Abstract
The hydrocele of the canal of Nuck is quite a rare condition and results from the failure of obliteration of the distal portion of evaginated parietal peritoneum within the inguinal canal which forms a sac containing fluid. It generally presents with painless inguinal swelling. Ultrasonography and MRI is plays an important role to differentiate from the other conditions presenting with inguinal swelling. We present the imaging findings of a case in 5-year-old girl.
Keywords: Hydrocele, canal of Nuck, ultrasound, MRI
A small pouch of patent peritoneal fold extending along the round ligament into the inguinal canal through the inguinal ring during development is called the canal of Nuck in women. The canal of Nuck is homologous to processus vaginalis in men. During the first year of life it undergoes complete obliteration. Incomplete obliteration resulting in fluid trapped in the peritoneal remnant is called hydrocele of the canal of Nuck and failure of obliteration may result in inguinal hernia (1, 2). To our knowledge radiological findings in a canal of Nuck hydrocele are reported in very few cases.
Case report
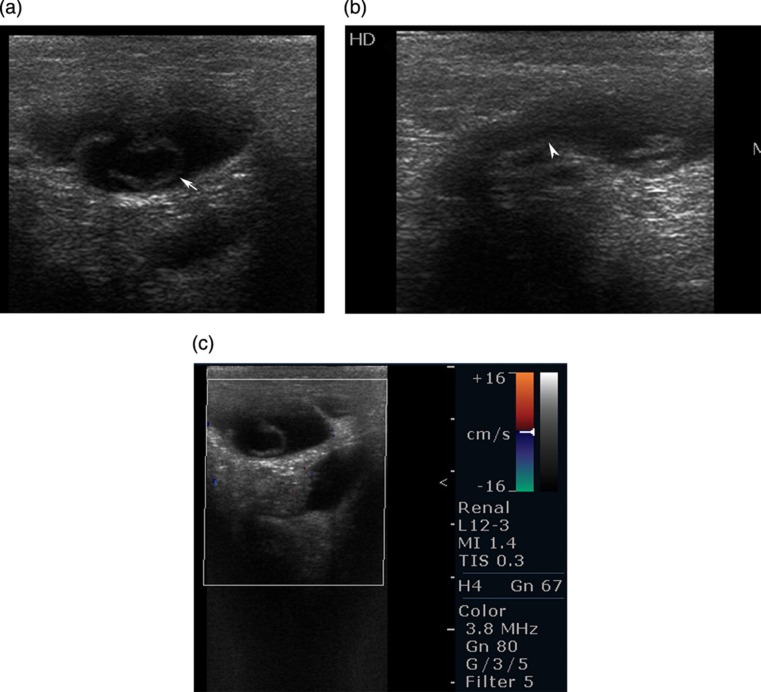
A 5-year-old girl presented with a palpable mass in the right inguinal region with occasional pain. Physical examination revealed smooth swelling in the right inguinal region which was tense but not tender. No thrill or bruit was seen over the swelling. Ultrasound examination of the right inguinal region was done using 7–12 MHz linear array transducer. There was well-defined sausage-shaped hypoechoic lesion with small internal septations (Fig. 1a) and the tail of the lesion was directed cranially and posteriorly. On color Doppler or power Doppler imaging no internal or peripheral vascularity was seen. On Valsalva maneuver the lesion did not change size or position.
Fig. 1.
Ultrasonography of the right inguinal area was performed with a 7–10 MHz linear array transducer. (a) Transverse view shows well-defined, sausage-shaped, hypoechoic lesion with small internal septations (arrow). (b) Longitudinal view shows sausage-shaped lesion with tail directed cranial and posteriorly (arrow head). (c) Color Doppler showing no internal or peripheral vascularity of the lesion
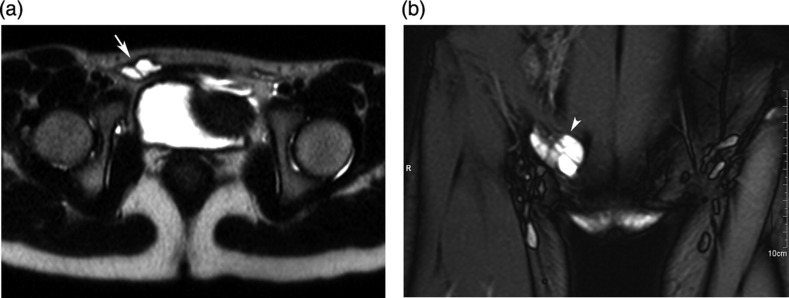
MRI was performed using 1.5-T system (Magnetom Avanto, Siemens, Erlangen, Germany) with a body coil. Axial and coronal T1 spin echo and T2 fast spin echo images of the inguinal region were obtained. Axial and coronal T2-weighted MR images showed a well-defined fluid intensity lesion in the right inguinal region with thin internal septa (Fig. 2). The lesion did not communicate with the peritoneal cavity. The signal intensity of the lesion was similar to the urinary bladder. The imaging features were consistent with hydrocele of canal of Nuck. The lesion was removed surgically and histopathology revealed the diagnosis of hydrocele of canal of Nuck.
Fig. 2.
MRI was performed with 1.5 Tesla superconducting magnet. T2 axial fast spin echo image (a) and coronal (b) fat-suppressed images showing well-defined, thin-walled, fluid intensity (hyperintense) lesion (arrow and arrow head) in the right inguinal canal with internal septa. No communication with the peritoneal cavity is seen
Discussion
The canal of Nuck was first described by the Dutch anatomist Anton Nuck in 1691 (3). The processus vaginalis within the inguinal canal in women is therefore called the canal of Nuck. The hydrocele of the canal of Nuck is a very rare condition and results from the failure of obliteration of the distal portion of the canal which forms a fluid-containing sac (4). The hydrocele of the canal of Nuck generally manifests as a painless swelling in the inguinal area and labium in adolescent age groups. Occasionally it may present with dull aching pain. The size of the lesion is usually small, averaging about 3 cm in length and about 0.3–0.5 cm in diameter (5). Herniation of the urinary bladder, ovary, and fallopian tubes into the canal of Nuck is rarely reported (3).
Ultrasound is the preferred investigation due to the superficiality of the lesion and is well-visualized with a high frequency linear array transducer. The lesion is typically seen as a well-defined hypoechoic or anechoic, sausage- or comma-shaped mass lying superficially and medial to the pubic bone in the inguinal canal with enhanced posterior through translucency (6). It may show cystic in appearance (7) or with septations within the lesion as seen in our case
To our knowledge, MRI findings in hydrocele of the canal of Nuck have been described in only a very few cases in the literature. It includes well-defined, thin-walled, sausage-shaped cystic lesion, which is hyperintense on T2 and hypointense on T1 in the inguinal area (8). Our case showed internal septations which have not been described in the literature. The wall of the hydrocele may show mild enhancement on contrast studies if the cyst is infected.
The differential diagnosis of inguinal masses in a young girl include Bartholin's cyst, lymphadenopathy, indirect inguinal hernia, and malignant and benign tumors. Complications of the hydrocele of the canal of Nuck are infection, hemorrhage, or a large cyst with retroperitoneal extension.
In conclusion, hydrocele of the canal of Nuck should be considered as a differential diagnosis in a girl presenting with swelling in the inguinal region. Ultrasound and MRI help to differentiate from other conditions presenting with swelling in the inguinal region. Typical findings on ultrasonography and MRI include well-defined, thin-walled, sausage-shaped, fluid-containing lesion in inguinal area with or without internal septations.
Footnotes
Conflict of interest:None.
References
- 1. Shadbolt CL, Heinze SB, Dietrich RB Imaging of groin masses: inguinal anatomy and pathologic conditions revisited. Radiographics 2001;21:S261–71 [DOI] [PubMed] [Google Scholar]
- 2. Anderson CC, Broadie TA, Mackey JE, et al. Hydrocele of the canal of Nuck: ultrasound appearance. Am Surg 1995;61:959–61 [PubMed] [Google Scholar]
- 3. Tubbs RS, Loukas M, Shoja MM, et al. Indirect inguinal hernia of the urinary bladder through a persistent canal of Nuck: case report. Hernia 2007;11:287–8 [DOI] [PubMed] [Google Scholar]
- 4. Patil SN, Bielamowicz K Female hydrocele of canal of nuck. J Ark Med Soc 2010;107:38–9 [PubMed] [Google Scholar]
- 5. Block RE Hydrocele of the canal of nuck. A report of five cases. Obstet Gynecol 1975;45:464–6 [PubMed] [Google Scholar]
- 6. Khanna PC, Ponsky T, Zagol B, et al. Sonographic appearance of canal of Nuck hydrocele. Pediatr Radiol 2007;37:603–6 [DOI] [PubMed] [Google Scholar]
- 7. Miklos JR, Karram MM, Silver E, et al. Ultrasound and hookwire needle placement for localization of a hydrocele of the canal of Nuck. Obstet Gynecol 1995;85:884–6 [DOI] [PubMed] [Google Scholar]
- 8. Park SJ, Lee HK, Hong HS, et al. Hydrocele of the canal of Nuck in a girl: ultrasound and MR appearance. Br J Radiol 2004;77:243–4 [DOI] [PubMed] [Google Scholar]