Abstract
Background and Aims: Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in children and adolescents. Obesity is a major risk factor for NAFLD; however, it has been shown that NAFLD is not rare in non-obese adults. The aim of this study was to determine the prevalence of NAFLD in obese and non-obese children and adolescents.
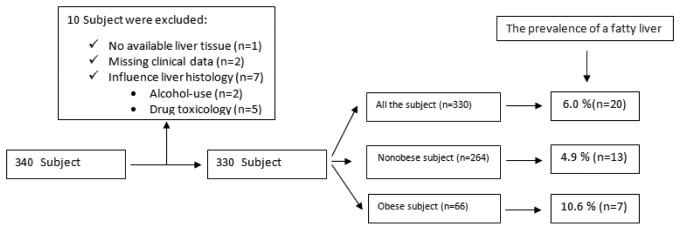
Methods: The medical records of 340 subjects (aged 2-20 years) in whom autopsy was performed were retrospectively reviewed. Of those, 10 subjects were excluded due to insufficient data. The remaining 330 subjects were included in the study, of whom 264 were normal weight and 66 were obese. All liver biopsy sections were evaluated by two pathologists in a blinded fashion.
Results: The prevalence of fatty liver was 6% among all the subjects and was higher in the overweight group than in the normal-weight group (10.6% vs 4.9%; p<0.001). The prevalence of NAFLD increased concomitant with age. There was no significant difference between sexes in cases with NAFLD. Simple steatosis was detected in 7 subjects. Steatohepatitis was determined as type 1 in 5 subjects, type 2 in 7 subjects, and as overlap in 1 subject.
Conclusions: This study demonstrated that NAFLD is an important public health problem not only in obese but also in non-obese children and adolescents. This suggests that whereas obesity may be a risk factor, other pathogenic factors may exist that could contribute to the NAFLD.
Keywords: fatty liver disease, obesity, children, adolescents, autopsy
Nonalcoholic fatty liver disease (NAFLD) describes a clinicopathologic condition that is characterized by lipid accumulation in excess of 5% of liver wet weight in patients with no history of excessive alcohol consumption1. It is probably the most common cause of liver disease in children and adolescents and can progress to cirrhosis and hepatocellular carcinoma1,2.
NAFLD cannot be correctly identified based on clinical features, biochemical parameters or imaging studies. Accurate diagnosis and staging of NAFLD requires a liver biopsy that cannot be used as a screening tool in population studies3. However, autopsy series are another means of estimating prevalence based on a histological diagnosis4.
The existing population-based prevalence studies suggest that NAFLD is a global problem. The prevalence of NAFLD in obese adolescents was between 10% and 25%, suggesting that obesity is a major risk factor for NAFLD5,6. However, to our knowledge, the prevalence of NAFLD in non-obese children and adolescents has not been reported.
We conducted this study to determine the prevalence of fatty liver disease by histology in an autopsy series of obese and non-obese children and adolescents.
Material and methods
Study Design and Cases:
We retrospectively studied the records of 340 children and adolescents aged 2 to 20 years in whom autopsy was performed by a medical examiner from 2006-2008. The minimum age accepted into the study was 2 years, which is the youngest reported age for biopsy-proven steatohepatitis4. Medical examiner records were reviewed for age, gender, weight, height, toxicology, and the mode and cause of death. Body mass index (BMI) was calculated according to the formula as weight (kg)/height (m)2. We defined obesity as BMI above the 95th percentile for age and sex based on established percentile curves for Turkish children7.
Exclusion criteria were missing clinical data or the absence of a liver slide for review and identification of factors that may influence liver histology (alcohol or drug use).
Liver Biopsy
Five-micrometer sections were cut from formalin-fixed paraffin-embedded tissue blocks of the liver. Slides stained with hematoxylin-eosin and trichrome were evaluated by two pathologists in a blinded fashion.
Steatosis was recorded as the percentage of hepatocytes containing macrovesicular fat or microvesicular fat. Fatty liver was defined as 5% of hepatocytes containing macrovesicular fat8. NAFLD was classified as simple steatosis, type 1 nonalcoholic steatohepatitis (NASH), characterized by steatosis with ballooning degeneration and lobular inflammation, with or without perisinusoidal fibrosis and without portal inflammation, or type 2 NASH, characterized by portal inflammation, with or without portal fibrosis, and no or minimal ballooning degeneration4. Macrovesicular and microvesicular steatosis, ballooning degeneration and perisinusoidal and pericellular fibrosis are shown in Figure 1-Figure 3, respectively. "Overlap" pattern was described with features common to both type 1 and 2 NASH patterns4 (Table 1).
Figure 1. Macrovesicular and microvesicular steatosis (H&E).
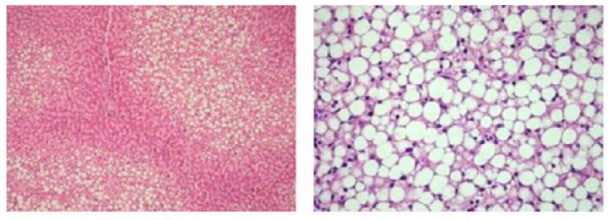
Figure 2. Ballooning degeneration (H&E).
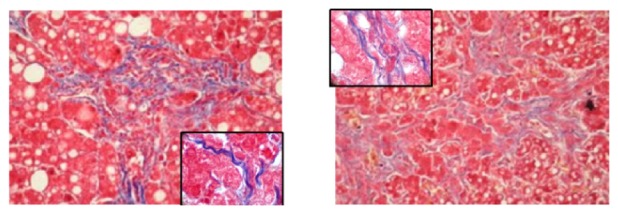
Figure 3. Perisinusoidal and pericellular fibrosis (trichrome) .
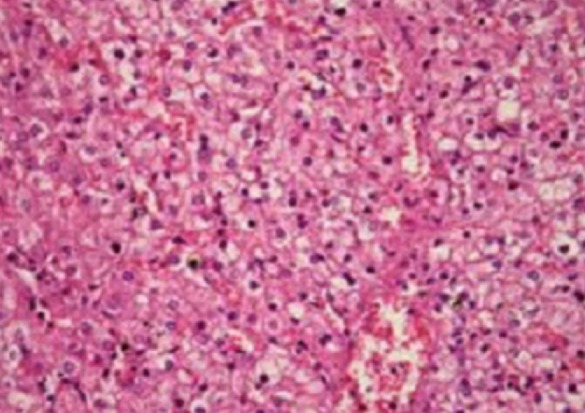
Table 1. Definition of Steatohepatitis Types.
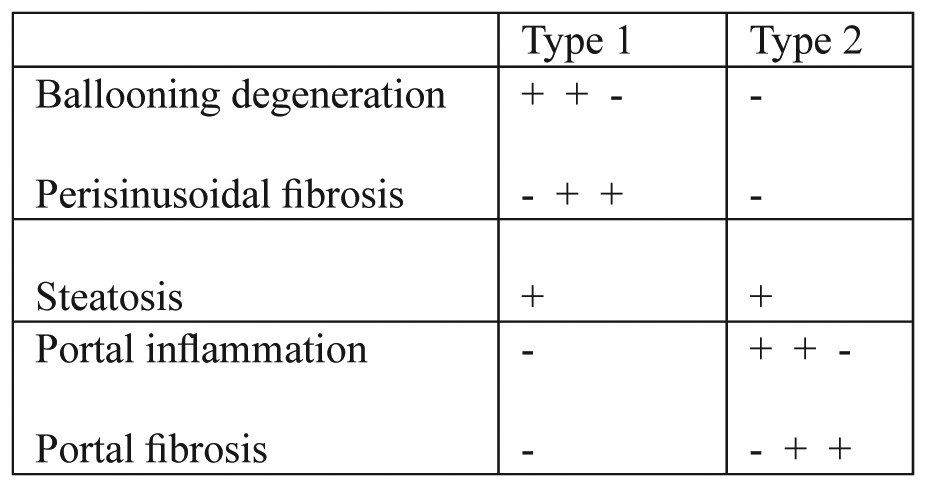
+ present, - absent.
Statistical analyses:
All the calculations were made using SPSS 13.0 for Windows (SPSS, Inc., Chicago, IL, USA). The difference between groups with and without NAFLD was compared using Mann-Whitney U test. The X2 test was used to compare the prevalence data. The results were expressed as median (range) or percentages. Values of p<0.05 were considered statistically significan.
Results
Autopsy was performed on 340 subjects (age range: 2-20 years) by the Ankara Forensic Group medical examiner. Of those, 10 subjects were excluded due to insufficient data. The remaining 330 subjects were included into the study, of whom 264 were normal weight and 66 obese. The prevalence of fatty liver was 6% among all the subjects and was higher in the overweight group than in the normal-weight group (10.6% vs 4.9%; p<0.001) (Figure 4).
Figure 4. Selection and distribution of cases and the prevalence of a fatty liver in the each group.
Fatty liver prevalence increased concomitant with age. While NAFLD was present in only 7 subjects aged 2 to 14 years, it was determined in 13 subjects aged 15 to 20 years. The minimum age was 9 years old in the obese-NAFLD group versus 2 years old in the normal weight-NAFLD group. In the obese group, there was no significant difference between sexes in cases with NAFLD, and those findings are given in Table 2.
Table 2. Clinical Characteristics of the subjects.
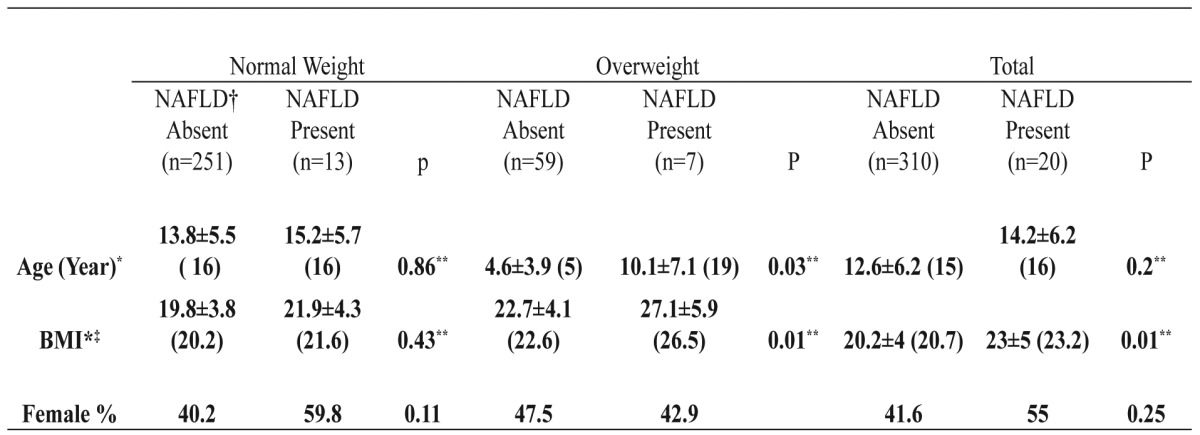
† Nonalcoholic fatty liver disease ‡Body Mass Indeks *Values are mean±SD (median) ** Mann-Whitney U test
Characteristic features of cases with NAFLD are shown in Table 3 according to age ranges. Motor vehicles were involved in all 10 deaths of cases with NAFLD. Other accidents (drowning, electric shock and falls) accounted for an additional 8 deaths. The remaining 2 cases died of other reasons.
Table 3. Characteristic features of subjects with NAFLD.
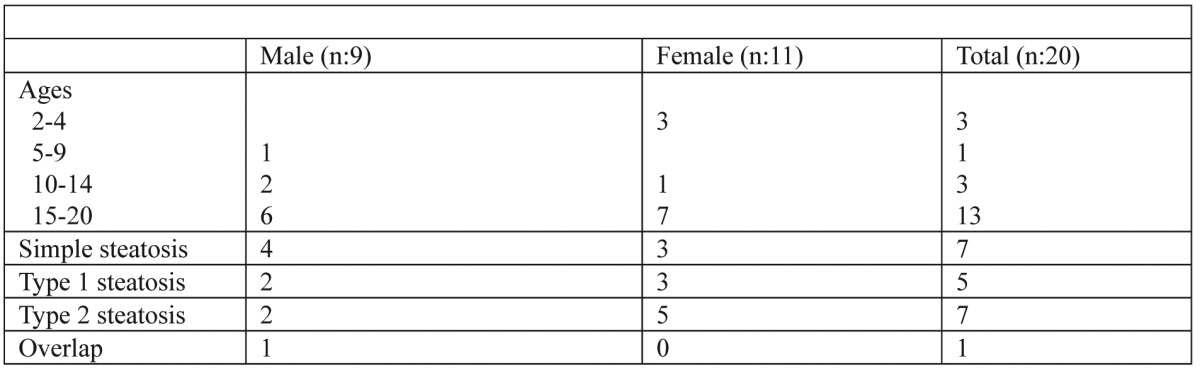
Simple steatosis was detected in 7 subjects. Steatohepatitis was characterized as type 1 in 5 subjects, type 2 in 7 subjects, and as overlap in 1 subject. The characteristic features of NAFLD subjects are given in Table 3
Discussion
We found that the prevalence of fatty liver in the obese and non-obese group was 10.6% and 4.9%, respectively. These findings clarify that fatty liver disease is also an important health problem in non-obese subjects.
Over the last decades, NAFLD has emerged as the leading cause of liver disease in pediatric populations worldwide and has increased in parallel to the rise in the prevalence of overweight people and obesity9,10. Mean BMI was significantly higher in patients with severe fatty liver11. However, it has been shown that an increased visceral adiposity, even in the presence of a normal weight, might be relevant in the pathogenesis of NAFLD12.
Many different methods are used to determine the prevalence of NAFLD. Most studies use serum aminotransferase elevations as a surrogate marker for fatty liver disease. In addition, some radiological methods such as ultrasonography, computed tomography and magnetic resonance imaging can be used13,14. However, the sensitivity and specificity of these methods have not been described. The gold standard diagnostic method is liver biopsy3. However, it is not feasible in a population-based study. Alternatively, autopsy series are means of estimating prevalence based on a histological diagnosis within select populations4. Another challenge is selection of a relevant population. The researchers expectedly worked on more overweight and obese children. However, NAFLD can be seen in normal-weight people.
The prevalence of NAFLD was reported to have a wide range (2.6-24%) in the world15-18. Based on ultrasound, fatty liver prevalence was predicted to be 2.6% in children of school-age in Japan14. In the United States, the National Health and Nutrition Examination Survey, cycle III (NHANES III) reported the rate of an elevated alanine aminotransferase in adolescents (age range: 12-18 years) as 3%19. A similar prevalence of abnormal ALT (3.2%) was reported by the Korean NHANES20. All of the reports have shown that pediatric fatty liver disease is also important.
It has been shown that NAFLD is not rare in non-obese adults2. Bacon et al21 worked on 33 adults who were diagnosed as clinical and histological NAFLD, of whom 61% were non-obese and 42% had normal glucose and lipid levels. Kim et al2 found that 16% of 460 normal-weight adults were diagnosed as NAFLD with ultrasound findings, whereas this ratio was 34% in obese individuals. We found that the frequency of NAFLD in non-obese children and adolescents aged 2-19 years was 4.9%, whereas it was 6% in the entire group and 10.6% in obese subjects.
Schwimmer et al4 reported the prevalence of histologically proven NAFLD as 9.6% in a case series of autopsies performed on children 2–19 years of age. In that study, the age group and methods were similar to those of our study. However, they found higher rates of NAFLD, which may be attributed to ethnicity. In another study, Wanless and Lentz22 found that the overall prevalence of steatohepatitis was 6.27% in adult autopsies of hospitalized patients, which is close to our records.
In the non-obese group, steatohepatitis was seen at a lower age than in the obese group, which may be explained by the role of hereditary factors in the etiopathogenesis of NAFLD. Previous studies have suggested that two single-nucleotide polymorphisms might confer a predisposition to NAFLD and insulin resistance23.
In our study, the prevalence of fatty liver was detected to increase with age. Studies demonstrate that frequency of fatty liver is higher in adolescents than in younger children, which explains the higher rate of NAFLD in adolescents, in view of the associated hormonal changes surrounding puberty or their increased control over unhealthy food choices and sedentary physical activity with age24. Hormonal changes during puberty may potentiate accumulation of fat in the liver.
NAFLD was reported as being more common in boys than girls24. These gender differences implicate estrogens as potentially protective, or indicate that androgens may aggravate NAFLD; however, we could not find any significant gender-related differences between our subjects with NAFLD.
Conclusion
The prevalence of fatty liver was 6% among all the subjects and was higher in the overweight group than in the normal-weight group (10.6% vs 4.9%; p<0.001). These findings state that fatty liver disease is also an important health problem in non-obese subjects. This suggests that whereas obesity may be a risk factor, other pathogenic factors may exist that could contribute to the NAFLD. Therefore, pediatricians should consider NAFLD in the differential diagnosis of abdominal pain, nonspecific symptoms such as fatigue or increased transaminase levels, even in normal–weight patients. Future studies may be useful in the development of strategies for early diagnosis and prevention of NAFLD in non-obese children and adolescents.
References
- 1.Reddy JK, Rao MS. Lipid metabolism and liver inflammation. II. Fatty liver disease and fatty acid oxidation. Am J Physiol Gastrointest Liver Physiol. 2006;290:G852–G858. doi: 10.1152/ajpgi.00521.2005. [DOI] [PubMed] [Google Scholar]
- 2.Kim HJ, Kim HJ, Lee KE, Kim DJ, Kim SK, Kim CW, et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med. 2004;164:2169–2175. doi: 10.1001/archinte.164.19.2169. [DOI] [PubMed] [Google Scholar]
- 3.Patton HM, Lavine JE, Van Natta ML, Schwimmer JB, Kleiner D, Molleston J. Clinical correlates of histopathology in pediatric nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1961–1971. doi: 10.1053/j.gastro.2008.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–1393. doi: 10.1542/peds.2006-1212. [DOI] [PubMed] [Google Scholar]
- 5.Vajro P, Fontanella A, Perna C, Orso G, Tedesco M, De VA. Persistent hyperaminotransferasemia resolving after weight reduction in obese children. J Pediatr. 1994;125:239–241. doi: 10.1016/s0022-3476(94)70202-0. [DOI] [PubMed] [Google Scholar]
- 6.Tazawa Y, Noguchi H, Nishinomiya F, Takada G. Serum alanine aminotransferase activity in obese children. Acta Paediatr. 1997;86:238–241. doi: 10.1111/j.1651-2227.1997.tb08881.x. [DOI] [PubMed] [Google Scholar]
- 7.Bundak R, Furman A, Gunoz H, Darendeliler F, Bas F, Neyzi O. Body mass index references for Turkish children. Acta Paediatr. 2006;95:194–198. doi: 10.1080/08035250500334738. [DOI] [PubMed] [Google Scholar]
- 8.Brunt EM. Nonalcoholic steatohepatitis: definition and pathology. Semin Liver Dis. 2001;21:3–16. doi: 10.1055/s-2001-12925. [DOI] [PubMed] [Google Scholar]
- 9.Shneider BL, Gonzalez-Peralta R, Roberts EA. Controversies in the management of pediatric liver disease: Hepatitis B, C and NAFLD: Summary of a single topic conference. Hepatology. 2006;44:1344–1354. doi: 10.1002/hep.21373. [DOI] [PubMed] [Google Scholar]
- 10.Matthiessen J, Velsing GM, Fagt S, Biltoft-Jensen A Jr, Stockmarr A, Andersen JS, et al. Prevalence and trends in overweight and obesity among children and adolescents in Denmark. Scand J Public Health. 2008;36:153–160. doi: 10.1177/1403494807085185. [DOI] [PubMed] [Google Scholar]
- 11.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM, et al. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 12.Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, et al. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 13.Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288:E462–E468. doi: 10.1152/ajpendo.00064.2004. [DOI] [PubMed] [Google Scholar]
- 14.Tominaga K, Kurata JH, Chen YK, Fujimoto E, Miyagawa S, Abe I, et al. Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci. 1995;40:2002–2009. doi: 10.1007/BF02208670. [DOI] [PubMed] [Google Scholar]
- 15.Barshop NJ, Sirlin CB, Schwimmer JB, Lavine JE. Review article: epidemiology, pathogenesis and potential treatments of paediatric non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2008;28:13–24. doi: 10.1111/j.1365-2036.2008.03703.x. [DOI] [PubMed] [Google Scholar]
- 16.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 17.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 18.Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40 Suppl 1:S5–10. doi: 10.1097/01.mcg.0000168638.84840.ff. [DOI] [PubMed] [Google Scholar]
- 19.Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr. 2000;136:727–733. [PubMed] [Google Scholar]
- 20.Park HS, Han JH, Choi KM, Kim SM. Relation between elevated serum alanine aminotransferase and metabolic syndrome in Korean adolescents. Am J Clin Nutr. 2005;82:1046–1051. doi: 10.1093/ajcn/82.5.1046. [DOI] [PubMed] [Google Scholar]
- 21.Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107:1103–1109. doi: 10.1016/0016-5085(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 22.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–1110. doi: 10.1002/hep.1840120505. [DOI] [PubMed] [Google Scholar]
- 23.Petersen KF, Dufour S, Hariri A, Nelson-Williams C, Foo JN, Zhang XM, et al. Apolipoprotein C3 gene variants in nonalcoholic fatty liver disease. N Engl J Med. 2010;362:1082–1089. doi: 10.1056/NEJMoa0907295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nobili V, Pinzani M. Paediatric non-alcoholic fatty liver disease. Gut. 2010;59:561–564. doi: 10.1136/gut.2009.187039. [DOI] [PubMed] [Google Scholar]


