Abstract
Urachal carcinoma is a rare neoplasm, which accounts for only 0.5–2% of bladder malignancies, and arises from a remnant of the fetal genitourinary tract. A 46-year-old woman presented with a history of pelvic pain and frequent daytime urination. Ultrasound (US), computed tomography (CT), and magnetic resonance (MR) demonstrated a supravesical heterogeneous mass with calcifications. The patient underwent a partial cystectomy with en-bloc resection of the mass and histopathological examination revealed the diagnosis of urachal adenocarcinoma. Urachal carcinomas are usually associated with poor prognosis and early diagnosis is fundamental. CT and MR are useful to correctly diagnose and preoperatively staging.
Keywords: Urinary, CT, MR imaging, ultrasound, bladder, neoplasms – primary
The urachus is an embryological remnant of urogenital sinus and allantois that usually involutes before birth and remains as the median umbilical ligament. Pathogenesis of urachal carcinoma is not fully understood. The prognosis is generally poor, because these tumors often are diagnosed late in the course of the disease and consequently the majority present with local invasion or metastatic disease. Although there are no specific imaging findings of urachal carcinomas, the most characteristic imaging feature is a midline supravesical mass with low-attenuation component and calcifications reflecting the mucin content. CT and MR also provide important information about the local extension of the tumor and distant metastases. Surgery is the mainstay of therapy. We report a case of primary adenocarcinoma of the urachus and describe and illustrate US, CT, and MR imaging findings.
Case report
A 46-year-old woman presented at our hospital with recurrent pelvic pain and frequent daytime urination of three months duration. Her medical history was unremarkable.
Despite suprapubic tenderness on palpation, physical examination was normal.
Complete blood count revealed marked increase in CEA to 1603 ng/mL (reference value <4 ng/mL) and slight increase in CA 125 to 46.5 U/mL (reference value <35 U/mL).
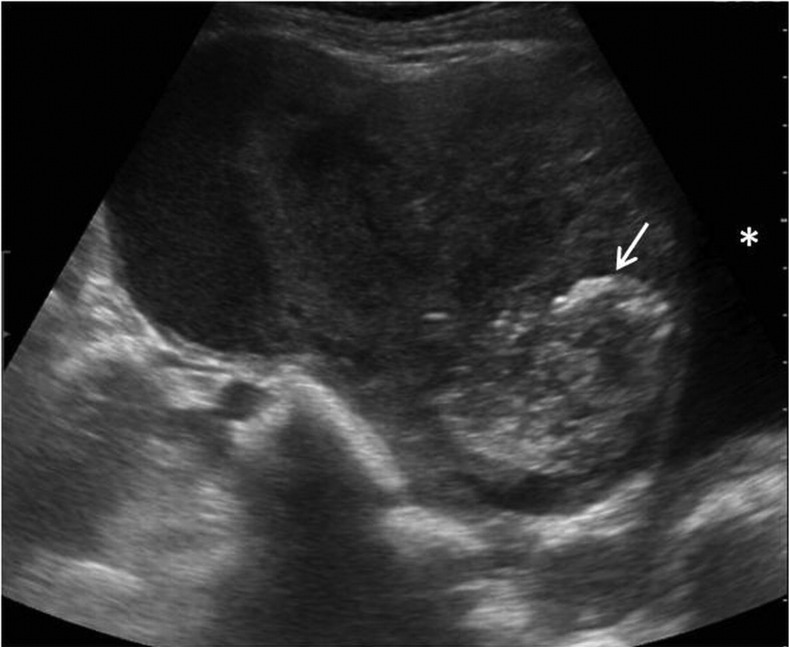
Pelvic ultrasound revealed a supravesical complex cystic mass with foci of increased echogenicity, suggestive of calcifications (Fig. 1).
Fig. 1.
Pelvic ultrasonography revealed a large complex cystic mass with calcifications (arrow) located superiorly to the bladder (*)
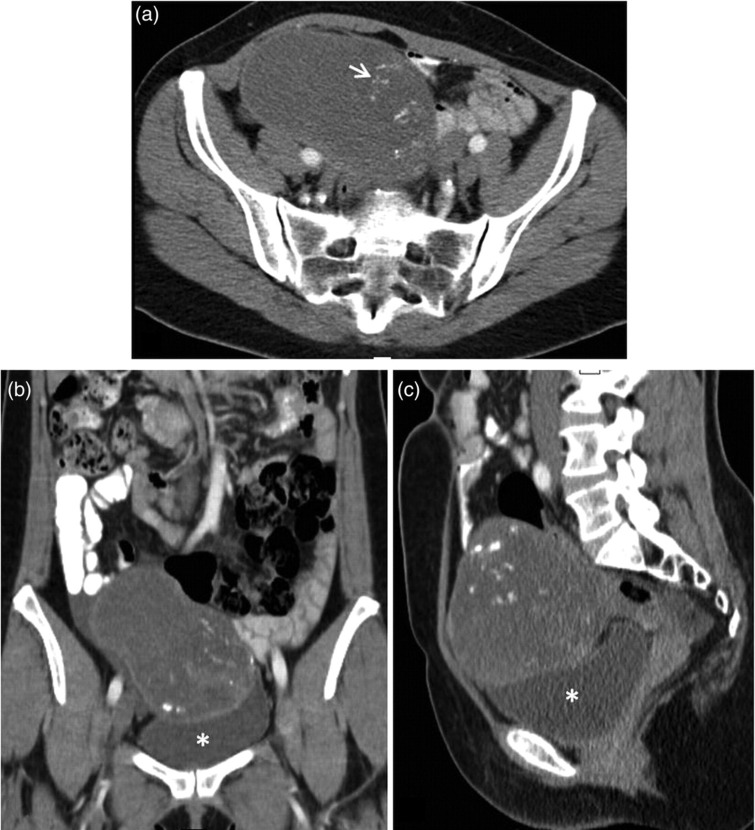
On contrast-enhanced CT it was seen a heterogeneous mass, of approximately 12.5 cm, extending through the anterosuperior wall of the bladder to the right flank. The lesion revealed low-attenuation and multiple dystrophic calcifications, suggestive of mucinous adenocarcioma. There was no evidence of local or distant metastases (Fig. 2).
Fig. 2.
On axial contrast-enhanced CT scan (a) was seen a large heterogeneous solid mass, with areas of low attenuation and dystrophic calcifications, suggestive of mucin content. Coronal (b) and sagittal (c) reformatted CT images, revealed the mass located superior to the bladder and extending through the right flank. The lesion contact the bladder but no focal thickening of the bladder wall was evident
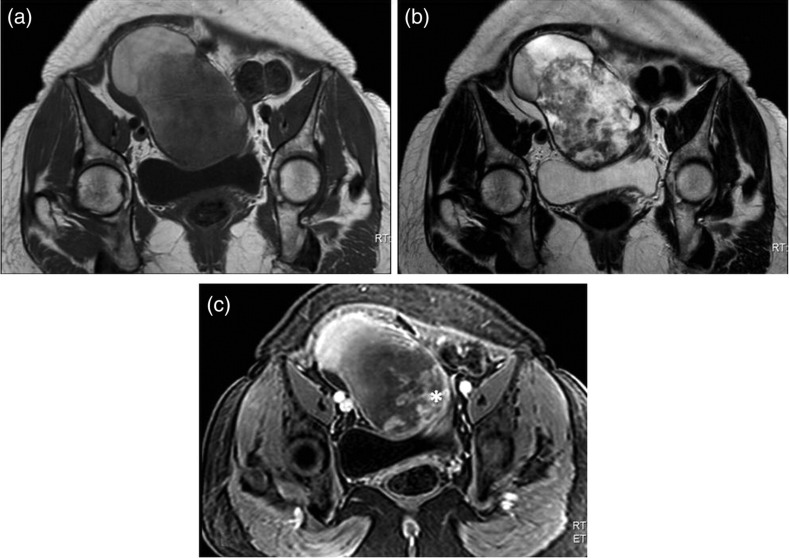
MR was performed to better characterize the lesion and revealed a large inhomogeneous mass in contact with the dome and superior wall of the bladder and occupying the right flank. The lesion showed high signal intensity on T2-weighted images and intermediate signal on T1-weighted images. After intravenous contrast administration the mass enhanced slightly peripherally (Fig. 3).
Fig. 3.
MR revealed an inhomogeneous mass with intermediate signal intensity on T1-weighted images (a) and high signal intensity on T2-weighted images (b). After the administration of gadolinium (c), the mass enhanced slightly peripherally and on solid vegetations (*)
Open laparotomy revealed that the lesion was strongly adhered to the wall of the bladder and partial cystectomy with en-bloc resection of the mass was performed. Histologic analysis revealed an urachal mucinous adenocarcinoma.
Discussion
The urachus is an embryologic remnant of the fetal genitourinary tract seen as a tubular structure extending in the midline between the dome of the bladder and the umbilicus that usually involutes before birth and remains in adults as the median umbilical ligament.
Primary adenocarcinomas of the urachus are extremely rare, representing only 0.5–2% of all bladder malignancies, although 34% of bladder adenocarcinomas are urachal in origin (1). It is believed to arise from malignant transformation of columnar or glandular metaplastic epithelium and mucin production is found in up to 75% of cases on histological analysis.
Urachal carcinomas mainly affect patients between 40 and 70 years old and have a male predilection (2). These tumors can be silent because of their extraperitoneal location, and consequently usually presents at an advanced stage, and often shows local invasion or metastases to the pelvic lymph nodes, lung, brain, liver, or bone. Hematuria, dysuria, abdominal pain, and umbilical discharge are the most frequent symptoms.
The diagnostic evaluation for urachal carcinoma should include a careful history and physical examination. A urine analysis with cytology may be helpful.
Although carcinoma of the urachus can occur in any site along the urachal tract, the most common locations are the dome of the bladder and the umbilicus.
US may demonstrate a supravesical complex cystic mass. CT or MR confirm the US findings and provide more information about local extent of the disease, pelvic lymph-node involvement, and systemic metastases. On CT urachal carcinoma is usually seen as a midline mass anterosuperior to the dome of the bladder that can be solid, cystic, or mixed. In 60% of cases low-attenuation components are seen, representing mucin content. Like other mucinous adenocarcinomas, urachal carcinomas may produce calcifications, which may occur in 50–70% of cases and are considered nearly pathognomonic for urachal adenocarcinoma (1, 3). On MR imaging a mass with increased signal intensity is usually seen on T2-weighted images because of the presence of mucin within the tumor (4).
The radiologic differential diagnosis includes benign urachal tumors that may mimic malignancy, like adenomas, fibromas, fibromyomas, and hamartomas, infected urachal remnants, and other malignant tumors like adenocarcinomas of non-urachal origin, transitional cell carcinomas, and metastases originating from primary lesions of the colon, prostate, or female genital tract (1, 5).
Primary treatment of localized disease includes wide local excision of the urachus, umbilicus, and surrounding soft tissue combined with partial or radical cystectomy and bilateral pelvic lymphadenectomy (6).
A cystoscopy is necessary to evaluate whether the carcinoma has penetrated the urothelium of the bladder and a transurethral biopsy should be performed if possible.
Footnotes
Conflict of interest:None.
REFERENCES
- 1. Yu JS, Kim KW, Lee HJ, et al. Urachal remnant diseases: spectrum of CT and US findings. Radiographics 2001;21:451–61 [DOI] [PubMed] [Google Scholar]
- 2. Ashley RA, Inman BA, Sebo TJ, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer 2006;107:712–20 [DOI] [PubMed] [Google Scholar]
- 3. Koster IM, Cleyndert P, Giard RW Best cases from the AFIP: urachal carcinoma. Radiographics 2009;29:939–42 [DOI] [PubMed] [Google Scholar]
- 4. Wong-You-Cheong JJ, Woodward PJ, et al. Neoplasms of the urinary bladder: radiologic-pathologic correlation. Radiographics 2006;26:553–80 [DOI] [PubMed] [Google Scholar]
- 5. Mengiardi B, Wiesner W, Stoffel F, et al. Case 44: adenocarcinoma of the urachus. Radiology 2002;222:744–7 [DOI] [PubMed] [Google Scholar]
- 6. Henly DR, Farrow GM, Zincke H Urachal cancer: role of conservative surgery. Urology 1993;42:635–9 [DOI] [PubMed] [Google Scholar]