Abstract
Hepatocellular carcinoma (HCC) rarely metastasizes to the extra ocular muscles (EOMs). We present a case of bilateral metastasis of HCC to the EOMs and focus on the magnetic resonance imaging (MRI) features. Orbital MRI revealed nodular enlargement of bilateral multiple EOMs, with isointensity on T1-weighted images and heterogeneous, intermediate-to-high signal intensity on T2-weighted images, and showed mild-to-significant heterogeneous contrast enhancement with gadolinium. Physicians should be aware of this rare cause of EOM enlargement, understand the radiologic characteristics of EOM metastasis, and thus make appropriate treatment strategy.
Keywords: Metastasis, extra ocular muscle, hepatocellular carcinoma, magnetic resonance imaging
Metastatic tumor accounts for 3–7% of orbital neoplasm and any part of the orbit may be involved (1). It is reported that the most common primary tumor are carcinoma of the breast and lung (1). Hepatocellular carcinoma (HCC) rarely metastasizes to the orbit, with few biopsy-proven cases reported in the English literature (2–10). Moreover, isolated metastasis to extra ocular muscles (EOMs) is considered relatively rare with limited availability of epidemiologic data. Here, we report a case of bilateral metastasis of HCC to the EOMs, with emphasis on the magnetic resonance imaging (MRI) features, and provide a review of the literature.
Case report
A 44-year-old man presenting with diplopia of three months' duration was admitted to our hospital in August 2011. A detailed history revealed that he had undergone partial resection for HCC in the S7 segment in March 2010.
Three months before his visit to us, he developed rapidly progressive proptosis and double vision. In addition, he reported a 7-kg weight loss within the past month. Ophthalmologic examination disclosed that his visual acuity was normal in both eyes with normal anterior and posterior segments. Motility examination of the right eye revealed severe limitation of adduction and depression, and moderate limitation of elevation and abduction. The left eye revealed severe limitation of adduction and abduction.
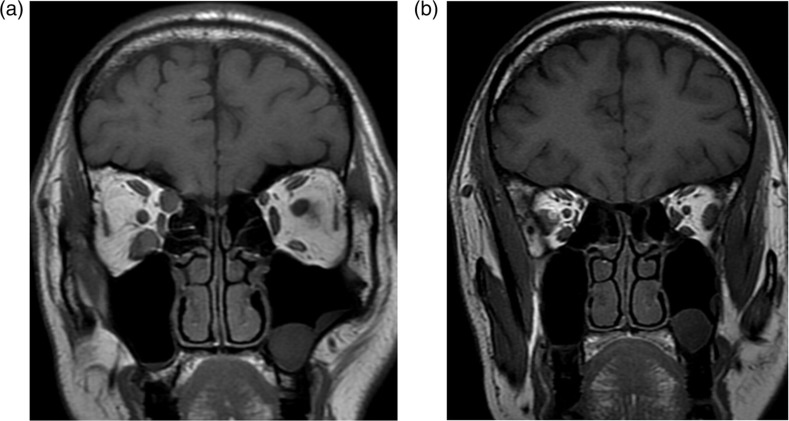
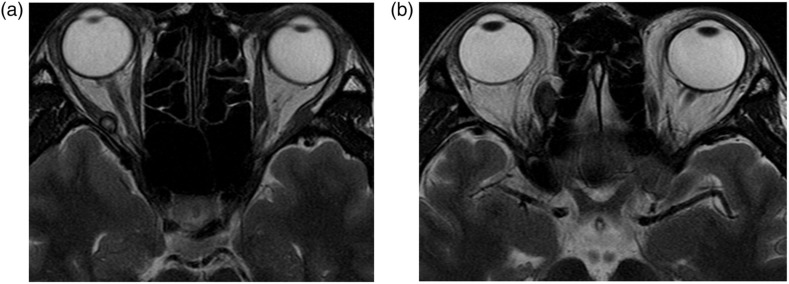
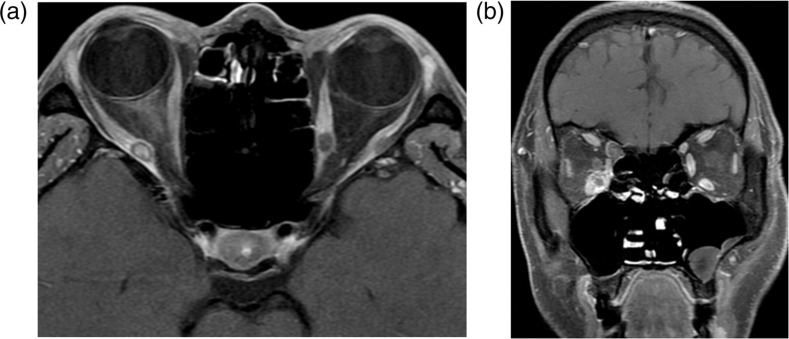
Orbital MRI showed nodular enlargement of the bilateral multiple EOMs, including the right superior oblique muscle, lateral rectus and inferior rectus, and the left lateral and medial rectus. The enlarged EOMs exhibited isointensity to cerebral white matter on T1-weighted images (Fig. 1) and heterogeneous intermediate-to-high signal intensity to cerebral white matter on T2-weighted images (Fig. 2). The muscle borders were well-defined, and there was mild-to-significant heterogeneous contrast enhancement with gadolinium (Fig. 3). The tendons were seen to be spared, and there was no evidence of orbital bone marrow involvement. Orbital echography revealed multiple enlarged EOMs with low internal reflectivity.
Fig. 1.
Coronal T1WI showing nodular enlargement of (a) the right superior oblique muscle and inferior rectus, as well as (b) the right lateral rectus, left lateral rectus, and medial rectus. The enlarged EOMs exhibited isointensity to cerebral white matter
Fig. 2.
(a, b) Axial T2WI showing heterogeneous intermediate-to-high signal intensity of the enlarged EOMs
Fig. 3.
Contrast-enhanced fat-suppressed (a) axial and (b) coronal T1WI showing mild-to-significant heterogeneous contrast enhancement of the enlarged EOMs
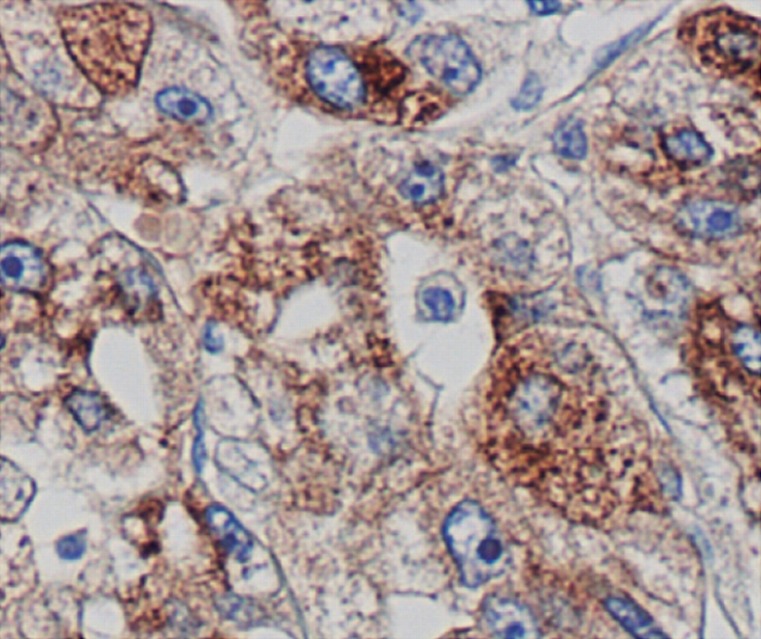
Biopsy of the right superior oblique muscle was performed by a lid crease incision. Microscopic examination revealed a diffuse infiltration of atypical polygonal cells, which contained hyperchromatic nuclei in the eosinophilic cytoplasm. Immunohistochemically, the tumor cells were positively stained for AFP (Fig. 4). These features were consistent with metastatic HCC with moderate differentiation. The patient received external beam radiation therapy to the orbit, which led to significant improvement of his bilateral proptosis and ocular motility.
Fig. 4.
The right superior oblique muscle tumor was positive by immunoperoxidase staining for AFP (×100)
Discussion
Metastatic HCC of the EOMs is rare. It occurs most commonly in the orbital bone when it involves the orbit. EOMs are the least common site, especially involvement of multiple muscles. To our knowledge, this is the first described case in the English-language radiologic literature of bilateral multiple EOMs enlargement from metastatic HCC.
The major presentations of metastatic HCC to the orbit are restriction of EOM motility and diplopia, which are also the presentations in our patient. These presentations are the result of the enlargement of the EOMs (2). Constant movement of the muscles or unfavorable chemical environment has been proposed as the cause for this rarity of metastasis to the EOMs (11), however, the mechanism remains unclear.
The orbital echography has been extensively used in orbital disease, but it is operator-dependent. MRI is the best tool to delineate EOM enlargement and signal intensity features. It has been reported that the most typical finding was a unilateral presentation of isolated rectus involvement (12). However, bilateral multiple EOMs were involved in our patient. Patrinely et al. (12) reported that nodular enlargement of the muscles was the most common appearance (50%) in EOM metastasis. The tendons were typically uninvolved, and muscle borders were sharp in 92% of cases (12). MR appearance of this tumor is non-specific, most metastasis show a signal intensity that is equal to muscle on T1-weighted imaging, and they characteristically present a signal intensity that is hyperintense to the brain parenchyma on T2-weighted imaging (13). In our case, the hyperintensity on T2-weighted images were heterogeneous, which may result from the necrosis and blood product in the parenchyma portion of the tumor.
The differential diagnosis for EOM metastasis includes thyroid-related orbitopathy and idiopathic orbital myositis, which are the common causes of EOM enlargement. Anti-thyroid antibodies are usually detectable on serology, and radiographic studies show fusiform enlargement of the muscles with spared tendons (14). Orbital myositis typically presents as isointense to muscle on T1-weighted imaging and isointense or minimally hyperintense to fat on T2-weighted imaging (14). Typically, an additional characteristic is that it presents slightly darker on T2-weighted images relative to their appearance on T1-weighted images, and the tendons are usually involved (15).
Usually, the metastasis is a late event in the progression of HCC, and therefore the prognosis after the assessment of these lesions is generally poor. Correct diagnosis for the EOM metastasis is important for planning the therapy. In recent years, chemotherapy and radiation has played an important role in treating extrahepatic metastasis.
In conclusion, we have described a case of bilateral multiple EOM metastasis from HCC. MR shows nodular enlargement of EOMs with isointensity on T1-weighted images and heterogeneous, intermediate-to-high signal intensity on T2-weighted images, and there was mild-to-significant heterogeneous contrast enhancement with gadolinium. Although the EOM metastasis is rare, physicians should understand its clinical and radiologic characteristics, and thus make appropriate treatment strategy.
Footnotes
Conflict of interest:None.
REFERENCES
- 1. Char DH, Miller T, Kroll S Orbital metastases: diagnosis and course. Br J Ophthalmol 1997;81:386–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tranfa F, Cennamo G, Rosa N et al. An unusual orbital lesion: hepatoma metastatic to the orbit. Ophthalmologica 1994;208:329–32 [DOI] [PubMed] [Google Scholar]
- 3. Schwab L, Doshi H, Shields JA et al. Hepatocellular carcinoma metastatic to the orbit in an African patient. Ophthalmic Surg 1994;25:105–6 [PubMed] [Google Scholar]
- 4. Loo KT, Tsui WM, Chung KH et al. Hepatocellular carcinoma metastasizing to the brain and orbit: report of three cases. Pathology 1994;26:119–22 [DOI] [PubMed] [Google Scholar]
- 5. Hosokawa C, Kawabe J, Okamura T et al. Usefulness of 99mTc-PMT SPECT and 18F-FDG PET in diagnosing orbital metastasis of hepatocellular carcinoma. Kaku Igaku 1994;31:1237–42 [PubMed] [Google Scholar]
- 6. Font RL, Maturi RK, Small RG et al. Hepatocellular carcinoma metastatic to the orbit. Arch Ophthalmol 1998;116:942–5 [DOI] [PubMed] [Google Scholar]
- 7. Scolyer RA, Painter DM, Harper CG et al. Hepatocellular carcinoma metastasizing to the orbit diagnosed by fine needle aspiration cytology. Pathology 1999;31:350–3 [DOI] [PubMed] [Google Scholar]
- 8. Kim IT, Na SC, Jung BY Hepatocellular carcinoma metastatic to the orbit. Korean J Ophthalmol 2000;14:97–102 [DOI] [PubMed] [Google Scholar]
- 9. Gupta R, Honavar SG, Vemuganti GK Orbital metastasis from hepatocellular carcinoma. Surv Ophthalmol 2005;50:485–9 [DOI] [PubMed] [Google Scholar]
- 10. Machado-Netto MC, Lacerda EC, Heinke T et al. Massive orbital metastasis of hepatocellular carcinoma. Clinics 2006;61: 359–62 [DOI] [PubMed] [Google Scholar]
- 11. Bloch RS, Gartner S The incidence of ocular metastatic carcinoma. Arch Ophthalmol 1971;85:673–5 [DOI] [PubMed] [Google Scholar]
- 12. Patrinely JR, Osborn AG, Anderson RL et al. Computed tomographic features of nonthyroid extraocular muscle enlargement. Ophthalmology 1989;96:1038–47 [DOI] [PubMed] [Google Scholar]
- 13. Char DH Clinical ocular oncology. 2nd edn Philadelphia, PA: SAGE Publications, 1997. [Google Scholar]
- 14. Bartalena L, Tanda AM Graves' Ophthalmopathy. N Engl J Med 2006;360:994–1001 [DOI] [PubMed] [Google Scholar]
- 15. Yan J, Wu Z, Li Y The differentiation of idiopathic inflammatory pseudotumor from lymphoid tumors of orbit: Analysis of 319 cases. Orbit 2004;23:245–54 [DOI] [PubMed] [Google Scholar]