Abstract
Blood pressure control and prevention of hypertension can be achieved by both pharmacological and lifestyle interventions; one important lifestyle intervention is physical activity. Participation in regular physical activity can modestly lower blood pressure by reducing total peripheral resistance; it can also reduce the risk of developing hypertension and improve morbidity and mortality outcomes. Therefore, physical activity is a recommended intervention for the majority of hypertensive or prehypertensive patients. The precise level of physical activity required to lower blood pressure is unknown; however, in the UK, national minimum physical activity guidelines would seem appropriate for most hypertensives. Current patient physical activity levels can be assessed easily using retrospective recall questionnaires; preparticipation screening and exercise modifications for high-risk patients may reduce the risk of adverse events during subsequent exercise; and identification of a patient's willingness to increase physical activity levels may help to tailor physical activity advice. Health professional counselling or advice on physical activity is currently the most effective researched intervention. Its success can be maximized by delivering physical activity advice and counselling multiple times using different health professionals in person or over the telephone and by offering additional written materials. While the most effective methods for increasing physical activity levels in patients are probably still unclear, physical activity is an advisable intervention for the majority of hypertensive patients.
Introduction
Hypertension is one of the most prevalent and significant cardiovascular disease (CVD) risk factors, with the risk of CVD death doubling with each 20 mmHg increase in systolic blood pressure.1 A propensity to develop essential hypertension with increasing age will be present in a large section of the population, although its development is not inevitable if appropriate lifestyle interventions are instituted. Treating hypertension reduces many associated health risks, often with a dose response; for example with only a small population reduction in systolic blood pressure (2 mmHg) a significant fall in the risk of coronary artery disease (7%) and stroke (10%) has been estimated.1 In the UK, lifestyle interventions are recommended by the National Institute of Clinical Excellence (NICE) for the majority of hypertensives, either in isolation or as an adjunct to drug therapy; one important lifestyle intervention is physical activity.2 As well as having a beneficial effect on blood pressure, regular physical activity has many other significant health benefits and is considered as important as a healthy diet and smoking cessation.3 However, the reductions in blood pressure observed due to physical activity interventions can be modest4 and the success of hypertension management using physical activity by direct physician intervention is equivocal. The aim of this review is to assess the effect of physical activity on blood pressure and to outline appropriate practical guidelines for physicians to use in the management of essential hypertension using physical activity.
Physical activity and blood pressure
Regular physical activity and high cardiovascular fitness in both normotensive and hypertensive individuals can reduce the risk of all-cause mortality (by up to 41% and 51%, respectively) and cardiovascular mortality (by up to 74% and 73%, respectively).5 Initiating regular physical activity can prevent the development of hypertension; observational epidemiological studies suggest a reduction in the risk of developing hypertension of up to 52% in those who exercise regularly and maintain their cardiovascular fitness.6
Dynamic endurance exercise initially causes a small drop in systolic blood pressure due to peripheral blood pooling;7 increased cardiac output follows, a rise typically causing up to 200 mmHg or more with vigorous exercise, the magnitude depending on the duration and intensity of the exercise,7 and can be more pronounced in hypertensives or those at risk of hypertension. The diastolic pressure response is variable, inasmuch as it may rise slightly, remain the same or fall.8 During sustained isometric exercise, both systolic and diastolic pressures increase due to occlusion of resistance vessels in contracting peripheral muscles. Following a single bout of exercise, there is a transient drop in systolic blood pressure (postexercise hypotension) of up to 14 mmHg.8 Postexercise hypotension may last for up to 22 hours depending on the frequency, duration, intensity and type of exercise performed. Shorter high-intensity bouts appear to have a greater postexercise hypotensive effect, particularly in prehypertensives, although longer exercise sessions of lower intensity may be more beneficial in achieving long-term reductions in blood pressure. Moderate resistance training elicits similar reductions in blood pressure.9
Prevention and management of essential hypertension with physical activity
NICE recommends that lifestyle modifications, including physical activity, be used as a first-line interventions to prevent hypertension and as continued adjuncts to drug therapy.2 Lifestyle modifications appear to confer only modest reductions in blood pressure (average systolic reduction, 3.1–6.9 mmHg; average diastolic reduction, 2.2–4.9 mmHg) (Table 1), although there are health benefits with even a relatively small (2 mmHg) drop in systolic blood pressure.1 Initiation of regular physical activity in hypertensives can lead to a sustained reduction in blood pressure by an average of 6.9 mmHg systolic (Table 1); reductions have been similar in resting and ambulatory measurement.10 This is slightly higher than the reduction of blood pressure in normotensives,4,10 and these effects on blood pressure appear to be independent of body mass or change in body mass.4 Individual responses to physical activity interventions vary considerably due to differences in adherence as well as factors such as sex and race;11 however, on average 31% of patients experience a drop of at least 10 mmHg in systolic blood pressure (Table 1).
Table 1.
Magnitude of the reduction in blood pressure in hypertensives following different lifestyle interventions
| Intervention | Details | Reduction in resting BP (mmHg) | Proportion of patients reporting a ≥10 mmHg fall in SBP13 |
|---|---|---|---|
| Physical activity (endurance)10 | Average: 40 minutes per session, 3 × per week at 65% heart rate reserve (>13 MET-hours per week) | SBP: 6.9DBP: 4.9 | 31% |
| Physical activity (resistance)9 | Average: two sets of 10 exercises with 8–25 reps (61% 1 rm). 2–3 days per week for 16.1 weeks | SBP: 3.1 (NS)DBP: 3.1 | Unknown |
| Diet13 | Variable interventions including weight reduction and reduced saturated fats | SBP: 6.0DBP: 4.8 | 40% |
| Relaxation strategies13 | Variable interventions including: stress management, education and physical techniques | SBP: 3.7DBP: 3.5 | 33% |
| Reduction in alcohol consumption13 | Regular advice on restricting alcohol consumption | SBP: 3.7DBP: 3.2 | 30% |
| Reduction in Na+ intake13 | Advised to restrict intake to: 70–100 mmol/day (4.2–6.0 g of salt) | SBP: 3.4DBP: 2.2 | 23% |
| Multiple lifestyle changes13 | Including diet and exercise | SBP: 5.5DBP: 4.5 | 26% |
BP, blood pressure; DBP, diastolic blood pressure; NS, not significant; SBP, systolic blood pressure
Physiological mechanisms underlying blood pressure reduction following physical activity
A reduction in total peripheral vascular resistance (of the order of 7%) explains postexercise hypotension and the chronic reductions in blood pressure observed with regular exercise.12 They are thought to be due to the following:8,12
Reduced sympathetic nerve activity as well as reduced plasma catecholamines;
Increased endothelial responsiveness to vasodilators;
Reduced plasma renin activity;
Reduced insulin resistance.
Pharmacological compared with physical activity interventions
While the use of physical activity can be an important and effective tool in the management of hypertension, the magnitude of the reduction in blood pressure is potentially far greater with pharmacological interventions. Doses of drugs can be titrated and the addition of different drugs can increase the magnitude of the reduction in blood pressure compared with physical activity; indeed a dose–response relationship between physical activity and blood pressure reduction has yet to be established. The dropout rate in drug trials is also often much lower (typically <10% per year)13 than for exercise intervention trials where the number needed to treat using primary care physical activity promotion to achieve the minimum physical activity recommendations at 12 months is 12 patients.14 As a consequence, in order to achieve the magnitude of reduction in blood pressure required for many hypertensive patients, drug therapy is likely to be the most effective tool.
Reducing the risk of CVD and mortality is the ultimate aim of blood pressure control, and there is convincing randomized controlled trial data showing significant reductions in stroke risk in those taking antihypertensive medications.13 However, with the exception of thiazide diuretics and angiotensin-converting enzyme inhibitors, there is little evidence of any reduction in the risk of all-cause mortality and myocardial infarction in those taking antihypertensive drugs (Table 2). Comparisons of outcomes between drug studies and those investigating the effects of physical activity are difficult because there are no randomized controlled trials investigating the effect of regular physical activity on CVD and mortality. On the other hand, there is strong prospective cohort evidence that participating in regular physical activity can significantly reduce the risk of both all-cause and CVD mortality (Table 2), as well as the risk of many other non-communicable diseases, with very few adverse side-effects.
Table 2.
Mortality and morbidity risk reductions with long-term antihypertensive medication and physical activity
| Intervention | All-cause mortality | Cardiovascular mortality | Myocardial infarction |
|---|---|---|---|
| ACE-I28 * | 10% | 19% | NR |
| Thiazide13 * | 9% | NR | 22% |
| β-Blocker13* | 6% (NS) | NR | 8% (NS) |
| Ca2+ channel blockers29 * | −6% (NS) | NR | 29% (NS) |
| Regular physical activity (self-reported)30† | 29% | 30% | NR |
| Regular physical activity (fitness tests)30 † | 41% | 57% | NR |
ACE-I, angiotensin-converting enzyme inhibitors; NR, not reported;NS, not significant
*Randomized control trials
†Prospective cohort studies
The overall health benefits apparent in such studies provide persuasive evidence of the need for physicians to consider physical activity as a treatment intervention in underactive patients. Furthermore, the high prevalence of suboptimal activity in the population at large (between 65% and 95% of adults in the UK, depending on method of measurement)15 suggests that a large number of patients would benefit from physical activity interventions.
Guidance for physicians managing hypertension with physical activity
Hypertension is managed predominantly by primary care physicians, and the NICE hypertension guidelines indicate that clinicians should ‘ascertain people's diet and exercise patterns because a healthy diet and regular exercise can reduce blood pressure, offer appropriate guidance and written or audiovisual materials to promote lifestyle changes’ as a first-line treatment or drug adjuvant.13 It is also recommended that exercise is prescribed by physicians to underactive patients as a preventative health-care intervention;16 this constitutes the majority of patients. Therefore, it is reasonable to assume that in the majority of primary care consultations, physical activity should be discussed; available data suggest that such discussions occur in less than 30% of cases.17
The number of physicians using physical activity as an intervention for hypertension management is not known precisely but is likely to be low. This may be because the use of physical activity as a health-care tool in a consultation can be time consuming, and there may be a lack of understanding on the part of physicians about the most appropriate and safe exercise interventions for many individuals. While each patient should be managed by the physician as an individual, a number of steps can be proposed for physicians considering offering physical activity as a management intervention for hypertension:
Identify the minimum physical activity level required for health benefits;
Ascertain the patient's current level of physical activity;
Ascertain the patient's willingness to increase their physical activity levels;
Preparticipation screening.
Subsequently physical activity interventions can be implemented.
Minimum physical activity levels required for health benefits in hypertensive patients
Several exercise intervention schedules have been studied;9,10 however, consensus on precise minimum and optimal levels of physical activity deemed necessary to have a therapeutic effect on blood pressure is lacking and these are likely to vary from one individual to the next. Aerobic endurance exercise at low to moderate intensities (40–70% VO2 max)12 appears to be very effective in achieving a significant long-term reduction in blood pressure. Longer exercise durations (30–45 minutes per session) appear more effective at reducing blood pressure than shorter sessions,18 although accumulated bouts of shorter exercise may be even more effective. It is important that regular exercise be maintained because the training effect on blood pressure is lost after 10 weeks of detraining.19
The benefits of increasing physical activity levels extend beyond improvement in blood pressure. While physical activity regimens that have been shown to reduce blood pressure are variable, they are broadly similar to the UK Department of Health recommended minimum physical activity guidelines (for adults aged 16–65 years).20 These guidelines would, therefore, be a suitable goal for hypertensive or prehypertensive patients to achieve as a minimum to reduce their blood pressure:
Thirty minutes of moderate intensity aerobic exercise five days per week;
Twenty minutes of vigorous intensity aerobic exercise three days per week; or
A combination of both.
It is also recommended that physical activity is performed every day and that on two days per week strengthening exercises are performed. Recommendations for older individuals (>65 years old) include more flexibility, balance and strengthening exercises to reduce the risk of falls and increase independence. There is more detailed guidance for exercise beginners and conditioned individuals. These guidelines are the minimum physical activity levels required for significant health outcomes, although the dose–response relationship between physical activity and health risk reductions means that higher levels of physical activity and improved fitness result in better health outcomes. However, a dose–response relationship between physical activity and fall in blood pressure has not been established.
Ascertaining a patient's current level of physical activity
Before any physical activity intervention is considered, it is important to accurately assess the current physical activity status of the patient, including occupational tasks, household chores and exercise. Furthermore, the total volume of physical activity performed is a function of the intensity, duration and frequency of activity, making an accurate assessment difficult. Therefore, a balance between accuracy and practicalities of assessment is required. Physical activity assessment methods available include:
Cardiovascular fitness measurement: The most important determinant of cardiovascular fitness is physical activity, and measurement of the former is more objective than other tools. It is not commonly done in clinical practice due to cost, lack of universal use and absence of ‘normal’ values. However, it may have value as a motivational tool to monitor changes, and may also help identify normotensive individuals who have an exaggerated blood pressure response to exercise and are at greater risk of developing hypertension in the future, thereby allowing pre-emptive interventions.
Prospective measurements of physical activity: These include the use of accelerometers, pedometers and diary recordings. These objective measures are often limited in what physical activity they can record. For example, pedometers would not accurately measure many forms of physical activity such as gardening or swimming. Their use is becoming more widespread in clinical practice, but their effectiveness has yet to be confirmed.16
Retrospective self-reported physical activity questionnaires: These are less reliable and are limited by patient recall bias and overestimation. However, they are by far the most commonly used tools for assessing physical activity in clinical practice due to their simplicity and reasonable level of accuracy. They can take less than 30 seconds to complete preconsultation, and can quickly stratify patients between inactive and active.21
If the patient is already judged to be optimally active, then positive re-inforcement about the benefits of physical activity, regular physical activity assessment and the use of other lifestyle interventions or drugs to control blood pressure are recommended.
Ascertaining a patient's willingness to increase physical activity
There are a number of theoretical behavioural change models used to assess a patient's willingness to change his or her physical activity habits; the most widely used is the transtheoretical model, which outlines stages through which individuals progress when changing their physical activity behaviours:22
Precontemplation: no intention to increase physical activity and unaware of the problem;
Contemplation: aware of the problem, thinking about increasing physical activity but no commitment;
Preparation: intending to increase physical activity in the next month and may have had previous unsuccessful attempts to increase physical activity;
Action: overt behaviour modification (increased physical activity) has begun but lasted less than six months;
Maintenance: Patients have been active for more than six months without relapse.
Tailoring advice or intervention to a patient's stage in the transtheoretical model may maximize subsequent increases in physical activity.22 The most appropriate intervention for a patient in the precontemplation stage may be education about the benefits of exercise. Other lifestyle or pharmacological interventions may be more successful in the short term for these patients.
Those in the action and maintenance stages who meet the minimum physical activity guidelines should receive positive reinforcement and regular follow-up. Patients in the contemplation stage should receive further advice and encouragement about the benefits and risks of exercise in an attempt to move them to the preparation phase and beyond. Those in the action and maintenance stages that do not meet the physical activity guidelines, as well as those at the preparation stage, should undergo preparticipation screening before consideration for physical activity interventions. Potentially the most successful interventions will be in those patients who are beyond the precontemplation phase, although it is important that each patient is treated as an individual, and increasing physical activity levels may not be appropriate for all individuals.
Preparticipation screening
Regular vigorous exercise significantly decreases the risk of cardiovascular events and delays mortality.3 However, it may trigger a cardiac event in itself if there is underlying CVD, and clearly many hypertensive patients have CVD or significant other cardiovascular risk factors. While the risk of an adverse cardiac event is extremely low (1 in 15,000 to 1 in 50,000)23 and the benefits far outweigh the risks in general, it would appear prudent for physicians to screen individuals to reduce the risk of an adverse event. Patients can be stratified according to risk (Table 3). It must be recognized that this is risk mitigation not removal, and all patients should be informed of the possible risks and benefits of taking part in physical activity.
Table 3.
Preparticipation stratification of patients when managing hypertension with physical activity24
| Medical status | Preparticipation screening and physical activity advice | |
|---|---|---|
| 1 | Asymptomatic, low CVD risk and BP <140/90 mmHg | Routine evaluation and self-directed physical activity |
| 2 | Asymptomatic, low CVD risk and hypertensive ≥140/90 mmHg | Routine evaluation and begin with moderate intensity exercise (<60% heart rate reserve) |
| 3 | Asymptomatic, high CVD risk and hypertensive ≥140/90 mmHg | Symptomatic exercise testing prior to start (for example, ECG exercise test) |
| 4 | Symptomatic CVD | Medical supervision during exercise initially |
BP, blood pressure; ECG, electrocardiogram
An absolute contraindication to exercise is a resting blood pressure of ≥200/115. For those in the third and fourth medical status categories in Table 3 it is advisable to limit very dynamic exercise (>90% VO2 max) and vigorous strength training since left ventricular pressures can reach very high levels (>250 mmHg systolic).24
There are some antihypertensive drug interactions with exercise that physicians and patients should be aware of and able to manage, even though these drugs are not necessarily contraindicated in physical activity:25
Beta-blockers reduce maximum heart rate resulting in reduced exercise capacity;
Diuretics increase the risk of hypotension and hypokalaemia;
Calcium channel blockers increase the risk of hypotension postexercise.
Physical activity interventions
The best established intervention is health professional counselling or advice on physical activity,14,16 which may include a formal written exercise prescription.26 There is strong evidence that brief counselling (3–10 minutes) is effective at increasing patient physical activity levels, particularly among middle-aged and older individuals over the short (6–12 weeks) and medium terms (12–52 weeks). Significant increases in longer-term (>12 months) activity have also been observed.14 The majority of successful counselling or advice has been delivered on multiple occasions either in person or over the telephone using different health professionals and has included written materials.14 A number of other strategies intended to improve the effectiveness of any intervention have also been researched, including the use of behavioural rather than cognitive (motivational) strategies to encourage increased physical activity.27 However, many physical activity research interventions are still in their infancy, and research in specific populations including different ethnic groups and the very elderly is under-represented. Other interventions include exercise referrals, providing patients with a pedometer to monitor their own physical activity and the use of community-based programmes for walking and cycling,16 though there is insufficient evidence for their universal use.14,16
Direct evidence of improvements in cardiac risk factors (including blood pressure) following direct physical activity intervention by health-care professionals is limited; furthermore, a proportion of patients will not adhere to or respond to physical activity interventions. For some patients, other lifestyle and pharmacological interventions will be more appropriate.2
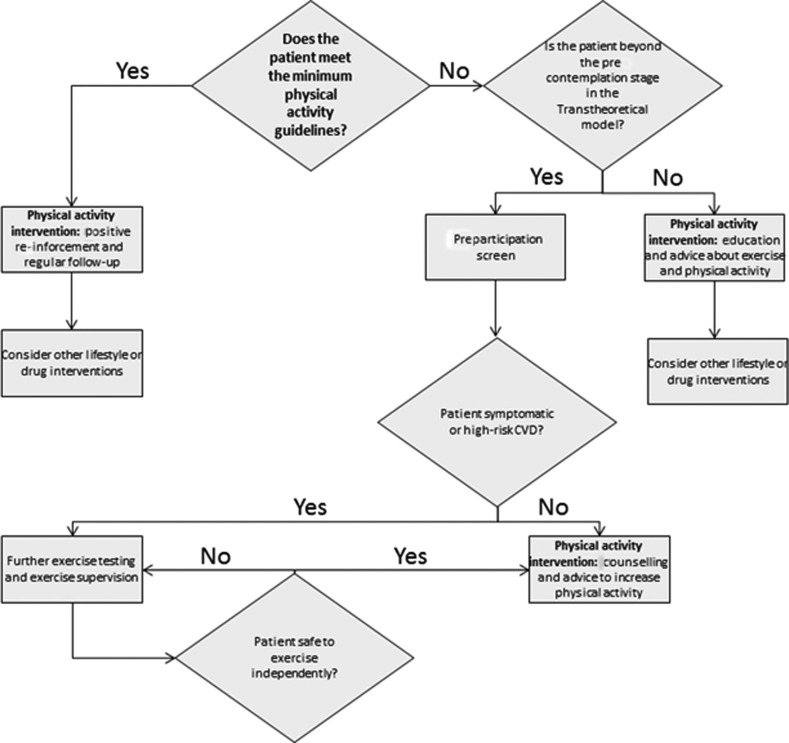
Conclusion
Preventing the development of hypertension and lowering blood pressure in the established hypertensive are important goals, since these reduce risk of CVD and its associated morbidities and mortality. This can be achieved by pharmacological and lifestyle interventions, including physical activity. Regular physical activity reduces the risk of developing hypertension, can be effective in lowering blood pressure in the established hypertensive and has numerous other important health benefits independent of changes in blood pressure. Consequently, managing hypertension with physical activity is advised for the majority of patients, either as adjuvant therapy or in isolation depending on the blood pressure and the individual patient. Practical steps to aid the physician using physical activity as an intervention in the management of hypertension are outlined in Figure 1. Health professional counselling and advice on physical activity is the best established physical activity intervention. While the most effective methods for increasing physical activity levels in patients in general are still unclear, these are likely to differ from one patient to another and individual tailoring is likely to be more successful than a ‘one size fits all’ prescription. In the future, individualized physical activity interventions, coupled with personalized pharmacotherapies,31 are likely to produce optimal blood pressure outcomes.
Figure 1.
Guidance for the management of patients with hypertension (<200/115) using physical activity as an intervention
DECLARATIONS
Competing interests
None
Funding
None
Ethical approval
None
Guarantor
JB and AF
Contributorship
JB performed the literature review. AF and JB contributed to the writing of this article
Acknowledgements
None
References
- 1. Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13 [DOI] [PubMed] [Google Scholar]
- 2. National Institute for Health and Clinical Excellence (NICE) Hypertension. Clinical Management of Primary Hypertension in Adults. London: SAGE Publications, 2011. [Google Scholar]
- 3. Chief Medical Officer At Least Five a Week: Evidence on the Impact of Physical Activity and Its Relationship to Health Department of Health, 2004. See http://sportkeighley.com/documents/Information/five_a_week.pdf (last checked 18 July 2012)
- 4. Whelton SP, Chin A, Xin X, He J Effect of aerobic exercise on blood pressure. Ann Intern Med 2002;136:493–503 [DOI] [PubMed] [Google Scholar]
- 5. Evenson KR, Stevens J, Thomas R, Cai J Effect of cardiorespiratory fitness on mortality among hypertensive and normotensive women and men. Epidemiology 2004;15:565–72 [DOI] [PubMed] [Google Scholar]
- 6. Blair SN, Goodyear NN, Gibbons LW, Cooper KH Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA 1984;252:487–90 [PubMed] [Google Scholar]
- 7. MacDonald JR, MacDougall JD, Interisano SA, et al. Hypotension following mild bouts of resistance exercise and submaximal dynamic exercise. Eur J Appl Physiol Occup Physiol 1999;79:148–54 [DOI] [PubMed] [Google Scholar]
- 8. MacDonald JR Potential causes, mechanisms, and implications of post exercise hypotension. J Hum Hypertens 2002;16:225–36 [DOI] [PubMed] [Google Scholar]
- 9. Cornelissen VA, Fagard RH Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens 2005;23:251–9 [DOI] [PubMed] [Google Scholar]
- 10. Cornelissen VA, Fagard RH Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension 2005;46:667–75 [DOI] [PubMed] [Google Scholar]
- 11. Hagberg JM, Park JJ, Brown MD The role of exercise training in the treatment of hypertension: an update. Sports Med 2000;30:193–206 [DOI] [PubMed] [Google Scholar]
- 12. Fagard RH, Cornelissen VA Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil 2007;14:12–7 [DOI] [PubMed] [Google Scholar]
- 13. National Clinical Guidance Centre Hypertension The Clinical Management of Primary Hypertension in Adults London: SAGE Publications, 2011. See: http://www.nice.org.uk/nicemedia/live/13561/56007/56007.pdf (last checked 18 July 2012) [Google Scholar]
- 14. Orrow G, Kinmonth AL, Sanderson S, Sutton S Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ 2012;344:e1389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. NHS Information Centre for Health and Social Care Health Survey Report 2008. Vol 1: Physical Activity and Fitness See http://www.ic.nhs.uk/webfiles/publications/HSE/HSE08/Volume_1_Physical_activity_and_fitness_revised.pdf (last checked 18 July 2012)
- 16. National Institute for Health and Clinical Excellence Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling – Public Health Intervention Guidance no.2. London: SAGE Publications, 2006. [Google Scholar]
- 17. Barnes PM, Schoenborn CA Trends in Adults Receiving a Recommendation for Exercise or Other Physical Activity From a Physician or Other Health Professional. NCHS data brief, no 86. Hyattsville, MD: SAGE Publications, 2012. See http://www.cdc.gov/nchs/data/databriefs/db86.pdf (last checked 18 July 2012) [PubMed] [Google Scholar]
- 18. Guidry MA, Blanchard BE, Thompson PD, et al. The influence of short and long duration on the blood pressure response to an acute bout of dynamic exercise. Am Heart J 2006;151:1322, e5,–1322 e12 [DOI] [PubMed] [Google Scholar]
- 19. Elley R, Bagrie E, Arroll B Do snacks of exercise lower blood pressure? A randomised crossover trial. N Z Med J 2006;119:U1996 [PubMed] [Google Scholar]
- 20. Department of Health, Physical Activity, Health Improvement and Protection Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers. London: SAGE Publications, 2011. See http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_128210.pdf (last checked 18 July 2012) [Google Scholar]
- 21. Physical Activity Policy, Health Improvement Directorate The General Practice Physical Activity Questionnaire (GPPAQ). A Screening Tool to Assess Adult Physical Activity Levels, within Primary Care. London: SAGE Publications, 2009. See http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_112134.pdf (last checked 18 July 2012) [Google Scholar]
- 22. Spencer L, Adams TB, Malone S, Roy L, Yost E Applying the transtheoretical model to exercise: a systematic and comprehensive review of the literature. Health Promot Pract 2006;7:428–43 [DOI] [PubMed] [Google Scholar]
- 23. Corrado D, Drezner J, Basso C, Pelliccia A, Thiene G Strategies for the prevention of sudden cardiac death during sports. Eur J Cardiovasc Prev Rehabil 2011;18:197–208 [DOI] [PubMed] [Google Scholar]
- 24. American College of Sports Medicine In: Whaley MH, ed. ACSM's Guidelines for Exercise Testing and Prescription. 7th edn Philadelphia: SAGE Publications, 2006. [Google Scholar]
- 25. Professional Associations for Physical Activity (Sweden) Physical Activity in the Prevention and Treatment of Disease. Stockholm: SAGE Publications, 2010. See http://www.fhi.se/PageFiles/10682/Physical-Activity-Prevention-Treatment-Disease-Webb.pdf (last checked 18 July 2012) [Google Scholar]
- 26. Sørensen JB, Skovgaard T, Puggaard L Exercise on prescription in general practice: a systematic review. Scand J Prim Health Care 2006;24:69–74 [DOI] [PubMed] [Google Scholar]
- 27. Conn VS, Hafdahl AR, Mehr DR Interventions to increase physical activity among healthy adults: meta-analysis of outcomes. Am J Public Health 2011;101:751–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Turnbull F Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362:1527–35 [DOI] [PubMed] [Google Scholar]
- 29. Staessen J, Wang J, Thijs L, Celis H, Gasowski J, Fagard R Use of dihydropyridines for antihypertensive treatment in older patients: evidence from the systolic hypertension in Europe trial. J Clin Basic Cardiol 2000;1:15–21 [PubMed] [Google Scholar]
- 30. Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S, Willich SN Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 2008;15:239–46 [DOI] [PubMed] [Google Scholar]
- 31. Ross S, Anand SS, Joseph P, Paré G Promises and challenges of pharmacogenetics: an overview of study design, methodological and statistical issues. J R Soc Med Cardiovasc Dis 2012;1:1.10.1258/cvd.2012.012001 [DOI] [PMC free article] [PubMed] [Google Scholar]