Abstract
Traumatic brain injury sometimes can lead to psychotic disorder which resembles schizophrenia. We report a 17-year-old boy, admitted to psychiatric department for psychotic symptomatology. He had suffered penetrating craniocerebral injury after stabbing by a billiard stick, three years earlier. On admission, he expressed delusions with paranoid and religious content. The magnetic resonance imaging of the brain showed a 10 cm large tubular area of posttraumatic encephalomalacia of the left hemisphere, whereas the electroencephalography revealed slow left temporal activity. The patient’s recovery was uneventful with clozapine at a dosage of 100 mg daily. This case shows the diagnostic challenge in differentiation between schizophrenia and psychotic disorder due to traumatic brain injury. The authors emphasise the importance of imaging of the brain, especially magnetic resonance, in establishing the diagnosis of psychotic disorder due to traumatic brain injury.
Keywords: head injury, psychiatry, radiology, MRI scan, traumatic brain injury
Psychotic disorder secondary to traumatic brain injury (PDTBI) is specified by clinical signs of hallucinations or delusions when there is a direct relation between psychosis and traumatic brain injury1,2. Although there are no published epidemiological data about stab brain injuries in the territory of Southeast Europe, in western countries stab brain injuries are relatively uncommon, because the adult calvarium usually provides an effective barrier3. We report the unusual case of PDTBI in relation to stab brain injury by a billiard stick.
Case report
A 17-year-old boy was admitted to the psychiatric department due to psychotic symptomatology. He had been intentionally stabbed by a billiard stick, which passed through his left orbit deeply into the brain three years earlier. At that time, the wound was treated conservatively. Meanwhile, he gradually started exhibiting social withdrawal, anhedonia, disinhibited behaviour accompanied by delusions and visual hallucinations. In his family history, there were no similar symptoms.
On admission, he expressed delusions with paranoid and religious content. The patient showed signs of bradypsychia, his mood was depressed and he had no insight of his condition. Except for the left eye mydriasis, the patient’s neurological findings were unremarkable.
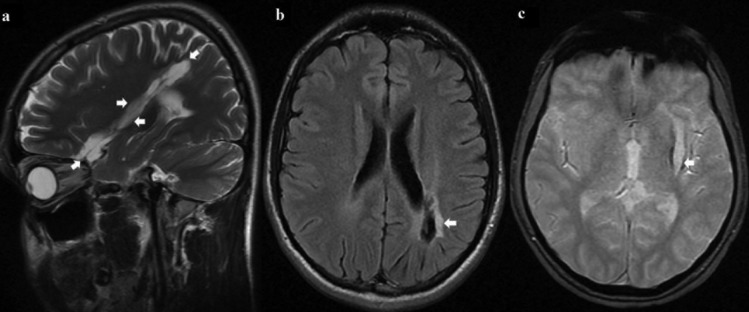
The magnetic resonance imaging of the brain showed a 10 cm large tubular area of posttraumatic encephalomalacia (Figure 1a) surrounded by a peripheral gliosis (Figure 1b) and hemosiderin rim (Figure 1c). The affected brain areas were left orbitofrontal region, insula, putamen, deep white matter and parietal lobe with consecutively slightly enlarged left lateral ventricle. The electroencephalography (EEG) showed slow left temporal activity. Abdominal ultrasound, chest radiography, blood and urine analysis showed no relevant abnormality.
The patient remained in the hospital for five weeks. He was initially given 12.5 mg of clozapine to the maximum dosage of 100 mg/day, which was reached by the second week. By the end of the third week his visual hallucinations had ceased and his delusions had become less intensive. Moreover, his depressed mood was not so pronounced. No side effects were recorded and the blood tests showed no alterations either.
Discussion
According to Bauer and Patzelt, penetrating craniocerebral injuries are frequently inflicted with a knife4. They occur almost exclusively in cases of homicide and only 13 cases were documented during a period of 30 years. However, to the best of our knowledge, only two cases of stab brain injury by a billiard stick were reported before. Orbitae and temporal regions are areas of thin bone where forcefully thrust sharp objects may penetrate easily. Usually, brain injury is limited to the wound tract with a good prognosis of recovery unless the brain stem is damaged4. Although reactive gliosis is the universal reaction to brain injury, the precise origin of the glial cells reacting to injury are unknown5.
It has been estimated that traumatic brain injury (TBI) increases the risk of psychosis two- to three-fold over that of general population6. Commonly, the latency period between TBI and new-onset psychosis is about four years, which makes establishing the diagnosis of PDTBI more difficult7. Nonetheless, Kim et al. argued that no firm conclusions could be made regarding the incidence or prevalence of PDTBI8. As pre-injury risk factors for PDTBI, Arciniegas et al reported male gender, neurodevelopmental and neuropsychiatric problems, and family history of schizophrenia9. In the present case, the risk factor was male gender, while personal and family history were not significant.
Traumatic lesions of temporal and frontal lobes are the most common injury risk factor1. Neuropsychologically, posttraumatic behavioural changes in our patient could be attributed mostly to the lesion of the frontal lobe, precisely prefrontal cortex that is responsible for executive functions such as initiation, mental flexibility, planning, working memory, problem solving, verbal reasoning, inhibition and mental flexibility10. Therefore, clinical symptoms are divided according to the affected cognitive function. The orbitofrontal syndrome, prominent in our case, is characterized by disinhibition, impulsive behaviour, poor judgement and insight, irritability and emotional lability11. The Vietnam Head Injury Study concluded that subjects with lesions limited to the frontal lobes tended to show more aggressive and violent behaviours compared with patients with non-frontal head injury and controls without head injury12. Moreover, a countless cases treated with abandoned infamous psychosurgical procedure called ‘frontal leucotomy’ testify in favour of the mentioned role of the prefrontal cortex13. While left hemispheric injury is associated with the development of schizophreniform posttraumatic psychosis, like in the present case (Figure 1), right hemispheric injury is more frequently associated with the development of delusions alone14.
Figure 1. Sagittal T2W (a, arrows), Axial T2 FLAIR (b) and Axial T2* GRE (c) MR images show a large tubular area of posttraumatic encephalomalacia. Note the rim of peripheral gliosis (b, arrow) and hemosiderin (c, arrow).
Electroencephalographic abnormalities together with posttraumatic epilepsy and cognitive impairments are the most common post-injury risk factors associated with PDTBI9. About 70% of the persons with PDTBI have EEG abnormalities that are manifested mostly (55%) as asymmetric temporal slowing, which was found in our patient as well15. According to the Diagnostic and statistical manual of mental disorders, the criteria for establishing the diagnosis of PDTBI are: prominent hallucinations or delusions; evidence from the history, physical examination, or laboratory findings that the disturbance was the direct physiological consequence of a medical condition; lack of evidence suggesting that the disturbance was better accounted for by another mental disorder; lack of evidence suggesting that the disturbance occurred exclusively during the course of a delirium16. Analysing 60 published cases of PTDBI, Fujii and Ahmed found that most patients experienced delusions (47 out of 60), while almost half the subjects experienced hallucinations (28 out of 60)16.
As far as medications are concerned, the ‘start-low, go-slow’ approach is recommended17. Anti-psychotic medications with potent anti-histaminic, anti-dopaminergic and anti-cholinergic properties should be avoided due to their tendency to produce significant adverse effects in these patients. Regarding the benefits and potential side effects, the atypical anti-psychotics such as clozapine, olanzapine, risperidone, quetiapine and ziprasidone are advised9.
Although many questions remain about how traumatic brain injury is associated with psychotic symptoms, this case certainly supports their relation. Among the abovementioned diagnostic modalities, magnetic resonance imaging of the brain plays a significant role and represents a contemporary method of establishing the diagnosis of PTDBI.
References
- 1.Fujii DE, Ahmed I. Characteristics of psychotic disorder due to traumatic brain injury: an analysis of case studies in the literature. J Neuropsychiatry Clin Neurosci. 2002;14:130–140. doi: 10.1176/jnp.14.2.130. [DOI] [PubMed] [Google Scholar]
- 2.Sachdev P. Schizophrenia-like psychosis and epilepsy: the status of the association. Am J Psychiatry. 1998;158:325–336. doi: 10.1176/ajp.155.3.325. [DOI] [PubMed] [Google Scholar]
- Dempsey LC, Winestock DP, Hoff JT. Stab wounds of the brain. West J Med. 1977;126:1–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer M, Patzelt D. Intracranial stab injuries: case report and case study. Forensic Sci Int. 2002;129:122–127. doi: 10.1016/s0379-0738(02)00271-2. [DOI] [PubMed] [Google Scholar]
- 5.Buffo A, Rite I, Tripathi P, Lepier A, Colak D, Horn AP, et al. Origin and progeny of reactive gliosis: a source of multipotent cells in the injured brain. Proc Natl Acad Sci U S A. 2008;105:3581–3586. doi: 10.1073/pnas.0709002105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Achté K, Jarho L, Kyykkä T, Vesterinen E. Paranoid disorders following war brain damage. Preliminary report. Psychopathology. 1991;24:309–315. doi: 10.1159/000284731. [DOI] [PubMed] [Google Scholar]
- 7.Fujii DE, Ahmed I. Psychotic disorder following traumatic brain injury: a conceptual framework. Cogn Neuropsychiatry. 2002;7:41–62. doi: 10.1080/135468000143000131. [DOI] [PubMed] [Google Scholar]
- 8.Kim E, Lauterbach EC, Reeve A, Arciniegas DB, Coburn KL, Mendez MF, et al. Neuropsychiatric complications of traumatic brain injury: a critical review of the literature (a report by the ANPA committee on Research) J Neuropsychiatry Clin Neurosci. 2007;19:106–127. doi: 10.1176/jnp.2007.19.2.106. [DOI] [PubMed] [Google Scholar]
- 9.Arciniegas DB, Harris S, Brousseau KM. Psychosis following traumatic brain injury. Int Rev Psychiatr. 2003;15:328–340. doi: 10.1080/09540260310001606719. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: a meta-analysis. Psychiatry Res. 2009;174:81–88. doi: 10.1016/j.pscychresns.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brower MC, Price BH. Neuropsychiatry of frontal lobe dysfunction in violent and criminal behaviour: a critical review. J Neurol Neurosurg Psychiatry. 2001;71:720–726. doi: 10.1136/jnnp.71.6.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grafman J, Schwab K, Warden D, Pridgen A, Brown HR, Salazar AM. Frontal lobe injuries, violence, and aggression: a report of the Vietnam Head Injury Study. Neurology. 1996;46:1231–1238. doi: 10.1212/wnl.46.5.1231. [DOI] [PubMed] [Google Scholar]
- 13.Mashour GA, Walker EE, Martuza RL. Psychosurgery: past, present, and future. Brain Res Brain Res Rev. 2005;48:409–419. doi: 10.1016/j.brainresrev.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Sachdev P, Smith JS, Cathcart S. Schizophrenia-like psychosis following traumatic brain injury: a chart based descriptive and case-control study. Psychol Med. 2001;31:231–239. doi: 10.1017/s0033291701003336. [DOI] [PubMed] [Google Scholar]
- 15.Guerreiro DF, Navarro R, Silva M, Carvalho M, Gois C. Psychosis secondary to traumatic brain injury. Brain Inj. 2009;23:358–361. doi: 10.1080/02699050902800918. [DOI] [PubMed] [Google Scholar]
- 16.Flaum M, Amador X. Schizophernia and other psychotic disorders. In: First MB, editor. Diagnostic and statistical manual of mental disorders, 4th edition-text revised (DSM-IV-TR) Washington DC: American Psychiatric Association. 2000:297–343. [Google Scholar]
- 17.McAllister TW. Traumatic brain injury and psychosis: what is the connection? Semin Clin Neuropsychiatry. 1998;3:211–223. [PubMed] [Google Scholar]


