Abstract
Splenic lymphangioma is a rare, benign lesion of the spleen that is characterized microscopically by a proliferation of thin-walled vascular channels filled by proteinacious material. Based on microscopic features, three types of lymphangiomas are described as simple capillary, cavernous, and cystic; however, the distinction between these types is not uniformly accepted. The cystic type is the most common type and has well described imaging characteristics. However, little is known about the less common cavernous and capillary forms of lymphangioma. Herein, we present a case of a patient with two synchronous colon cancers that presented with a concomitant splenic mass that was initially suspected to be metastatic disease. Despite the use of multiple imaging modalities including computed tomography (CT), magnetic resonance imaging (MRI), nuclear imaging, and contrast-enhanced ultrasound, the final diagnosis of cavernous lymphangioma was made following core needle biopsy of the lesion. A thorough review of literature and this case now demonstrate the difficulty in differentiating atypical forms of splenic lymphangiomas from other benign lesions such as hemangioma.
Keywords: Spleen, benign, lymphangioma, imaging, contrast enhancement, colon cancer
Lymphangioma is an uncommon primary splenic tumor that originates from the non-hematolymphoid tissue of the spleen's red pulp (1–4). These tumors may present in a variety of fashions, from incidental lesions noted on abdominal imaging to rapidly growing lesions resulting in splenic rupture (5–7). Moreover, lymphangiomatosis may occur in children when there is mediastinal, axillary, and neck involvement by lymphangioma (4). In terms of imaging characteristics, the literature suggests that splenic lymphangiomas are generally cystic lesions that are hypoechoic or anechoic on ultrasound with possible septations (2, 8). On CT scan, they are well circumscribed, low attenuation lesions (3). On MRI, lymphangiomas are bright on T2 and dark on T1-weighted image (9). No significant enhancement is expected on either CT or MRI studies. In some cases, calcifications may be seen in the walls of cysts. Finally, bleeding may occur within the dilated lymphatic ducts, altering MR and CT appearance.
In this article, we present an unusual situation where a splenic lesion was found in a patient with two synchronous colon cancers. Initially, the lesion was suspected to be metastatic disease; however, it remained stable on follow-up studies, and a subsequent PET scan did not show abnormal FDG uptake in the spleen. Thus, a benign splenic mass was favored. The type of lesion was not identifiable despite the use of multiple imaging modalities including CT, nuclear-tagged RBC scan, MRI, and contrast-enhanced ultrasound. Final diagnosis was made by a core needle biopsy. A literature review in combination with the case we present demonstrate that the imaging characteristics of lymphangiomas could be atypical making it difficult to differentiate it from other benign lesions and the definite diagnosis may require tissue sampling.
Case report
The patient was a 67-year-old Caucasian man who was found to have two colorectal masses on colonoscopy; which were diagnosed as a well-differentiated adenocarcinoma and a moderate-to-poorly differentiated adenocarcinoma. His CEA level was 15.1 ng/mL at presentation (normal healthy smoker <5.5 ng/mL). CT scan of the abdomen demonstrated a 1.0-cm left adrenal nodule and a 6-cm heterogeneous, ill-defined mass in the spleen (Fig. 1). The attenuation of the splenic mass measured 42 Hounsfield units (HU) on the portal venous phase. This was unchanged on the 4 min delayed images. The left adrenal nodule was found to be adenoma on follow-up exams. Assuming metastatic disease, chemotherapy was initiated. The CEA level dropped to 0.9 ng/mL (within normal range) suggestive of a biochemical response to therapy. Meanwhile, a follow-up CT scan of abdomen and pelvis demonstrated stable size of the splenic lesions, suggestive of benign etiology.
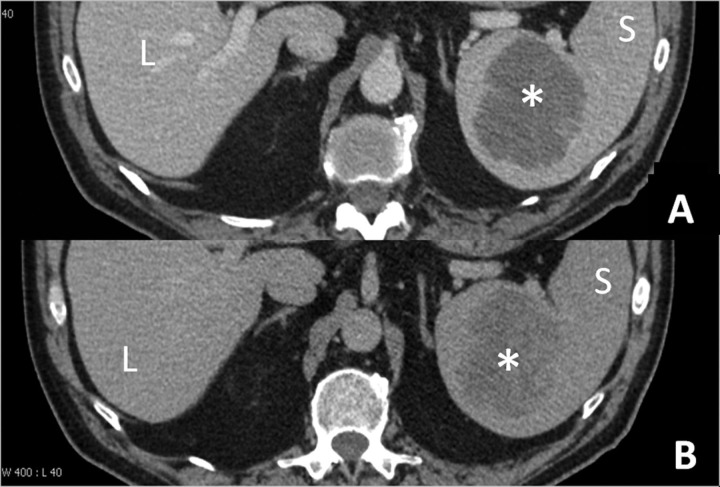
Fig. 1.
Initial CT scan of abdomen in the portal venous phase (a) and the 4 min delayed excretory phase (b). A 6-cm mass was seen in the spleen with density of 42 Hounsfield units (HU) on portal venous phase image that did not change on delayed images. A subsequent CT scan of abdomen was performed without contrast and demonstrated the density of lesion was 28 HU (image not shown) indicating that there was mild enhancement in the splenic lesion retrospectively. L, liver; S, spleen; *, splenic mass
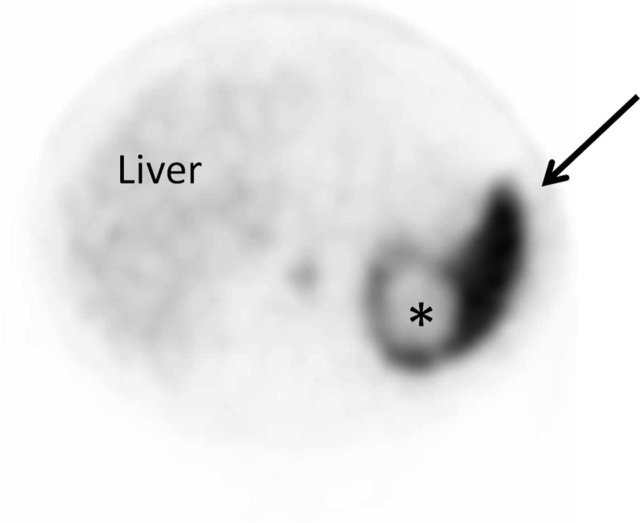
To confirm if the splenic lesion was benign, a PET scan was performed, which did not show FDG uptake in the splenic mass (Fig. 2).
Fig. 2.
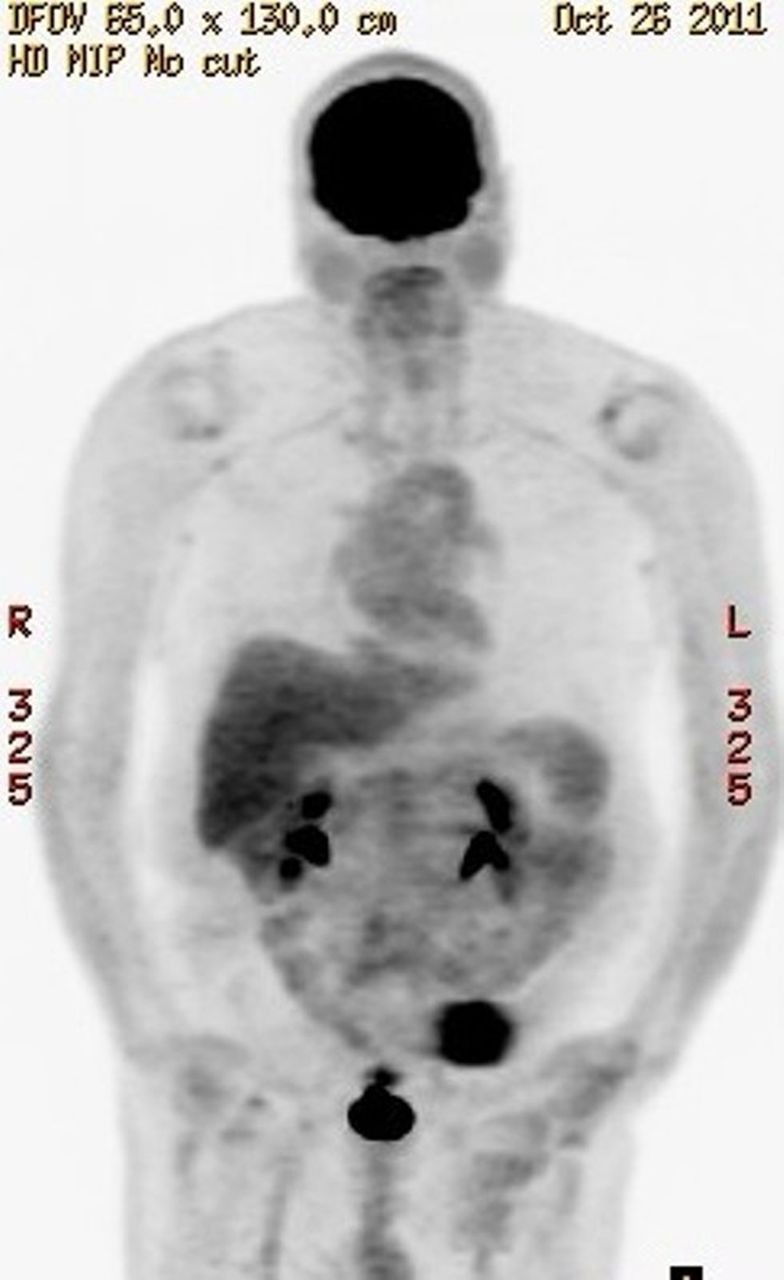
PET scan does not show any abnormal FDG uptake in the expected location of splenic lesion. Increased FDG is seen in renal collecting systems, bladder, and over the left lower quadrant of abdomen at the site of colostomy
Given that the most common benign lesion of the spleen is a hemangioma, a radiolabeled red blood cell (RBC) scan was performed to further characterize this lesion (Fig. 3). During the dynamic and delayed images, the RBC scan demonstrated a photopenic region in the spleen that corresponded to the mass. This made the diagnosis of hemangioma unlikely.
Fig. 3.
Axial SPECT image of the upper abdomen that was obtained 2 h after the intravenous injection of four mCi of Tc-99m labeled autologous RBCs. A photopenic region (*) is seen in the spleen (arrow) that corresponds to the splenic mass. Lack of RBC retention in the mass on delayed image excludes a hemangioma
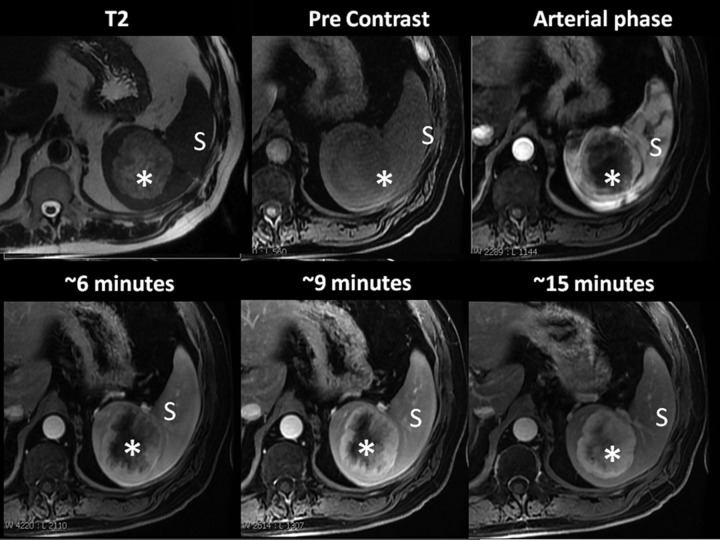
Because the tagged RBC scan did not confirm the diagnosis of hemangioma, an MRI of the abdomen was performed with and without Gadovist IV contrast (Fig. 4). The MRI showed a rounded, well-defined heterogeneously high T2 and low T1 signal lesion in the spleen with centripetal fill-in of contrast on delayed images. However, the lesion did not demonstrate homogeneous fill-in on the most delayed sequences. Nevertheless, MRI findings were reported to be suggestive of hemangioma or hemangioendothelioma. This was in some opposition to the tagged RBC scan. To further delineate the nature of the lesion, a contrast-enhanced ultrasound was recommended.
Fig. 4.
Axial contrast-enhanced MRI of splenic lesion (S, spleen; *, splenic mass). The lesion is well-defined and hyperintense on T2-weighted images and demonstrates centripetal fill-in of contrast on three-dimensional spoiled gradient echo pulse sequence with fat suppression (TE 1.96 ms, TR 4.36 ms) following the IV administration of 20 cc of Gadovist contrast agent. However, the most delayed images still do not show homogeneous filling. This pattern is commonly seen with hemangioma rather than lymphangioma
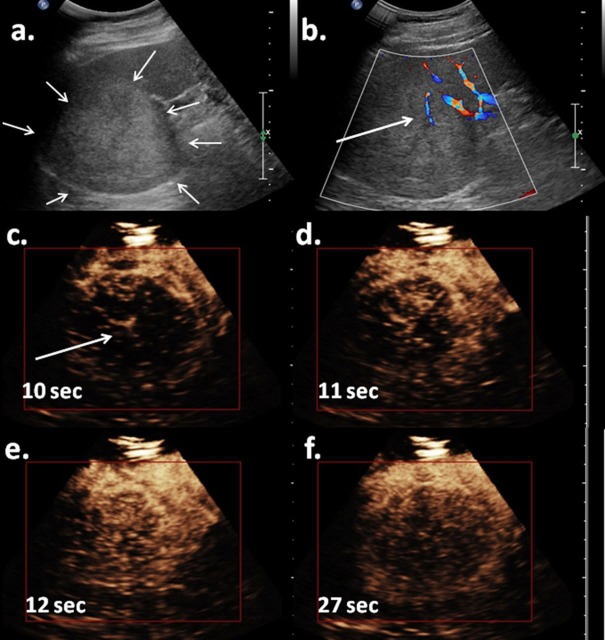
Doppler and gray scale ultrasound studies were performed followed by intravenous contrast injection of a total of four doses of 0.2 mL, Definity (Lantheus Medical Imaging, N Billerica, MA, USA). A Philips iU 22 ultrasound machine (Philips Medical Systems, Bothell, WA, USA) with C5-1 and X6-1 transducers were used for contrast study with contrast specific mode (Fig. 5). Pre-contrast images demonstrated a mildly hyperechoic mass in the spleen with peripheral vascular flow on Doppler images. Post-contrast ultrasound images immediately after contrast injection demonstrated straight vessels feeding the mass in the spleen. The lesion showed heterogeneous early enhancement and early wash-out. Again, the ultrasound findings were not typical for either a hemangioma or a lymphangioma.
Fig. 5.
(a) Gray-scale ultrasound showed a mildly hyperechoic mass in the spleen. (b) Color Doppler study showed some color signals inside of the lesion. (c, d) Immediately after intravenous injection of definity, the lesion showed internal straight vessels (arrow), and (e) heterogenous enhancement, to a slightly less degree than surrounding spleen, with early wash-out (f). The enhancement pattern is not typical for a lymphangioma and suggested benign lesions such as hamartoma or sclerosing antiomatoid nodular transformation (SANT)
Finally, a core biopsy of the splenic lesion was done in the operating room at the time of colectomy. At the time of operation, the patient was noted to have a large palpable mass centered in the superior pole of the spleen but adjacent to several splenic hilar vessels. Upon palpation of the splenic hilum, there was no evidence of regional lymphadenopathy. A suitable core needle biopsy window was identified on ultrasound in order to avoid vascular injury. Using an 18-gauge core needle, two passes were made in the splenic mass under ultrasound guidance without complication.
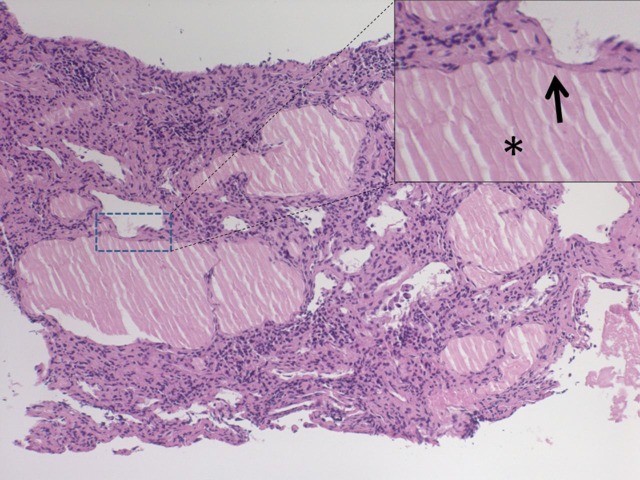
Histological sections showed the proliferation of variably sized thin-walled vascular channels filled with thin eosinophilic fluid and was reported as benign spleen with dilated lymphatics (Fig. 6).
Fig. 6.
H&E staining of the core biopsy of spleen lesion. There are dilated lymphatic channels with attenuated single layer lining (arrow) that are filed with proteinaceous materials (*). No RBC is seen within these dilated channels. This pattern is consistent with lymphangioma
Discussion
Lymphangiomas of the spleen are rare. Microscopically, lymphangiomas are composed of a proliferation of variably sized, thin-walled vascular channels lined by a single layer of attenuated endothelium and filled with eosinophilic, proteinaceous material. Lymphangiomas can be classified as capillary, cavernous, or cystic based upon the size of dilated channels (1); however, the distinction is not always clear and is not uniformly accepted among pathologists. Nevertheless, the most common type of solitary splenic lymphangioma appears as a cystic lesion and its correlated imaging characteristics are described as hypo- or anechoic lesions on ultrasound, low attenuation and non-enhancing masses on CT scan, and high T1 and low T1 signal intensity (3, 5, 8, 10, 11). Most radiology literature simply describes the imaging findings of splenic lymphangioma as mentioned above and does not talk about atypical imaging features. However, there are a small number of case reports in the literature of biopsy proven lymphangioma that demonstrated a very different imaging characteristics such as a solid mass instead of cystic, mildly increased echogenicity on ultrasound instead of being hypoechoic-anechoic, and with fill-in contrast enhancement on delayed images on CT and MRI (7, 12–16). These unusual imaging features of splenic lymphangioma include the MRI characteristics of a case of solitary splenic lymphangioma (12). In this report, a splenic lymphangioma was iso-intense on pre-contrast T1-weighted images with peripheral enhancement and central fill-in on delayed post-contrast images. They proposed that this pattern of enhancement for lymphangioma is due to stagnant contrast material in the rich stromal component of the tumor. This is very similar to what we noticed in our patient. Another case report by Bader et al. in 1998 described capillary and cavernous lymphangiomatosis of spleen to be slightly hyperechoic on ultrasound, hypoattenuating to the normal spleen on pre-contrast CT, and mildly enhancing on post-contrast CT images (14).
Contrast-enhanced ultrasound (CEUS) is a fairly new imaging modality, but has been used extensively for liver tumor characterization (17, 18). We found only one article on CEUS imaging of lymphangioma (13); which demonstrated heterogeneous, rapid, enhancement of the lesion with slow wash-out. Given the fact that ultrasound contrast agents remain intravascular, this pattern of enhancement is not expected in a typical lymphangioma that is composed of dilated lymphatic channels.
Similar to the few case reports presented above, the pattern of enhancement of the splenic lesion in our case was complex. For instance, CT demonstrated very mild enhancement, US demonstrated mild arterial enhancement with wash-out on delay, and MRI demonstrated heterogeneous progressive centripetal fill-in pattern. We hypothesized that this complex pattern of enhancement could be explained by combining multiple factors such as the presence of septation in the mass, the nature and size of the contrast agent, and the sensitivity of the imaging modality to detect contrast agent. For instance, contrast agents for ultrasound are microbubbles with mean diameter of 2–3 µm, and thus are pure intravascular agents; however, ultrasound imaging has a very high sensitivity and is able to detect microbubbles in the small septum within the mass and thus could show enhancement. The contrast agents for CT or MRI are much smaller molecular agents, and will leak into interstitial space causing enhancement.
Our data combined with a review of the literature demonstrate that splenic lymphangioma may present with a wide spectrum of imaging characteristics. Table 1 summarizes the distinct imaging features of typical (cystic) lymphangioma, hemangioma, and reported atypical lymphangiomas in the spleen.
Table 1.
Summary of overlapping imaging features of typical splenic lymphangioma, splenic hemangioma, and atypical splenic lymphangioma as reported in the literature. The atypical form of lymphangioma may mimic hemangioma on CT, MRI, and US. However, the combination of findings in different modalities could help to differentiate them from each other
| CT | Ultrasound | MRI enhancement | Tagged RBC scan | |
|---|---|---|---|---|
| Typical splenic lymphangioma | No enhancement | Hypo or anechoic | No enhancement | Photopenic |
| Splenic hemangioma | Progressive centripetal enhancement | Echogenic. Progressive enhancement | Progressive centripetal enhancement | Slow filling, follows blood pool after 2 h |
| Reported atypical splenic lymphangioma | Mild heterogeneous enhancement | Heterogeneous, arterial enhancement, wash-out | Progressive centripetal enhancement | Photopenic |
The presented case in this report is unique for the fact that the splenic lesion was incidentally found along with a left adrenal nodule in a case of synchronous colorectal cancers. In addition, the imaging characteristics were not compatible with the more common form of lymphangioma. Thus, multiple other imaging modalities and tissue sampling were needed to characterize this lesion. In these situations, the different appearances on RBC tagged nuclear scan and CEUS, can aid in narrowing the differential diagnosis.
ACKNOWLEDGEMENTS
Salary support for Mohammad Eghtedari was provided by NIH Grant T32EB005970.
Footnotes
Conflict of interest:None.
REFERENCES
- 1. Abbott RM, Levy AD, Aguilera NS, et al. From the archives of the AFIP: primary vascular neoplasms of the spleen: radiologic-pathologic correlation. Radiographics 2004;24:1137–63 [DOI] [PubMed] [Google Scholar]
- 2. Giovagnoni A, Giorgi C, Goteri G Tumours of the spleen. Cancer Imaging 2005;5:73–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levy AD, Cantisani V, Miettinen M Abdominal lymphangiomas: imaging features with pathologic correlation. Am J Roentgenol 2004;182:1485–91 [DOI] [PubMed] [Google Scholar]
- 4. Avigad S, Jaffe R, Frand M, et al. Lymphangiomatosis with splenic involvement. JAMA 1976;236:2315–7 [PubMed] [Google Scholar]
- 5. Solomou EG, Patriarheas GV, Mpadra FA, et al. Asymptomatic adult cystic lymphangioma of the spleen: case report and review of the literature. Magn Reson Imaging 2003;21:81–4 [DOI] [PubMed] [Google Scholar]
- 6. Patti R, Iannitto E, Di Vita G Splenic lymphangiomatosis showing rapid growth during lactation: a case report. World J Gastroenterol 2010;16:1155–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Seki H, Ueda T, Kasuya T, et al. Lymphangioma of the jejunum and mesentery presenting with acute abdomen in an adult. J Gastroenterol 1998;33:107–11 [DOI] [PubMed] [Google Scholar]
- 8. Bezzi M, Spinelli A, Pierleoni M, et al. Cystic lymphangioma of the spleen: US-CT-MRI correlation. Eur Radiol 2001;11:1187–90 [DOI] [PubMed] [Google Scholar]
- 9. Luna A, Ribes R, Caro P, et al. MRI of focal splenic lesions without and with dynamic gadolinium enhancement. Am J Roentgenol 2006;186:1533–47 [DOI] [PubMed] [Google Scholar]
- 10. Pistoia F, Markowitz SK Splenic lymphangiomatosis: CT diagnosis. Am J Roentgenol 1988;150:121–2 [DOI] [PubMed] [Google Scholar]
- 11. Kwon AH, Inui H, Tsuji K, et al. Laparoscopic splenectomy for a lymphangioma of the spleen: report of a case. Surg Today 2001;31:258–61 [DOI] [PubMed] [Google Scholar]
- 12. Chang WC, Liou CH, Kao HW, et al. Solitary lymphangioma of the spleen: dynamic MR findings with pathological correlation. Br J Radiol 2007;80:e4–6 [DOI] [PubMed] [Google Scholar]
- 13. Yu X, Yu J, Liang P, et al. Real-time contrast-enhanced ultrasound in diagnosing of focal spleen lesions. Eur J Radiol 2012;81:430–6 [DOI] [PubMed] [Google Scholar]
- 14. Bader TR, Ranner G, Klimpfinger M Case report: CT appearance of capillary and cavernous lymphangiomatosis of the spleen in an adult. Clin Radiol 1998;53:379–81 [DOI] [PubMed] [Google Scholar]
- 15. Hwang SS, Choi HJ, Park SY Cavernous mesenteric lymphangiomatosis mimicking metastasis in a patient with rectal cancer: a case report. World J Gastroenterol 2009;15:3947–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Takayama A, Nakashima O, Kobayashi K, et al. Splenic lymphangioma with papillary endothelial proliferation: a case report and review of the literature. Pathol Int 2003;53:483–8 [DOI] [PubMed] [Google Scholar]
- 17. Wilson SR, Jang HJ, Kim TK, et al. Diagnosis of focal liver masses on ultrasonography: comparison of unenhanced and contrast-enhanced scans. J Ultrasound Med 2007;26:775–87, quiz 88–90 [DOI] [PubMed] [Google Scholar]
- 18. Quaia E, Calliada F, Bertolotto M, et al. Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 2004;232:420–30 [DOI] [PubMed] [Google Scholar]