Abstract
Throughout evolution sunlight produced vitamin D in the skin has been critically important for health. Vitamin D, known as the sunshine vitamin, is actually a hormone. Once it is produced in the skin or ingested from the diet it is converted sequentially in the liver and kidneys to its biologically active form 1,25-dihydroxyvitamin D. This hormone interacts with its receptor in the small intestine to increase the efficiency of intestinal calcium and phosphate absorption for the maintenance of the skeleton throughout life. Vitamin D deficiency during the first few years of life results in a flattened pelvis making it difficult for childbirth. Vitamin D deficiency causes osteopenia and osteoporosis increasing risk of fracture. Essentially every tissue and cell in the body has a vitamin D receptor. Therefore vitamin D deficiency has been linked to increased risk for preeclampsia, requiring a Cesarean section for birthing, multiple sclerosis, rheumatoid arthritis, type I diabetes, type II diabetes, heart disease, dementia, deadly cancers and infectious diseases. Therefore sensible sun exposure along with vitamin D supplementation of at least 2000 IU/d for adults and 1000 IU/d for children is essential to maximize their health.
Historical Perspective
At the turn of the 20th century, rickets was rampant in the industrialized cities of northern Europe and North America.(1) Vitamin D deficiency resulted in severe growth retardation and poor mineralization of the skeleton resulting in bony deformities especially of the lower extremities, classically known as rickets. What is not fully appreciated however is that vitamin D deficiency in utero and during the first few years of life had additional potentially deadly consequences for women during their child bearing years. Their pelvis was often flattened, their pelvic outlet was reduced in size, making it difficult if not impossible to have a vaginal delivery. It was because of rickets in childbearing women that led to the common practice of cesarean sectioning. It has been suggested that the driver in evolution for skin pigment to have decreased was due to the fact that heavily pigmented women who migrated into Europe would have had an especially difficult time in making enough vitamin D therefore increasing their risk as well as their infant’s risk for vitamin D deficiency. For female infants and children who developed rickets this would have made it very difficult for them during their childbearing years to have given birth successfully. Therefore within a few generations skin pigmentation would have had to be substantially reduced in order to sustain the reproductive capacity of humans who migrated north and south of the equator. This is the likely reason why Neanderthals were not dark skinned and hairy hominids but rather redheaded with Celtic white skin. (2)
Vitamin D Sources and Metabolism
The major source of vitamin D is exposure to sunlight. When the sun strikes the skin the ultraviolet B portion of the sun spectrum enters into the viable epidermis and dermis and is absorbed by 7-dehydrocholesterol which is converted to vitamin D3.(Fig 1)(3) Once formed previtamin D3 is rapidly converted to vitamin D3 by a temperature dependent process. Time of day, season of the year, latitude, aging, sunscreen use and degree of skin pigmentation can all have a dramatic influence on the cutaneous production of vitamin D3. For example living above Atlanta Georgia essentially no vitamin D can be produced in the skin from November through February. Vitamin D production does not occur before 9 AM and ceases after 4 PM even in the summer.(Fig 2) (4–6) People of color require much longer exposure to sunlight because their skin pigment acts as a natural sunscreen reducing their ability to make vitamin D3 in the skin when compared to a Caucasian exposed to the same amount of sunlight. African Americans often need 5 to 10 times longer exposure compared to Caucasians to make the same amount of vitamin D in the skin which explains why they are at much higher risk for vitamin D deficiency. A sunscreen with an SPF of 30 absorbs approximately 95% of incident UVB radiation and thus reduces the production of vitamin D in the skin by about 95%.(8) Aging also influences the production of vitamin D and a person 70 years of age has only about 25% of the capacity to produce vitamin D compared to a 20-year-old.(9) Exposure to sunlight through glass will not produce any vitamin D because glass absorbs all UVB radiation.
Figure 1.
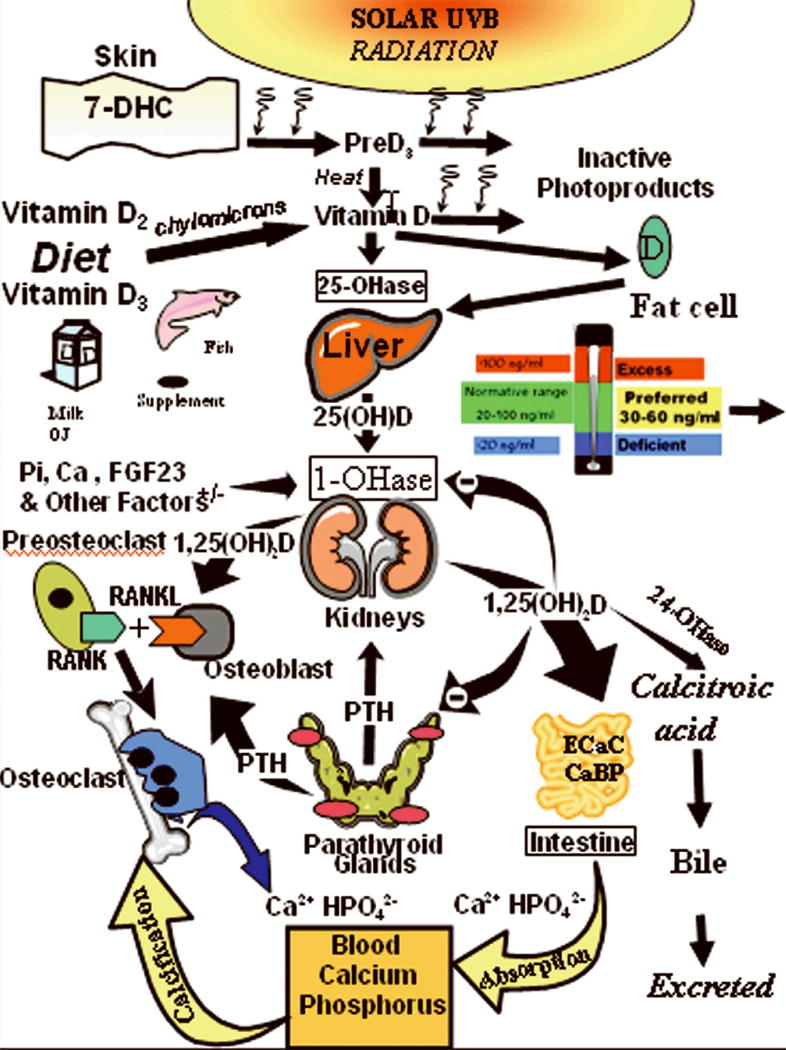
Schematic representation of the synthesis and metabolism of vitamin D for regulating calcium, phosphorus and bone metabolism. During exposure to sunlight 7-dehydrocholesterol in the skin is converted to previtamin D3. PreD3 immediately converts by a heat dependent process to vitamin D3. Excessive exposure to sunlight degrades previtamin D3 and vitamin D3 into inactive photoproducts. Vitamin D2 and vitamin D3 from dietary sources is incorporated into chylomicrons, transported by the lymphatic system into the venus circulation. Vitamin D (D represents D2 or D3) made in the skin or ingested in the diet can be stored in and then released from fat cells. Vitamin D in the circulation is bound to the vitamin D binding protein which transports it to the liver where vitamin D is converted by the vitamin D-25-hydroxylase to 25-hydroxyvitamin D [25(OH)D]. This is the major circulating form of vitamin D that is used by clinicians to measure vitamin D status (although most reference laboratories report the normal range to be 20-100 ng/ml, the preferred healthful range is 30-60 ng/ml). It is biologically inactive and must be converted in the kidneys by the 25-hydroxyvitamin D-1α-hydroxylase (1-OHase) to its biologically active form 1,25-dihydroxyvitamin D [1,25(OH)2D]. Serum phosphorus, calcium fibroblast growth factors (FGF-23) and other factors can either increase (+) or decrease (-) the renal production of 1,25(OH)2D. 1,25(OH)2D feedback regulates its own synthesis and decreases the synthesis and secretion of parathyroid hormone (PTH) in the parathyroid glands. 1,25(OH)2D increases the expression of the 25-hydroxyvitamin D-24-hydroxylase (24-OHase) to catabolize 1,25(OH)2D to the water soluble biologically inactive calcitroic acid which is excreted in the bile. 1,25(OH)2D enhances intestinal calcium absorption in the small intestine by stimulating the expression of the epithelial calcium channel (ECaC) and the calbindin 9K (calcium binding protein; CaBP). 1,25(OH)2D is recognized by its receptor in osteoblasts causing an increase in the expression of receptor activator of NFκB ligand (RANKL). Its receptor RANK on the preosteoclast binds RANKL which induces the preosteoclast to become a mature osteoclast. The mature osteoclast removes calcium and phosphorus from the bone to maintain blood calcium and phosphorus levels. Adequate calcium and phosphorus levels promote the mineralization of the skeleton. Holick copyright 2007. Reproduced with permission.
Figure 2.
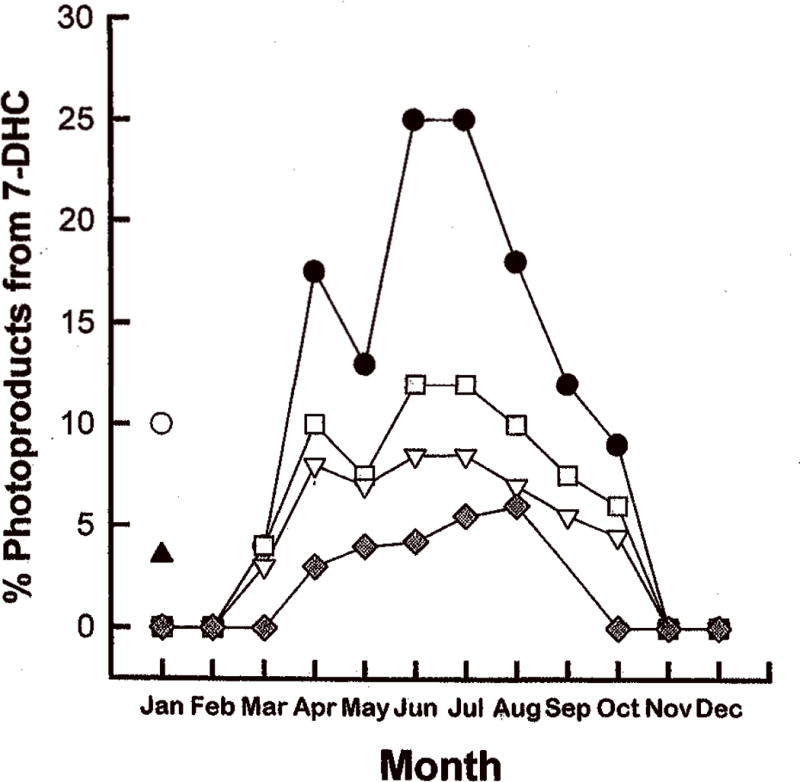
Photosynthesis of previtamin D3 after exposure of 7-dehydrocholesterol (7-DHC) to sunlight. Measurements were as follows: in Boston (42°N) after 1 hr (□) and 3 hr (◻) and total photoproducts (previtamin D3, lumisterol, and tachysterol) after 3 h in Boston (●); in Edmonton, Canada (52°N), after 1 hr (■); in Los Angeles (34°N) (▲) and Puerto Rico (18°N) in January (○). Reprinted with permission from Webb et al. [6].
Very few foods naturally contain vitamin D. (Table 1)(3) The major sources are wild caught salmon, other oily fish, cod liver oil and mushrooms which have enhanced vitamin D when exposed to UVB radiation. Some foods are fortified with vitamin D including milk and some other dairy products including yogurt and some cheeses, cereals and some juices. There are two forms of vitamin D. Vitamin D3 is produced in the skin and is also generated from lanolin which is then used for food fortification and vitamin D3 supplements. Vitamin D2 is made in yeast and mushrooms exposed to UVB radiation. Vitamin D2 is the only pharmaceutical form of vitamin D and available by prescription in the United States and is used in some supplements and food fortification. Vitamin D2 is as effective as vitamin D3 in maintaining both children’s and adults’ vitamin D status.(10)
TABLE 1.
Sources of Vitamin D2 and Vitamin D3 (with permission, copyright Holick 2010)
| SOURCE | VITAMIN D CONTENT IU = 25 ng |
|---|---|
| Natural Sources |
|
| Cod liver oil | ~400 – 1,000 IU/tsp vitamin D3 |
| Salmon, fresh wild caught | ~600-1,000 IU/3.5 oz vitamin D3 |
| Salmon, fresh farmed | ~100-250 IU/3.5 oz vitamin D3, vitamin D2 |
| Salmon, canned | ~300-600 IU/3.5 oz vitamin D3 |
| Sardines, canned | ~300 IU/3.5 oz vitamin D3 |
| Mackerel, canned | ~250 IU/3.5 oz vitamin D3 |
| Tuna, canned | 236 IU/3.5 oz vitamin D3 |
| Shiitake mushrooms, fresh | ~100 IU/3.5 oz vitamin D2 |
| Shiitake mushrooms, sun dried | ~1,600 IU/3.5 oz vitamin D2 |
| Egg yolk | ~20 IU/yolk vitamin D3 or D2 |
| Sunlight/UVB radiation | ~20,000 IU equivalent to exposure to 1 minimal erythemal dose (MED) in a bathing suit. Thus, exposure of arms and legs to 0.5 MED is equivalent to ingesting ~ 3,000 IU vitamin D3. |
| Fortified Foods | |
| Fortified milk | 100 IU/8 oz usually vitamin D3 |
| Fortified orange juice | 100 IU/8 oz vitamin D3 |
| Infant formulas | 100 IU/8 oz vitamin D3 |
| Fortified yogurts | 100 IU/8 oz usually vitamin D3 |
| Fortified butter | 56 IU/3.5 oz usually vitamin D3 |
| Fortified margarine | 429/3.5 oz usually vitamin D3 |
| Fortified cheeses | 100 IU/3 oz usually vitamin D3 |
| Fortified breakfast cereals | ~100 IU/serving usually vitamin D3 |
| Pharmaceutical Sources in the United States | |
| Vitamin D2 (Ergocalciferol) | 50,000 IU/capsule |
| Drisdol (vitamin D2) liquid | 8000 IU/cc |
| Supplemental Sources | |
| Multivitamin | 400, 500, 1000 IU vitamin D3 or vitamin D2 |
| Vitamin D3 | 400, 800, 1000, 2000, 5,000, 10,000, and 50,000 IU |
Once vitamin D (D represents D2 or D3) is made in the skin or ingested it travels to the liver where it is converted to 25-hydroxyvitamin D [25(OH)D].(Fig 1) 25(OH)D is the major circulating form of vitamin D that is measured by a physician to determine a person’s vitamin D status. (2) However 25(OH)D is biologically inert and is transported to the kidneys where it is converted to its active form 1,25-dihydroxyvitamin D [1,25(OH)2D]. (Fig 1) 1,25(OH)2D travels to the intestine and interacts with its receptor the vitamin D receptor (VDR) to enhance intestinal calcium absorption. It also travels to the skeleton to help maintain a healthy skeleton by enhancing the bone remodeling process.
Consequences of Vitamin D Deficiency on Bone and Muscle Health
It is now recognized that vitamin D deficiency is one of the most common medical conditions in the world. (1,3.11) It has been estimated that upwards of 50% of both children and adults living in the United States, Canada, Mexico, Europe, Asia, New Zealand and Australia are vitamin D deficient. (3) When a child or adult is vitamin D deficient they are unable to absorb enough calcium from their diet to satisfy their body’s calcium requirement and this results in an increase in the production of parathyroid hormone (PTH). PTH efficiently removes calcium from the skeleton to maintain the blood calcium level which is essential for neuromuscular and all metabolic activities.(5) As a result a child will not be able to accrue his or her maximum bone density especially during their growth spurt. Young and middle-aged adults will begin to lose on average 0.5% of their skeletal mass per year and over a period of 10 to 20 years can lose as much as 5 to 10% of their skeletal mass increasing their risk for osteoporosis and fracture. After menopause women begin to rapidly lose as much as 3-5% of their bone mass due to the loss of estrogen stimulation on the skeleton and vitamin D deficiency exacerbates this loss increasing further risk for a woman developing osteoporosis earlier in life putting her at higher risk for fracture.(5,11)
Vitamin D deficiency in early childhood causes rickets which is rarely seen except for children who are exclusively breast-fed and who do not receive any vitamin D supplementation. (1,12,13) Vitamin D deficiency in an older child and in all adults causes a mineralization defect of the skeleton identical to what happens in a younger child developing rickets. The difference is the very young child essentially has no mineral in the skeleton and as a result has a variety of skeletal deformities. Older children and adults have enough mineral in the skeleton preventing them from developing overt skeletal deformities. Instead the mineralization defect prevents the collagen from being properly mineralized. This results not only in a decrease in the bone mineral density but also causes throbbing aching bone pain as well as muscle weakness and muscle pain. This disease is known as osteomalacia and is often misdiagnosed as fibromyalgia. (14,15) Ninety percent of 150 children and adults (ages 10-65 years) who presented to a local emergency department with aches and pains in their bones and muscles were found to be vitamin D deficient. (14)
Vitamin D deficiency increases risk for muscle weakness and falling.(1) Studies in both female children and women have demonstrated that increasing their vitamin D status improves their muscle strength.(16) For older men and women this can reduce their risk of falling by as much as 72% thereby reducing risk of fracture. (17,18)
Other Consequences of Vitamin D Deficiency
It is now recognized that pregnant women are at very high risk for vitamin D deficiency. It was reported that 76% of moms at the time that they gave birth were vitamin D deficient despite the fact that they took a prenatal vitamin and drank two glasses of milk a day on average thus obtaining approximately 600 IU of vitamin D a day. 81% of their newborns were also found to be vitamin D deficient. (19) During pregnancy vitamin D deficiency has been associated with a 3-4 fold increase risk for developing preeclampsia, the most serious complication of pregnancy. (20) Because vitamin D is so important for muscle function it was not a surprise that in over 400 women who were having their first child there was a more than 300% increase risk for them requiring a Cesarean section if they were vitamin D deficient. (21)
Lactating moms are at high risk for vitamin D deficiency even if they’re taking their prenatal vitamin. As a result they put their infant at risk for vitamin D deficiency if the infant receives as his or her sole source of nutrition human breast milk.(12,13) It is for this reason that the American Academy of Pediatrics has now recommended that all infants and all children should receive 400 IU of vitamin D supplement daily. (22) For a lactating woman to put enough vitamin D in her milk to satisfy her infant’s requirement she would need to take 4000-6000 IU of vitamin D a day.(13) Although this sounds like an extraordinarily high amount of vitamin D is very likely that our hunter gatherer forefathers exposed to sunlight daily were making thousands of IUs of vitamin D a day in their skin and therefore it is not unreasonable to believe that 4000-6000 IU of vitamin D a day is what we all require to satisfy our bodies’ requirement.
Infants who received 2000 IU of vitamin D daily during their first year of life were found 31 years later to have reduced their risk of developing type I diabetes by 88%.(23) Infants born above 35° N and who live above this latitude for the first 10 years of life have 100% increased risk of developing multiple sclerosis for the rest of their life. (24) Women who had the highest intake of vitamin D reduced their risk of developing multiple sclerosis by 41%.(25) Women who had the highest intake of vitamin D were also found to reduce their risk of developing rheumatoid arthritis by 44%.(26)
It has been recognized for more than 20 years that living at higher latitudes increases risk of developing and dying of a variety of cancers including colorectal cancer, breast cancer, prostate cancer and pancreatic cancer.(27,28) Women who had the most sun exposure as teenagers and young adults reduce their risk of developing breast cancer later in life by 50-60%.(29) Women who had the highest intake of vitamin D reduce their risk of developing breast cancer by 50%.(30) Postmenopausal women who took 1100 IU of vitamin D3 a day for four years reduce their risk of developing all cancers by 60%.(31)
It is well documented over 100 years ago that vitamin D deficiency in children markedly increased their risk for upper respiratory tract infections.(1) There have been several studies reporting that vitamin D deficiency is associated with increased risk for upper respiratory tract infections, wheezing disorders as well as asthma in children. (32) Japanese schoolchildren who took 1200 IU of vitamin D a day from December through March reduced their risk of developing influenza infection by almost 50%.(33)
It has been estimated that upwards of 50 million teenage boys and girls are at risk for vitamin D deficiency or insufficiency. They have a 2.4 fold higher risk for developing high blood pressure, 2.5 fold higher risk for having elevated blood sugar and a fourfold increased risk for having pre-type II diabetes (metabolic syndrome). (34,35)
Vitamin D deficiency has also been associated with a 33% increased risk of developing type II diabetes in men and women. (36) Vitamin D deficiency is associated with increased risk for hypertension. Men and women who were vitamin D deficient had a 50% increased risk for having a myocardial infarction (37) and those who had a myocardial infarction and were vitamin D deficient had 100% increased risk of dying from their heart attack.(38)
Definition and Causes of Vitamin D Deficiency and Insufficiency
Based on provocative testing and other clinically relevant data vitamin D deficiency has been defined as a 25(OH)D < 20 ng/ml.(3,39) However to maximize intestinal calcium absorption in women and to have all of the other health benefits of vitamin D it has been recommended that children and adults should have a blood level of 25(OH)D > 30ng/ml.(40) Therefore vitamin D insufficiency has been defined as a 25(OH)D of 21-29 ng/ml.(3)(Fig 1)
The major cause for vitamin D deficiency globally is a lack of appreciation that sun induced vitamin D synthesis was the major source of vitamin D for most children and adults with the exception of peoples living far north and south of the equator. These people quickly realized that eating fatty fish, blubber from seals and liver from polar bears was essential for overall health and well-being. They are excellent dietary sources for vitamin D.
The message that you should never be exposed to direct sunlight has caused the vitamin D deficiency pandemic.(41) In the skin cancer capital of the world, Australia, the slip, slap, slop has caused widespread vitamin D deficiency. 87% of dermatologists in Australia were found to be vitamin D deficient at the end of the summer. (42) People who always wear sunscreen before going outdoors place themselves at high risk for vitamin D deficiency since a sun protection factor of 30 used properly reduces vitamin D3 synthesis in the skin by more than 95%.(8) People of color including both Hispanics and blacks are at much higher risk for vitamin D deficiency because not only do they avoid sun exposure so as not to enhance the color of their skin but often put a sunscreen on before going outdoors. Their skin pigment often gives them a sun protection factor of at least 8 thereby reducing their efficiency to make vitamin D3 in their skin by 50 to 90%. When African-American men and women were exposed to simulated sunlight they were unable to raise their blood levels of vitamin D3 whereas white adults who received the same amount of simulated sunlight raised their blood levels of vitamin D3 by almost 50 fold. (7) African American adults required 5-10 times longer exposure and they only raised their blood levels by about 10-20 fold.
Obesity is associated with vitamin D deficiency. Vitamin D is fat soluble and is therefore efficiently sequestered in the body fat making it difficult to return into the circulation.(43) This is the reason why men and women with a BMI greater than 30 require at least 2-5 fold increase in their vitamin D requirement. (3)
Patients with a variety of fat malabsorption syndromes including inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, cystic fibrosis and patients who have had gastric bypass surgery are unable to efficiently absorb vitamin D and often require much higher doses to satisfy their vitamin D requirement.(3) A silent cause for vitamin D deficiency due to intestinal malabsorptioin is caused by celiac disease. Often this disease is diagnosed when it is realized that a patient who is vitamin D deficient does not respond appropriately to vitamin d therapy and thus has a malabsorption problem.
Prevention and Treatment for Vitamin D Deficiency
It has been assumed that drinking a couple of glasses of milk each containing 100 IU of vitamin D along with a multivitamin and a balanced diet was more than adequate to satisfy a child’s and adult’s vitamin D requirement. However it is now realized that for adults and probably also for children greater than one year of age that for every 100 IU of vitamin D ingested the blood level of 25(OH)D increases by approximately 0.6-1 ng/ml.(10,44) When healthy adults in Boston at the end of the winter received 1000 IU of vitamin D2 or vitamin D3 daily for three months they raised their blood level of 25(OH)D by approximately 10 ng/ml.(Fig 3)(10) The white men and women had an average 25(OH)D of 18 ng/ml and the black men and women had on average a 25(OH)D of 15 ng/ml. Thus 1000 IU of vitamin D3 a day raised the blood level of the white men and women to 28 ng/ml and the black men and women to 25 ng/ml. Therefore based on this and other studies it is clear that 1000 IU of vitamin D a day in the winter without any contribution of vitamin D from the sun was unable to raise and sustain a blood level of 25(OH)D above 30 ng/ml.
Figure 3.
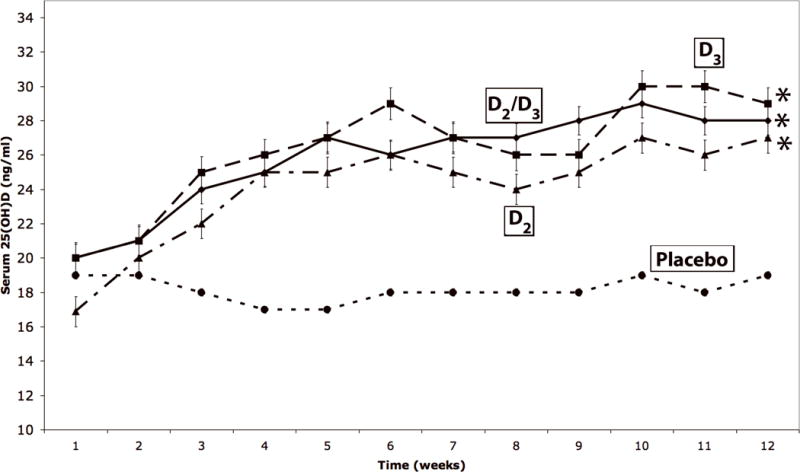
Mean (± SEM) serum 25-hydroxyvitamin D levels after oral administration of vitamin D2 and/or vitamin D3. Healthy adults recruited at the end of the winter received either placebo [(n = 14; 1,000 IU of vitamin D3 [D3, n = 20; (-■-)], 1,000 IU of vitamin D2 [D2, n = 16; (-▲-)] or 500 IU of vitamin D2 and 500 IU of vitamin D3 [D2 and D3, n = 18; (-□-)] daily for 11 weeks. The total 25-hydroxyvitamin D levels are demonstrated over time. *P = 0.027 comparing 25(OH)D over time between vitamin D3 and placebo. **P=0.041 comparing 25(OH)D over time between 500 IU vitamin D3 + 500 IU vitamin D2 and placebo. ***P=0.023 comparing 25(OH)D over time between vitamin D2 and placebo. Reproduced with permission (10)
Pre-pubertal and teenage girls who received 2000 IU of vitamin D3 a day for one year were able to raise their blood levels of 25(OH)D above 30 ng/ml and were found to have better bone density and improved muscle function compared to girls who received only 400 IU of vitamin D a day for the same period of time. (16)
When an adult in a bathing suit (woman in a bikini type bathing suit) has their whole body exposed to a tanning bed that was equivalent to being exposed to sunlight that caused a light pinkness to their skin 24 hours later (defined as one minimal erythemal dose) raised their blood level of vitamin D similar to the adult taking approximately 15,000-20,000 IU of vitamin D as a single dose.(Fig 4) Vitamin D made in the skin has at least 2-3 times longer in the circulaton when compared to ingesting vitamin D.(Fig 4)(45) Therefore the body has a large capacity to make vitamin D with minimum sun exposure. This is the reason for the recommendation that exposure to arms and legs (which is approximately 20-25% of the body surface when wearing shorts and a short sleeve shirt or blouse) to about 5-15 minutes three times a week (of course depending on time of day, season of the year, latitude and degree of skin pigmentation) between the hours of 10 AM and 3 PM for white adults during the spring, summer and fall can help provide them with their vitamin D requirement. As can be seen in figure 5, sensible exposure to ultraviolet radiation (similar to sunlight) is very effective in raising blood levels of 25(OH)D into a healthy range above 30 ng/ml and is more effective than ingesting 1000 IU of vitamin D a day. I recommend that since one cannot always depend on sun exposure because of work habits, concerns about the damaging effects from sunlight etc. that healthy adults should take a supplement containing 2000 IU of vitamin D a day along with ingesting a multivitamin containing 400 IU of vitamin D and three servings of dairy or other vitamin D fortified foods for a total of 3000 IU of vitamin D a day. Men and women who took an equivalent of 3000 IU of vitamin D a day for up to six years were able to maintain a blood level of 25-hydroxyvitamin D on average of between 40-60 ng/ml. (Fig 6)(46)
Figure 4.
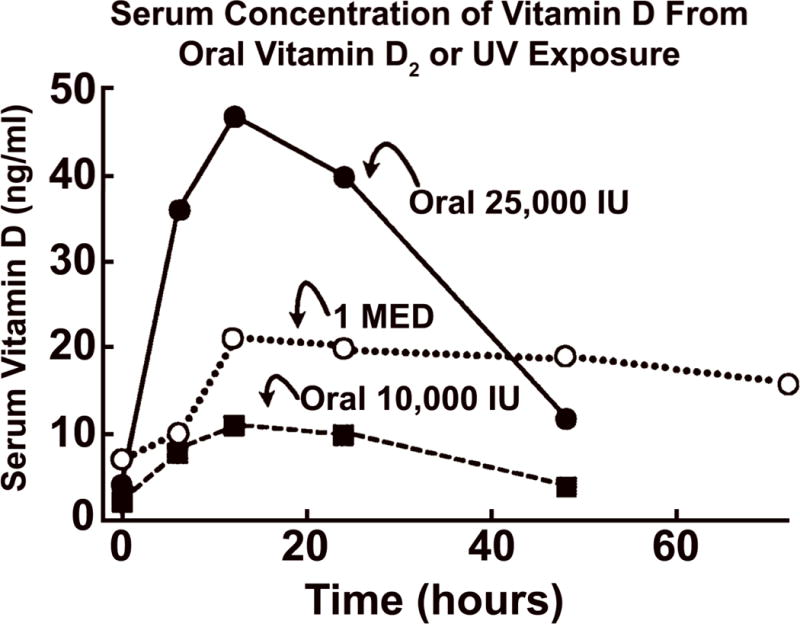
Comparison of serum vitamin D3 levels after a whole-body exposure (in a bathing suit; bikini for women) to 1 MED (minimal erythemal dose) of simulated sunlight compared with a single oral dose of either 10,000 or 25,000 IU of vitamin D2. Reproduced with permission from Holick copyright 2004
Figure 5.
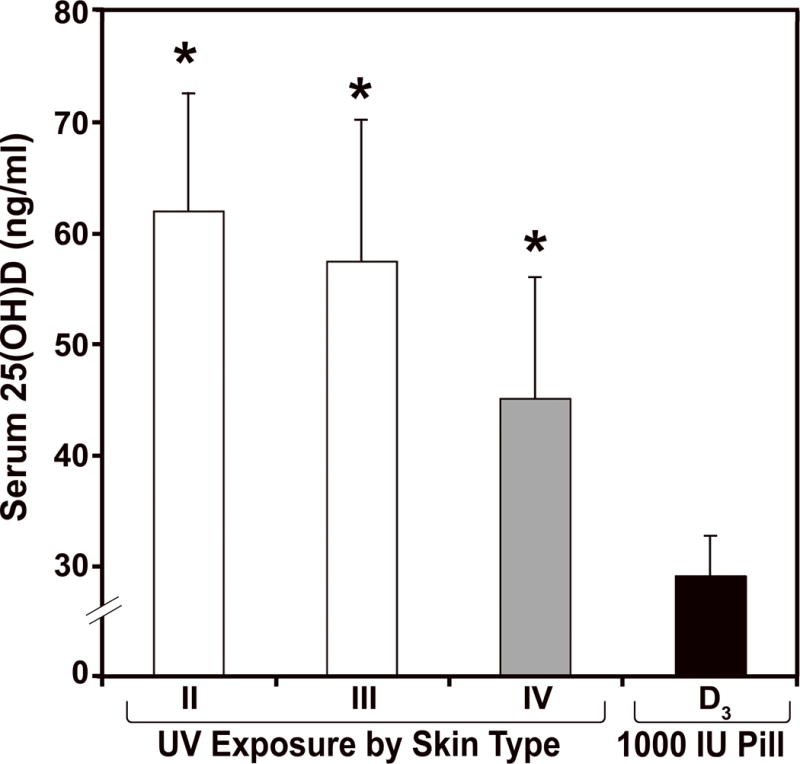
The serum 25-hydroxyvitamin D levels in healthy adults with skin types II, III, and IV exposed to 0.75 MEDs of simulated sunlight in a bathing suit 3 times a week for 12 weeks compared to healthy adults receiving a daily dose of 1000 IU of vitamin D3 daily for 12 weeks *p < 0.01. Copyright Holick 2010; reproduced with permission.
Figure 6.
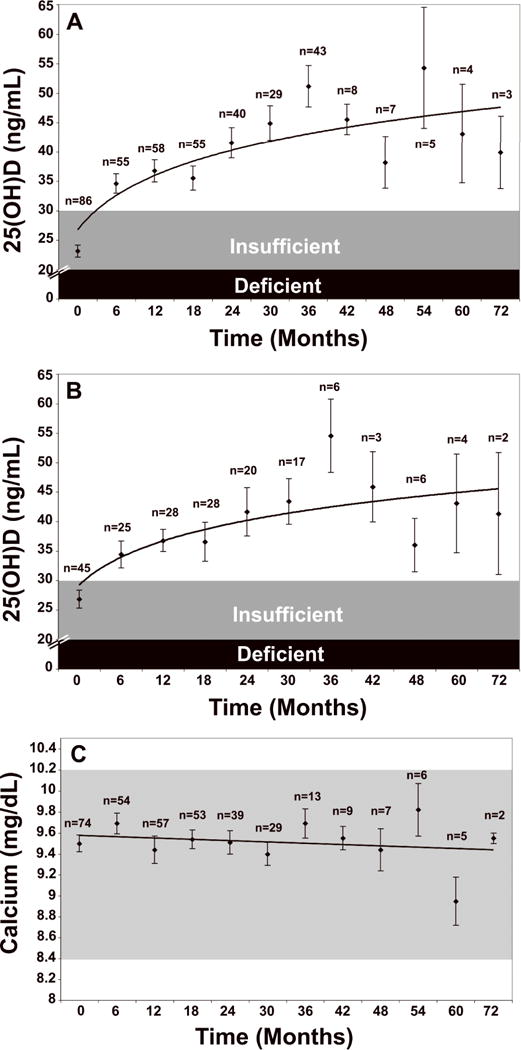
A. Mean serum 25-hydroxyvitamin D [25(OH)D] levels in all patients: Includes patients treated with 50,000 IU vitamin D2 every 2 weeks (maintenance therapy, N=81), including those patients with vitamin D insufficiency who were initially treated with 8 weeks of 50,000 IU vitamin D2 weekly prior to maintenance therapy (N=39). Error bars represent standard error of the mean, mean result over 5 years shown. Time 0 is initiation of treatment, results shown as mean values averaged for 6 month intervals. When mean 25(OH)D in each 6 month group was compared to mean initial 25(OH)D, p < 0.001 up until month 43; p < 0.001 when all remaining values after month 43 were compared to mean initial 25(OH)D. Pietras et al; reproduced with permission.(46)
Children from the day they are born should take at least 400 IU of vitamin D a day as recommended by the American Academy of Pediatrics. (22) However based on a variety of studies 1000 IU of vitamin D a day total from supplements and diet may be more beneficial for infants and children. (22) However based on a variety of studies 1000 IU of vitamin D a day total from supplements and diet may be more beneficial for infants and children.(3,5) Teenagers, like adults, should take a 2000 IU supplement a day if they are not active outside and getting adequate sensible sun exposure to produce an adequate amount of vitamin D. Children and adults of color cannot depend on sun exposure for their vitamin D requirement unless they are outside for prolonged periods of time either due to outdoor activities or an outdoor occupation. Therefore children should take at least 1000 IU of vitamin D a day and black teenagers and adults 2000 IU of vitamin D a day. If they are obese they may need 2-5 times more vitamin D to satisfy their requirement.(Table 2)
TABLE 2.
| IOM Recommendations | Dr. Holick’s Recommendations for Patients at Risk for Vitamin D Deficiency | |||||
|---|---|---|---|---|---|---|
| Life Stage Group | AI | EAR | RDA | UL | Daily Allowance (IU/d) | UL (IU) |
| Infants | ||||||
| 0 to 6 mo | 400 IU (10 μg) | --- | --- | 1,000 IU (25 μg) | 400 – 1,000 | 2,000 |
| 6 to 12 mo | 400 IU (10 μg) | --- | --- | 1,500 IU (38 μg) | 400 – 1,000 | 2,000 |
| Children | ||||||
| 1–3 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 2,500 IU (63 μg) | 600 – 1,000 | 4,000 |
| 4–8 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 3,000 IU (75 μg) | 600 – 1,000 | 4,000 |
| Males | ||||||
| 9–13 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 4,000 |
| 14–18 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 4,000 |
| 19–30 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 31–50 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 51–70 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| > 70 y | --- | 400 IU (10 μg) | 800 IU (20 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| Females | ||||||
| 9–13 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 4,000 |
| 14–18 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 4,000 |
| 19–30 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 31–50 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 51–70 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| > 70 y | --- | 400 IU (10 μg) | 800 IU (20 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| Pregnancy | ||||||
| 14–18 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 19–30 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 31–50 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| Lactation* | ||||||
| 14–18 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 19–30 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
| 31–50 y | --- | 400 IU (10 μg) | 600 IU (15 μg) | 4,000 IU (100 μg) | 1,500 – 2,000 | 10,000 |
Recommended Adequate Intakes (AI), Estimated Average Requirement (EAR), Recommended Dietary Allowance (RDA) and Tolerable Upper Limit (UL) by the Institute of Medicine (IOM) and Dr. Holick’s recommendation for Daily Allowance and safe Upper Limit (UL) for vitamin D for children and adults who are not obtaining adequate vitamin D from sun exposure and who are at risk for vitamin D deficiency.
To effectively treat vitamin D deficiency quickly it is wise to fill up the vitamin D tank which is on empty. To accomplish this I give 50,000 IU of vitamin D2 once a week for eight weeks which is equivalent to taking 6000 IU of vitamin D a day.(46) A similar strategy is also effective in children.(47) After treating the vitamin D deficiency to prevent recurrence I give my patients 50,000 IU of vitamin D2 once every two weeks thereafter which is equivalent to 3000 IU/d. Six years on this therapy is effective in maintaining blood levels of 25(OH)D above 30 ng/ml with no observed toxicity.(46)(Fig 6)
Utility of the 25-Hydroxyvitamin D Assays
There are several assays that are used commercially to measure 25(OH)D which is the gold standard for determining a patient’s vitamin D status. The antibody-based assays are able to measure the total 25(OH)D and the liquid chromatography tandem mass spectroscopy (LCMSMS) assay separates 25(OH)D2 from 25(OH)D3. Therefore the antibody-based assay provides the total blood level of 25(OH)D which is used to determine a persons vitamin D status. The LCMSMS assay not only provides the total 25(OH)D but also the individual blood levels of 25(OH)D2 and 25(OH)D3. Since there is very little vitamin D2 in the diet, most children and adults have essentially 100% of their total 25(OH)D as 25(OH)D3. Therefore patients who are being treated for vitamin D deficiency with vitamin D2 the advantage of having a follow-up blood sample sent for an LCMSMS assay is that there should be a significant increase in the serum 25(OH)D2. The serum 25(OH)D3 would be reflective of sun exposure which produces vitamin D3 in the skin and the ingestion of a vitamin D supplement that contains vitamin D3. If there is no significant increase in the 25(OH)D2 in patients who are being treated with vitamin D2 then either the patient is not compliant or is malabsorbing the vitamin. If there is a small increase in the serum 25(OH)D2 then I usually recommend increasing the frequency of taking the vitamin D2. An alternative is to cut the capsule in half and add it to a small amount of milk swirl it and then drink it since that some patients are unable to digest the gelatin capsule or are allergic to the gelatin and glycerin components of the capsule.
Conclusion
Recently The Institute of Medicine (IOM) recommended a significant increase in vitamin D intake of up to three fold for older children and adults. (48) They also recognize that vitamin D is less toxic than once thought and therefore increased the tolerable upper limit (UL) for children and adults. (Table 2) However there were several recent studies that have suggested that higher intakes for children and adults may have some additional nonskeletal health benefits.(31,33,34, 35,37,49,50)
There is no downside to increasing either a child’s or adult’s vitamin D intake to what is recommended in table 2. The only time that you should be concerned about taking the amount of vitamin D recommended in table 2 is if you are suffering from a chronic granulomatous disorder such as sarcoidosis. (5) These patients still need some vitamin D but usually only enough to raise their blood level of 25(OH)D to between 20-30 ng/ml to avoid causing hypercalcemia and hypercalciuria. Children and women of all ages should be particularly concerned about their vitamin D status. Vitamin D deficiency will result in growth retardation and inadequate bone mineralization especially for teenage girls during their growth spurt. Women of childbearing age should also be vigilant about their vitamin D status since it can improve pregnancy outcomes and improve the health of their developing infant. Young and middle-aged adults benefit from increasing their vitamin D status from sensible sun exposure and vitamin D supplementation by decreasing their risk for autoimmune diseases, deadly cancers including prostate, colon and breast cancer, type II diabetes, heart disease, cognitive dysfunction and infectious disease.(Fig 2) Children need an adequate supply of vitamin D in order to reduce their risk for developing asthma, wheezing disorders and upper respiratory tract infections including influenza infection. It may also reduce their risk for developing many of the chronic diseases that have now been associated with vitamin D deficiency.(Fig 7)
Figure 7.
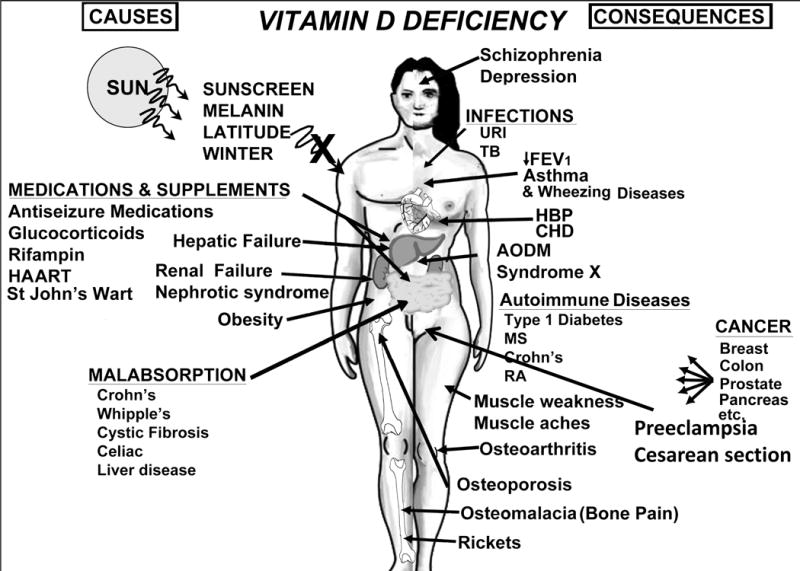
A Schematic Representation of the Major Causes for Vitamin D Deficiency and Potential Health Consequences. Holick copyright 2010. Reproduced with permission.
Not only has the sun been demonized for more than 40 years unchallenged (41) which is the major cause for the vitamin D deficiency epidemic but it has also been accepted by the medical community and lay public that fat-soluble vitamin D is potentially highly toxic. Vitamin D can cause intoxication which is associated with a high blood calcium causing calcification of blood vessels and the kidneys that can lead to death.(3) However vitamin D intoxication is one of the rarest medical conditions.(52,55) The reason is that adults can take up to 10,000 IU of vitamin D a day for at least five months without any untoward toxicity.(44) It is caused by inadvertent or intentional ingestion of excessively high amounts of vitamin D. This is usually in the range of 50,000 IU of vitamin D a day for several months. We reported an adult who took on average 1 million IU of vitamin D3 a day that he had purchased on the internet. His calcium was over 15 mg percent and his 25(OH)D was greater than 500 ng/ml.(54) Therefore a blood level of 25(OH)D up to 100 ng/ml is considered to be safe. Usually blood levels of 25(OH)D above 200 ng/ml have been associated with vitamin D intoxication resulting in hypercalcemia, hyperphosphatemia, nephrocalcinosis and soft tissue calcification. It should be noted that even excessive exposure to sunlight will not cause vitamin D intoxication because any excess vitamin D is destroyed by the sun.(13)
Acknowledgments
This work was supported in part by the UV Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. 2006;116(8):2062–2072. doi: 10.1172/JCI29449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lalueza-Fox C, Rompler H, Caramelli D, et al. 1 Receptor Allele Suggests Varying Pigmentation Among Neanderthals. Science. 2007;38:1453. doi: 10.1126/science.1147417. [DOI] [PubMed] [Google Scholar]
- 3.Holick MF. Vitamin D Deficiency. N Eng J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 4.Holick MF, Chen TC, Sauter ER. Vitamin D and Skin Physiology: A D-Lightful Story. J Bone Miner Res. 2007;22(S2):V28–V33. doi: 10.1359/jbmr.07s211. [DOI] [PubMed] [Google Scholar]
- 5.Holick MF. Vitamin D and Health: Evolution, Biologic Functions, and Recommended Dietary Intakes for Vitamin D. Clin Rev Bone Miner Metab. 2009;7(1):2–19. [Google Scholar]
- 6.Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373–378. doi: 10.1210/jcem-67-2-373. [DOI] [PubMed] [Google Scholar]
- 7.Clemens TL, Henderson SL, Adams JS, et al. Increased skin pigment reduces the capacity of skin to synthesis vitamin D3. Lancet. 1982;1(8263):74–76. doi: 10.1016/s0140-6736(82)90214-8. [DOI] [PubMed] [Google Scholar]
- 8.Matsuoka LY, Ide L, Wortsman J, MacLaughlin J, et al. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64:1165–1168. doi: 10.1210/jcem-64-6-1165. [DOI] [PubMed] [Google Scholar]
- 9.Holick MF, Matsuoka LY, Wortsman J. Age, Vitamin D, and solar ultraviolet. Lancet. 1989:1104–110. doi: 10.1016/s0140-6736(89)91124-0. [DOI] [PubMed] [Google Scholar]
- 10.Holick MF, Biancuzzo RM, Chen TC, et al. Vitamin D2 is as effective as vitamin D3 in maintaining circulating concentrations of 25-hydroxyvitamin D. J Clin Endocrinol Metab. 2008;93(3):677–681. doi: 10.1210/jc.2007-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 12.Holick MF. Case 3-2009: A 9-Month-Old Boy with Seizures. New Eng J Med CPC. 2009;360(4):398–1407. doi: 10.1056/NEJMcpc0807821. [DOI] [PubMed] [Google Scholar]
- 13.Hollis BW, Wagner CL. Assessment of dietary vitamin D requirements during pregnancy and lactation. Am J Clin Nut. 2004;79:717–726. doi: 10.1093/ajcn/79.5.717. [DOI] [PubMed] [Google Scholar]
- 14.Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003;78:1463–1470. doi: 10.4065/78.12.1463. [DOI] [PubMed] [Google Scholar]
- 15.Gloth FM, III, Lindsay JM, Zelesnick LB, et al. Can vitamin D deficiency produce an unusual pain syndrome? Arch Intern Med. 1991;151:1662–1664. [PubMed] [Google Scholar]
- 16.El-Hajj Fuleihan Ghada, Mona Nabulsi, Hala Tamim, et al. Effect of Vitamin D Replacement on Musculoskeletal Parameters in School Children: A Randomized Controlled Trial J. Clin Endocrinol Metab. 2006;91:405–412. doi: 10.1210/jc.2005-1436. [DOI] [PubMed] [Google Scholar]
- 17.Bischoff-Ferrari, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692. doi: 10.1136/bmj.b3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broe KE, Chen TC, Weinberg J, et al. A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. J Am Geriatr Soc. 2007;55(2):234–39. doi: 10.1111/j.1532-5415.2007.01048.x. [DOI] [PubMed] [Google Scholar]
- 19.Lee JM, Smith JR, Philipp BL, et al. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin Pediatr. 2007;46:42–44. doi: 10.1177/0009922806289311. [DOI] [PubMed] [Google Scholar]
- 20.Bodnar LM, Catov JM, Simhan HN, et al. Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92(9):3517–22. doi: 10.1210/jc.2007-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merewood A, Mehta SD, Chen TC, et al. Association between vitamin D deficiency and Primary Cesarean Section. J Clin Endocrinol Metab. 2009;94(3):940–5. doi: 10.1210/jc.2008-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner CL, Greer FR, The Section on Breastfeeeding and Committee on Nutrition Prevention of Rickets and Vitamin D Deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142–1152. doi: 10.1542/peds.2008-1862. [DOI] [PubMed] [Google Scholar]
- 23.Hypponen E, Laara E, Jarvelin M-R, et al. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001;358:1500–1503. doi: 10.1016/S0140-6736(01)06580-1. [DOI] [PubMed] [Google Scholar]
- 24.Ponsonby A-L, McMichael A, van der Mei I. Ultraviolet radiation and autoimmune disease: insights from epidemiological research. Toxicology. 2002;181–182:71–78. doi: 10.1016/s0300-483x(02)00257-3. [DOI] [PubMed] [Google Scholar]
- 25.Munger KL, Levin LI, Hollis BW, et al. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA. 2006;296:2832–2838. doi: 10.1001/jama.296.23.2832. [DOI] [PubMed] [Google Scholar]
- 26.Merlino LA, Curtis J, Mikuls TR, et al. Iowa Women’s Health Study. Vitamin D intake is inversely associated with rheumatoid arthritis. Arthritis Rheum. 2004;50(1):72–77. doi: 10.1002/art.11434. [DOI] [PubMed] [Google Scholar]
- 27.Garland CF, Garland FC, Gorham ED, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006;96(2):252–61. doi: 10.2105/AJPH.2004.045260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grant WB. Lower vitamin-D production from solar ultraviolet-B Irradiance may explain some differences in cancer survival rates. Journal of the National Medical Association. 2006;98(3):357–64. [PMC free article] [PubMed] [Google Scholar]
- 29.Knight JA, Lesosky M, Barnett H, et al. Vitamin D and reduced risk of breast cancer: a population-based case-control study. Cancer Epidemiol Biomarkers Prev. 2007;16(3):422–499. doi: 10.1158/1055-9965.EPI-06-0865. [DOI] [PubMed] [Google Scholar]
- 30.Garland CF, Gorham ED, Mohr SB, et al. Vitamin D and prevention of breast cancer: Pooled analysis. J Steroid Biochem Mol Biol. 2007;103(3–5):708–11. doi: 10.1016/j.jsbmb.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Lappe JM, Travers-Gustafson D, Davies KM, et al. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85(6):1586–1591. doi: 10.1093/ajcn/85.6.1586. [DOI] [PubMed] [Google Scholar]
- 32.Ginde AA, Mansbach JM, Camargo CA. Association Between Serum 25-Hydroxyvitamin D Level and Upper Respiratory Tract Infection in The Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009;169(4):384–390. doi: 10.1001/archinternmed.2008.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Urashima M, Segawa T, Okazaki M, et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91:1255–60. doi: 10.3945/ajcn.2009.29094. [DOI] [PubMed] [Google Scholar]
- 34.Mansbach JM, Ginde AA, Camargo CA. Serun 25-Hydroxyvitamin D Levels Among US Children Aged 1 to 11 Years: Do Children Need More Vitamin D? Pediatrics. 2009;124:1404–1410. doi: 10.1542/peds.2008-2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Melamed ML, Muntner P, Michos ED, et al. Serum 25-hydroxyvitamin D levels and the prevalence of peripheral arerial disease: results from NHANES 2001 to 2004. Arterioscler Thromb Vasc Biol. 2008;28(6):1179–85. doi: 10.1161/ATVBAHA.108.165886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pittas AG, Dawson-Hughes B, Li T, et al. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care. 2006;29(3):650–56. doi: 10.2337/diacare.29.03.06.dc05-1961. [DOI] [PubMed] [Google Scholar]
- 37.Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167(16):1730–7. doi: 10.1001/archinte.167.16.1730. [DOI] [PubMed] [Google Scholar]
- 39.Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805–806. doi: 10.1016/s0140-6736(05)78933-9. [DOI] [PubMed] [Google Scholar]
- 40.Heaney RP, Dowell MS, Hale CA, et al. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22(2):142–146. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- 41.Wolpowitz D, Gilchrest BA. The vitamin D questions: how much do you need and how should you get it? J Am Acad Dermatol. 2006;54:301–317. doi: 10.1016/j.jaad.2005.11.1057. [DOI] [PubMed] [Google Scholar]
- 42.Czarnecki D, Meehan CJ, Bruce F. The vitamin D status of Australian dermatologists. Clin and Experimen Derm. 2009;34:621–638. doi: 10.1111/j.1365-2230.2008.03002.x. [DOI] [PubMed] [Google Scholar]
- 43.Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72:690–693. doi: 10.1093/ajcn/72.3.690. [DOI] [PubMed] [Google Scholar]
- 44.Heaney RP, Davies KM, Chen TC, et al. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77:204–210. doi: 10.1093/ajcn/77.1.204. [DOI] [PubMed] [Google Scholar]
- 45.Haddad JG, Matsuoka LY, Hollis BW, et al. Human plasma transport of vitamin D after its endogenous synthesis. J Clin Invest. 1993;91:2552–2555. doi: 10.1172/JCI116492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pietras SM, Holick MF. Vitamin D Supplementation. Comments and Opinions. Arch Intern Med. 2010;170(6):572–573. doi: 10.1001/archinternmed.2010.44. [DOI] [PubMed] [Google Scholar]
- 47.Gordon CM, Williams AL, Feldman HA, et al. Treatment of hypovitaminosis D in infants and toddlers. J Clin Endocrinol Metab. 2008;93(7):2716–21. doi: 10.1210/jc.2007-2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.IOM (Institute of Medicine) Dietary Reference Intakes for Calcium and Vitamin D. Washington DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 49.Holick MF. Health benefits of vitamin D and sunlight: a D-bate. Nat Rev Endocrinol. 2011;7:73–85. doi: 10.1038/nrendo.2010.234. [DOI] [PubMed] [Google Scholar]
- 50.Dong Y, Stallmann-Jorgenson IS, Pollock NK, Harris RA, Keeton D, Huang Y, Bassali R, Gao D, Thomas J, Pierce GL, White J, Holick MF, Zhu H. A 16-week randomized clinical trial of 2,000 IU daily vitamin D3 supplementation in black youth: 25-hydroxyvitamin D, adiposity, and arterial stiffness. J Clin Endocrinol Metab. 2010;95(10):4584–4591. doi: 10.1210/jc.2010-0606. [DOI] [PubMed] [Google Scholar]
- 51.Demetriou ETW, Pietras SM, Holick MF. Hypercalcemia and Soft Tissue Calcification Owing to Sarcoidosis: The Sunlight-Cola Connection. J Bone Miner Res. 2010;25(7):1695–1699. doi: 10.1002/jbmr.51. [DOI] [PubMed] [Google Scholar]
- 52.Vieth R, Chan PCR, MacFarlane GD. Efficacy and safety of vitamin D3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr. 2001;73:288–294. doi: 10.1093/ajcn/73.2.288. [DOI] [PubMed] [Google Scholar]
- 53.Koutkia P, Chen TC, Holick MF. Vitamin D Intoxication Associated with an Over-the-Counter Supplement. N Engl J Med. 2001;345(1):66–67. doi: 10.1056/NEJM200107053450115. [DOI] [PubMed] [Google Scholar]


