Abstract
Bilateral paramedian thalamic stroke is a special ischemic pattern that results from occlusion of the artery of Percheron (AOP), a rare anatomic variant of the paramedian arteries. We report a case of bilateral thalamic infarctions, with a dramatic improvement after thrombolysis. DSA demonstrated recanalization of AOP with possible unreported variation.
Keywords: Angiography, MRI, thalamic stroke, thrombolysis
Bilateral paramedian thalamic stroke is a special ischemic pattern that results from the occlusion of the artery of Percheron (AOP), a rare anatomic variant of the paramedian arteries (1–4). Three possible variations involving the paramedian thalamic-mesencephalic arterial supply have been reported (5), but none of them described the contralateral posterior cerebral artery (PCA) supply. We report a case of bilateral thalamic infarctions with a DSA-approved contralateral PCA variation.
Case report
A 61-year-old woman was admitted to the emergency room with sudden onset of unconsciousness. CT showed no acute hemorrhage or infarctions. She received thrombolysis (rt-PA) within 6 h and Glasgow Coma Scale (GCS) score was back to 15 right after. However, she still complained of drowsiness and mild memory deficit. Diffusion-weighted imaging (DWI) the next day showed symmetrical paramedian thalamic high signal intensity (Fig. 1). The patient was then transferred to our hospital after 20 days. On admission she was somnolent and disoriented to time and place. Neurological examination showed vertical gaze palsy and upgoing plantar reflexes bilaterally.
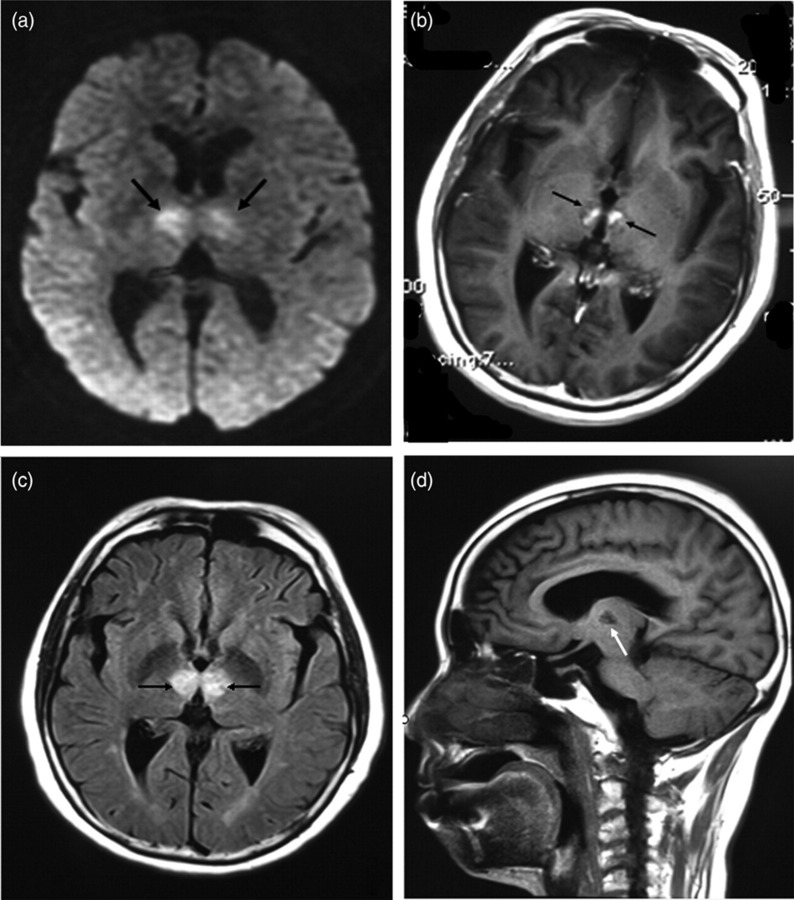
Fig. 1.
(a) Axial trace diffusion-weighted image obtained 24 h after the onset of symptoms showed bilateral thalamic areas of high signal intensity (black arrows) suggesting acute paramedian thalamic infarcts. (b) Axial T1-weighted post-contrast image obtained after 20 days showed contrast enhancement in the bilateral thalamic infarcts (black arrows). (c) Axial flair-weighted image showed rounded areas (black arrows) of increased signal intensity in the medial thalamus. (d) Lateral T1-weighted image showed bilateral paramedian thalamic without anterior thalamus and midbrain area of low signal intensity (white arrow)
She had no history of diabetes, hypertension, hyperlipidemia, or atrial fibrillation. Laboratory investigations were unremarkable. An MRI after three weeks showed symmetric enhanced signals in the paramedian thalamus (Fig. 1). Digital subtraction angiography (DSA) showed that the P1 segment of the right PCA was absent. The P2 segment was supplied by the right posterior communicating artery (PcomA). A stenotic AOP originated from the left P1 segment was also visualized (Fig. 2).
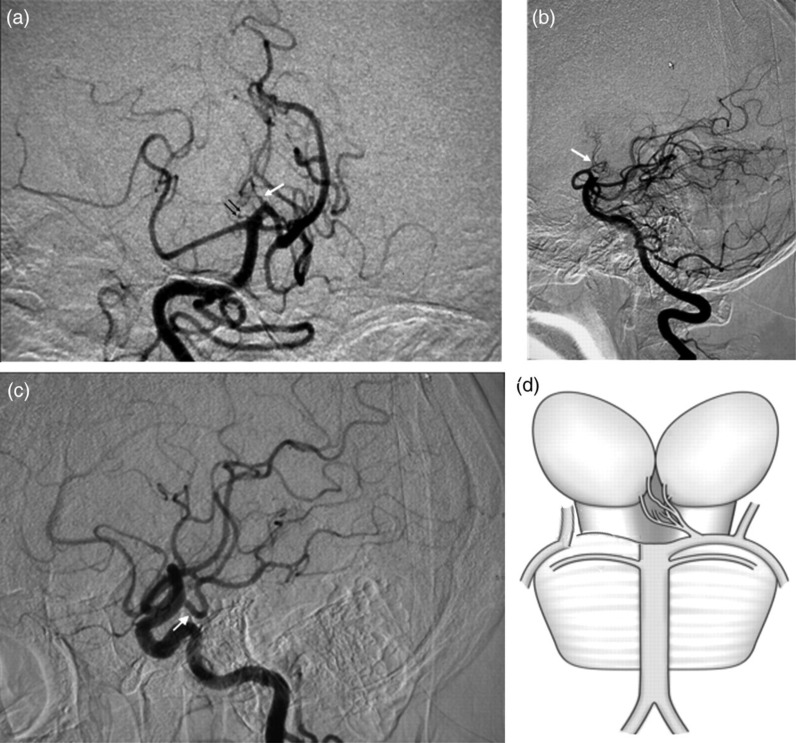
Fig. 2.
(a, b) DSA of the right vertebral injection, anteroposterior view (a) and lateral view (b) showed a stenotic AOP originating from the left P1 segment (white arrow). The P1 segment of the right PCA was absent (black double-arrow). (c) DSA of the right carotid artery injection showed the abnormally enlarged right PcomA could be the source of the right PCA (white arrow). (d) A schematic diagram represents a possible new variant of AOP. The P1 segment of the right PCA is absent while the AOP originates from the left
She was discharged 2 weeks later with full consciousness but severe cognitive impairment.
Discussion
Bilateral paramedian thalamic strokes are typically characterized by a triad of altered mental status, vertical gaze palsy, and memory impairment (2). This patient presented with the alteration of consciousness, followed by severe cognitive impairment and vertical gaze palsy after thrombolysis, which was in accordance with the triad of bilateral paramedian thalamic infarctions. An occluded AOP, although revascularized later, could explain all these symptoms. The thalamus is predominantly supplied by multiple small vessels originating from the PcomA and the P1 and P2 segments of the PCA. The AOP is an uncommon anatomic variant, in which a single dominant thalamoperforating artery supplies the bilateral medial thalamus with variable contribution to the rostral midbrain. However, it is very difficult to detect AOP by DSA after bilateral paramedian thalamus infarction. Lazzaro analyzed 37 patients with AOP infarction, among whom only one had a DSA-approved AOP due to possible self-recanalization (3). The patient in this case not only had DSA-approved AOP, but also severe AOP stenosis. DSA proved that the vessel was recanalized after thrombolysis, which was supported by the clinical improvement of the patient. Interestingly, the patient did not have one of the traditional vascular risk factors like hypertension or diabetes. The DSA did not demonstrate obvious stenosis of other vessels either. What could be the underlining etiology in this case? The probable explanation could be that both sides of the thalamus were supplied by: the AOP with approvable rCBF of approximately 80–90 mL/min/100 g, twice as much as the average cerebral rCBF (4). This could have created an internal hypertensive environment and made the AOP itself more vulnerable to arteriosclerosis with increasing age.
Percheron described three possible variations involving the paramedian thalamic-mesencephalic arterial supply (5). However, the P1 segment and PcomA were not completely evaluated in any of these types. In this case, we demonstrated an AOP variant together with the absence of the contralateral P1 segment. The absence seems more like an anatomic variant than acute occlusion because the right PcomA was abnormally enlarged, indicating that it could be the source of the right PCA. We believe that the presence of AOP combined with the absence of the contralateral P1 could be a new type of anatomic variant which has not been reported before.
In conclusion, we suggest that if the absence of the P1 segment is observed in patients with bilateral thalamic infarctions, the contralateral PCA might harbor an unusual AOP type. More angiographic evidence is needed to certify whether the existence of AOP has any relationship with the absence of the opposite P1 segment. Secondly, the arteriosclerotic thrombosis due hypertension might be the etiology of AOP infarctions. Thrombolysis after acute AOP infarctions seems highly suggested.
References
- 1. Bogousslavsky J, Regli F, Uske A Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology 1988;38:837–48 [DOI] [PubMed] [Google Scholar]
- 2. Schmahmann JD Vascular syndromes of the thalamus. Stroke 2003;34:2264–78 [DOI] [PubMed] [Google Scholar]
- 3. Lazzaro N.A. Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum. Am J Neuroradiol 2010;31:1283–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yonas H, Darby JM, Marks EC CBF measured by Xe -CT: approach to analysis and normal values. J Cereb Blood Flow Metab 1991;11:716–25 [DOI] [PubMed] [Google Scholar]
- 5. Percheron G The anatomy of the arterial supply of the human thalamus and its use for the interpretation of the thalamic vascular pathology. Z Neurol 1973;205:1–13 [DOI] [PubMed] [Google Scholar]