Abstract
Objective
To rank pollutants in two Nigerian water supply schemes according to their effect on human health using a risk-based approach.
Methods
Hazardous pollutants in drinking-water in the study area were identified from a literature search and selected pollutants were monitored from April 2010 to December 2011 in catchments, treatment works and consumer taps. The disease burden due to each pollutant was estimated in disability-adjusted life years (DALYs) using data on the pollutant’s concentration, exposure to the pollutant, the severity of its health effects and the consumer population.
Findings
The pollutants identified were microbial organisms, cadmium, cobalt, chromium, copper, iron, manganese, nickel, lead and zinc. All were detected in the catchments but only cadmium, cobalt, chromium, manganese and lead exceeded World Health Organization (WHO) guideline values after water treatment. Post-treatment contamination was observed. The estimated disease burden was greatest for chromium in both schemes, followed in decreasing order by cadmium, lead, manganese and cobalt. The total disease burden of all pollutants in the two schemes was 46 000 and 9500 DALYs per year or 0.14 and 0.088 DALYs per person per year, respectively, much higher than the WHO reference level of 1 × 10−6 DALYs per person per year. For each metal, the disease burden exceeded the reference level and was comparable with that due to microbial contamination reported elsewhere in Africa.
Conclusion
The estimated disease burden of metal contamination of two Nigerian water supply systems was high. It could best be reduced by protection of water catchment and pretreatment by electrocoagulation.
Résumé
Objectif
Classer les polluants dans deux systèmes nigérians d'approvisionnement en eau en fonction de leur effet sur la santé humaine, en utilisant une approche fondée sur le risque.
Méthodes
Dans la zone d'étude, les polluants dangereux dans l'eau potable ont été identifiés grâce à une recherche documentaire, et certains polluants ont été suivis d'avril 2010 à décembre 2011 dans des bassins versants, des installations de traitement et au robinet des consommateurs. La charge de morbidité due à chaque polluant a été estimée en années de vie ajustées sur l'incapacité (DALY) à l'aide des données relatives à la concentration des polluants, l'exposition aux polluants, la gravité de leurs effets sur la santé et la population des consommateurs.
Résultats
Les polluants identifiés étaient des organismes microbiens, le cadmium, le cobalt, le chrome, le cuivre, le fer, le manganèse, le nickel, le plomb et le zinc. Tous ont été détectés dans les bassins versants, mais seuls le cadmium, le cobalt, le chrome, le manganèse et le plomb dépassaient les valeurs indicatives de l'Organisation mondiale de la Santé (OMS) après traitement de l'eau. Une contamination postérieure au traitement a été observée. Selon les estimations, la charge de morbidité la plus lourde résultait du chrome dans les deux systèmes, suivi par le cadmium, le plomb, le manganèse et le cobalt, par ordre décroissant. La charge de morbidité totale de tous les polluants des deux systèmes était de 46 000 et 9500 DALY par an ou de 0,14 et 0,088 DALY par personne et par an, respectivement. Elle était donc beaucoup plus élevée que le niveau de référence de l'OMS, soit 1×10−6 DALY par personne et par an. Pour chaque métal, la charge de morbidité dépassait le niveau de référence et était comparable à celle due à la contamination microbienne signalée ailleurs en Afrique.
Conclusion
Les estimations de la charge de morbidité de la contamination métallique des deux systèmes nigérians d'approvisionnement en eau étaient élevées. Les meilleures façons de réduire la charge de morbidité seraient la protection du bassin versant et le prétraitement par électrocoagulation.
Resumen
Objetivo
Clasificar los contaminantes de dos sistemas de suministro de agua de Nigeria en función de su efecto sobre la salud humana a través de un enfoque basado en el riesgo.
Métodos
Se identificaron los contaminantes peligrosos presentes en el agua potable del área de estudio mediante una investigación bibliográfica y entre abril de 2010 y diciembre de 2011 se controlaron los contaminantes seleccionados en las cuencas, las plantas de tratamiento y los grifos de los consumidores. Se calculó la carga de morbilidad causada por cada contaminante en años de vida ajustados por discapacidad (AVAD) a partir de los datos de la concentración del contaminante, la exposición al mismo, la gravedad de sus efectos sobre la salud y la población de consumidores.
Resultados
Los contaminantes identificados fueron organismos microbianos, cadmio, cobalto, cromo, cobre, hierro, manganeso, níquel, plomo y zinc. Todos los contaminantes fueron detectados en las cuencas, pero sólo las cantidades de cadmio, cobalto, cromo, manganeso y plomo superaron los valores de referencia de la Organización Mundial de la Salud de (OMS) después del tratamiento del agua. Se observó una contaminación posterior al tratamiento. La carga estimada de la enfermedad fue mayor para el cromo en ambos esquemas, seguido en orden decreciente por el cadmio, plomo, manganeso y cobalto. La carga total de la enfermedad de todos los contaminantes en los dos sistemas fue, respectivamente, de 46 000 y 9500 AVAD por año o 0,14 y 0,088 AVAD por persona y año, muy por encima del nivel de referencia de la OMS de 1 × 10 − 6 AVAD por persona y año. La carga de morbilidad para cada metal superó el nivel de referencia y fue comparable con aquella por contaminación microbiana evidenciada en otras partes de África.
Conclusión
La carga de morbilidad estimada de la contaminación por metales de dos sistemas de suministro de agua nigerianos fue alta. La mejor forma para reducir la carga de morbilidad sería la protección de la captación de agua y el tratamiento previo mediante electrocoagulación.
ملخص
الغرض
ترتيب الملوثات في مخططين لإمدادات المياه في نيجيريا وفقاً لتأثيرها على صحة الإنسان باستخدام نهج قائم على المخاطر.
الطريقة
تم تحديد الملوثات الخطرة في مياه الشرب في منطقة الدراسة من الأبحاث المنشورة وتم رصد الملوثات المحددة في الفترة من نيسان/أبريل 2010 إلى كانون الأول/ديسمبر 2011 في مستجمعات المياه ومحطات المعالجة وصنابير المستهلكين. وتم تقدير عبء المرض الناتج عن كل ملوث بالنسبة لسنوات العمر المصححة باحتساب مدد العجز باستخدام البيانات المعنية بتركيز الملوث والتعرض للملوث وخطورة آثاره الصحية والفئات السكانية للمستهلكين.
النتائج
كانت الملوثات التي تم تحديدها عبارة عن كائنات عضوية جرثومية والكادميوم والكوبلت والكروم والنحاس والحديد والمنغنيز والنيكل والرصاص والزنك. وتم اكتشافها جميعاً في مياه المستجمعات ولكن لم يتعدى قيم المبدأ التوجيهي لمنظمة الصحة العالمية بعد معالجة المياه سوى الكادميوم والكوبلت والكروم والمنغنيز والرصاص. ولوحظ وجود تلوث بعد معالجة المياه. وكان أكبر عبء للمرض وفق التقديرات في الكروم في كلا المخططين، يليه تنازلياً الكادميوم والرصاص والمنغنيز والكوبلت. وكان إجمالي عبء المرض لجميع الملوثات في المخططين 46000 و9500 سنة من سنوات العمر المصححة باحتساب مدد العجز لكل سنة أو 0.14 و0.088 سنة من سنوات العمر المصححة باحتساب مدد العجز لكل شخص سنوياً، على التوالي، وهو ما يزيد بشدة عن المستوى المرجعي للمنظمة 1× 10 −6 سنة من سنوات العمر المصححة باحتساب مدد العجز لكل شخص سنوياً. وبالنسبة لكل معدن، تعدى عبء المرض المستوى المرجعي وكان من الممكن مقارنته بذلك الناتج عن التلوث الجرثومي الذي تم الإبلاغ عنه في مناطق أخرى في أفريقيا.
الاستنتاج
كان عبء المرض الناجم عن تلوث المعادن في نظامين من نظم إمدادات المياه في نيجيريا وفق التقديرات مرتفعاً. ويمكن تقليله على الوجه الأمثل من خلال حماية مستجمعات المياه والمعالجة المسبقة عن طريق التخثير الكهربي.
摘要
目的
根据对人体健康的影响,使用基于风险的方法,对尼日利亚两个供水方案的污染物进行评级。
方法
从文献检索中确定研究区域饮用水中的有害污染物,监测2010 年4 月到2011 年12 月集水区、污水处理厂和消费者的水龙头的选定污染物。使用污染物浓度、污染物接触、健康影响严重程度和消费者人群的相关数据以伤残调整寿命年(DALY)为单位估计每个污染物造成的疾病负担。
结果
确定的污染物有微生物、镉、钴、铬、铜、铁、锰、镍、铅和锌。所有污染物在集水区检测,但仅镉、钴、铬、锰、铅在水处理之后超过世界卫生组织(WHO)指导值。观察处理后污染物。在两个方案中,铬的估计疾病负担最大,然后按递减顺序依次是镉、铅、锰和钴。在两个方案中,所有污染物的合计疾病负担分别是每年4.6 万和9500 DALY,或者每年每人0.14 和0.088 DALY,比世界卫生组织的每年每人1 × 10-6 DALY的参考水平高很多。对于每种金属,疾病负担均超过参考水平,与非洲其他地方报告的微生物污染造成的疾病负担相当。
结论
尼日利亚两个供水方案的金属污染物估计疾病负担较高。保护集水区和电絮凝法预处理可能是减少污染的最佳方法。
Резюме
Цель
Осуществить ранжирование загрязняющих веществ в двух нигерийских системах водоснабжения по степени их влияния на здоровье человека с использованием риск-ориентированного подхода.
Методы
Опасные загрязняющие вещества в питьевой воде в исследуемом районе идентифицировались с помощью поиска литературы, а мониторинг отдельных загрязняющих веществ осуществлялся с апреля 2010 года по декабрь 2011 года в водосборных бассейнах, очистных сооружениях и кранах потребителей. Бремя заболеваний, обусловленное каждым загрязняющим веществом, оценивалось в скорректированных на нетрудоспособность годах жизни (ДАЛИ) с использованием данных о концентрации загрязняющего вещества, воздействии данного загрязняющего вещества, тяжести его последствий для здоровья и популяции потребителей.
Результаты
Были идентифицированы следующие загрязняющие вещества: микроорганизмы, кадмий, кобальт, хром, медь, железо, марганец, никель, свинец и цинк. Все они были обнаружены в водосборных бассейнах, однако только содержание кадмия, кобальта, хрома, марганца и свинца превысило нормативные значения, установленные Всемирной организацией здравоохранения (ВОЗ) для воды, прошедшей обработку. Было обнаружено присутствие загрязняющих веществ после обработки. В обеих системах расчетное бремя болезней было максимальным для хрома, а затем в порядке убывания следовали кадмий, свинец, марганец и кобальт. Общее бремя болезней всех загрязняющих веществ в двух системах составило 46 000 и 9500 ДАЛИ в год, или 0,14 и 0,088 ДАЛИ на человека в год, соответственно, что намного выше, чем контрольный уровень ВОЗ, равный 1×10−6 ДАЛИ на человека в год. Для каждого металла бремя болезней превысило контрольный уровень и было сопоставимо с влиянием микробного загрязнения, наблюдаемого в других странах Африки.
Вывод
Расчетное бремя болезней в результате загрязнения металлами воды в двух нигерийских системах водоснабжения было высоким. Лучшим способом его снижения является защита водосборов и предварительная обработка воды методом электрокоагуляции.
Introduction
In the fourth edition of the Guidelines for drinking-water quality, the World Health Organization (WHO) reiterates that a risk-based approach should be used to inform management decisions on the safety of drinking-water supplies.1 This approach entails the comprehensive assessment of both the risk to health and risk management and should encompass all stages of the water supply system, from water catchment to human consumption.1–3 In contrast, the concentration-based approach relies solely on determining whether the end product complies with standards that ensure consumer safety.2 Nevertheless, even with the risk-based approach, the concentration of contaminants in water ultimately determines the level of risk. However, in addition to concentration, the risk-based approach also takes into account parameters such as the level and duration of exposure to contaminants, their toxicity and the severity of the diseases they produce in assessing the need for mitigation. Furthermore, since this approach involves estimating the number of disability-adjusted life years (DALYs), it provides a framework for systematically comparing the disease burden associated with different pollutants,4 whether microbial, chemical or radiological.1
In this paper, we used a risk-based approach to identify the pollutants that posed the greatest risk to human health in two Nigerian water supply schemes and which should, therefore, be prioritized for removal.
Methods
Two water supply schemes in Nigeria were investigated: the Asejire and Eleyele schemes in Oyo State, which was included in “hydrological area 6” in the WHO and United Nations Children’s Fund (UNICEF) country report for Nigeria.5 The Asejire scheme, which was commissioned in 1972, is located in a suburb of the metropolis of Ibadan, about 30 km east of the city centre; the Eleyele scheme, which was commissioned in 1942, is situated within the metropolis. Ibadan is the capital of Oyo State and covers the largest area of any city in any country in tropical Africa.6 It is also the third most populous city in Nigeria: in 2010, the population was 2 893 137.6
The two water supply schemes are managed by the Water Corporation of Oyo State and together provide an urban piped water supply to around 25% of the people in Ibadan.7,8 Water for the Asejire scheme is collected by a dam on the River Osun and the level is maintained at about 81 m7 throughout the year, thereby ensuring a regular supply. Farming is prohibited in the catchment area7 and trees were planted on the banks of the dam to prevent soil erosion and silting. The Eleyele scheme’s dam collects water from two major rivers: the Ona and Ogunpa, which pass through Ibadan and are often polluted with effluent from unregulated industrial, commercial and residential quarters.7 Water for the treatment works is abstracted using a low-lift pump in the Asejire scheme and by gravity in the Eleyele scheme. Water purification is carried out using the conventional techniques of screening, aeration, coagulation, flocculation, sedimentation, filtration and chlorination. Treated water is delivered to consumers by tankers and through a pipe distribution system, which includes high-lift pumps and booster stations in strategic locations. Piped water is supplied mostly to yard and community taps, except in a few affluent areas where domestic water systems are common. Water is often stored in household containers because the supply is inconsistent. Secondary water treatment in homes is rare. The water supply schemes are unable to recover their operating costs despite government aid. Hence, the water supply is intermittent owing to a lack of chemicals and the high cost of pumping. Moreover, infrastructure maintenance is poor and as much as 40% of water can be lost from the distribution system.7,9
Identifying pollutants
We searched PubMed and Google scholar using the phrase “drinking water of Ibadan” to identify scientific articles published between 2000 and 2010 on relevant hazardous pollutants. We then selected pollutants whose reported concentration exceeded regulatory guideline values. In particular, we looked for chemicals prioritized by WHO10 (i.e. arsenic, fluoride and nitrate) but no study reported a high level. In fact, a project sponsored by WHO and UNICEF in Nigeria in 2004 and 20055 reported that all water from utility pipes and tankers studied complied with guidelines for arsenic, fluoride and nitrate. The hazardous pollutants we identified for inclusion in our investigation were: microbial organisms, cadmium, cobalt, chromium, copper, iron, manganese, nickel, lead and zinc.
For the two water supply schemes, we sampled water from dams, treatment works and consumer taps, which we regarded as the end-point of the distribution system, in 12 communities within the Ibadan metropolis: Apete, Eleyele, Mokola and Sango for the Eleyele scheme and Agodi, Alafara Oje, Basorun, Bere, Beyeruka, Iwo Road, Oduoba and Ojaba for the Asejire scheme. Dam water was sampled where the river enters the dam, in the middle of the dam and at the outlet to the treatment works. After treatment, samples were collected at three different taps within each treatment works. For the Asejire scheme, six different consumer taps were sampled in each community, whereas, for the Eleyele scheme, a variable number of samples was collected because water was not distributed equally at all times to all consumer taps. Before collection, we ran off the tap water for about 20 seconds, which is longer than most people would. Sampling was carried out every two months from April 2010 to December 2011. The Eleyele scheme was shut down temporarily between July 2011 and December 2011 because of flooding, which reduced the number of treated water samples collected at both the treatment works and consumer taps.
For microbiological screening, we collected water samples in aseptic, nonfluorescent 100-ml glass bottles with screw caps. Treated water samples collected at treatment works and consumer taps were dechlorinated using sodium thiosulfate. Within 2 hours of sampling, water was screened for the presence of total coliforms and Escherichia coli using Colilert powder. The bottles were capped and incubated for 24 hours at 35 °C. Yellow coloration indicated the presence of total coliforms and fluorescence at 365 nm indicated the presence of E. coli. Each water sample was screened three times.
For heavy metal analysis, water samples were collected in metal-free, plastic bottles with screw caps and nitric acid was added to achieve a pH below 2. Samples were stored in an ice chest below 4 °C and immediately transferred to a deep freezer on arrival at the laboratory. Metal digestion was carried out using nitric acid within 24 hours and metal concentrations were determined by atomic absorption spectrometry.
Risk assessment
We compared the concentrations of hazardous pollutants in water from treatment works and consumer taps with WHO guidelines1 (Table 1, available at: http://www.who.int/bulletin/volumes/91/8/12-115774) and identified those that exceeded guideline limits: they were cadmium, chromium, cobalt, lead and manganese (Table 2). In assessing the risk to health associated with the presence of a particular metal, we adopted the approach used by Crawford-Brown and Crawford-Brown,4 who related the risk of each individual health outcome associated with a particular metal to the probability of that health outcome occurring and the severity of the outcome, expressed in DALYs:
| (1) |
where the probability depends on exposure to the metal and its toxicity:
Table 1. Metal and microbial contamination and pH for two water supply schemes, Nigeria, 2010–2011.
| Location sampleda | No. of samples | Dry season |
Wet season |
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Microbial indicatorb |
pH | Upper 95% CI limit of concentration (mg/l) |
Microbial indicatorb |
pH | Upper 95% CI limit of concentration (mg/l) |
|||||||||||||||||||||
| Total coliforms | E. coli | Cd | Co | Cr | Cu | Fe | Mn | Ni | Pb | Zn | Total coliforms | E. coli | Cd | Co | Cr | Cu | Fe | Mn | Ni | Pb | Zn | |||||
| Asejire water supply scheme | ||||||||||||||||||||||||||
| Agodi | 60 | – | – | 7.55 | 0.05 | 0.02 | 0.14 | 0.09 | 0.55 | 0.02 | 0.04 | 0.14 | 0.43 | – | – | 7.43 | 0.03 | 0.09 | 0.27 | 0.04 | 0.31 | 0.16 | 0.02 | 0.24 | 0.32 | |
| Alafara Oje | 60 | – | – | 7.54 | 0.05 | 0.02 | 0.15 | 0.05 | 0.65 | 0.01 | 0.06 | 0.17 | 0.50 | – | – | 7.41 | 0.05 | 0.08 | 0.24 | 0.02 | 0.34 | 0.15 | 0.02 | 0.25 | 0.29 | |
| Basorun | 60 | – | – | 7.48 | 0.08 | 0.04 | 0.16 | 0.07 | 0.86 | 0.00 | 0.08 | 0.21 | 0.75 | – | – | 7.40 | 0.06 | 0.11 | 0.29 | 0.02 | 0.44 | 0.14 | 0.05 | 0.30 | 0.32 | |
| Bere | 60 | – | – | 7.50 | 0.07 | 0.02 | 0.17 | 0.03 | 0.72 | 0.01 | 0.07 | 0.17 | 0.65 | – | – | 7.50 | 0.04 | 0.10 | 0.26 | 0.01 | 0.35 | 0.14 | 0.04 | 0.26 | 0.31 | |
| Beyeruka | 60 | – | – | 7.48 | 0.05 | 0.02 | 0.14 | 0.05 | 0.58 | 0.02 | 0.06 | 0.16 | 0.56 | – | – | 7.44 | 0.04 | 0.08 | 0.26 | 0.01 | 0.24 | 0.15 | 0.03 | 0.25 | 0.34 | |
| Iwo Road | 60 | – | – | 7.52 | 0.07 | 0.03 | 0.17 | 0.06 | 0.72 | 0.02 | 0.07 | 0.19 | 0.68 | – | – | 7.53 | 0.06 | 0.10 | 0.23 | 0.01 | 0.29 | 0.12 | 0.05 | 0.28 | 0.29 | |
| Oduoba | 60 | – | – | 7.45 | 0.09 | 0.04 | 0.16 | 0.03 | 0.94 | 0.00 | 0.09 | 0.20 | 0.81 | – | – | 7.51 | 0.06 | 0.07 | 0.24 | 0.02 | 0.47 | 0.09 | 0.06 | 0.31 | 0.41 | |
| Ojaba | 60 | – | – | 7.42 | 0.06 | 0.02 | 0.14 | 0.05 | 0.63 | 0.01 | 0.08 | 0.17 | 0.65 | – | – | 7.55 | 0.05 | 0.08 | 0.28 | 0.02 | 0.37 | 0.13 | 0.04 | 0.27 | 0.34 | |
| Treatment works | 30 | – | – | 7.60 | 0.01 | 0.03 | 0.18 | 0.01 | 0.17 | 0.01 | 0.01 | 0.09 | 0.17 | – | – | 7.59 | 0.01 | 0.10 | 0.28 | 0.01 | 0.19 | 0.19 | 0.03 | 0.23 | 0.26 | |
| Dam water | 30 | + | + | 7.22 | 0.15 | 0.09 | 0.25 | 0.14 | 0.62 | 0.20 | 0.15 | 0.23 | 0.33 | + | + | 7.09 | 0.23 | 0.24 | 0.38 | 0.31 | 1.28 | 0.55 | 0.27 | 0.62 | 0.59 | |
| Eleyele water supply scheme | ||||||||||||||||||||||||||
| Apete | 48 | – | – | 7.30 | 0.05 | 0.01 | 0.09 | 0.03 | 0.62 | 0.06 | 0.03 | 0.15 | 0.28 | – | – | 7.41 | 0.04 | 0.12 | 0.10 | 0.01 | 0.48 | 0.32 | 0.01 | 0.38 | 0.26 | |
| Eleyele | 60 | – | – | 7.42 | 0.03 | 0.00 | 0.11 | 0.05 | 0.52 | 0.08 | 0.01 | 0.14 | 0.24 | – | – | 7.52 | 0.01 | 0.13 | 0.12 | 0.01 | 0.42 | 0.30 | 0.02 | 0.37 | 0.23 | |
| Mokola | 60 | – | – | 7.45 | 0.05 | 0.01 | 0.11 | 0.05 | 0.66 | 0.09 | 0.06 | 0.16 | 0.28 | – | – | 7.55 | 0.05 | 0.11 | 0.13 | 0.03 | 0.51 | 0.28 | 0.05 | 0.40 | 0.27 | |
| Sango | 32 | – | – | 7.27 | 0.04 | 0.00 | 0.09 | 0.04 | 0.57 | 0.06 | 0.02 | 0.15 | 0.22 | – | – | 7.58 | 0.03 | 0.13 | 0.11 | 0.02 | 0.46 | 0.28 | 0.02 | 0.38 | 0.26 | |
| Treatment works | 25 | – | – | 7.50 | 0.03 | 0.01 | 0.11 | 0.05 | 0.44 | 0.10 | 0.04 | 0.14 | 0.22 | – | – | 7.62 | 0.01 | 0.13 | 0.12 | 0.01 | 0.38 | 0.31 | 0.03 | 0.37 | 0.23 | |
| Dam water | 30 | + | + | 7.62 | 0.40 | 0.06 | 0.27 | 0.22 | 0.77 | 0.21 | 0.19 | 0.30 | 0.45 | + | + | 7.38 | 0.44 | 0.23 | 0.51 | 0.42 | 1.97 | 0.70 | 0.31 | 0.84 | 0.56 | |
| WHO MCL1 | NA | NA | NA | 6.5–8.5c | 0.003 | 0.10d,e | 0.05 | 2.0 | 2.0 | 0.04 | 0.07 | 0.01 | 3.0 | NA | NA | 6.5–8.5c | 0.003 | 0.10d,e | 0.05 | 2.0 | 2.0 | 0.04 | 0.07 | 0.01 | 3.0 | |
Cd, cadmium; CI, confidence interval; Co, cobalt; Cr, chromium; Cu, copper; E. coli, Escherichia coli; Fe, iron; MCL, maximum contaminant level; Mn, manganese; NA, not applicable; Ni, nickel; Pb, lead; WHO, World Health Organization; Zn, zinc.
a Water was sampled at consumer taps in the districts of Ibadan listed, at the output of treatment works and at the source dam.
b Contamination by total coliforms and Escherichia coli was recorded as present (i.e. +) or absent (i.e. –).
c Maximum contaminant level from the United States Environmental Protection Agency.
d Maximum contaminant level from the environmental media evaluation guide for children (California Department of Public Health).11
e Maximum contaminant level from health-based groundwater quality criteria (New Jersey Department of Environmental Protection) 12
Table 2. Mean metal concentrations, two water supply schemes, Nigeria, 2010–2011.
| Location sampled | Mean upper 95% CI limit of concentrationa (mg/l) |
||||
|---|---|---|---|---|---|
| Cd | Co | Cr | Mn | Pb | |
| Asejire water supply scheme | |||||
| Consumer tap waterb | 0.06 | 0.08 | 0.23 | 0.10 | 0.25 |
| Treatment works | 0.01 | 0.08 | 0.25 | 0.13 | 0.18 |
| Dam water | 0.20 | 0.19 | 0.34 | 0.43 | 0.49 |
| Eleyele water supply scheme | |||||
| Consumer tap waterb | 0.04 | 0.09 | 0.12 | 0.23 | 0.31 |
| Treatment works | 0.02 | 0.09 | 0.12 | 0.24 | 0.29 |
| Dam water | 0.43 | 0.17 | 0.43 | 0.54 | 0.66 |
| WHO MCL1 | 0.003 | 0.10c,d | 0.05 | 0.04 | 0.01 |
Cd, cadmium; CI, confidence interval; Co, cobalt; Cr, chromium; MCL, maximum contaminant level; Mn, manganese; Pb, lead; WHO, World Health Organization.
a The mean annual upper 95% confidence interval (CI) limit for the concentration was calculated from the mean upper 95% CI limit of the concentration in the dry season (Cd) and the mean upper 95% CI limit of the concentration in the wet season (Cw) by assuming that the dry season lasted 4 months and the wet season, 8 months and using the formula: ((Cd × 4) + (Cw × 8))⁄12.
b The mean upper 95% CI limit of the concentration in consumer tap water during the wet and dry seasons was calculated by averaging measurements in all supply areas for a particular scheme during the respective season.
c Maximum contaminant level from the environmental media evaluation guide for children (California Department of Public Health).11
d Maximum contaminant level from health-based groundwater quality criteria (New Jersey Department of Environmental Protection.)12
| (2) |
Exposure
As a summary measure of biologically relevant exposure to a metal in water, we used the chronic daily intake of the metal, in mg per kg per day, by children and adult females and males, as defined in Equation 3, Equation 4 and Equation 5.13–16
For the oral ingestion of treated water:
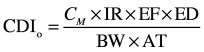 |
(3) |
where CDIo is the oral chronic daily intake, CM is the upper 95% confidence interval (CI) limit for the concentration of the metal in water, IR is the ingestion rate, EF is exposure frequency, ED is exposure duration, BW is body weight and AT is the lifetime averaging time.
For dermal contact with treated water:
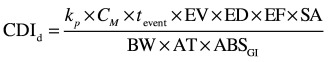 |
(4) |
where CDId is the dermal chronic daily intake, kp is the skin permeability coefficient, tevent is the exposure event duration, EV is the event frequency, SA is the skin surface area involved and ABSGI is the gastrointestinal absorption fraction.
Combining these terms, the total chronic daily intake (CDI) is given as:
| (5) |
In calculations, we used exposure data from Adewuyi et al.17 because they reflect typical water usage in Nigeria (Table 3, available at: http://www.who.int/bulletin/volumes/91/8/12-115774).
Table 3. Parameters for calculating exposure to metallic contaminants in water17.
| Parameter | Consumera | Value | Type of exposure |
|---|---|---|---|
| Ingestion rate | Adult | 2 l/day | Oral |
| Child | 1 l/day | Oral | |
| Exposure duration | Adult | 30 years | Oral and dermal |
| Child | 6 years | Oral and dermal | |
| Exposure frequency | Adult or child | 350 days per year | Oral and dermal |
| Body weight | Adult male | 70 kg | Oral and dermal |
| Adult female | 58 kg18 | Oral and dermal | |
| Child | 15 kg | Oral and dermal | |
| Lifetime averaging time | Adult or child | 54 years × 365 days per year | Oral and dermal |
| Event frequency | Adult or child | 1 event per day | Dermal |
| Event duration | Adult | 0.25 hours per event | Dermal |
| Child | 0.25 hours per event | Dermal | |
| Skin surface area | Adult | 18 000 cm2 | Dermal |
| Child | 6600 cm2 | Dermal | |
| Skin permeability coefficient | |||
| Cadmium | Adult or child | 1 × 10−3 cm/hour | Dermal |
| Cobalt | Adult or child | 0.4 × 10−3 cm/hour | Dermal |
| Chromium | Adult or child | 2 × 10−3 cm/hour | Dermal |
| Iron | Adult or child | 1 × 10−3 cm/hour | Dermal |
| Manganese | Adult or child | 1 × 10−3 cm/hour | Dermal |
| Lead | Adult or child | 0.1 × 10−3 cm/hour | Dermal |
| Gastrointestinal absorption fraction | |||
| Cadmium | Adult or child | 5% | Dermal |
| Cobalt | Adult or child | 80% | Dermal |
| Chromium | Adult or child | 2.5% | Dermal |
| Manganese | Adult or child | 6% | Dermal |
| Lead | Adult or child | 15% | Dermal |
a Children were aged less than 6 years and adults, 7 to 54 years.
Toxicity
Crawford-Brown and Crawford-Brown4 and Pennington et al.19 argue that measures of toxicity, such as the reference dose, acceptable daily intake, tolerable daily intake and minimal risk level, were developed for assessing the health risk of individual hazardous substances in a regulatory context, not for comparing hazards. Consequently, Crawford-Brown and Crawford-Brown proposed using the 1% benchmark dose as the metric of toxicity for the noncancerous effects of a substance. This is the dose at which 1% of the population would develop the specified health outcome and is usually expressed in mg per kg per day. Alternatively, Pennington et al. proposed a central estimate of the effect dose, ED10, also expressed in mg per kg per day, which is the dose that results in a 10% increase in the incidence of the specified health outcome relative to the background level. In addition, the health risk can be extrapolated for lower doses using a slope factor, βED10. We used Pennington et al.’s approach for estimating noncancerous effects on health and selected the following algorithms for ED10:
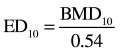 |
(6) |
| (7) |
| (8) |
For cadmium and chromium, we estimated ED10 using values for BMD10 obtained from the literature, where BMD10 is the lower 95% confidence limit for the dose that results in a 10% increase in the incidence of the specified health outcome relative to the background level.19 For cobalt and manganese, we used the no-observable-adverse-effect level (NOAEL) and the lowest-observable-adverse-effect level (LOAEL), respectively, both of which are expressed in mg per kg per day. These algorithms all assume a linear relationship between dose and response. Where dose levels were obtained in mice, we used a subchronic-to-chronic conversion factor of 3.3 and an animal-to-human conversion factor of 13 to derive equivalent dose levels in humans, as recommended by Pennington et al.19 We did not use the additional “margin-of-safety” factor of 3 that is generally used for regulatory purposes. We then calculated values for βED10 from the ED10 values for all noncarcinogenic health outcomes associated with these four metals (Table 4, available at: http://www.who.int/bulletin/volumes/91/8/12-115774):
Table 4. Parameters for estimating the toxicity of metal contaminants in water.
| Metal contaminant and health outcome | BMD10a (mg/kg per day) | NOAEL (mg/kg per day) | LOAEL (mg/kg per day) | ED10b (mg/kg per day) | βED10c (mg/kg per day) |
|---|---|---|---|---|---|
| Cadmium | |||||
| Renal abnormality | 0.036 × 10−3 (0.6 µg/g creatinine)20 | NA | NA | 0.067 × 10−3 | 1500 |
| Osteoporosis | 0.03 × 10−3 (0.5 µg/g creatinine)21–23 | NA | NA | 0.056 × 10−3 | 1800 |
| Cobalt | |||||
| Goitre and hypothyroidism | NA | 0.0524 | NA | 0.08 | 1.3 |
| Cardiomyopathy | NA | 0.0524 | NA | 0.08 | 1.3 |
| Polycythaemia vera | NA | 0.0524 | NA | 0.08 | 1.3 |
| Chromium | |||||
| Chronic liver inflammation | 0.14d, 25 | NA | NA | 0.013 | 330 |
| Diffuse epithelial hyperplasia in the duodenum | 0.09d, 25 | NA | NA | 3.9 × 10−3 | 1100 |
| Histiocytic infiltration of the liver | 0.12d, 25 | NA | NA | 5.2 × 10−3 | 830 |
| Acinus cytoplasmic alteration in the pancreas | 0.52d, 25 | NA | NA | 0.022 | 191 |
| Oral cavity and oropharyngeal cancer | NA | NA | NA | NA | 0.25 (i.e. 0.5 × CSFe) |
| Oesophageal cancer | NA | NA | NA | NA | 0.25 (i.e. 0.5 × CSFe) |
| Gastric cancer | NA | NA | NA | NA | 0.25 (i.e. 0.5 × CSFe) |
| Small intestine cancer | NA | NA | NA | NA | 0.25 (i.e. 0.5 × CSFe) |
| Manganese | |||||
| Neurological abnormality | NA | NA | 0.08126,27 | 0.024 | 4.2 |
CSF, cancer slope factor; BMD, is the lower 95% confidence limit for the dose that results in a 10% increase in the incidence of the specified health outcome relative to the background level; ED, exposure duration; LOAEL, lowest-observable-adverse-effect level; NA, not applicable; NOAEL, no-observable-adverse-effect level.
a BMD10 is the lower 95% confidence limit for the dose that results in a 10% increase in the incidence of the specified health outcome relative to the background level.19
b ED10 is the central estimate of the effect dose associated with a 10% increase in the incidence of the health outcome relative to the background level.19
c βED10 is a slope factor used for calculating health risk at low doses.
d Since the source BMD10 value was for mice, the equivalent dose levels in humans were derived using an animal-to-human conversion factor of 13 and a subchronic-to-chronic conversion factor of 3.3.
e The cancer slope factor (CSF) for chromium given by the United States Environmental Protection Agency is 0.5.28
 |
(9) |
Since we were not able to obtain data on the reference toxic dose for lead in water, we applied WHO’s method for estimating the health risks of lead.29 First, we compared the lead concentrations we observed with the results of a cross-sectional study carried out in the District of Columbia in the United States of America,30,31 which linked levels of lead in water to blood lead levels. That study reported that people who drank water with a lead concentration greater than 0.3 mg per litre, which was comparable to levels observed in our study, had a blood lead level below the level of concern of the United States Centers for Disease Control and Prevention: 10 µg per dl for children aged 6 months to 15 years and 25 µg per dl for adults. Hence, we assumed that the blood lead level corresponding to the lead concentrations in water we observed (Table 1) would fall within the range of 5 to 10 µg per dl and, in calculations, we used a mean of 7.5 µg per dl, which is associated with a mean reduction of 0.65 in intelligence quotient in children and a mean increase of 0.625 mmHg and 0.4 mmHg in systolic blood pressure in adult males and females, respectively.29
The presence of chromium in treated water has been associated with several types of cancer, assuming all species of the metal are oxidized to Cr6+: oral, oesophageal, gastric and small intestine cancer.32,33 To estimate βED10 for the carcinogenic effects of chromium, we adopted the method proposed by Crettaz et al.,34 which relates the cancer slope factor (CSF) for chromium given by the United States Environmental Protection Agency (i.e. 0.5 kg–days per mg) to βED10:
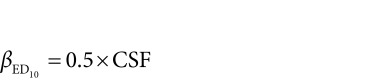 |
(10) |
Probability
For each health outcome associated with cadmium, cobalt, chromium and manganese contamination, we used the estimates for exposure and toxicity obtained in the previous steps of the calculation to derive the probability of that health outcome:
| (11) |
where LPO is the lifetime probability of the outcome.
For lead, we calculated the probability of mild mental retardation (PMMR) associated with a mean reduction of 0.65 in intelligence quotient in children aged 4 years or under using the equation given by Fewtrell et al.:29
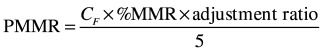 |
(12) |
where CF is the fraction of consumers aged 4 years or under (Table 5, available at: http://www.who.int/bulletin/volumes/91/8/12-115774) and %MMR is the percentage of consumers that will enter the intelligence quotient range indicating mild mental retardation. The adjustment ratio takes into account mental retardation caused by communicable diseases and iodine deficiency and the higher incidence of mental retardation in developing countries relative to developed countries. Fewtrell et al.29 give a value of 0.24% for %MMR and 2.05 for the regional adjustment ratio.
Table 5. Disease burden associated with lead contamination of water from consumer taps, two water supply schemes combined, Nigeria, 2010–2011.
| Consumer | Age rangea (years) | Fraction of all consumers (CF) | Health outcome |
Estimated disease burden (DALYs per person per year [x 10−3]) |
||||
|---|---|---|---|---|---|---|---|---|
| Type | RR29 | Probability | Individual health outcome | All health outcomes | ||||
| All | 0–4 and 15–54 | 0.6877 | All | NA | NA | NA | 1.6 | |
| Child | 0–4 | 0.1815 | Mild mental retardation | NA | 0.18 × 10−3 | 0.0022 | NA | |
| Adult female | 15–54 | 0.2341 | Ischaemic heart disease | 1.024 | 8.9 × 10−3 | 0.11 | NA | |
| Stroke | 1.032 | 0.012 | 0.15 | NA | ||||
| Hypertensive disease | 1.063 | 0.023 | 0.29 | NA | ||||
| Other cardiac disease | 1.007 | 2.6 × 10−3 | 0.032 | NA | ||||
| Adult male | 15–54 | 0.2721 | Ischaemic heart disease | 1.038 | 0.014 | 0.17 | NA | |
| Stroke | 1.052 | 0.020 | 0.25 | NA | ||||
| Hypertensive disease | 1.101 | 0.037 | 0.46 | NA | ||||
| Other cardiac disease | 1.034 | 0.013 | 0.16 | NA | ||||
DALY, disability-adjusted life year; NA, not applicable; RR, relative risk.
a Mild mental retardation is largely irreversible and is considered to occur only in the first year of life. The burden in children aged between 1 and 14 years is attributed to events in the first year. Since the population data available were for the 0–4 year age group, we assumed that the probability of mild mental retardation for infants aged under 1 year was one fifth that for the 0–4 year age group (Equation 12).29
For adults, the probability of cardiovascular disease due to lead (PCVDL) in men and women was calculated using:
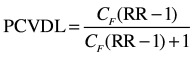 |
(13) |
where CF is the fraction of consumers aged 15 to 54 years who were male or female, respectively, and RR is the corresponding relative risk of cardiovascular disease in men or women (Table 5).
Severity
The severity of each health outcome was quantified by obtaining an estimate of the associated degree of disability. For all outcomes other than cancer, we used the value of 0.67 DALYs per affected person attributable to irreversible systemic disease given by Pennington et al.19 Crettaz et al.34 derived the number of DALYs per person due to tumours at various sites using international data reported by Murray and Lopez:35 for oral cavity and oropharyngeal cancer, it was 3.5 DALYs per affected person; for oesophageal cancer, 9.3 DALYs per person; and for gastric cancer, 7.2 DALYs per person. Although these authors did not report a figure for cancer of the small intestine, they suggested a default value of 6.7 DALYs per affected person.34
Risk
The total risk to health of each individual metal contaminant (IR), expressed in DALYs per person per year, was calculated by summing the risks for each health outcome associated with that metal:
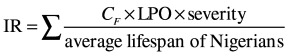 |
(14) |
where CF is the fraction of consumers exposed to the health outcome (Table 6 and Table 7, both available at: http://www.who.int/bulletin/volumes/91/8/12-115774), severity is expressed in DALYs per affected person and the average lifespan of Nigerians is 54 years.36
Table 6. Disease burden due to metal contamination of water from treatment works, two water supply schemes, Nigeria, 2010–2011.
| Metal contaminant and health outcome | Consumera | Fraction of all consumers (CF) | Asejire water supply scheme |
Eleyele water supply scheme |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronic daily intake (mg/kg per day [x 10−3]) | Lifetime probability of health outcome | Estimated disease burden (DALYs per person per year [x 10−3]) |
Chronic daily intake (mg/kg per day [x 10−3]) | Lifetime probability of health outcome | Estimated disease burden (DALYs per person per year [x 10−3]) |
||||||
| Individual health outcome associated with metal | All health outcomes associated with metal | Individual health outcome associated with metal | All health outcomes associated with metal | ||||||||
| Cadmium | All | 1 | NA | NA | NA | 6.1 | NA | NA | NA | 15 | |
| Renal abnormality | All | 1 | NA | NA | 2.8 | NA | NA | NA | 6.8 | NA | |
| Child | 0.2425 | 0.073 | 0.11 | NA | NA | 0.18 | 0.26 | NA | NA | ||
| Adult female | 0.3726 | 0.19 | 0.28 | NA | NA | 0.47 | 0.69 | NA | NA | ||
| Adult male | 0.3849 | 0.16 | 0.25 | NA | NA | 0.39 | 0.59 | NA | NA | ||
| Osteoporosis | All | 1 | NA | NA | 3.3 | NA | NA | NA | 8.3 | NA | |
| Child | 0.2425 | 0.073 | 0.13 | NA | NA | 0.18 | 0.32 | NA | NA | ||
| Adult female | 0.3726 | 0.19 | 0.35 | NA | NA | 0.47 | 0.84 | NA | NA | ||
| Adult male | 0.3849 | 0.16 | 0.29 | NA | NA | 0.39 | 0.71 | NA | NA | ||
| Cobalt | All | 1 | NA | NA | NA | 0.051 | NA | NA | NA | 0.063 | |
| Goitre and hypothyroidism | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.021 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Cardiomyopathy | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.021 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Polycythaemia vera | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.021 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Chromium | All | 1 | NA | NA | NA | 110 | NA | NA | NA | 54 | |
| Chronic liver inflammation | All | 1 | NA | NA | 15 | NA | NA | NA | 7.2 | NA | |
| Child | 0.2425 | 1.8 | 0.60 | NA | NA | 0.87 | 0.29 | NA | NA | ||
| Adult female | 0.3726 | 4.6 | 1.5 | NA | NA | 2.2 | 0.73 | NA | NA | ||
| Adult male | 0.3849 | 3.9 | 1.3 | NA | NA | 1.9 | 0.62 | NA | NA | ||
| Diffuse epithelial hyperplasia in the duodenum | All | 1 | NA | NA | 50 | NA | NA | NA | 24 | NA | |
| Child | 0.2425 | 1.8 | 2.0 | NA | NA | 0.87 | 0.96 | NA | NA | ||
| Adult female | 0.3726 | 4.6 | 5.1 | NA | NA | 2.2 | 2.4 | NA | NA | ||
| Adult male | 0.3849 | 3.9 | 4.3 | NA | NA | 1.9 | 2.1 | NA | NA | ||
| Histiocytic infiltration of the liver | All | 1 | NA | NA | 38 | NA | NA | NA | 18 | NA | |
| Child | 0.2425 | 1.8 | 1.5 | NA | NA | 0.87 | 0.72 | NA | NA | ||
| Adult female | 0.3726 | 4.6 | 3.8 | NA | NA | 2.2 | 1.8 | NA | NA | ||
| Adult male | 0.3849 | 3.9 | 3.3 | NA | NA | 1.9 | 1.6 | NA | NA | ||
| Acinus cytoplasmic alteration in the pancreas | All | 1 | NA | NA | 8.7 | NA | NA | NA | 4.2 | NA | |
| Child | 0.2425 | 1.8 | 0.35 | NA | NA | 0.87 | 0.17 | NA | NA | ||
| Adult female | 0.3726 | 4.6 | 0.89 | NA | NA | 2.2 | 0.42 | NA | NA | ||
| Adult male | 0.3849 | 3.9 | 0.75 | NA | NA | 1.9 | 0.36 | NA | NA | ||
| Oral cavity and oropharyngeal cancer | All | 1 | NA | NA | 0.034 | NA | NA | NA | 0.015 | NA | |
| Child | 0.2425 | 0.98 | 0.25 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.7 | 0.67 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.3 | 0.57 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Oesophageal cancer | All | 1 | NA | NA | 0.091 | NA | NA | NA | 0.041 | NA | |
| Child | 0.2425 | 0.98 | 0.25 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.7 | 0.67 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.3 | 0.57 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Gastric cancer | All | 1 | NA | NA | 0.071 | NA | NA | NA | 0.032 | NA | |
| Child | 0.2425 | 0.98 | 0.25 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | 0.032 | NA | ||
| Adult female | 0.3726 | 2.7 | 0.67 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.3 | 0.57 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Small intestine cancer | All | 1 | NA | NA | 0.066 | NA | NA | NA | 0.030 | NA | |
| Child | 0.2425 | 0.98 | 0.25 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.7 | 0.67 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.3 | 0.57 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Manganese | All | 1 | NA | NA | NA | 0.099 | NA | NA | NA | 0.18 | |
| Neurological abnormality | All | 1 | NA | NA | 0.099 | NA | NA | NA | 0.18 | NA | |
| Child | 0.2425 | 0.96 | 0.40 × 10−3 | NA | NA | 1.7 | 7.1 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.5 | 0.010 | NA | NA | 4.5 | 0.018 | NA | NA | ||
| Adult male | 0.3849 | 2.1 | 8.6 × 10−3 | NA | NA | 3.8 | 0.016 | NA | NA | ||
DALY, disability-adjusted life year; NA, not applicable.
a Children were aged under 6 years and adults, 7 to 54 years.
Table 7. Disease burden due to metal contamination of water from consumer taps, two water supply schemes, Nigeria, 2010–2011.
| Metal contaminant and health outcome | Consumera | Fraction of all consumers (CF) | Asejire water supply scheme |
Eleyele water supply scheme |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronic daily intake (mg/kg per day [x 10−3]) | Lifetime probability of health outcome | Estimated disease burden (DALYs per person per year [x 10−3]) |
Chronic daily intake (mg/kg per day [x 10−3]) | Lifetime probability of health outcome | Estimated disease burden (DALYs per person per year [x 10−3]) |
||||||
| Individual health outcome associated with metal | All health outcomes associated with metal | Individual health outcome associated with metal | All health outcomes associated with metal | ||||||||
| Cadmium | All | 1 | NA | NA | NA | 38 | NA | NA | NA | 31 | |
| Renal abnormality | All | 1 | NA | NA | 17 | NA | NA | NA | 14 | NA | |
| Child | 0.2425 | 0.44 | 0.66 | NA | NA | 0.36 | 0.53 | NA | NA | ||
| Adult female | 0.3726 | 1.1 | 1.7 | NA | NA | 0.93 | 1.4 | NA | NA | ||
| Adult male | 0.3849 | 0.96 | 1.5 | NA | NA | 0.79 | 1.2 | NA | NA | ||
| Osteoporosis | All | 1 | NA | NA | 21 | NA | NA | NA | 17 | NA | |
| Child | 0.2425 | 0.44 | 0.80 | NA | NA | 0.36 | 0.65 | NA | NA | ||
| Adult female | 0.3726 | 1.1 | 2.1 | NA | NA | 0.93 | 1.7 | NA | NA | ||
| Adult male | 0.3849 | 0.96 | 1.8 | NA | NA | 0.79 | 1.4 | NA | NA | ||
| Cobalt | All | 1 | NA | NA | NA | 0.051 | NA | NA | NA | 0.063 | |
| Goitre and hypothyroidism | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.021 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Cardiomyopathy | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.021 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Polycythaemia vera | All | 1 | NA | NA | 0.017 | NA | NA | NA | 0.21 | NA | |
| Child | 0.2425 | 0.53 | 0.65 × 10−3 | NA | NA | 0.62 | 0.77 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.4 | 1.7 × 10−3 | NA | NA | 1.6 | 2.1 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 1.2 | 1.5 × 10−3 | NA | NA | 1.4 | 1.7 × 10−3 | NA | NA | ||
| Chromium | All | 1 | NA | NA | NA | 100 | NA | NA | NA | 54 | |
| Chronic liver inflammation | All | 1 | NA | NA | 14 | NA | NA | NA | 7.2 | NA | |
| Child | 0.2425 | 1.7 | 0.55 | NA | NA | 0.87 | 0.29 | NA | NA | ||
| Adult female | 0.3726 | 4.3 | 1.4 | NA | NA | 2.2 | 0.73 | NA | NA | ||
| Adult male | 0.3849 | 3.6 | 1.2 | NA | NA | 1.9 | 0.62 | NA | NA | ||
| Diffuse epithelial hyperplasia in the duodenum | All | 1 | NA | NA | 46 | NA | NA | NA | 24 | NA | |
| Child | 0.2425 | 1.7 | 1.8 | NA | NA | 0.87 | 0.96 | NA | NA | ||
| Adult female | 0.3726 | 4.3 | 4.7 | NA | NA | 2.2 | 2.4 | NA | NA | ||
| Adult male | 0.3849 | 3.6 | 4.0 | NA | NA | 1.9 | 2.1 | NA | NA | ||
| Histiocytic infiltration of the liver | All | 1 | NA | NA | 35 | NA | NA | NA | 18 | NA | |
| Child | 0.2425 | 1.7 | 1.4 | NA | NA | 0.87 | 0.72 | NA | NA | ||
| Adult female | 0.3726 | 4.3 | 3.5 | NA | NA | 2.2 | 1.8 | NA | NA | ||
| Adult male | 0.3849 | 3.6 | 3.0 | NA | NA | 1.9 | 1.6 | NA | NA | ||
| Acinus cytoplasmic alteration in the pancreas | All | 1 | NA | NA | 8.0 | NA | NA | NA | 4.2 | NA | |
| Child | 0.2425 | 1.7 | 0.32 | NA | NA | 0.87 | 0.17 | NA | NA | ||
| Adult female | 0.3726 | 4.3 | 0.82 | NA | NA | 2.2 | 0.42 | NA | NA | ||
| Adult male | 0.3849 | 3.6 | 0.69 | NA | NA | 1.9 | 0.36 | NA | NA | ||
| Oral cavity and oropharyngeal cancer | All | 1 | NA | NA | 0.032 | NA | NA | NA | 0.015 | NA | |
| Child | 0.2425 | 0.90 | 0.23 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.5 | 0.62 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.1 | 0.52 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Oesophageal cancer | All | 1 | NA | NA | 0.084 | NA | NA | NA | 0.041 | NA | |
| Child | 0.2425 | 0.90 | 0.23 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.5 | 0.62 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.1 | 0.52 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Gastric cancer | All | 1 | NA | NA | 0.065 | NA | NA | NA | 0.032 | NA | |
| Child | 0.2425 | 0.90 | 0.23 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.5 | 0.62 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.1 | 0.52 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Small intestine cancer | All | 1 | NA | NA | 0.060 | NA | NA | NA | 0.030 | NA | |
| Child | 0.2425 | 0.90 | 0.23 × 10−3 | NA | NA | 0.45 | 0.11 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 2.5 | 0.62 × 10−3 | NA | NA | 1.2 | 0.30 × 10−3 | NA | NA | ||
| Adult male | 0.3849 | 2.1 | 0.52 × 10−3 | NA | NA | 1.0 | 0.26 × 10−3 | NA | NA | ||
| Manganese | All | 1 | NA | NA | NA | 0.077 | NA | NA | NA | 0.18 | |
| Neurological abnormality | All | 1 | NA | NA | 0.077 | NA | NA | NA | 0.18 | NA | |
| Child | 0.2425 | 0.74 | 3.0 × 10−3 | NA | NA | 1.6 | 6.8 × 10−3 | NA | NA | ||
| Adult female | 0.3726 | 1.9 | 7.8 × 10−3 | NA | NA | 4.3 | 0.018 | NA | NA | ||
| Adult male | 0.3849 | 1.6 | 6.6 × 10−3 | NA | NA | 3.6 | 0.015 | NA | NA | ||
DALY, disability-adjusted life year; NA, not applicable.
a Children were aged under 6 years and adults, 7 to 54 years.
Then we calculated the total risk to the consumer population (RCP) for each water supply scheme, expressed in DALYs per year, from the individual risks associated with all metal contaminants (IRMC) in each scheme, weighted according to observed contaminant levels:
| (15) |
In estimating the consumer population for each water supply scheme, we used information on the distribution capacities of the schemes and the percentage of the population of Ibadan covered by the two schemes. The Asejire scheme provided 82 000 m3 per day and the Eleyele scheme, 27 000 m3 per day, which correspond to 75% and 25% of the total supplied by the two schemes, respectively. In theory, this total should have accounted for 25% of the water supply for the metropolis. However, we assumed a reduction of 5% due to leakage and another reduction of 5% due to political exaggeration; consequently, we assumed these supplies accounted for 15% of the supply to Ibadan. Using population data for 2010, we estimated that the consumer population for the two schemes combined was 433 971: 325 478 for the Asejire scheme (i.e. 75%) and 108 493 for the Eleyele scheme (i.e. 25%).
Results
The results of our analysis of water samples from dams, treatment works and consumer taps are shown in Table 1 for selected pollutants. Although the total coliform and E. coli tests were positive for dam water from both water supply schemes, these contaminants were absent from water from treatment works and consumer taps.
The upper 95% CI limit for the concentrations of cadmium, chromium, lead, manganese, and nickel in dam water exceeded WHO guideline values1 in both wet and dry seasons, whereas the concentrations of copper, iron and zinc were below guideline values. The upper 95% CI limit for the concentration of cobalt in dam water exceeded the maximum contaminant level given by both the environmental media evaluation guide for children11 and health-based groundwater quality criteria12 in the wet season but not in the dry season (Table 1). Although water treatment reduced these concentrations substantially, metal contamination also occurred in the distribution system: levels of cadmium, copper, iron, lead, nickel and zinc were much higher at consumer taps than in water leaving the treatment works. In particular, the upper 95% CI limit for the concentrations of cadmium, chromium, manganese and lead in treated water exceeded WHO guideline values (Table 2).1 Consequently, these four metals were used in the risk assessment. Cobalt was also included because no WHO guideline value was available.
Table 5 shows the disease burden due to lead contamination. Table 6 and Table 7 show the estimated disease burden due to cadmium, cobalt, chromium and manganese contamination of the two water supply systems. Table 6 shows the hypothetical disease burden that would result if consumers received water directly from the treatment works. This was used for comparison with the disease burden associated with water from consumer taps (Table 7). Comparison of Table 6 and Table 7 shows that there was no difference in the disease burden due to chromium, manganese or cobalt contamination between water from treatment works and water from consumer taps. In contrast, the estimated number of DALYs per person per year attributable to cadmium contamination was much greater for water from consumer taps. We could not carry out a similar comparison for lead because we estimated the disease burden using a concentration range rather than a mean value.
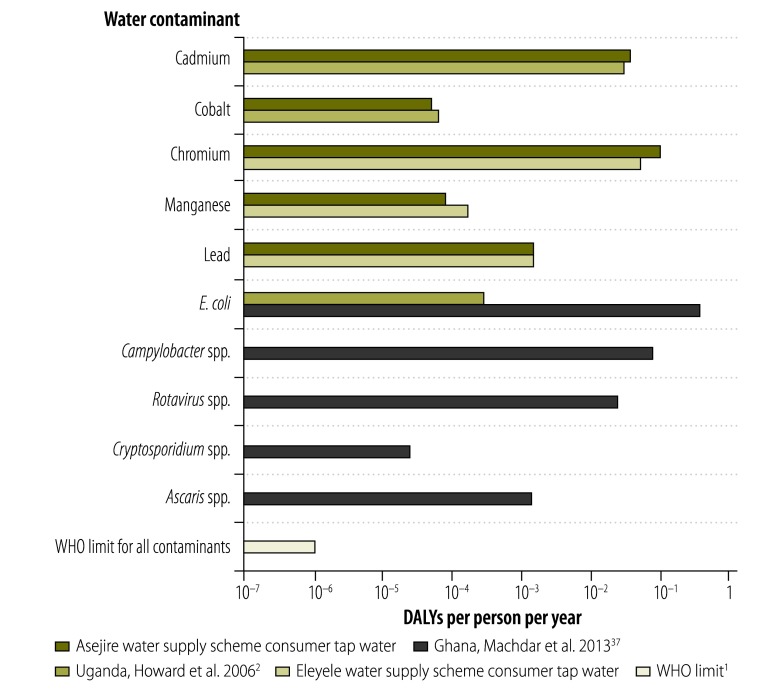
We also compared our estimates of the disease burden due to water contamination at consumer taps supplied by the two water supply schemes with that associated with WHO’s reference limit and with microbial contamination reported in the literature (Fig. 1). The disease burden due to chromium contamination alone in our study was around 100 000 times that associated with WHO’s reference limit and around 1000 times that due to pathogenic E. coli contamination of treated water in Uganda, which was 0.292 × 10−3 DALYs per person per year.2 Recently, Machdar et al.37 reported that the disease burden, in DALYs per person per year, due to different types of contamination in Ghana was 0.395 for pathogenic E. coli, 0.0813 for Campylobacter spp., 0.026 for rotavirus, 0.025 × 10−3 for Cryptosporidium spp. and 1.4 × 10−3 for Ascaris spp.
Fig. 1.
Disease burden of water supply scheme contamination in Nigeria compared with literature values, 2010–2011
DALY, disability-adjusted life year; E. coli, Escherichia coli; WHO, World Health Organization.
Table 8 shows the total disease burden due to each metal contaminant among consumers supplied by the two water supply schemes. Chromium had the largest effect on human health in both schemes, followed in decreasing order by cadmium, lead, manganese and cobalt. The total number of DALYs per year attributable to metal contamination of the Asejire and Eleyele water supply schemes was 46 000 and 9500, respectively. This is equivalent to 0.14 and 0.088 DALYs per person per year, respectively: both values are much higher than the WHO reference limit of 1 × 10−6 DALYs per person per year but lower than the 0.5 DALYs per person per year reported for microbial contaminants in Ghana.37
Table 8. Disease burden due to metal contamination of consumer tap water in populations using two water supply schemes, Nigeria, 2010–2011.
| Water supply scheme | Estimated disease burden (DALYs per year) |
|||||
|---|---|---|---|---|---|---|
| Cd | Co | Cr | Mn | Pb | Total | |
| Asejire | 12 000 | 17 | 33 000 | 25 | 520 | 46 000 |
| Eleyele | 3400 | 6.8 | 5900 | 20 | 170 | 9500 |
Cd, cadmium; Co, cobalt; Cr, chromium; DALY, disability-adjusted life year; Mn, manganese; Pb, lead.
Discussion
Our risk-based approach to identifying the pollutants in two Nigerian water supply schemes that posed the greatest risk to human health showed that the most important were chromium, cadmium, lead, manganese and cobalt, in decreasing order of their effect on health. The estimated disease burden due to each metal contaminant far exceeded reference limits and was comparable with the results of African studies of the disease burden of microbial contamination. In contrast, total coliforms and E. coli were not present in consumer tap water in the Nigerian water supply schemes, which indicates that treatment was effective in removing microbial contaminants present in dam water. Nevertheless, given the large number of pathogens that could be present in water, this negative finding should be taken with some degree of caution.
Metal contamination also occurred in the distribution system and, in particular, post-treatment contamination was substantial for cadmium and lead. However, most of the disease burden associated with these two contaminants appeared to be due to contaminated dam water and ineffective treatment. Consequently, reducing the disease burden could best be achieved by protecting water catchment and upgrading water treatment systems. Several studies have shown that electrocoagulation can reduce the quantity of metal ions in water to a very low level.38–41 The technique could be particularly effective when used before conventional chemical treatment. Further, comparison of the disease burden due to metal contamination observed in our study and that due to microbial contamination in other African studies indicates that chemical contaminants could be as important as microbial contaminants in piped water supplies.
Acknowledgements
This study was made possible by the World Academy of Sciences (TWAS) in Trieste and the Council of Scientific and Industrial Research in New Delhi, which awarded a doctoral fellowship to Tunde O Etchie.
Competing interests:
None declared.
References
- 1.Guidelines for drinking water quality. 4th edition. Geneva: World Health Organization; 2011. [Google Scholar]
- 2.Howard G, Pedley S, Tibatemwa S. Quantitative microbial risk assessment to estimate health risks attributable to water supply: can the technique be applied in developing countries with limited data? J Water Health. 2006;4:49–65. [PubMed] [Google Scholar]
- 3.Bartram J, Corrales L, Davison A, Deere D, Drury D, Gordon B et al. Water safety plan manual: step-by-step risk management for drinking-water suppliers. Geneva: World Health Organization; 2009. Available from: http://whqlibdoc.who.int/publications/2009/9789241562638_eng_print.pdf [accessed 20 March 2013]. [Google Scholar]
- 4.Crawford-Brown D, Crawford-Brown S. Cumulative risk assessment framework for waterborne contaminants. J Environ Protect. 2012;3:400–13. doi: 10.4236/jep.2012.35050. [DOI] [Google Scholar]
- 5.Ince M, Basir D, Oni OOO, Awe EO, Ogbechie V, Korve K et al. Rapid assessment of drinking-water quality in the Federal Republic of Nigeria: country report of the pilot project implementation in 2004–2005 Geneva & New York: World Health Organization & United Nations Children’s Fund; 2010. [Google Scholar]
- 6.Ajayi O, Agbola SB, Olokesusi BF, Wahab B, Taiwo OJ, Gbadegesin M et al. Flood management in an urban setting: a case study of Ibadan metropolis. In: Martins O, Idowu OA, Mbajiorgu CC, Jimoh OD, Oluwasanya GO, editors. Hydrology for disaster management Nsukka: Nigerian Association of Hydrological Sciences; 2012:65-81. Available from: http://journal.unaab.edu.ng/index.php/NAHS/article/download/914/882 [accessed 21 May 2013].
- 7.African Development Bank Group [Internet]. Project: urban water supply and sanitation for Oyo and Taraba States. Country: Nigeria. Project appraisal report. Available from: http://www.afdb.org/fileadmin/uploads/afdb/Documents/Project-and-Operations/AR%20Nigeria002En.pdf [accessed 21 May 2013].
- 8.Oyo State [Internet]. Oyo State Water Corporation launches urban water supply. Oyo State Press/News 6 November 2012. Available from: http://www.oyostate.gov.ng/oyo-state-water-corporation-launches-urban-water-supply [accessed 15 April 2013].
- 9.African Development Bank Group [Internet]. Nigeria: project completion report, Ibadan Water Supply II Project. Abidjan: ADBG, Infrastructure Department, Central and West Region; 2004. Available from: http://www.afdb.org/en/documents/project-operations/projectprogramme-completion-reports/2/http://[accessed 17 May 2013]. [Google Scholar]
- 10.Thompson T, Fawell J, Kunikane S, Jackson D, Appleyard S, Callen P et al. Chemical safety of drinking-water: assessing priorities for risk management Geneva: World Health Organization; 2007. Available from: http://whqlibdoc.who.int/publications/2007/9789241546768_eng.pdf [accessed 15 April 2013]. [Google Scholar]
- 11.California Department of Public Health. Evaluation of potential exposure to contaminants in private well water: Cloverdale, Sonoma County, California. Atlanta: United States Department of Health and Human Services, Agency for Toxic Substances and Disease Registry; 2009. Available from: http://www.ehib.org/projects/PrivateWellCloverdaleHC_121009.pdf [accessed 15 April 2013].
- 12.Site remediation and waste management program, New Jersey Department of Environmental Protection.Development of site-specific impact to ground water soil remediation standards using the soil-water partition equation. Trenton: New Jersey Department of Environmental Protection; 2008. Available from: http://www.nj.gov/dep/srp/guidance/rs/partition_equation.pdf [accessed 15 April 2031].
- 13.Risk assessment guidance for Superfund. Volume 1. Human health evaluation manual (Part A). Interim final Washington: United States Environmental Protection Agency; 1989 (EPA/540/1−89/002). Available from: http://www.epa.gov/oswer/riskassessment/ragsa/index.htmhttp://[accessed 15 April 2013].
- 14.Risk assessment guidance for Superfund. Volume I: human health evaluation manual (Part E: supplemental guidance for dermal risk assessment). Final. Washington: United States Environmental Protection Agency; 2004 (EPA/540/99/005). Available from: http://www.epa.gov/oswer/riskassessment/ragse/pdf/part_e_final_revision_10-03-07.pdf [accessed 21 May 2013].
- 15.Dermal exposure assessment: a summary of EPA approaches. Washington: Environmental Protection Agency; 2007 (EPA/600/R-07/040F). Available from: http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=183584 [accessed 15 April 2013].
- 16.WHO human health risk assessment toolkit: chemical hazards Geneva: World Health Organization; 2010. Available from: http://libdoc.who.int/publications/2010/9789241548076_eng.pdf [accessed 30 March 2013].
- 17.Adewuyi GO, Etchie AT, Etchie TO.Health risk assessment of exposure to metals in a Nigerian water supply. Hum Ecol Risk AssessEpub2012. Jun 6 [Google Scholar]
- 18.Ebersole KE, Dugas LR, Durazo-Arvizu RA, Adeyemo AA, Tayo BO, Omotade OO, et al. Energy expenditure and adiposity in Nigerian and African-American women. Obesity (Silver Spring) 2008;16:2148–54. doi: 10.1038/oby.2008.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pennington D, Crettaz P, Tauxe A, Rhomberg L, Brand K. Assessing human health response in life cycle assessment using ED10s and DALYs: Part 2 – noncancer effects. Risk Anal. 2002;22:947–63. doi: 10.1111/1539-6924.00263. [DOI] [PubMed] [Google Scholar]
- 20.Suwazono Y, Nogawa K, Uetani M, Miura K, Sakata K, Okayama A, et al. Application of hybrid approach for estimating the benchmark dose of urinary cadmium for adverse renal effects in the general population of Japan. J Appl Toxicol. 2011;31:89–93. doi: 10.1002/jat.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallagher CM, Kovach JS, Meliker JR. Urinary cadmium and osteoporosis in US women > or = 50 years of age: NHANES 1988-1994 and 1999-2004. Environ Health Perspect. 2008;116:1338–43. doi: 10.1289/ehp.11452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akesson A, Vahter M. Health effects of cadmium in Sweden. Stockholm: Karolinska Institutet; 2011. Available from: http://ki.se/content/1/c6/12/28/21/bilaga3.pdf [accessed 15 April 2013].
- 23.Engström A, Michaelsson K, Suwazono Y, Wolk A, Vahter M, Akesson A. Long-term cadmium exposure and the association with bone mineral density and fractures in a population-based study among women. J Bone Miner Res. 2011;26:486–95. doi: 10.1002/jbmr.224. [DOI] [PubMed] [Google Scholar]
- 24.Stopford W. Re: comments concerning your draft toxicology profile for cobalt Durham: Duke University Medical Center; 2002. Available from: http://duketox.mc.duke.edu/atsdrcobaltcomments1.pdf [accessed 15 April 2013].
- 25.Agency for Toxic Substances and Disease Registry. Toxicological profile for chromium. Atlanta: United States Department of Health and Human Services; 2012. Available from: http://www.atsdr.cdc.gov/toxprofiles/tp7.pdfhttp://[accessed 15 April 2013].
- 26.Wasserman GA, Liu X, Parvez F, Factor-Litvak P, Ahsan H, Levy D, et al. Arsenic and manganese exposure and children’s intellectual function. Neurotoxicology. 2011;32:450–7. doi: 10.1016/j.neuro.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agency for Toxic Substances and Disease Registry. Toxicological profile for manganese. Atlanta: United States Department of Health and Human Services; 2012. Available from: http://www.atsdr.cdc.gov/toxprofiles/tp151.pdf [accessed 15 April 2013].
- 28.United States Environmental Protection Agency [Internet]. Regional screening level (RSL) tapwater supporting table November 2012. Washington: EPA; 2012. Available from: http://www.epa.gov/reg3hwmd/risk/human/rb-concentration_table/Generic_Tables/pdf/restap_sl_table_bwrun_NOV2012.pdf [accessed 21 May 2013].
- 29.Fewtrell L, Kaufmann R, Prüss-Üstün A. Lead: assessing the environmental burden of disease at national and local levels Geneva: World Health Organization; 2003 (WHO Environmental Burden of Disease Series, No. 2). Available from: http://www.who.int/quantifying_ehimpacts/publications/en/leadebd2.pdf [accessed 15 April 2013]. [Google Scholar]
- 30.Centers for Disease Control and Prevention Blood lead levels in residents of homes with elevated lead in tap water – District of Columbia. MMWR Morb Mortal Wkly Rep. 2004;53:268–70. [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention Notice to readers. Examining the effect of previously missing blood lead surveillance data on results reported in MMWR. MMWR Morb Mortal Wkly Rep. 2010;59:592–3. [Google Scholar]
- 32.Snow ET. Scientific review of public health goal for hexavalent chromium in drinking water Launceston: University of Tasmania, School of Human Life Sciences; 2010. Available from: http://oehha.ca.gov/water/phg/pdf/092010SnowReview.pdf [accessed 15 April 2013]. [Google Scholar]
- 33.Analysis of oral, esophageal and stomach cancer incidence near chromium-contaminated sites in Jersey City Trenton: New Jersey Department of Health and Senior Services and New Jersey Department of Environmental Protection; 2010. Available from: http://www.state.nj.us/health/eoh/cehsweb/documents/hudson_co_chromium_hc.pdf [accessed 15 April 2013].
- 34.Crettaz P, Pennington D, Rhomberg L, Brand K, Jolliet O. Assessing human health response in life cycle assessment using ED10s and DALYs: Part 1 – cancer effects. Risk Anal. 2002;22:931–46. doi: 10.1111/1539-6924.00262. [DOI] [PubMed] [Google Scholar]
- 35.Murray C, Lopez A. The global burden of disease: a comprehensive assessment of mortality and disability from disease, injuries, and risk factors in 1990 and projected to 2020 Cambridge: Harvard School of Public Health; 1996 (Global Burden of Disease and Injury Series, vols. I & II). [Google Scholar]
- 36.World Health Organization [Internet]. Nigeria: health profile Geneva: WHO; 2012. Available from: http://www.who.int/gho/countries/nga.pdf [accessed 15 April 2013].
- 37.Machdar E, van der Steen NP, Raschid-Sally L, Lens PNL. Application of quantitative microbial risk assessment to analyze the public health risk from poor drinking water quality in a low income area in Accra, Ghana. Sci Total Environ. 2013;449:134–42. doi: 10.1016/j.scitotenv.2013.01.048. [DOI] [PubMed] [Google Scholar]
- 38.Adhoum N, Monser L, Bellakhal N, Belgaied J-E. Treatment of electroplating wastewater containing Cu2+, Zn2+ and Cr(VI) by electrocoagulation. J Hazard Mater. 2004;112:207–13. doi: 10.1016/j.jhazmat.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 39.Orescanin V, Kollar R, Nad K. The application of the ozonation/electrocoagulation treatment process of the boat pressure washing wastewater. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2011;46:1338–45. doi: 10.1080/10934529.2011.606423. [DOI] [PubMed] [Google Scholar]
- 40.Yadav AK, Singh L, Mohanty A, Satya S, Sreekrishnan TR. Removal of various pollutants from wastewater by electrocoagulation using iron and aluminium electrode. Desalination Water Treat. 2012;46:352–8. doi: 10.1080/19443994.2012.677560. [DOI] [Google Scholar]
- 41.Barrera-Díaz CE, Lugo-Lugo V, Bilyeu B. A review of chemical, electrochemical and biological methods for aqueous Cr(VI) reduction. J Hazard Mater. 2012;223-224:1–12. doi: 10.1016/j.jhazmat.2012.04.054. [DOI] [PubMed] [Google Scholar]