Abstract
Background: The purpose of this study was to evaluate the attitudes and behavior of surgeons regarding preoperative smoking cessation.
Methods: A total of 109 anonymous questionnaires were distributed to non-vascular surgeons in our hospital, inquiring about their smoking attitudes, their smoking cessation advice practices, whether they appreciated the benefits of preoperative smoking cessation, and their knowledge of smoking cessation methods.
Results: Eighty questionnaires (from 51 resident doctors and 29 academic staff) were returned (response rate: 73.40%). Of the surgeons, 17.50% were current smokers. Although 40% of the surgeons surveyed believed that preoperative smoking cessation reduces postoperative complications, 31.2% of the surgeons (25/63) had given smoking cessation advice at least to 1 patient in the last month. Most of the resident doctors (39.2%) advised smoking cessation within a month; prior to surgery however, the academic staff (27.6%) advised cessation immediately before the operation (p=0.038). There was a significant difference between academic sfaff and resident doctors concerning the method to increase a patient’s chance of quitting (p=0.045), even among current smokers (p=0.049).
Conclusion: The surgeons who participated in the questionnaire were aware that smoking cessation improves outcome, but most of them did not appreciate that providing brief advice, referring to cessation services, or prescribing nicotine replacement therapy (NRT) may be of benefit in helping patients to quit. It is necessary to educate surgeons about the scale of the benefit and the efficacy of smoking cessation interventions or to set up systematic frameworks to offer smoking cessation advice to preoperative patients who smoke.
Keywords: preoperative smoking cessation, postoperative complications, surgeons, smoking cessation methods
Although tobacco smoking remains the leading cause of preventable death in the world1, current statistics indicate that it will not be possible to reduce tobacco related-deaths over the next 30 to 50 years, unless tobacco users are encouraged to quit. In this regard, health care professionals have a key role to play by working through the health care system to motivate and advise users to quit2. In particular many health care environments, including hospitals, have implemented no-smoking policies. Thus inpatients are ideally placed to receive smoking cessation advice and counseling3. However, the benefit of preoperative and long-term postoperative smoking cessation has been shown recently, too4,5.
Each year millions of cigarette smokers require surgery and anesthesia, so surgeons can play an important role in tobacco control and prevention of deaths due to cigarette smoking6. Two major benefits could result from efforts to help patients quit smoking. Firstly, smoking increases the risk of some postoperative complications, including pulmonary complications, such as atelectasis and pneumonia; cardiovascular complications, such as myocardial ischemia; and wound-related complications, such as infection7,8. Even temporary abstinence from smoking may reduce the risk of these complications and improve surgical outcomes9. Secondly, a surgical episode may represent a “teachable moment” that encourages smokers to permanently quit, with great benefits to their long-term health. However, little attention has been paid to the role of anesthesiologists and surgeons in addressing tobacco use. Indeed, although many surgical specialists recognize the adverse effects of smoking on both short and long-term outcomes, few are familiar with methods to help their patients quit smoking9. Moreover, some may have concerns with specific issues related to perioperative smoking cessation, such as whether it is safe for smokers to quit immediately before surgery or for physicians to administer nicotine replacement therapy (NRT) in surgical patients. In addition, they can help prevent or minimize smoking-related illnesses, such as lung cancer and cervical cancer by acting as healthy role models, by changing their own smoking behaviors and altering their smoking cessation practices toward patients6,10.
Despite the high prevalence of smoking (33.4%) in Turkey11, during the past 10 years increasing interest has been shown to smoking cessation (SC), both in terms of education and counseling12. So, we aimed to determine surgeons’ smoking knowledge and attitudes and to explore whether surgeons are advising their patients regarding smoking cessation and offering interventions.
Methods
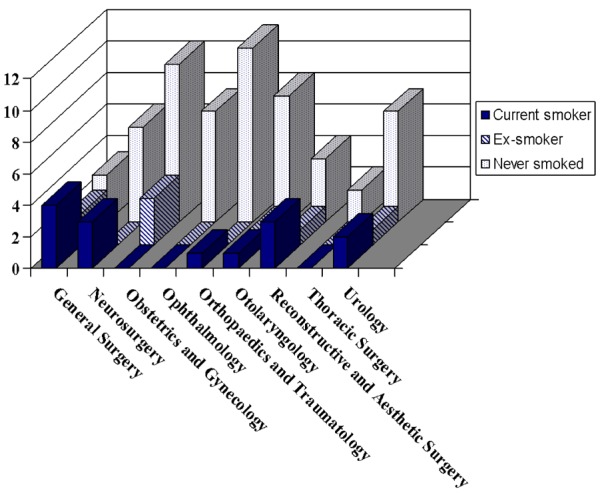
A modified form of the questionnaire handed in Turkish, originally developed from the study of Owen and et al13 was distributed to 109 surgeons (37 [33,94%] academic staff, and 72 [66,06%] resident doctors) who regularly see surgery patients preoperatively (Figure 1). Vascular surgeons were not included in this study, as smoking is intimately involved in the “pathogenesis of atherosclerosis and affects the results of treatment.
Figure 1. The distribution of the department of surgeons according to their smoking status.
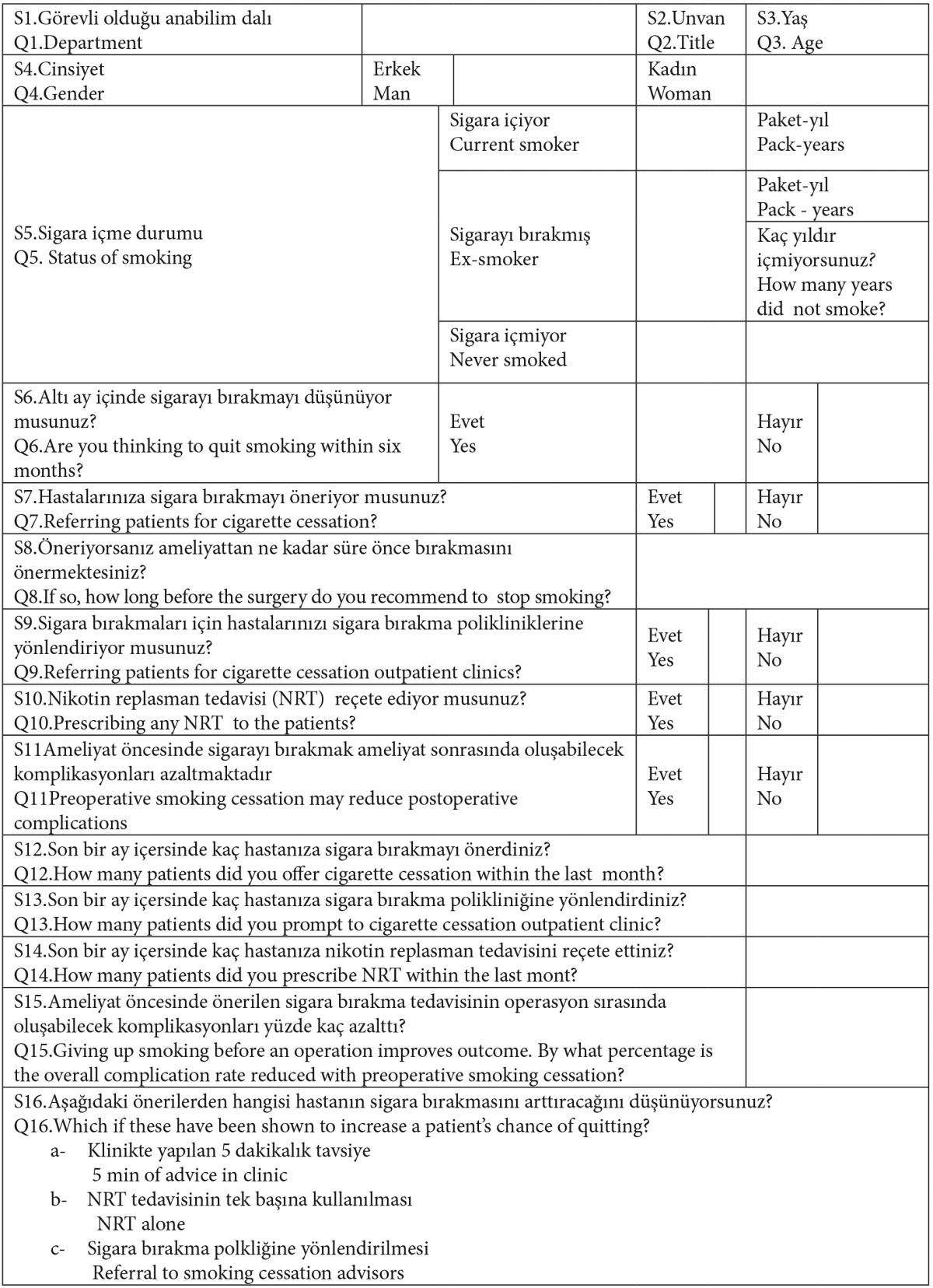
It was a self-administered questionnaire consisted of 16 questions investigating the demographic features and personal smoking behaviors of surgeons; pack years ( where one “pack year” is 20 cigarettes smoked/day for one year)14 and attitudes toward smoking cessation; how often they had given smoking cessation advice, prescribed nicotine replacement therapy (NRT), or referred patients to smoking cessation services in the preceding month (Table 1).
Table 1. The form of the questionnaire.
Smoking status was used to classify the participants into three groups: never smoked, ex-smoker (defined as an individual who had stopped smoking at least 1 year prior to the time of the survey), and current smoker15.
Statistical analysis
All data analyses was done using the SPSS for Windows (version 16.0, SPSS, Chicago, II, USA), with the level of significance set at p<0.05. The results are expressed as mean ±S.E. in this study. The results of the study were evaluated using the factorial design ANOVA. There were two factors in this study: the academic member factor, which consisted of academic staff and resident doctors, and the smoking status of the academic members (smoked or never smoked). Mann-Whitney U tests were used to evaluate the parameters which did not provide the precondition of parametric tests. Differences between the smoking status group and the academic members group were assessed using Pearson’s chi-square test.
Results
A total of 80 non-vascular surgeons (34.61±0.90 years old) responded to the questionnaire (response rate: 73.40%). Fifty-one (29.58±0.40 years old) were resident doctors, and 29 of them (43.45±1.12 years old) were academic staff (Mann-Whitney U, p=0.000).
The chi-square analysis indicated that there was not a significant difference in smoking status between academic staff and resident doctors. The current smoking prevalence of the Turkish male surgeons in the study was 17.50% (n=14, 12.05±2.03 pack .years). Five of them (6.25%) were academic staff. Ten of the current smokers admitted that they were considering quitting within 6 months. There were 4 ex-smokers in each group, and 58 participants (72.5%) indicated that they had never smoked (Table 2).
Table 2. The demographic properties of the surgeons and their knowledge about the efficacy of smoking cessation interventions and the benefit of preoperative smoking cessation.
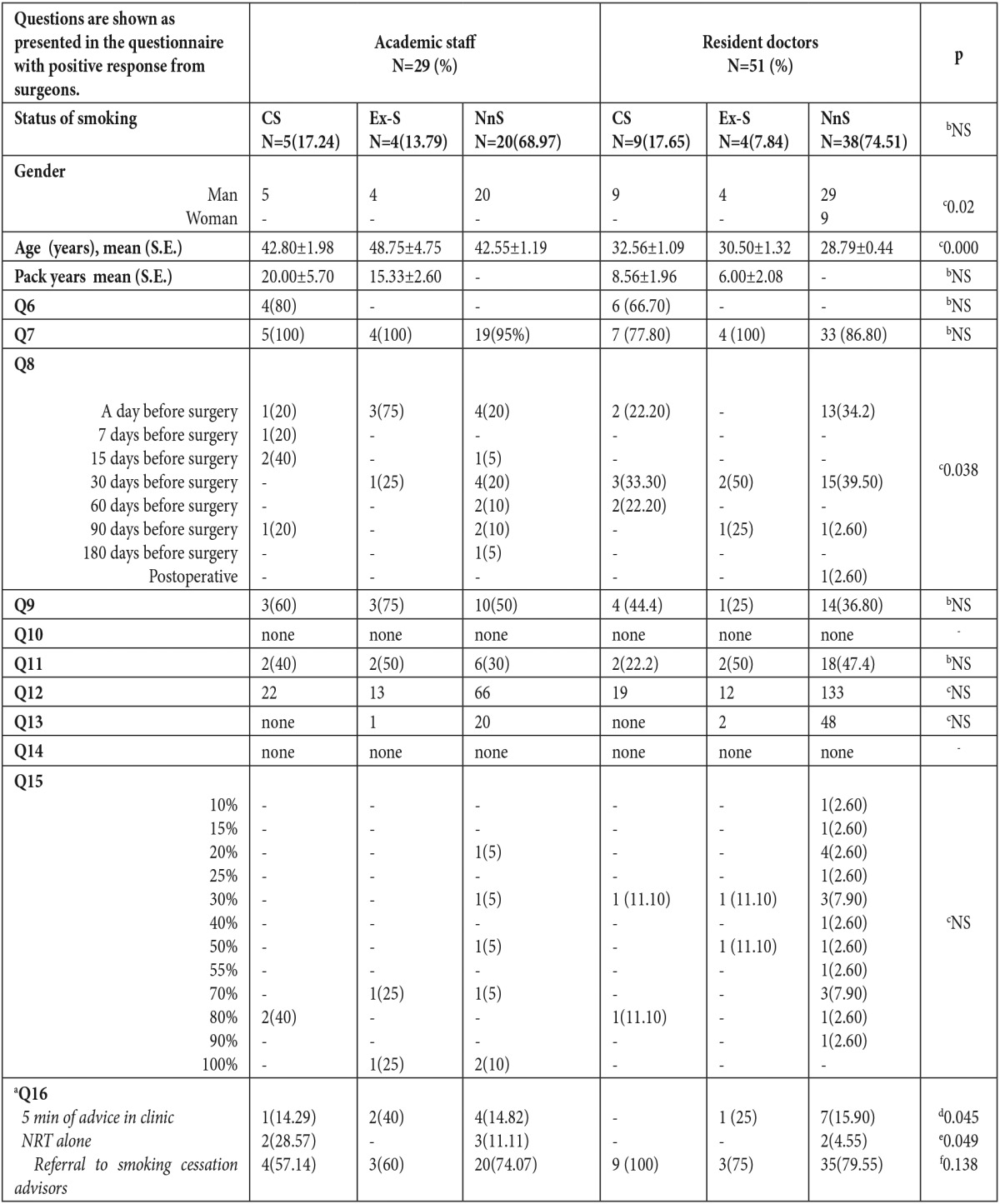
NRT:nicotine replacement therapy. NS: nonspecific. CS: Current smoker, EX-S:Ex-smoker, NnS:Nonsmoker. aThe answers were given more than once. bPearson’s chi-square test. p<0.05, c,Mann-Whitney U p<0.05 or p<0.01.dthe answers of the participants or eonly current smokers or f only nonsmokers to the question; the methods used to increase a patient’s chance of quitting, Mann-Whitney U p<0.05.
Although 40% of the surgeons believed that preoperative smoking cessation reduced postoperative complications. Only 4 surgeons reported advising cessation within the previous 8 months prior to surgery. Most of the resident doctors (66.7%) had advised smoking cessation within a month prior to surgery however, academic staff (34.78%) advised smoking cessation immediately before the operation (a day before surgery) (Mann-Whitney U p=0.038), (Table 2).
With regard to referral of patients to cigarette cessation outpatient clinics, the academic member/smoking status interaction and the differences between academic member factor means and smoking status factor means were not statistically significant. Only 43.8% of the surgeons indicated that they offered their patients a referral to a smoking cessation outpatient clinic. None of them offered NRT to their patients.
There was a significant difference between academic staff and resident doctors in the methods used to increase a patient’s chance of quitting (Mann-Whitney U p=0.045), even in those currently smokers (Mann Whitney U p=0.049). However this was not supported by nonsmoking participants (p>0,05). Most of them (85.7%) indicated that referral to a smoking cessation outpatient clinic enhances a patient’s chance of successful cessation. (Table 2).
Discussion
The main finding of this study was that there was a conflict in the duration of preoperative smoking cessation and the methods employed to increase a patient’s chance of quitting between academic staff and resident doctors and also between current smokers and nonsmokers.
Smoking prevalence among Turkish doctors was reported to range between 32.6% and 66.2% in a meta-analysis of 22 studies16. The highest percentage of smokers was found among physicians of surgical medicine, and the lowest percentage of smokers was found in the physicians of primary care medicine in our country17,18. Contrary to Kaetsu et al19, this finding is consistent with the findings of other studies20. In our study, 17.50% of surgeons, most of them being resident doctors (11.25%), were current smokers, which is not consistent with the results of other studies17,18,21. Ten of the current smokers (71.24%) stated that they would try to quit smoking within 6 months, so these findings reflected that they had the necessary courage and motivation to quit smoking.
It is well-documented that smoking cessation has significant benefits on mortality and morbidity22; however, many smokers never consider quitting until a health problem occurs. There is strong evidence that patients concern smoking cessation with certain events. Pregnancy, disease diagnosis, and hospitalization are associated with increased rates of spontaneous smoking cessation compared with the rate in the general population. Among hospitalized patients, it appears that the chances of quitting increase with the intensity of medical interventions6. The United States Public Health Service Guideline on Tobacco Use and Dependence states that “all physicians should strongly advise every patient who smokes to quit”23. The scheduling of patients for surgery is an appropriate time-point to help reduce the preoperative and postoperative complications of smoking cigarettes and encourage quitting. Among patients scheduled for surgery, those undergoing more extensive interventions (for example, those undergoing inpatient versus outpatient procedures) have a greater likelihood of spontaneously quitting after surgery24. Thus, surgery can serve as a teachable moment as defined25. Raw et al26 found that 3 min of advice in a clinic increased a patient’s chance of quitting by 2%. More intensive interventions are even more effective, and there is a dose-response relationship between the total time spent in interventions and efficacy24.
However, our results demonstrate that surgeons are not using these interventions and they are not aware of their efficacy. Clinical practice guidelines formulated by the United States Public Health Service recommend efficacious techniques for the provision of tobacco interventions by clinicians, codified as the “5 As” approach—ask, advise, assess, assist, and arrange27. In this study, although the majority of the participants, especially nonsmoking resident doctors, reported that they adviced for smoking cessation, only few performed further efforts, such as referring smoking cessation outpatient clinics (43.8%). This finding is consistent with previous studies on physician delivered smoking cessation interventions in other countries28,29. Several barriers to adoption of the 5 As approach by clinicians have been identified, including lack of time, training, and low self-efficacy30,31. There is not difference for the academic staff and the resident doctors in our study.
What is unknown in most cases is the minimum duration of preoperative abstinence necessary to confer benefit. Observational studies suggest that at least 2 months of preoperative abstinence is required for full benefit32,33. Some researchers have interpreted such observational studies as showing that quitting smoking within a few weeks before surgery actually increases the risk of complications32, but other researchers assert the contrary34. However, it is important to know the fact that some important adverse effects in pulmonary and cardiovascular system induced by nicotine and CO could be restored within 24 to 48 hours of smoking cessation35.
Additionally, all of the participants stated that they never offered NRT to their patients for smoking cessation or managing withdrawal symptoms that do occur. Owen et al13 reported a similar result in their study. They indicated that most surgeons did not appreciate how much more successful cessation attempts were likely to be if they are augmented with NRT and referral to cessation services. There was a significant difference between academic staff and resident doctors regarding the methods used to increase a patient’s chance of quitting, even in current smokers, in our study. Most of them (85.7%) indicated that referral to a smoking cessation outpatient clinic enhances the chance of success. However, this was not supported by nonsmoking participants in our study.
This study has several potential limitations. The primary limitation is whether this sample is representative of Turkish surgeons of an university hospital. Another limitation to the study was that vascular surgeons were not included in this study as smoking is intimately involved in the pathogenesis of atherosclerosis and affects the results of treatment. We assume that this group of surgeons would have significantly different results from the rest of the surgical workforce. Finally, this survey methodology relies on self-report of behavior, which may not reflect actual behavior. It is possible that social desirability may result in bias in our estimates of male surgeons’ attitudes and behavior concerning smoking cessation activities.
In conclusion, the surgeons who participated in the questionnaire were aware that smoking cessation improves outcomes, but most of them did not realize that providing brief advice, referring patients to cessation services, or prescribing NRT may be of benefit in helping patients to quit. Further, there was a difference between academic staff and resident doctors in applications to increase a patient’s chance of quitting. Although these findings cannot be generalized to all Turkish surgeons, our results show that there are difficulties in integrating smoking cessation treatment into surgical departments. Surgeons, both academic staff and resident doctors, should actively participate in tobacco control training and education to improve their knowledge and attitudes toward smoking. This will lead to improvements in surgeons’ own smoking behavior, as well as the frequency with which they inquire about patients’ smoking status and encouraging patients to quit smoking. More importantly, interventions should be designed for surgical patients in Turkey, as successful innovations could both improve perioperative outcomes.
*Presented as e-poster at 31st National Congress of Turkish Respiratory Society
References
- 1.Report on the Global Tobacco Epidemic (2008) WHO. http://www.who.int/tobacco/mpower/mpower_report_tobacco_crisis_2008.pdf. Accessed 1 Aug 2011.
- 2.Saddichha S, Rekha DP, Patil BK, Murthy P, Benegal V, Isaac MK. Knowledge, attitude and practices of Indian dental surgeons towards tobacco control: advances towards prevention. Asian Pac J Cancer Prev. 2010;11:939–942. [PubMed] [Google Scholar]
- 3.Cropley M, Theadom A, Pravettoni G, Webb G. The effectiveness of smoking cessation interventions prior to surgery: a systematic review. Nicotine Tob Res. 2008;10:407–412. doi: 10.1080/14622200801888996. [DOI] [PubMed] [Google Scholar]
- 4.Thomsen T, Tonnesen H, Moller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg. 2009;96:451–461. doi: 10.1002/bjs.6591. [DOI] [PubMed] [Google Scholar]
- 5.Moller A, Tonnesen H. Risk reduction: perioperative smoking intervention. Best Pract Res Clin Anaesthesiol. 2006;20:237–248. doi: 10.1016/j.bpa.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Warner DO. Helping surgical patients quit smoking: Why, When, and How. Anesth Analg. 2005;101:481–487. doi: 10.1213/01.ANE.0000159152.31129.84. [DOI] [PubMed] [Google Scholar]
- 7.Egan TD, Wong KC. Perioperative smoking cessation and anesthesia: A review. J Clin Anesth. 1992;4:63–72. doi: 10.1016/0952-8180(92)90123-i. [DOI] [PubMed] [Google Scholar]
- 8.Myles PS, Iacono GA, Hunt JO, Fletcher H, Morris J, McIlroy D, et al. Risk of respiratory complications and wound infection in patients undergoing ambulatory surgery: smokers versus nonsmokers. Anesthesiology. 2002;97:842–847. doi: 10.1097/00000542-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Warner DO, Sarr MG, Offord K, Dale LC. Anesthesiologists, general surgeons, and tobacco interventions in the perioperative period. Anesth Analg. 2004;99:1776–1783. doi: 10.1213/01.ANE.0000136773.40216.87. [DOI] [PubMed] [Google Scholar]
- 10.Yao T, Ong M, Lee A, Jiang Y, Mao Z. Smoking Knowledge, Attitudes, Behavior, and Associated Factors among Chinese Male. Surgeons World J Surg. 2009;33:910–917. doi: 10.1007/s00268-009-9938-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gürcan A, Demir Ö. [Family Structure Survey 2006]. Yayın No:3046. Ankara: Türkiye İstatistik Kurumu Matbaası. 2006 (Turkish) [Google Scholar]
- 12.Gokirmak M, Ozturk O, Bircan A, Akkaya A. The attitude toward tobacco dependence and barriers to discussing smoking cessation: a survey among Turkish general practitioners. Int J Public Health. 2010;55:177–183. doi: 10.1007/s00038-009-0109-8. [DOI] [PubMed] [Google Scholar]
- 13.Owen D, Bicknell C, Hilton C, Lind J, Jalloh I, Owen M, et al. Preoperative smoking cessation: a questionnaire study. Int J Clin Pract. 2007;61:2002–2004. doi: 10.1111/j.1742-1241.2007.01565..x. [DOI] [PubMed] [Google Scholar]
- 14.Prignot J. Quantification and chemical markers of tobacco-exposure. Eur J Respir Dis. 1987;70:1–7. [PubMed] [Google Scholar]
- 15.Sawabata N, Miyoshi S, Matsumura A, Ohta M, Maeda H, Sueki H, et al. Prognosis of smokers following resection of pathological stage I non-small-cell lung carcinoma. Gen Thorac Cardiovasc Surg. 2007;55:420–424. doi: 10.1007/s11748-007-0159-x. [DOI] [PubMed] [Google Scholar]
- 16.Tezcan S, Yardım N. [Prevalance of smooking between the doctors, nurses and medical faculty students at some health facilities in Turkey] Tuberk Toraks (Turkish) 2003;51:390–397. [PubMed] [Google Scholar]
- 17.Salepçi B, Fidan A, Çağlayan B, Torun E, Durmuş N, Aktürk AÜ, et al. [Smoking rates of health care workers at a General Training Hospital in Istanbul and their attitudes and knowledge about smoking] Solunum (Turkish) 2006;8:156–162. [Google Scholar]
- 18.Demiralay R. The behaviour and attitude of physicians in the Lakes Region towards smoking. Turk J Med Sci. 2003;33:329–334. [Google Scholar]
- 19.Kaetsu A, Fukushima T, Moriyama M, Shigematsu T. Change of the smoking behavior and related lifestyle variables among physicians in Fukuoka, Japan: a longitudinal study. J Epidemiol. 2002;12:208–216. doi: 10.2188/jea.12.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samuels N. Smoking among hospital doctors in Israel and their attitudes regarding anti-smoking legislation. Public Health. 1997;111:285–288. doi: 10.1038/sj.ph.1900388. [DOI] [PubMed] [Google Scholar]
- 21.Akpınar F, Borlu A, Şarlı ŞM, Balcı E, Horoz D, Gün I, et al. [Some characteristics of life pattern and the problems to come across while working in the asistants to specialize in Erciyes University Medical Faculty Hospital] TAF Prev Med Bull Turkish. 2008;7:311–316. [Google Scholar]
- 22.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service Report. JAMA. 2000;283:3244–3254. [PubMed] [Google Scholar]
- 24.Warner DO, Patten CA, Ames SC, Offord K, Schroeder D. Smoking behavior and perceived stress in cigarette smokers undergoing elective surgery. Anesthesiology. 2004;100:1125–1137. doi: 10.1097/00000542-200405000-00014. [DOI] [PubMed] [Google Scholar]
- 25.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 26.Raw M, McNeill A, West R. Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Health Education Authority. Thorax. 1998;53 (Suppl. 5, part 1):S1–S19. doi: 10.1136/thx.53.2008.s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff: A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jordan TR, Dake JR, Price JH. Best practices for smoking cessation in pregnancy: Do obstetrician/gynecologists use them in practice? J Womens Health (Larchmt) 2006;15:400–124419. doi: 10.1089/jwh.2006.15.400. [DOI] [PubMed] [Google Scholar]
- 29.Doescher MP, Saver BG. Physicians’ advice to quit smoking. The glass remains half empty. J Fam Pract. 2000;49:543–547. [PubMed] [Google Scholar]
- 30.Boldemann C, Gilljam H, Lund KE, Helgason AR. Smoking cessation in general practice: The effects of a quitline. Nicotine Tob Res. 2006;8:785–790. doi: 10.1080/14622200601004059. [DOI] [PubMed] [Google Scholar]
- 30.Kai T, Maki T, Takahashi S, Warner DO. Perioperative tobacco use interventions in Japan: A survey of thoracic surgeons and anaesthesiologists. Br J Anaesth. 2008;100:404–410. doi: 10.1093/bja/aem400. [DOI] [PubMed] [Google Scholar]
- 32.Warner MA, Offord KP, Warner ME, Lennon RL, Conover MA, Jansson-Schumacher U. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc. 1989;64:609–616. doi: 10.1016/s0025-6196(12)65337-3. [DOI] [PubMed] [Google Scholar]
- 33.Warner MA, Divertie MB, Tinker JH. Preoperative cessation of smoking and pulmonary complications in coronary artery bypass patients. Anesthesiology. 1984;60:380–383. doi: 10.1097/00000542-198404000-00022. [DOI] [PubMed] [Google Scholar]
- 34.Moores LK. Smoking and postoperative pulmonary complications:An evidence-based review of the recent literature. Clin Chest Med. 2000;21:139–146. doi: 10.1016/s0272-5231(05)70013-7. [DOI] [PubMed] [Google Scholar]
- 35.Lida H. Preoperative assessment of smoking patient. Masui. 2010;59:838–843. [PubMed] [Google Scholar]


