Abstract
OBJECTIVE
To determine if children born prematurely exhibit atypical responses to normally occurring sensory stimuli, as measured by the Sensory Profile.
STUDY DESIGN
This is a cross-sectional study of children born at ≤32 weeks gestation, followed at 1 to 8 years of age. The Sensory Profile questionnaire was completed by each child’s primary caregiver. The overall Sensory Profile was considered atypical if any quadrant or section score was >2 s.d. from the mean of the Sensory Profile validation group. Bivariate analyses were performed to determine associations between risk factors for adverse neurodevelopment and overall atypical Sensory Profiles. A section or quadrant was considered atypical if its score was >2 s.d. from the mean. A test of proportions was used to compute observed versus expected scores for each section and quadrant (Sensory Profile scores were based on a normal distribution so one would expect approximately 95% of participants to score within 2 s.d. of the mean).
RESULT
Of our 107 participants, 39% had an atypical score in at least one section or quadrant. No specific perinatal or neonatal risk factors were associated with atypical overall Sensory Profiles (P≥0.05 for all). Children born prematurely were at risk of having atypical scores in the auditory, tactile and vestibular processing sections, and in the four Sensory Profile quadrants (P<0.05).
CONCLUSION
Children born prematurely exhibit atypical sensory behaviors on the Sensory Profile. Further investigation to understand the underlying neural mechanisms and to develop effective interventions are critical to support neurodevelopment for these children.
Keywords: Sensory Profile, prematurity, sensory behavior, follow-up
INTRODUCTION
For years, parents, teachers and health-care providers have noted that children born prematurely exhibit atypical sensory behaviors to normally occurring sensory stimuli. The sensory differences described in this population extend beyond the well-characterized vision and hearing deficits to problems involving unimodal sensory processing and multimodal sensory integration.
An interesting corollary is that children born prematurely are also more likely than their term counterparts to score positively on autism screening tests like the Modified Checklist for Autism in Toddlers (M-CHAT) and the Social Communication Questionnaire.1,2 Children born prematurely have positive screening rates of 16 to 26%, as compared with children born at term, who have positive screening rates of 3 to 5%.1–4 Using gold standard diagnostic techniques, the incidence of autism in children born prematurely is closer to 5%, which is lower than the screening rates, but significantly higher than the incidence of autism in the general population (1%).5,6
This finding raises the important question of why so many children born prematurely are demonstrating features commonly seen in children with the classic autism phenotype. Problems with basic sensory processing have been increasingly implicated in autism, with 90% of autistic children exhibiting sensory abnormalities.7 It is possible that brain injury and neurodevelopmental impairments related to prematurity may also impact basic sensory processing.8 As most autism screening tests evaluate sensory sensitivities (e.g., the M-CHAT question, ‘does your child seem oversensitive to noise?’),9 it is conceivable that the high rate of positive autism screening in children born prematurely reflects, in part, the sensory processing abnormalities seen in this population.10
Although atypical sensory behaviors are often described in children born prematurely, limited data exist that quantitatively measure this finding. One instrument that can be used to assess sensory behaviors is the Sensory Profile questionnaire.11,12 The Sensory Profile is a validated caregiver-completed questionnaire that assesses a child’s responses to common sensory experiences. The profile has been shown to discriminate 90% of children with autism, other pervasive developmental disorders, and attention deficit and hyperactivity disorder from controls.13 However, no published studies to date have reported Sensory Profile results in premature infants (≤32 weeks gestation).
To test the hypothesis that infants born prematurely exhibit atypical sensory behaviors, we performed a cross-sectional study assessing children born at ≤32 weeks, at 1 to 8 years of age, with the Sensory Profile.
METHODS
Study design and participants
This is a cross-sectional study of sensory processing behaviors in children born prematurely. Inclusion criteria included gestational age ≤32 weeks at delivery, participation in the University of California, San Francisco Intensive Care Nursery Follow-Up Program, age at examination of 1 to 8 years and caregiver completion of the Sensory Profile between 1 June 2009 and 31 December 2011. Parental consent was obtained for the use of the participants’ data. This project was approved by the University of California San Francisco’s Institutional Review Board.
Sensory Profile
The Sensory Profile is a caregiver-completed questionnaire designed by Winnie Dunn, PhD, OTR, FAOTA. It assesses a child’s behavioral responses to normally occurring sensory stimuli.11,12 Two versions of the Sensory Profile exist for children: an infant/toddler version (for ages birth to 3 years) and a standard version (for ages 3 to 10 years). The Sensory Profile provides scores in ‘sections’ and ‘quadrants.’ The sections common to both the infant/toddler and the standard versions are: auditory processing, visual processing, tactile processing, vestibular processing and oral sensory processing. In addition, both versions provide scores for four quadrants: low registration, sensory seeking, sensory sensitivity and sensory avoiding.
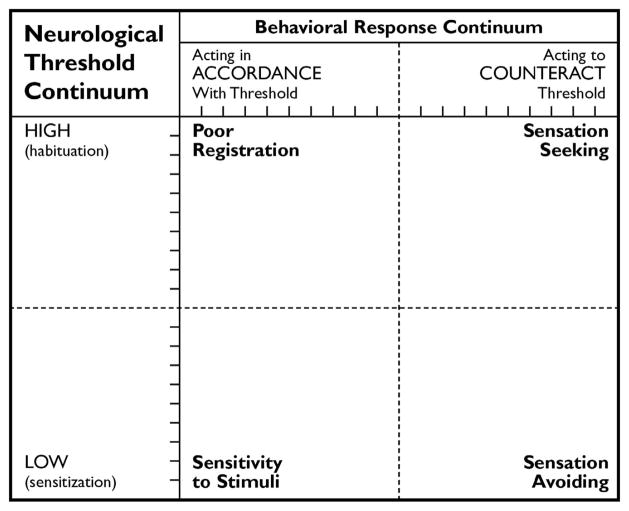
The Sensory Profile quadrants are graphically depicted in Figure 1. Theoretically, infants with abnormal scores in the low registration and sensation seeking quadrants require a large amount of sensory input to process stimuli. However, the behavioral responses of children with abnormal scores in these quadrants differ; those with abnormal low registration scores respond passively (for example, require loud speech or touch to gain attention), whereas those with abnormal sensory seeking scores respond actively (for example, make extra sounds with toys, in order to increase sensory input). Children with abnormal scores in the sensory sensitivity and sensation avoiding quadrants are easily bothered by stimuli. The behavioral responses of children with abnormal scores in these quadrants again differ; those with abnormal sensory sensitivity scores respond passively (for example, are distracted and/or have difficultly eating when in a noisy environment), and those with abnormal sensation avoiding scores take an active approach (for example, resist being held, in order to decrease sensory input).
Figure 1.
Sensory Profile quadrants: relationship between neurologic thresholds and behavioral responses. Sensory Profile.
*Note that ‘poor registration’ in this figure corresponds with the low registration quadrant. ‘sensitivity to stimuli’ in this figure corresponds with the sensory sensitivity quadrant. Copyright 1999 NCS Pearson. Reproduced with permission. All rights reserved.12 ‘Sensory Profile’ is a trademark, in the United States and/or other countries, of Pearson Education or its affiliate(s).
The Sensory Profile classifies children as having typical performance, probable differences from typical (1 s.d. from the mean of the Sensory Profile validation group),11,12 or definite differences from typical (2 s.d. from the mean of the validation group) in each section and quadrant, using predetermined score cutoffs. The score cutoffs, which were derived from validation studies on the Sensory Profile, follow a normal distribution.11,12
For this study, the Sensory Profile was universally distributed to parents of children who presented to the follow-up clinic (for their 12- to 18-month, 4- to 5-year or 8-year visits) between June 2009 and December 2011. Caregivers responded to questions describing their child’s typical behaviors in specified scenarios (for example, ‘my child seems unaware of wet or dirty diapers’) using a five-level Likert scale (always/almost always, frequently, occasionally, seldom and never/almost never). The infant/toddler version of the Sensory Profile was administered to parents of children aged 6 to 36 months, and the standard version of the Sensory Profile was administered to parents of children aged 3 to 10 years. Age was corrected for prematurity until 3 years.
We performed analyses on the overall Sensory Profile, each section and each quadrant. A child was determined to have an atypical overall Sensory Profile if any section or quadrant score was >2 s.d. from the expected mean, based on the validation group. A child was determined to have an atypical score in a specific section or quadrant if he or she scored >2 s.d. from the expected mean in that area. As per the Sensory Profile User’s Manual, if caregivers did not answer a specific question on the questionnaire, no score could be calculated for the section or quadrant that included that item.11,12 This occurred, for example, when questions were asked about behaviors related to television, and participants were not exposed to television. When this occurred, the section or quadrant containing that item was scored as missing, and the remaining scores were analyzed. The analysis of the overall Sensory Profile did not completely exclude participants with a missing section or quadrant score; instead, all available scores were included in order to fully utilize the data.
Risk factors
Perinatal and neonatal risk factors for abnormal neurodevelopment were extracted from the participants’ medical records by one investigator (ACW). The dichotomous variables examined were: pregnancy-induced hypertension, chorioamnionitis, necrotizing enterocolitis (defined as Bell’s classification ≥II, treated medically or surgically, and ‘spontaneous perforations’ occurring before 7 days of life), intraventricular hemorrhage (based on head ultrasound, ≤grade II versus ≥grade III), periventricular leukomalacia (based on head ultrasound, defined as persistent echogenicity progressing to cystic changes), chronic lung disease (persistent oxygen requirement at 36 weeks gestation) and retinopathy of prematurity requiring laser surgery. The continuous variables examined were: gestational age (weeks), birth weight (grams), maternal age (years) and maternal education (years of school completed).
The relationships between atypical overall Sensory Profiles and abnormal neurodevelopmental outcomes (that is, cognitive score <70 and/or cerebral palsy) were also analyzed. Cognitive scores were based on the cognitive test administered to the child at the time of the Sensory Profile (the Bayley test in children <42 months, the Wechsler Preschool and Primary Scale of Intelligence in children 3.5 to 6 years, and the Wechsler Intelligence Scale for Children in children >6 years). Neurologic examinations were performed by neonatologists, neurologists, or nurse practitioners trained in developmental and behavioral pediatrics. Cognitive testing was performed by nurse practitioners or psychiatrists trained in the proper administration of the tests.
Statistical analyses
As described above, the overall Sensory Profile was considered atypical if any section or quadrant was >2 s.d. from the mean of the validation group. To assess the association between atypical Sensory Profiles and commonly identified risk factors for abnormal neurodevelopment, we performed bivariate analyses using χ2 tests for categorical variables and t-tests for continuous variables. A P-value <0.05 was set as the level of statistical significance.
The section and quadrant scores of the participants were categorized as typical (within 2 s.d. of the mean of the validation group) and atypical (>2 s.d. from the mean of the validation group). As the Sensory Profile cutoff scores for each section and quadrant were created using a normal distribution, we were able to perform a test of proportions to compare the observed proportion of children with atypical scores to those expected in a normal population (based on the validation group). Based on a normal distribution, one would expect 5% of scores in each section or quadrant to be atypical. Therefore, no direct control group was required for this study.
Although many perinatal and neonatal risk factors were examined, we report P-values without adjustment for multiple hypothesis testing. If such an adjustment were performed, it would require that each result detract from the others. This method would be impractical in our premature population, as there are plausible relationships between each risk factor and our outcome (an atypical overall Sensory Profile).14 We chose instead to rely on scientific judgment instead of an adjusted level of statistical significance, and did not adjust for multiple hypothesis testing.
All analyses were performed using STATA 11 statistical software (StataCorp, College Station, TX, USA).
RESULTS
A total of 107 children received a Sensory Profile between 2009 and 2011. Table 1 shows the characteristics of the overall population.
Table 1.
Characteristics of study participants
| Variable | Study population (n = 107) | Children with typical Sensory Profiles (n = 65) | Children with atypical Sensory Profiles (n = 42) | P-valuea |
|---|---|---|---|---|
| Demographics | ||||
| Male sex, % | 53 | 51 | 57 | 0.52 |
| Gestational age in weeks, mean (s.d.) | 28.3 (2.3) | 28.5 (2.2) | 27.9 (2.4) | 0.22 |
| Birth weight in grams, mean (s.d.) | 1159 (379) | 1176 (381) | 1133 (378) | 0.58 |
| Prenatal risk factors | ||||
| Pregnancy-induced hypertension, % | 26 | 30 | 20 | 0.23 |
| Chorioamnionitis, % | 10 | 8 | 12 | 0.47 |
| Neonatal risk factors | ||||
| Necrotizing enterocolitis, % | 5 | 5 | 5 | 0.96 |
| Intraventricular hemorrhage (grades III or IV), % | 6 | 3 | 11 | 0.14 |
| Cystic periventricular leukomalacia, % | 6 | 3 | 11 | 0.14 |
| Chronic lung disease, % | 24 | 17 | 34 | 0.05 |
| Retinopathy of prematurity requiring laser surgery, % | 7 | 5 | 10 | 0.29 |
| Socioeconomic risk factors | ||||
| Maternal age in years, mean (s.d.) | 30.8 (6.5) | 31.3 (6.4) | 30.1 (6.6) | 0.36 |
| Maternal education in years, mean (s.d.) | 14.9 (2.8) | 15.1 (2.6) | 14.5 (3) | 0.42 |
| Characteristics at follow-up | ||||
| Age at examination in years, mean (s.d.) | 2.9 (2.0) | 2.6 (1.8) | 3.3 (2.2) | 0.10 |
| Abnormal neurologic examination, % | 10 | 9 | 12 | 0.65 |
| Cognitive score <70 | 2 | 3 | 0 | 0.26 |
Bivariate analysis comparing risk factors in children with typical and atypical Sensory Profiles.
In this study, 42 participants (39%) had an atypical overall Sensory Profile (at least one quadrant or section score >2 s.d. from the mean of the Sensory Profile validation group). Of note, 93 participants (87%) had an overall Sensory Profile with at least one quadrant or section score that was >1 s.d. from the mean of the validation group. Of those with atypical overall Sensory Profiles, 58% had an atypical performance in multiple sections or quadrants. The incidence of atypical overall Sensory Profiles was similar in children evaluated at 1 to 4 years of age (37%; n = 70) and children evaluated at 4 to 8 years of age (43%; n = 37; P = 0.54). No perinatal or neonatal factors were associated with the increased risk of atypical overall Sensory Profiles in children born prematurely (P≥0.05 for all, Table 1). There was no suggestion that an atypical overall Sensory Profile was related to cognitive or motor outcome at follow-up.
Of the five Sensory Profile sections, the auditory, tactile and vestibular processing sections appeared to be most affected, with relative sparing of the oral sensory processing and visual processing domains (Table 2). Although significantly more participants than expected (based on the validation group) had atypical scores in each of the four quadrants, nearly a quarter (23%) of the participants had an atypical score in the low registration quadrant.
Table 2.
Percentage of participants with atypical Sensory Profile quadrant and section scores
| Na | Atypical score (% of participants) | P-value† | |
|---|---|---|---|
| Sections | |||
| Auditory processing | 99 | 12 | <0.01 |
| Visual processing | 96 | 2 | 0.19 |
| Tactile processing | 86 | 10 | 0.02 |
| Vestibular processing | 102 | 13 | <0.01 |
| Oral sensory processing | 88 | 9 | 0.08 |
| Quadrants | |||
| Low registration | 91 | 24 | <0.01 |
| Sensory seeking | 85 | 11 | 0.02 |
| Sensory sensitivity | 90 | 10 | 0.03 |
| Sensory avoiding | 87 | 11 | <0.01 |
P-value based on test of proportion between observed values and expected (based on the Sensory Profile validation group).
Numbers vary based on non-response to specific questions on the Sensory Profile.
DISCUSSION
In this study, we found that 39% of children born prematurely (at a gestational age of ≤32 weeks) had an atypical overall Sensory Profile (a section or quadrant score >2 s.d. from the expected mean, based on the Sensory Profile validation group). The sensory sections most likely to be affected were auditory, tactile and vestibular processing. In addition, in this study, children born prematurely had atypical performance in all four Sensory Profile quadrants. It is notable that sensory differences were so prevalent in our cohort, given that we studied a relatively stable Neonatal Intensive Care Nursery population. These findings support the growing literature that children born prematurely experience difficulties with sensory processing.
Our study’s finding of atypical auditory, tactile and vestibular processing scores (with a trend toward an increase in atypical oral sensory processing scores) in children born prematurely are consistent with the published literature. Only one published study has used the Sensory Profile to evaluate premature infants; this study looked specifically at late-preterm infants (infants born at 34 to 36 weeks of gestation). The authors found that at 1 year of age, late-preterm infants were more likely than their term counterparts to score atypically on the auditory processing and oral sensory processing components of the Sensory Profile.15 Although late-preterm infants are increasingly recognized as being at risk for neurodevelopmental impairments when compared with term infants, they are at lower risk of such impairments than are infants born at ≤32 weeks. As our study included infants born at earlier gestational ages, and as the infants in our study were seen in follow-up at older ages (when atypical sensory behavior may be more apparent), it not surprising that our participants had more atypical Sensory Profiles sections than the infants in the late-preterm study.
Several physiologic studies support our findings that premature infants have atypical auditory, tactile and vestibular processing. School-aged children who were born prematurely have more deficits in motion processing than term infants, as measured by random dot kinematograms.16 Similarly, those born prematurely were more likely than those born at term to demonstrate decreased sensitivity to thermal modalities and to exhibit tactile defensiveness.17,18 In addition, childhood electrophysiologic auditory responses were lower in amplitude in children born prematurely than in children born at term, showing differences in auditory processing.19
In addition to having atypical performance in three of five sensory domains, our population of children born prematurely had atypical performance in all four Sensory Profile quadrants. This finding indicates that there is no consistent pattern of neurologic threshold (sensitivity to sensory inputs) and behavioral response in children born prematurely.
In this study, no specific perinatal or neonatal risk factors were associated with having an atypical overall Sensory Profile, which may in part have been due to low prevalence in our population. The association with chronic lung disease approached statistical significance (P = 0.05). As chronic lung disease has previously been reported to increase the risk of cognitive delay, cerebral palsy, and hearing and vision impairments,20,21 it is not surprising that it may also be associated with sensory processing differences. In addition, there was a trend toward an increased risk of an atypical Sensory Profile with older age at follow-up (P = 0.1). This may reflect developmental evolution, in that atypical sensory behaviors may become more apparent or severe as children age. Alternatively, parents of children with persistent or noticeable deficits may be more likely than parents of children without deficits to seek care at a high-risk follow-up clinic.
A trend was also seen toward increased brain injury (grades III to IV intraventricular hemorrhage and cystic periventricular leukomalacia) and atypical overall Sensory Profiles (P = 0.14 for each). We anticipated these associations, because brain injury is a well-recognized risk factor for adverse neurodevelopment.21 It is possible that prematurity-associated white matter injury to the brain, perhaps to the sensory cortices, and/or connections between brainstem nuclei, thalamic relays, primary cortex and/or integration areas, may have a role in atypical sensory processing. In this study, we used head ultrasounds to determine brain injury. As studies have shown improved detection of white matter injury with magnetic resonance imaging (as compared with ultrasound imaging),22 the relationship between brain injury and atypical overall Sensory Profiles may be better elucidated with magnetic resonance imaging studies. Other potential explanations for the potential association between brain injury and atypical Sensory Profiles are that the ex utero environment (with its associated noxious stimuli) may affect development in children born prematurely and that potentially harmful interventions associated with prematurity (for example, oxygen therapy) contribute to atypical sensory behaviors.
This study was performed at a single institution, which may limit its generalizability. However, our sample appeared to be representative, as the incidences of neonatal risk factors in our population appear consistent with what has been reported in the literature (Table 1).23 Another limitation is that as we studied infants and children across a wide range of ages, we combined data from both the infant/toddler Sensory Profile and the standard Sensory Profile. As this was a descriptive study of the Sensory Profile in children born prematurely, and as both versions share the five sections and four quadrants analyzed in this study, we felt this to be reasonable. Finally, we defined ‘atypical’ as any score that was >2 s.d. from the mean of the validation group (thus, both high and low scores that were >2 s.d. from the mean were grouped together). Future studies with larger sample sizes should be performed to better discriminate among children at the different ends of the spectrum (for example, ‘always/almost always’ versus ‘never/almost never’) and to better assess risk factors for having an atypical Sensory Profile. The Sensory Profile is a caregiver-reported questionnaire, not a direct assessment tool, and is therefore subjective. However, this perspective is beneficial, as in the case of sensory processing, it is the subjective experiences of the child and family that impact quality of life.
In conclusion, this study provides data that children born prematurely exhibit atypical sensory behaviors across multiple sensory domains. Our findings add credence to anecdotal reports that children born prematurely process sensory stimuli in an atypical manner. It also provides an alternative explanation for why children born prematurely have a high frequency of scoring positive on autism screening tests. By better recognizing the sensory sensitivities exhibited by these high-risk children, and differentiating them from the classic autism phenotype, we ultimately hope to enable children born prematurely to receive optimized interventions to improve their daily functioning. In addition, we hope to gain understanding of the mechanisms behind these findings. Further work in this area is essential to effectively guide treatment of this pervasive sequela of premature delivery. At present, we suggest that practitioners who care for former premature infants screen for sensory sensitivities and refer children with sensory differences to appropriate community resources (developmental–behavioral pediatricians, child neurologists and occupational therapists).
Acknowledgments
AJB receives funding from the NINDS (R01). EJM receives funding from the Wallace Research Foundation and the NIMH (K23). This project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 RR024131. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Limperopoulos C, Bassan H, Sullivan NR, Soul JS, Robertson RL, Jr, Moore M, et al. Positive screening for autism in expreterm infants: prevalence and risk factors. Pediatrics. 2008;121(4):758–765. doi: 10.1542/peds.2007-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N. Autism spectrum disorders in extremely preterm children. J Pediatr. 2010;156(4):525–531e2. doi: 10.1016/j.jpeds.2009.10.041. [DOI] [PubMed] [Google Scholar]
- 3.Kuban KC, O’Shea TM, Allred EN, Tager-Flusberg H, Goldstein DJ, Leviton A. Positive screening on the Modified Checklist for Autism in Toddlers (M-CHAT) in extremely low gestational age newborns. J Pediatr. 2009;154(4):535–540e1. doi: 10.1016/j.jpeds.2008.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yama B, Freeman T, Graves E, Yuan S, Karen Campbell M. Examination of the properties of the Modified Checklist for Autism in Toddlers (M-CHAT) in a population sample. J Autism Dev Disord. 2012;42(1):23–34. doi: 10.1007/s10803-011-1211-3. [DOI] [PubMed] [Google Scholar]
- 5.Pinto-Martin JA, Levy SE, Feldman JF, Lorenz JM, Paneth N, Whitaker AH. Prevalence of autism spectrum disorder in adolescents born weighing <2000 grams. Pediatrics. 2011;128(5):883–891. doi: 10.1542/peds.2010-2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Prevalence of autism Ssectrum disorders-autism and developmental disabilities monitoring netwok, 14 sites, United States, 2008. MMWR. 2012;61(3):1–19. [PubMed] [Google Scholar]
- 7.Leekam SR, Nieto C, Libby SJ, Wing L, Gould J. Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord. 2007;37(5):894–910. doi: 10.1007/s10803-006-0218-7. [DOI] [PubMed] [Google Scholar]
- 8.Marco EJ, Hinkley LB, Hill SS, Nagarajan SS. Sensory processing in autism: a review of neurophysiologic findings. Pediatr Res. 2011;69(5 Pt 2):48R–54R. doi: 10.1203/PDR.0b013e3182130c54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robins D, Fein D, Barton M. The Modified Checklist for Autism in Toddlers (M-CHAT) University of Connecticut; Storrs, CT, USA: 1999. [Google Scholar]
- 10.Luyster RJ, Kuban KC, O’Shea TM, Paneth N, Allred EN, Leviton A, et al. The modified checklist for autism in toddlers in extremely low gestational age newborns: individual items associated with motor, cognitive, vision and hearing limitations. Paediatr Perinat Epidemiol. 2011;25(4):366–376. doi: 10.1111/j.1365-3016.2010.01187.x. [DOI] [PubMed] [Google Scholar]
- 11.Dunn W. Infant/Toddler Sensory Profile User’s Manual. NCS Pearson; San Antonio TX, USA: 2002. [Google Scholar]
- 12.Dunn W. Sensory Profile User’s Manual. NCS Pearson; Minneapolis, MN, USA: 1999. [Google Scholar]
- 13.Ermer J, Dunn W. The sensory profile: a discriminant analysis of children with and without disabilities. Am J Occup Ther. 1998;52(4):283–290. doi: 10.5014/ajot.52.4.283. [DOI] [PubMed] [Google Scholar]
- 14.Savitz DA, Olshan AF. Multiple comparisons and related issues in the interpretation of epidemiologic data. Am J Epidemiol. 1995;142(9):904–908. doi: 10.1093/oxfordjournals.aje.a117737. [DOI] [PubMed] [Google Scholar]
- 15.Bart O, Shayevits S, Gabis LV, Morag I. Prediction of participation and sensory modulation of late preterm infants at 12 months: a prospective study. Res Dev Disabil. 2011;32(6):2732–2738. doi: 10.1016/j.ridd.2011.05.037. [DOI] [PubMed] [Google Scholar]
- 16.MacKay TL, Jakobson LS, Ellemberg D, Lewis TL, Maurer D, Casiro O. Deficits in the processing of local and global motion in very low birthweight children. Neuropsychologia. 2005;43(12):1738–1748. doi: 10.1016/j.neuropsychologia.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Walker SM, Franck LS, Fitzgerald M, Myles J, Stocks J, Marlow N. Long-term impact of neonatal intensive care and surgery on somatosensory perception in children born extremely preterm. Pain. 2009;141(1–2):79–87. doi: 10.1016/j.pain.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 18.Case-Smith J, Butcher L, Reed D. Parents’ report of sensory responsiveness and temperament in preterm infants. Am J Occup Ther. 1998;52(7):547–555. doi: 10.5014/ajot.52.7.547. [DOI] [PubMed] [Google Scholar]
- 19.Gomot M, Bruneau N, Laurent JP, Barthelemy C, Saliba E. Left temporal impairment of auditory information processing in prematurely born 9-year-old children: an electrophysiological study. Int J Psychophysiol. 2007;64(2):123–129. doi: 10.1016/j.ijpsycho.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116(6):1353–1360. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 21.Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med. 2006;355(7):685–694. doi: 10.1056/NEJMoa053792. [DOI] [PubMed] [Google Scholar]
- 22.Hintz SR, O’Shea M. Neuroimaging and neurodevelopmental outcomes in pre-term infants. Semin Perinatol. 2008;32(1):11–19. doi: 10.1053/j.semperi.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 23.Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196(2):147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]