there were 7 869 661 hospital admissions, and 33.1% of them took place during the hot season. Of the causes of admission selected for analysis, the most common one was respiratory diseases, which accounted for 17.1% of the admissions. This was followed by admissions for cancer (16.1%), circulatory diseases (15.1%), unintentional injuries (10.4%), infectious diseases (5.1%) and intentional injuries (0.3%).
Table 1. Hospital admissions during cold and hot seasons, by cause of admission, Hong Kong Special Administrative Region, China, 1998–2009.
| Cause | No. (%) of admissions |
|
|---|---|---|
| November–Marcha | June–Septemberb | |
| Unintentional injuries | 334 291 (10.0) | 270 942 (10.4) |
| Intentional injuries | 7 921 (0.2) | 7 038 (0.3) |
| Infectious diseases | 165 959 (5.0) | 132 647 (5.1) |
| Chronic diseases | ||
| Respiratory | 620 073 (18.6) | 444 628 (17.1) |
| Circulatory | 544 027 (16.3) | 393 495 (15.1) |
| Cancer | 501 898 (15.1) | 419 058 (16.1) |
| Renal failure | 345 166 (10.4) | 267 804 (10.3) |
| Diabetes | 80 190 (2.4) | 62 477 (2.4) |
| Cirrhosis | 6 984 (0.2) | 5 195 (0.2) |
| All other causes | 725 727 (21.8) | 601 857 (23.1) |
| Total | 3 332 203 (100) | 2 605 141 (100) |
a Cold season.
b Hot season.
Note: Principal diagnoses were coded in accordance with the International statistical classification of diseases and related health problems, ninth revision:28 unintentional injuries, 800–957 and E800–E949; intentional injuries, E950–E959 and E960–E969; infectious diseases, 001–139, 320–323 and 614–616; renal failure, 584–586; diabetes, 249–250; cirrhosis, 571.5, 571.6, 571.8 and 571.9; cancer, 140–239; circulatory diseases, 390–459; respiratory diseases: 460–519.
Source: Hospital Authority of Hong Kong Special Administrative Region.
Hot season
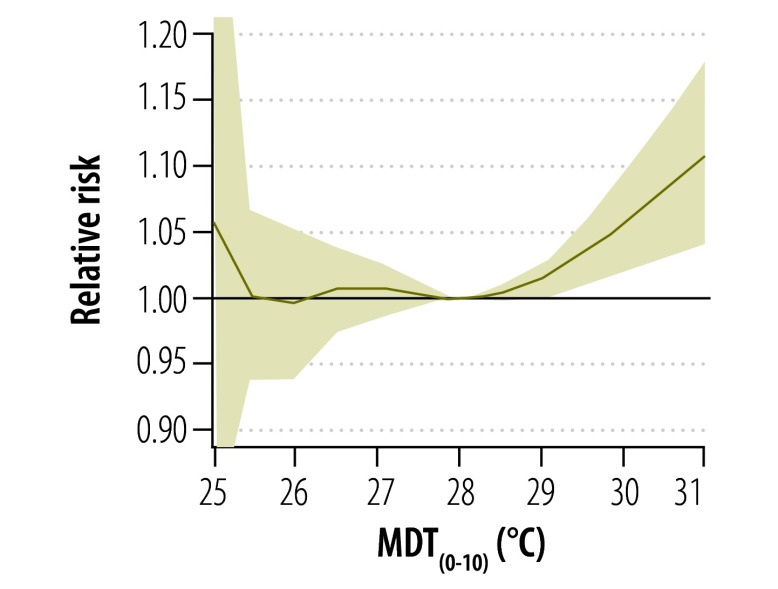
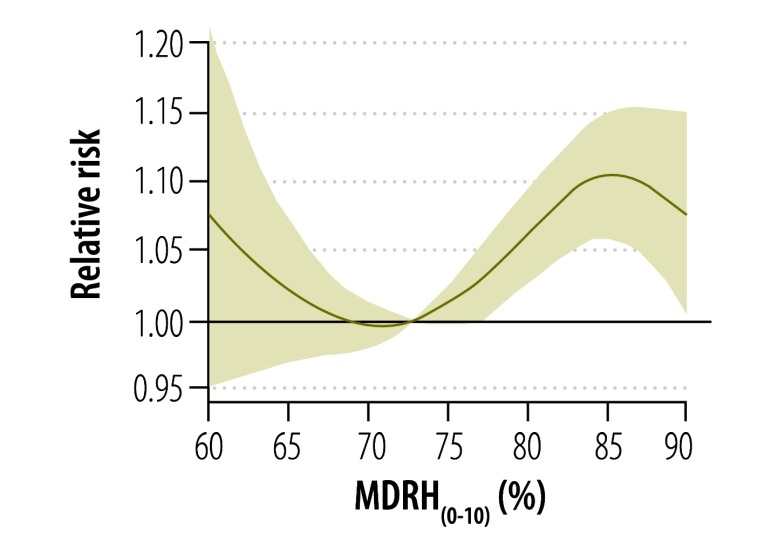
In the initial distributed lag models, the effects of high temperature on admissions peaked over a lag period of 3 to 6 days (lags 3–6) but persisted until the 10th day (lag 10) during the hot season. A smooth term with a maximum representing the MDT with a lag of 0 to 10 days (MDT(0–10)) was used in the subsequent generalized additive model, along with smooth terms for MDRH with a lag of 0 to 10 days (MDRH(0–10)), average DTGSR with the same lag period (DTGSR(0–10)) and MDWS with the same lag period (MDWS(0–10)). Same-day rainfall (square-root-transformed) was also included in all models based on the hypothesis that heavy rain would deter people from going to hospital. All terms were initially allowed a maximum of 5 degrees of freedom, with actual degrees of freedom determined by cross-validation using R’s mixed GAM computation vehicle (mgcv) package. In the final model, MDT(0–10) showed a statistically significant positive association with daily admissions that was roughly linear above 29 °C (Fig. 1). The association between MDRH10 and hospitalizations was complex (Fig. 2), but it was positive and approximately linear between humidity values of about 73% and 84% (i.e. the 20th and 80th percentiles of the variable’s distribution). Mean DTGSR(0–10) and MDWS(0–10) were positively and linearly associated with the number of daily admissions, although the associations were not statistically significant (P = 0.23 and 0.49, respectively); mean NO2, lagged by 0–4 days, was positively associated with the number of hospitalizations, with the association being linear over most of the range of this variable. The final model hockey stick terms created for temperature were:
| THOT = MDT(0-10) – | 29 |
if MDT(0–10) ≥ 29 °C, 0 otherwise:
| TCOLD = 29 – MDT(0–10) |
if MDT(0–10) < 29 °C, 0 otherwise.
Fig. 1.
Relative risk of hospitalization as a function of mean daily temperature lagged by 0–10 days (MDT(0–10)), Hong Kong Special Administrative Region, China, 1998–2009
Fig. 2.
Relative risk of hospitalization as a function of mean daily relative humidity lagged by 0–10 days (MDRH(0–10)), Hong Kong Special Administrative Region, China, 1998–2009
Linear terms were used for DTGSR(0–10), MDWS(0–10), and NO2 and a smooth term with a maximum of 5 degrees of freedom was adopted to account for MDRH(0–10). In this final model, a significant association (P = 0.003) was found between MDT and daily hospital admissions at temperatures above 29 °C. For every rise of 1 °C above this threshold, there was a 4.5% (95% confidence interval, CI: 2.1–7.0) increase in admissions. MDRH(0–10) remained nonlinearly and significantly (P < 0.001) associated with admissions, in a pattern similar to that in Fig. 2. The number of admissions showed a significant positive association with mean NO2 concentration, a non-significant negative association (P = 0.18) with MDWS(0–10) and a non-significant positive association (P = 0.64) with DTGSR(0–10).
In subgroup analyses of the causes of hospitalization, a rise in admissions for respiratory diseases, infectious diseases and unintentional injuries was noted at temperatures above 28.5 °C. There was no significant rise in admissions due to other causes, including cancer, circulatory diseases, diabetes mellitus, renal failure or cirrhosis, at these temperatures.
For respiratory diseases, the initial model showed an increase in admissions at an MDT10 above 28.5 °C; a similar association was noted between admissions and mean MDRH(0–10). In the subsequent model, a significant increase in admissions for respiratory diseases was found at temperatures above 28.5 °C (P < 0.001). For every rise of 1 °C above this threshold, admissions rose by 7.6% (95% CI: 5.1–10.2). Mean MDRH(0–10) remained nonlinearly and significantly (P < 0.001) associated with the number of admissions, in a pattern similar to that in Fig. 2. For every increase of 10 mg per m3 in mean O3 concentration lagged by 0–4 days, admissions for respiratory diseases rose by 1.6% (95% CI: 0.7–2.4; P = 0.0002); the association between mean NO2 concentration and admissions became non-significant after controlling for O3. Mean DTGSR(0–10) was significantly (P = 0.003) associated with admissions; for every increase of 5 milliJoules per m2 in mean DTGSR(0–10) (approximately equal to the interquartile range for this variable), admissions for respiratory diseases rose by 3.2% (95% CI: 1.2– 5.2).
For infectious diseases, the initial model showed a significant association (P = 0.01) between MDT(0–10) and the number of daily admissions at MDT(0–10) values above 28.5 °C. Mean MDRH(0–10) also showed a significant (P = 0.0003) S-shaped association with admissions at MDRH(0–10) values between 73% and 84%. This pattern was also noted for admissions due to other causes. Mean DTGSR(0–10) was not significantly associated with admissions for infectious diseases. The subsequent model showed a significant association (P < 0.001) between admissions for infectious diseases and MDT(0–10) at temperatures above 28.5 °C; for every rise of 1 °C above this threshold, there was a 4.5% (95% CI: 2.2–6.9) increase in admissions. Admissions for Salmonella infections were particularly sensitive to the effect of hot temperatures; they rose by 11.4% (P < 0.001) on the same day and over the following 14 days for every rise of 1 °C in MDT(0–14) within the range of temperatures observed in the hot season (22.2–31.8 °C). MDWS(0–14) was also significantly (P = 0.006) and negatively associated with admissions for infectious diseases, whereas mean MDRH(0–14) remained significantly (P < 0.001) and positively associated with admissions, in a pattern similar to than in Fig. 3.
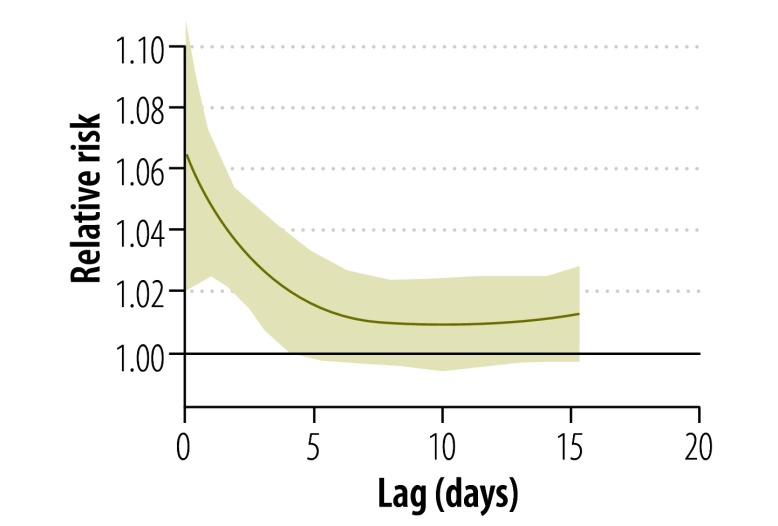
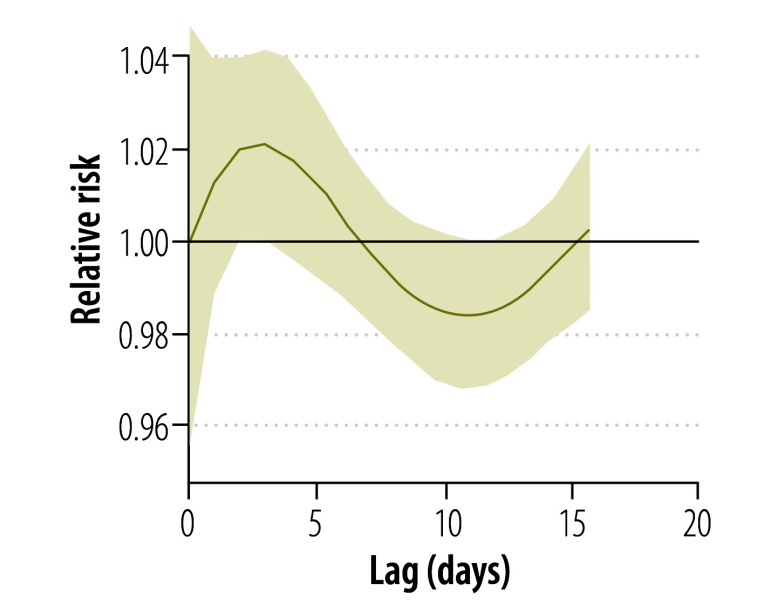
Fig. 3.
Relative risk of hospitalization for any cause at 32 °C versus 29 °C (lag 0–10 days) during the hot season,a Hong Kong Special Administrative Region, China, 1998–2009
a June to September.
Fig. 3 shows that during the hot season, admissions due to all causes peaked 3 to 6 days after a hot day. Fig. 4 shows that admissions for respiratory diseases peaked immediately and remained higher but declined slowly over the next 4 days. Fig. 5 indicates that admissions for infectious diseases peaked about 3 to 5 days after a hot day.
Fig. 4.
Relative risk of hospitalization for a respiratory disease at 32 °C versus 29 °C (lag 0–10 days) during the hot season,a Hong Kong Special Administrative Region, China, 1998–2009
a June to September.
Fig. 5.
Relative risk of hospitalization for an infectious disease at 32 °C versus 29 °C (lag 0–10 days) during the hot season,a Hong Kong Special Administrative Region, 1998–2009
a June to September.
Our findings also indicate a significant (P = 0.006) increase of 1.9% (95% CI: 0.6–3.2) in admissions for unintentional injuries for every rise of 1 °C in MDT above 28.5 °C. The number of admissions due to intentional injuries (self-harm or harm to others) was not significantly associated with a rise in MDT above a certain threshold.
We conducted additional analyses by sex and age group for admissions due to respiratory and infectious diseases (Table 2). No significant differences were observed between the sexes. For respiratory disease admissions, the increase observed during hot weather was greater among children (0–14 years) and young adults (15–59 years) than among people aged 60–74 years or people 75 years of age or older. For infectious disease hospitalizations, the increase in admissions observed during hot weather was greater among people 75 years of age or older than among younger people.
Table 2. Increase in admissions for respiratory and infectious diseases during the hot season (June to September), by sex and age, in Hong Kong Special Administrative Region, China, 1998–2009.
| Characteristic | Respiratory diseases |
Infectious diseases |
|||
|---|---|---|---|---|---|
| Increasea (95% CI) | P | Increasea (95% CI) | P | ||
| Sex | |||||
| Male | 7.5 (5.0 to 10.0) | < 0.0001 | 3.0 (0.1 to 6.0) | 0.041 | |
| Female | 7.5 (4.4 to 10.6) | < 0.0001 | 6.0 (3.0 to 9.0) | 0.0002 | |
| Age (years) | |||||
| < 15 | 19.5 (12.9 to 26.4) | < 0.0001 | 3.7 (0.2 to 7.4) | 0.038 | |
| 15–59 | 8.2 (4.0 to 12.6) | 0.0001 | 0.9 (–2.7 to 4.1) | 0.60 | |
| 60–74 | 7.1 (3.4 to 11.1) | 0.0002 | 2.6 (–2.0 to 7.3) | 0.26 | |
| ≥ 75 | 4.9 (1.9 to 8.0) | 0.0014 | 9.6 (5.6 to 13.8) | 0.0001 | |
CI, confidence interval.
a This represents the percentage increase in hospitalizations for every increase of 1 °C above 28.5 °C in mean daily outdoor temperature.
Cold season
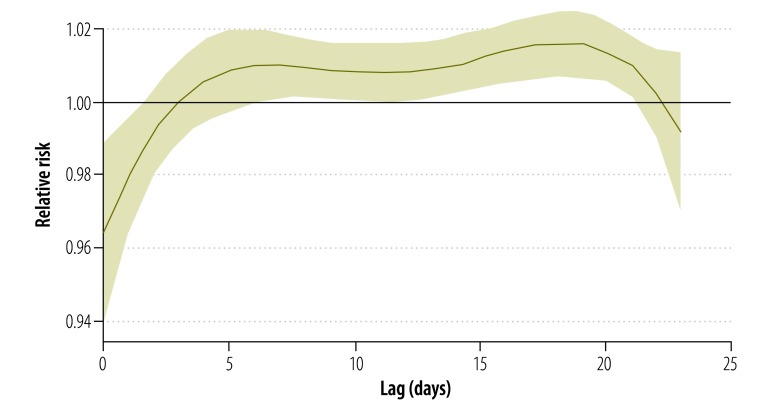
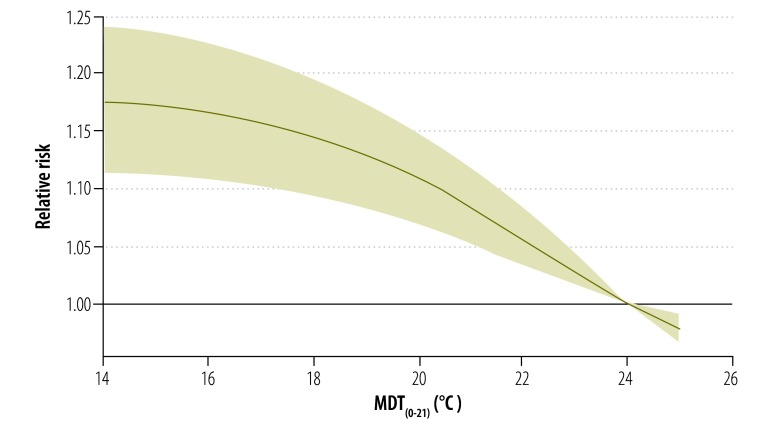
In the initial distributed lag models, cold temperatures, lagged by 0–2 days, showed a negative association with admissions, but the association became positive from lag 3 onwards, peaked from lags 5 to 17 and remained positive to lag 21 (Fig. 6). In subsequent analyses we adopted the MDT lagged by 0 to 21 days (MDT(0–21)), along with averages of the other meteorological variables, lagged by 0 to 21 days. For air pollutants, the distributed lag models showed an association between admissions and mean NO2 only on the same day (lag 0) and the previous day (lag 1). Other pollutants, however, showed no significant association with admissions after controlling for mean NO2. Therefore, in the model we used mean NO2, lagged by 0 and 1 days (NO2(0–1)), and we dropped other pollutants. In subsequent analyses in which smooth terms were used for these variables, the associations between the number of admissions and MDT(0–21) (Fig. 7) and mean NO2(0–1) were linear over most of the variable ranges, and the associations between admissions and mean MDRH(0–21) and MDWS(0–21) were weak and nonlinear but significant. The model showed no significant association between admissions and mean DTGSR(0–21). Therefore, in the final models we used linear terms for MDT(0–21) and mean NO2(0–1) and smooth terms for mean MDRH(0–21) and MDWS(0–21), and we dropped DTGSR(0–21) from the models.
Fig. 6.
Relative risk of hospitalization for any cause at 10 °C versus 25 °C (lag 0–21 days) during the cold season,a Hong Kong Special Administrative Region, 1998–2009
a November to March.
Fig. 7.
Relative risk of hospitalization as a function of mean daily temperature during the cold seasona lagged by 0–21 days (MDT(0–21)), Hong Kong Special Administrative Region, 1998–2009
a November to March.
In the cold season model, colder temperatures were positively and significantly (P < 0.0001) associated with admissions across the temperature range observed in the cold season (8.2 to 26.9 °C). For every drop of 1 °C below the top value in this range (26.9 °C) there was a 1.4% (95% CI: 0.9–1.8) increase in admissions. For every increase of 10 mg per m3 in NO2(0–1) there was a 1.2% (95% CI: 0.8–1.5; P = 0.0015) increase in admissions.
In subgroup analyses by cause of admission, the models with linear terms for mean NO2(0–1) and MDT(0–21), and without other pollutants or DTGSR(0–21), were also appropriate for admissions for infectious diseases. For every 1 °C drop in MDT(0–21) from 26.9 °C there was a 1.0% (95% CI: 0.4–1.6; P = 0.002) increase in admissions. For every increase of 10 µg per m3 in NO2(0–1) there was a 0.9% (95% CI: 0.4–1.5) increase in admissions.
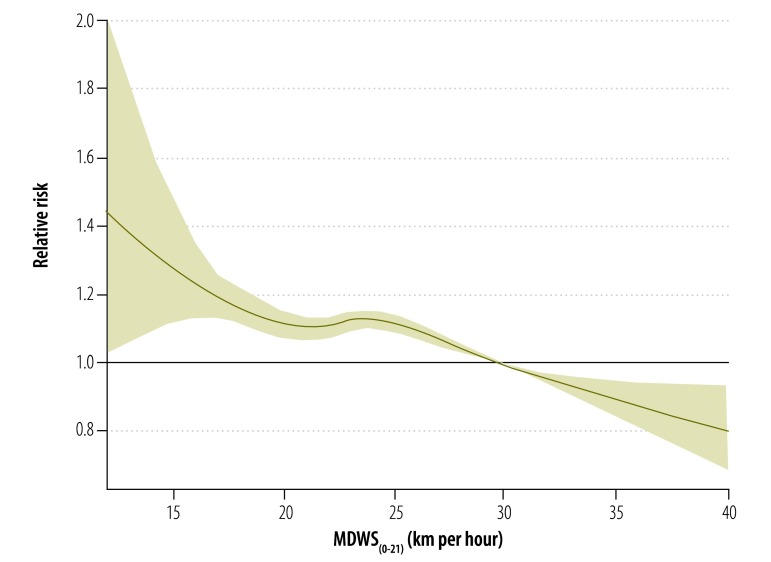
For respiratory disease admissions, linear terms were used for MDT(0–21), mean NO2(0–1) and mean O3, lagged by 0–1 days (O3(0–1)), and smooth terms were used for MDWS(0–21) and MDRH(0–21). In this model, every 1 °C drop below 26.2 °C in MDT(0–21) was accompanied by a 4.3% (95% CI: 3.6–4.7) increase in admissions. Every increase of 10 µg per m3 in mean NO2(0–1) was accompanied by a 0.5% (95% CI: 0.03–1.0; P = 0.035) increase in admissions, and every increase of 10 µg per m3 in O3(0–1) was associated with a 2.2% (95% CI: 1.7–2.7; P < 0.0001) increase in admissions. MDWS(0–21) also showed a highly significant (P < 0.0001) association with admissions for respiratory diseases. A sharp decrease in admissions was noted at MDWS(0–21) values of 10 to 20 kilometres per hour (km/h), followed by a slight increase at values between 20 and 24 km/h (which roughly corresponds to the interquartile range for wind speed) and by another sharp decrease at values between 24 and 40 km/h (Fig. 8).
Fig. 8.
Relative risk of hospitalization for a respiratory disease as a function of mean daily wind speed during the cold seasona lagged by 0–21 days (MDWS(0–21)), Hong Kong Special Administrative Region, 1998–2009
a November to March.
For cardiovascular disease admissions, linear terms were appropriate for MDT(0–21), MDRH(0–21) and mean NO2(0–1), but MDWS(0–21) and DTGSR(0–21) were dropped. In this model, every decrease of 1 °C was accompanied, on average, by a 2.1% (95% CI: 1.6–2.5; P < 0.0001) increase in hospitalizations. For every increase of 10 µg per m3 in NO2(0–1) there was, on average, a 1.6% (95% CI: 1.1–2.0; P < 0.0001) increase in admissions. For every rise of 10% in MDRH(0–21), hospital admissions rose by 1.6% (95% CI: 0.3–2.9; P = 0.014). There was no significant association between MDT(0–21) and hospital admissions for renal disease or cancer; however, increases in mean NO2(0–1) were accompanied by significant increases in admissions for these diseases.
We conducted subgroup analyses by age and sex for hospital admissions due to respiratory, infectious and cardiovascular diseases (Table 3). Admissions for respiratory diseases were highly sensitive to cold temperatures among children and people 75 years of age or older, and admissions for infectious and cardiovascular diseases were the most sensitive to cold temperatures among people aged 75 years or older. No strong effect modification by sex was noted.
Table 3. Increase in hospital admissions for respiratory, infectious and cardiovascular diseases as a function of changes in mean daily temperature, by sex and age, Hong Kong Special Administrative Region, China, 1998–2009.
| Characteristic | Respiratory diseases |
Infectious diseases |
Cardiovascular diseases |
|||||
|---|---|---|---|---|---|---|---|---|
| Increasea (95% CI) | P | Increasea (95% CI) | P | Increasea (95% CI) | P | |||
| Sex | ||||||||
| Male | 4.1 (3.6 to 4.7) | < 0.0001 | 1.2 (0.5 to 2.0) | 0.0021 | 1.7 (1.1 to 2.3) | < 0.0001 | ||
| Female | 4.7 (4.1 to 5.3) | < 0.0001 | 0.9 (0.2 to 1.6) | 0.0070 | 2.2 (1.6 to 2.7) | < 0.0001 | ||
| Age (years) | ||||||||
| < 15 | 5.0 (4.0 to 6.1) | < 0.0001 | 1.3 (0.3 to 2.3) | 0.015 | 1.1 (–0.4 to 2.5) | 0.14 | ||
| 15–59 | 2.2 (1.3 to 3.1) | < 0.0001 | 0.7 (0.0 to 1.5) | 0.055 | 0.2 (–0.6 to 1.0) | 0.60 | ||
| 60–74 | 3.7 (3.1 to 4.4) | < 0.0001 | 0.1 (–0.7 to 0.8) | 0.84 | 0.9 (0.3 to 1.6) | 0.0048 | ||
| ≥ 75 | 5.1 (4.6 to 5.6) | 0.0001 | 3.4 (2.4 to 4.4) | 0.0001 | 3.8 (3.3 to 4.4) | < 0.0001 | ||
CI, confidence interval.
a This represents the percentage increase in hospitalizations for every drop of 1 °C in mean temperature (lag 0–21) over the cooler temperature ranges (8.2–26.9 °C).
The number of daily hospitalizations due to accidental causes was not associated with same-day MDT during the cold season, but it showed a significant positive association with MDWS and mean NO2 concentrations (both with lag 0) and a negative association with MDRH. A higher MDT (lag 0) showed a significant positive association with the number of hospitalizations for intentional injuries (assaults and attempted suicides); every increase of 1 °C above the lower end of the temperature range observed during the cold season (8.2 °C) was accompanied by a 2.4% (95% CI: 1.6–3.1); P < 0.0001) increase in admissions.
Discussion
In this study, the high temperature thresholds above which morbidity, as reflected in hospital admissions, increases were 0.3 to 0.8 °C higher (28.5–29.0 °C) than the threshold above which mortality was found to increase in our previous study (28.2 °C).26 Overall, hospitalizations increased by 4.5% for every 1 °C increase in mean daily temperature above 29.0 °C; they also rose by 1.4% for each 1 °C decrease over the range of temperatures (8.2–26.9 °C) observed in the cold season. Thus, in Hong Kong SAR, a subtropical city, elevated temperatures affect morbidity to a greater degree than colder temperatures. However, since the effect of cold temperatures operates over a wider temperature range than that of hot temperatures, over the course of a year excess morbidity during cold temperatures exceeds excess morbidity during hot temperatures.
In subgroup analyses, admissions for respiratory and infectious diseases and accidents increased during both the hot and the cold season, but during the cold season cardiovascular disease admissions also increased. We found that sensitivity to high temperatures varies by age, an effect that has been seen in other studies. For example, in London, during hot weather the risk of having a respiratory condition is especially high among people who are older than 75 years, and the risk of having a respiratory or renal condition is also higher among children less than 5 years old.12,29 In our study, children (aged less than 15 years) were more vulnerable than adults to being admitted to hospital for respiratory conditions during high and low temperatures, but people 75 years of age or older showed a higher risk of being admitted for respiratory conditions only during lower temperatures.
MDRH was found to be strongly associated with the number of admissions for causes other than injuries during the hot season. This was true overall and in most subgroups, especially when humidity hovered between about 72% and 85%. In Hong Kong SAR, MDRH rarely drops below 72% in the summer, and values above 85% usually occur only on cooler days, when the temperature drops below our heat thresholds of 28.5–29 °C. Therefore, our results suggest that higher MDRH exacerbates the effects of high temperatures on health. The decline in admissions when MDRH rises above 85% suggests that high humidity may have a beneficial effect when temperatures cool. Higher MDWS was generally accompanied by fewer admissions for infectious diseases during the hot season and by fewer admissions for respiratory diseases during the cold season. This was an unexpected finding, since high winds can exacerbate the physiological effects of cold temperatures. One explanation may be that higher winds mitigate the physiological effects of high temperatures by facilitating the body’s natural cooling processes. Another possibility is that stronger winds help to clear pollutants from high concentration areas such as roadsides. Thus, for a given measured pollutant level, actual exposure may be less on days with high winds. In a recent study, wind speeds on hot days (mean temperature above 29 °C) were found to have a significant positive association with daily mortality, and the association was stronger in areas with a high urban heat island index.30 This merits further study.
This study has the limitations that are inherent to statistical models. First, we conducted a retrospective ecological study and the ecologic fallacy cannot be ruled out. In addition, we assumed that the increase in hospital admissions resulted solely from an increase in disease occurrence and that all patients sought care from a particular hospital system. In reality, several system-specific factors could have biased the data in the hospital admission records, among them patterns of clinical diagnosis on admission, admission policies and clinical auditing and reporting practices. Although the Hospital Authority covers 83% of all hospital services in Hong Kong SAR and the system provides good clinical services to all patients, regardless of their socioeconomic status or demographic characteristics, a small fraction of patients in Hong Kong SAR probably still prefer to go to private hospitals because waiting times are shorter and they can choose the physician. The retrospective nature of our data also failed to provide the information needed to control for factors that influence the risk of falling ill during hot weather. These include, for example, medical conditions leading to poor temperature regulation,31 ethnic group,24 alcoholism, living on a higher floor32 and activities such as working and exercising outdoors.31 In addition, there is scientific controversy surrounding the accuracy of temperature predictions, which makes it difficult to assess the impact of temperature on health. Our retrospective database was quite comprehensive and spanned more than 10 years, but because of the way in which the data were collected and recorded, it did not allow for fine geographic analyses that might have shed more light on how urban planning and design might affect the interplay between outdoor temperature and morbidity.
This study’s greatest strength lies in the use of meteorological and pollution data covering more than a decade to examine hospital admissions as a function of MDT and pollution levels in a Chinese city. Our finding that hospital admissions are affected by temperature corroborates findings from Taiwan, China,10 and South Australia, where ambulance transport of assault victims has been noted to increase by 13% during heat waves.11 Our findings will contribute to a better understanding of how temperature can affect health in a densely-populated Asian urban setting and will prove useful in the planning of clinical services and of emergency contingency response during periods of prolonged heat. Measures to increase public awareness, educate the public about self-protection and coordinate multidisciplinary and intersectoral responses will be required.
Acknowledgements
The authors thank the Hong Kong SAR Observatory, the Hospital Authority and the Environmental Protection Department for providing the data sets for this study.
Funding:
This work was supported by the Health and Health Services Research Fund of the Food and Health Bureau of the government of Hong Kong SAR [Ref: 08090261].
Competing interests:
None declared.
References
- 1.Pachauri RK, Reisinger A, editors. Climate change 2007: synthesis report. Contribution of Working Groups I, II and III to the fourth assessment report of the Intergovernmental Panel on Climate Change. Geneva: Intergovernmental Panel on Climate Change; 2007. [Google Scholar]
- 2.Pirard P, Vandentorren S, Pascal M, Laaidi K, Le Tertre A, Cassadou S, et al. Summary of the mortality impact assessment of the 2003 heat wave in France. Euro Surveill. 2005;10:153–6. [PubMed] [Google Scholar]
- 3.Davis RE, Knappenberger PC, Michaels PJ, Novicoff WM. Changing heat-related mortality in the United States. Environ Health Perspect. 2003;111:1712–8. doi: 10.1289/ehp.6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hajat S, Kovats RS, Atkinson RW, Haines A. Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health. 2002;56:367–72. doi: 10.1136/jech.56.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001;12:662–7. doi: 10.1097/00001648-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Grize L, Huss A, Thommen O, Schindler C, Braun-Fahrländer C. Heat wave 2003 and mortality in Switzerland. Swiss Med Wkly. 2005;135:200–5. doi: 10.4414/smw.2005.11009. [DOI] [PubMed] [Google Scholar]
- 7.Michelozzi P de D, de Donato F, Bisanti L, Russo A, Cadum E, DeMaria M, et al. The impact of the summer 2003 heat waves on mortality in four Italian cities. Euro Surveill. 2005;10:161–5. [PubMed] [Google Scholar]
- 8.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–7. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 9.McMichael AJ, Wilkinson P, Kovats RS, Pattenden S, Hajat S, Armstrong B, et al. International study of temperature, heat and urban mortality: the ‘ISOTHURM’ project. Int J Epidemiol. 2008;37:1121–31. doi: 10.1093/ije/dyn086. [DOI] [PubMed] [Google Scholar]
- 10.Tai CC, Lee CC, Shih CL, Chen SC. Effects of ambient temperature on volume, specialty composition and triage levels of emergency department visits. Emerg Med J. 2007;24:641–4. doi: 10.1136/emj.2006.045310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nitschke M, Tucker GR, Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med J Aust. 2007;187:662–5. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 12.Kovats RS, Hajat S, Wilkinson P.Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med 200461893–8.http//dx..org/10.1136/oem.2003.012047 10.1136/oem.2003.012047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fish PD, Bennett GCJ, Millard PH. Heatwave morbidity and mortality in old age. Age Ageing. 1985;14:243–5. doi: 10.1093/ageing/14.4.243. [DOI] [PubMed] [Google Scholar]
- 14.Mastrangelo G, Fedeli U, Visentin C, Milan G, Fadda E, Spolaore P. Pattern and determinants of hospitalization during heat waves: an ecologic study. BMC Public Health. 2007;7:200. doi: 10.1186/1471-2458-7-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleury M, Charron DF, Holt JD, Allen OB, Maarouf AR. A time series analysis of the relationship of ambient temperature and common bacterial enteric infections in two Canadian provinces. Int J Biometeorol. 2006;50:385–91. doi: 10.1007/s00484-006-0028-9. [DOI] [PubMed] [Google Scholar]
- 16.Bangs MJ, Larasati RP, Corwin AL, Wuryadi S. Climatic factors associated with epidemic dengue in Palembang, Indonesia: implications of short-term meteorological events on virus transmission. Southeast Asian J Trop Med Public Health. 2006;37:1103–16. [PubMed] [Google Scholar]
- 17.Thammapalo S, Chongsuwiwatwong V, McNeil D, Geater A. The climatic factors influencing the occurrence of dengue hemorrhagic fever in Thailand. Southeast Asian J Trop Med Public Health. 2005;36:191–6. [PubMed] [Google Scholar]
- 18.Yé Y, Louis VR, Simboro S, Sauerborn R. Effect of meteorological factors on clinical malaria risk among children: an assessment using village-based meteorological stations and community-based parasitological survey. BMC Public Health. 2007;7:101. doi: 10.1186/1471-2458-7-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Checkley W, Epstein LD, Gilman RH, Figueroa D, Cama RI, Patz JA, et al. Effect of El Niño and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children. Lancet. 2000;355:442–50. doi: 10.1016/s0140-6736(00)82010-3. [DOI] [PubMed] [Google Scholar]
- 20.Paz S. The West Nile Virus outbreak in Israel (2000) from a new perspective: the regional impact of climate change. Int J Environ Health Res. 2006;16:1–13. doi: 10.1080/09603120500392400. [DOI] [PubMed] [Google Scholar]
- 21.D’Souza RM, Becker NG, Hall G, Moodie KB. Does ambient temperature affect foodborne disease? Epidemiology. 2004;15:86–92. doi: 10.1097/01.ede.0000101021.03453.3e. [DOI] [PubMed] [Google Scholar]
- 22.Hashizume M, Armstrong B, Hajat S, Wagatsuma Y, Faruque ASG, Hayashi T, et al. Association between climate variability and hospital visits for non-cholera diarrhoea in Bangladesh: effects and vulnerable groups. Int J Epidemiol. 2007;36:1030–7. doi: 10.1093/ije/dym148. [DOI] [PubMed] [Google Scholar]
- 23.Stéphan F, Ghiglione S, Decailliot F, Yakhou L, Duvaldestin P, Legrand P. Effect of excessive environmental heat on core temperature in critically ill patients: an observational study during the 2003 European heat wave. Br J Anaesth. 2005;94:39–45. doi: 10.1093/bja/aeh291. [DOI] [PubMed] [Google Scholar]
- 24.Jones TS, Liang AP, Kilbourne EM, Griffin MR, Patriarca PA, Wassilak SG, et al. Morbidity and mortality associated with the July 1980 heat wave in St Louis and Kansas City. JAMA. 1982;247:3327–31. [PubMed] [Google Scholar]
- 25.Luton D, Alran S, Fourchotte V, Sibony O, Oury J-F. Paris heat wave and oligohydramnios. Am J Obstet Gynecol. 2004;191:2103–5 . doi: 10.1016/j.ajog.2004.05.090. [DOI] [PubMed] [Google Scholar]
- 26.Chan EY, Goggins WB, Kim JJ, Griffiths SM. A study of intracity variation of temperature-related mortality and socioeconomic status among the Chinese population in Hong Kong. J Epidemiol Community Health. 2012;66:322–7. doi: 10.1136/jech.2008.085167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan EYY, Goggins WB, Kim JJ, Griffiths S, Ma TKW. Help-seeking behavior during elevated temperature in Chinese population. J Urban Health. 2011;88:637–50. doi: 10.1007/s11524-011-9599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.International statistical classification of diseases and related health problems, ninth revision. Geneva: World Health Organization; 1978. [Google Scholar]
- 29.Johnson H, Kovats RS, McGregor G, Stedman J, Gibbs M, Walton H, et al. The impact of the 2003 heat wave on mortality and hospital admissions in England. Health Stat Q. 2005;25:6–11. [PubMed] [Google Scholar]
- 30.Goggins WB, Chan EYY, Ng E, Ren C, Chen L. Effect modification of the association between short-term meteorological factors and mortality by urban heat islands in Hong Kong. PLoS One. 2012;7:e38551. doi: 10.1371/journal.pone.0038551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dixit SN, Bushara KO, Brooks BR. Epidemic heat stroke in a midwest community: risk factors, neurological complications and sequelae. Wis Med J. 1997;96:39–41. [PubMed] [Google Scholar]
- 32.Kilbourne EM, Choi K, Jones TS, Thacker SB, The Field Investigation Team Risk factors for heatstroke: a case-control study. JAMA. 1982;247:3332–6. doi: 10.1001/jama.1982.03320490030031. [DOI] [PubMed] [Google Scholar]