Abstract
To analyse the possible factors contributing to spontaneous cerebrospinal fluid (CSF) rhinorrhea and to assess the outcome of Transnasal endoscopic repair at our centre. Retrospective case series of patients with spontaneous CSF rhinorrhea at our institution from Jan 2006 to May 2010. 7 patients were diagnosed with spontaneous CSF rhinorrhea. 5 of the 7 patients were obese, middle aged females managed with Transnasal endoscopic repair with fascia lata auto graft. Successful repair of CSF rhinorrhea was achieved in all the patients with a single endoscopic procedure; no patient required a revision procedure. Spontaneous CSF rhinorrhea is a rare condition seen mostly in middle aged obese females with the anterior part of the cribriform plate being the most common site of leak. HRCT paranasal sinus (1 mm cuts) was an effective modality of investigation in our study with ancillary investigations been CT Cisternography, CSF analysis and MRI for inactive leaks. In the absence of a large breech of the skull base, endoscopic repair of CSF rhinorrhea carries a high success rate with a high safety margin and very low morbidity rate.
Keywords: Cerebrospinal fluid, Rhinorrhea, Endoscopic sinus surgery
Introduction
Cerebrospinal fluid (CSF) leak occurs as a result of an abnormal communication between the subarachnoid space and a pneumatized area in the skull base that includes the sinonasal tract. This communication or fistula must involve a breech of the arachnoid and dura matter, the bone of skull base, and the underlying mucosa [1]. CSF rhinorrhea can be classified according to the etiology into traumatic and non-traumatic [2]. Traumatic fistulae are subdivided into accidental, which compose the majority (up to 80%), and iatrogenic or post-surgical (16%). The non-traumatic or primary CSF fistula accounts for less than 4% of all CSF fistulae. The non traumatic CSF fistula can be further classified into high pressure or normal pressure.
Because of the serious potential complications of CSF rhinorrhea, (e.g. meningitis, brain abscess, pneumocephalus) prompt management and repair of all CSF rhinorrhea cases should be attempted. Different approaches have been described for the repair of sinonasal CSF fistula, including the intracranial approach [3] which has a high failure rate (up to 70%) [3, 4]. Multiple extra cranial approaches have been used for repair of CSF leak [5–10]. Mattox and Kennedy [11] were the first to explain the details of endoscopic repair, reporting an initial success rate of 88% with a final success rate of 100%. Careful review of the literature reveals a minor emphasis on non-traumatic CSF leak. Most of the published studies discuss CSF leaks of traumatic origin as it is considered the most common.
Materials and Methods
We reviewed the patients who presented in our department with CSF rhinorrhea. Patients with spontaneous CSF leak were included in our retrospective study, while those with history of trauma, previous nasal surgery, congenital malformations of the skull base were excluded from the study. 7 patients (Table 1) were included in the study. The most common presenting symptom was continuous watery nasal discharge. All the patients underwent a diagnostic nasal endoscopic examination. The presence of CSF was confirmed by CSF analysis. CT scan coronal cuts (1 mm) (Fig. 1) of the paranasal sinuses were obtained for all the patients. Additional investigations included CT cisternography, MRI paranasal sinus.
Table 1.
Description of the clinical details of the patients in the study
| Our data | |||||||
|---|---|---|---|---|---|---|---|
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Age/sex | 40/m | 39/f | 40/f | 40/f | 28/m | 54/f | 58/f |
| Weight (Kg) | 70 | 74 | 90 | 97 | 80 | 79 | 79 |
| C/c | Watery Nd | Watery Nd | Watery Nd + cough + Sn | WateryNd + Ha | Watery Nd | Watery Nd + Sn | Watery Nd |
| Duration of c/c | 1 months | 4 months | 1 year | 20 days | 3 months | 2 months | 6 months |
| Side | R | R | L | L | L | R | R followed by L |
| Site of leak | R Cribri | R Cribri | L Cribri extending to post eth | L Cribri | L Cribri | R Cribri | R Cribri L Cribri |
| Olfaction | N | N | N | N | N | N | N |
| Csf pressure | Raised | Raised | Raised | Raised | Raised | Raised | Raised |
| Surgery | Sep + Fess + Tner | Sep + Fess + Tner | Fess + Tner | Sep + Fess + Tner | Sep + Fess + Tner | Sep + Fess + Tner | Sep + Fess + Rt Tner, Lt Tner |
| Site of leak on table | R Cribri | R Cribri | R Cribri | L Cribri | L Cribri | R Cribri | R Cribri L Cribri |
| Size of the leak | 2 mm | 2.5 mm | 2.5 cms | 3 mm | 2 mm | 3 mm | 2 mm |
| Graft | Fascia lata | Fascia lata | Fascia lata | Fascia lata | Fascia lata | Fascia lata | Fascia lata |
| Leak free Postop period | 9 months | 7 months | 7 months | 9 months | 2 years | 8 months | 3 years and 4 months |
| Invesg | CSF anal + CT + MRI | CSF anal + CT + MRI | CT PNS | CSF anal + CT + CT cist | CSF anal + CT + CT cist | CT cist | CSF anal + CT PNS |
C/c Chief complaints, Ha head ache, Sn sneezing, R right, L left, Sep septoplasty, Tner transnasal endoscopic repair of CSF leak, CSF anal CSF analysis, CT Cist CT cisternography, Cribri cribriform plate
Fig. 1.

CT Scan paranasal sinus coronal cut (1 mm) depicting the defect in the Rt Cribriform plate
The most common site for CSF leak was the anterior part of cribriform plate (Fig. 2) according to the study. The repair of the CSF leak was done by the extracranial transnasal endoscopic approach under GA. One patient initially complained of watery nasal discharge from the right nasal cavity. She was diagnosed to have a cribriform plate defect on the right side, repaired by the trans nasal endoscopic approach, was asymptomatic for 3 years following the surgery and later after 3 years she complained of watery nasal discharge from the left nasal cavity, was investigated and diagnosed with a left cribriform plate defect and managed with the Trans nasal endoscopic procedure for CSF repair. She has been asymptomatic since then.
Fig. 2.
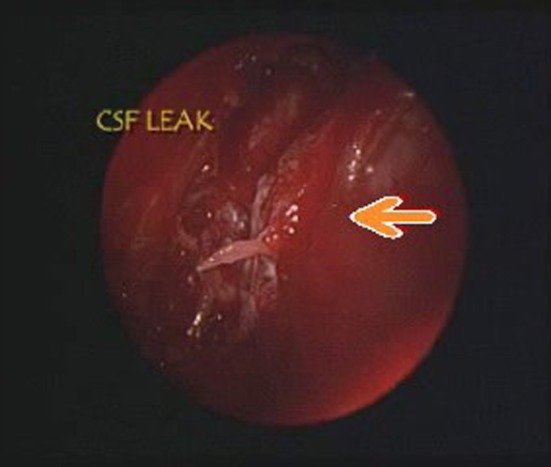
Intra operative endoscopic view depicts the site of CSF leak
Operative Technique
Pre operatively lumbar drain was kept, CSF pressure was raised in all the patients. Patient under general anaesthesia, adequate exposure to the site of leak was obtained. Once the site of leak was identified, the mucosa from the edges of the bony defect was denuded. Fascia lata graft harvested from the thigh and trimmed to appropriate size. Fascia lata is placed by the underlay technique laterally and overlay technique medially followed by another layer of Fascia lata over the initial graft, followed by gel foam and merocel nasal pack. Merocel pack was removed on the third post operative day. Lumbar drain was kept for 2 days post operatively.
Results
Out of the seven, five were females and two were males, their ages ranged between 40 and 60 years and weight between 70 and 97 kg, the follow up period ranged between 5 months and 3 years and 4 months. The most common site of leak was the anterior cribriform plate with size of the leak in 6 patients ranged between 2 and 3 mm. The clear fluids collected from the patients were sent for CSF analysis and was confirmed to be CSF in all the seven patients. CSF pressure was elevated in all our patients. HRCT scan paranasal sinus studies were positive in all of the seven patients. CT cisternography was done and positive in two patients, MRI (T2) were done in two patients and was used to localize the defect where the leak was not active during the study. Endonasal endoscopic approach under general anaesthesia was used in all the patients to repair the CSF leak with auto graft fascia lata.
All the patients had successful cessation of the rhinorrhea after a single procedure with post operative leak free periods ranging from 4 months to 2 years No major complications occurred secondary to surgical management.
Discussion
Non-traumatic CSF rhinorrhea can be spontaneous, caused by a bony defect. The causes of spontaneous CSF rhinorrhea are variable and not very well understood. Obesity is a very important risk factor. Overweight increases intra abdominal and intra thoracic pressure. This may effect blood circulation in cranial venous collectors and lead to development of permanent benign intracranial hypertension [12, 13]. Spontaneous CSF leak might also occur secondary to focal atrophy of the olfactory nerve in the region of the cribriform plate. Additionally, defective development of the bony skull base could allow the arachnoid and brain tissue to protrude through the nose [14].
Spontaneous CSF leaks are idiopathic in nature; however, recent evidence has led us to realize that spontaneous CSF rhinorrhea is in reality secondary to an intracranial process, namely elevated intracranial pressure (ICP) as well as with factors such as sneezing, coughing, or other causes of normal fluctuations in cerebrospinal fluid pressure [15]. The causes of elevated ICP can be multifactorial; nevertheless, once elevated ICP develops, the pressure exerted on areas of the anterior skull base (e.g, cribriform, lateral recess of the sphenoid sinus) result in remodeling and thinning of the bone. Ultimately, the bone is weakened until a defect is formed. If a defect is large, brain parenchyma may be herniated as well Since the communication between a sterile intracranial compartment and a non-sterile sinonasal cavity can lead to life threatening complications (e.g., meningitis, pneumocephalus, or brain abscess [16–18], prompt diagnosis and management is demanded. Chemical analysis of the collected samples of the rhinorrhea is important to confirm the nature of the CSF fluid.
Radiological investigations play a pivotal role in identifying the underlying etiology of CSF rhinorrhea and in detecting the site, side, and size of the leaking fistula. With thin 1 mm cuts of coronal section, a CT scan was helpful in detecting bony dehiscence. Other CT findings in CSF leak cases include deviation of christa galli, causative intracranial lesions (e.g. encephalocele), complications of CSF leak (e.g. pneumocephalus),or fluid in the extracranial compartment adjacent to the fistula site [16]. High resolution CT scan has an overall sensitivity of 70% in detecting bony dehiscence [19]. However, the rate of detection is much lower in cases of spontaneous CSF rhinorrhea with less than 2 mm skull base defects, due to partial volume averaging, resulting in false positive and false negative results [20]. MRI is a valuable non-invasive test for detecting and localizing CSF leak. Modification of MRI technique by using both T2 MRI images with fluid attenuated inversion recovery (FLAIR) imaging was very helpful in localizing CSF rhinorrhea. A FLAIR sequence is also capable of differentiating skull base cystic lesions of a CSF nature (arachnoid cyst, meningocele) from non-CSF lesions with similar signal intensity on T1,T2 sequence (e.g. epidermoid, inflammatory sinus changes) [21, 22].
CT cisternography is another valuable radiographic study that is considered the procedure of choice in detecting CSF leak [23–25]. It requires administration of a low osmolar non-ionic iodine contrast agent into the subarachnoid space with a subsequent search for agent egress through the fistula site [16]. The sensitivity can reach up to 90% in active leaks. However, this technique is invasive and the sensitivity can be as low as 40% in cases of intermittent or inactive leaks [26].
Surgical management of CSF rhinorrhea can be achieved by an intracranial or extracranial approach. The decision depends on the size and pathology causing the leak. Management of CSF rhinorrhea by an intracranial approach [27] carries morbidity and failure rates between 20 and 40% [28, 29]. On the other hand, an endoscopic approach is less morbid and has a success rate of 90–100% [11]. In the present study endoscopic approach for closure of the leak was done with combined overlay and underlay technique. This technique is useful for defects localized to the cribriform area since this combined technique doesn’t cause alteration of olfaction post operatively. Adjunctive techniques that can be used to increase the success rate of CSF fistula repair include perioperative antibiotics, diuretics, lumbar drain, and complete bed rest with elevation of the head.
We did not obtain results with respect to the use or withholding the use of these techniques due to ethical considerations and the results have to be viewed in this perspective. The contribution of adjunctive techniques to the overall success needs further evaluation.
Conclusion
Spontaneous CSF rhinorrhea is a relatively rare condition occurring due to different etiologies mostly seen in middle aged obese female patients. Prompt diagnosis and management of the condition is necessary because of the potential risky complications. Proper history taking, preoperative examination, precise preoperative localization is essential for successful repair. Among the multiple techniques available for localisation include HRCT paranasal sinus, CT Cisternography, MRI paranasal sinus. In the absence of a large skull base lesion or tumor, endoscopic repair of a CSF fistula with auto graft fascia lata carries a high success rate with a very high margin of safety and very low morbidity rate.
All our cases were cribriform plate defects 2–3 mm in size where the dura cannot be elevated medially. Fascia lata was placed as an overlay graft medially, and in an underlay fashion posteriorly, anteriorly, and laterally. Cartilage is not suitable at this site due to its inelasticity. Our maximum follow up is for 3 years with an average follow up of 15 months. No recurrences were seen. One case came with CSF leak from the cribriform plate of the non operated side which was also surgically repaired.
Contributor Information
D. S. Deenadayal, Email: aarticlinic@yahoo.com
D. Vidyasagar, Email: dvsag@rediffmail.com
References
- 1.Zapalac JS, Marple BF, Schwade ND. Skull base cerebrospinal fluid fistulas: comprehensive diagnostic algorithm. Otolaryngol Head Neck Surg. 2002;126:669–676. doi: 10.1067/mhn.2002.125755. [DOI] [PubMed] [Google Scholar]
- 2.Ommaya AK, DiChiro G, Baldwin M, et al. Nontraumatic cerebrospinal fluid rhinorrhea. J Neurol Neurosurg Psychiatry. 1968;31:214–255. doi: 10.1136/jnnp.31.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dandy WD. Pneumocephalus (intracranial pneumocele or aerocele) Arch Surg. 1926;12:949–982. doi: 10.1001/archsurg.1926.01130050003001. [DOI] [Google Scholar]
- 4.Park JI, Strezlow VV, Freidman WH. Current management of cerebrospinal fluid rhinorrhea. Laryngoscope. 1983;93:1294–1300. doi: 10.1002/lary.1983.93.10.1294. [DOI] [PubMed] [Google Scholar]
- 5.Dohlman G. Spontaneous cerebrospinal rhinorrhea. Acta Otolaryngol Suppl (Stockh) 1948;67:20–23. doi: 10.3109/00016484809129635. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch O. Successful closure of cerebrospinal fluid rhinorrhea by endonasal surgery. Arch Otolaryngol. 1952;56:1–13. doi: 10.1001/archotol.1952.00710020018001. [DOI] [PubMed] [Google Scholar]
- 7.Vrabec DP, Hallberg OE. Cerebrospinal fluid rhinorrhea. Arch Otolaryngol. 1964;80:218–229. doi: 10.1001/archotol.1964.00750040224022. [DOI] [PubMed] [Google Scholar]
- 8.Wigand ME. Transnasal ethmoidectomy under endoscopic control. Rhinology. 1981;19:7–15. [PubMed] [Google Scholar]
- 9.Stankiewicz JA. Complications of endoscopic intranasal ethmoidectomy: an update. Laryngoscope. 1989;99:686–690. doi: 10.1288/00005537-198907000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Papay FA, Maggiano H, Dominquez S, et al. Rigid endoscopic repair of paranasal sinus cerebrospinal fluid fistula. Laryngoscope. 1989;99:1195–1201. doi: 10.1288/00005537-198911000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Mattox DE, Kennedy DW. Endoscopic management of cerebrospinal fluid leaks and cephaloceles. Laryngoscope. 1990;100:857–862. doi: 10.1288/00005537-199008000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Badia L, Loughran S, Lund V. Primary spontaneous cerebrospinal fluid rhinorrhea and obesity. Am J Rhinol. 2001;15:117–119. doi: 10.2500/105065801781543736. [DOI] [PubMed] [Google Scholar]
- 13.Clark D, Bullock P, Hui T, Firth J. Benign intracranial hypertension: a cause of CSF rhinorrhea. J Neurol Neurosurg Psychiatry. 1994;57:847–849. doi: 10.1136/jnnp.57.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casiano RR, Jassir D. Endoscopic cerebrospinal fluid rhinorrhea repair: is lumbar drain necessary? Otolaryngol Head Neck Surg. 1999;121:745–750. doi: 10.1053/hn.1999.v121.a98754. [DOI] [PubMed] [Google Scholar]
- 15.O’Connell JEA. The cerebrospinal fluid pressure as an aetiological factor in the development of lesions affecting the central nervous system. Brain. 1953;76:279–298. doi: 10.1093/brain/76.2.279. [DOI] [PubMed] [Google Scholar]
- 16.Wax MK, Ramadan HH, Ortiz O, et al. Contemporary management of cerebrospinal fluid rhinorrhea. Otolaryngol Head Neck Surg. 1997;116:442–449. doi: 10.1016/S0194-5998(97)70292-4. [DOI] [PubMed] [Google Scholar]
- 17.Calvert CA, Caims H. Discussion on injuries of the frontal and ethmoid sinuses. Proc R Soc Med. 1942;35:805–810. [PMC free article] [PubMed] [Google Scholar]
- 18.Munro D. The modern treatment of craniocerebral injuries with special reference to the maximum permissible mortality and morbidity. N Engl J Med. 1935;213:893–906. doi: 10.1056/NEJM193511072131901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stone JA, Castillo M, Neelon B, Mukherji SK. Evaluation of CSF Leaks : high resolution CT compared with contrast enhanced CT and radionuclide cisternography. Am J Neuroradiol. 1999;20(4):706–712. [PMC free article] [PubMed] [Google Scholar]
- 20.Lund VJ, Savy L, Llyod G, Howard D (2000) Optimum imaging and diagnosis of cerebrospinal fluid rhinorrhoea. J Laryngol Otol 114(12):988–992 [DOI] [PubMed]
- 21.Gacek RR, Gacek MR, Tart R. Adult spontaneous cerebrospinal fluid otorhoea: diagnosis and management. Am J Otolaryngol. 1999;20:770–776. doi: 10.1016/S0196-0709(99)90001-7. [DOI] [PubMed] [Google Scholar]
- 22.Bradely WG, GM Bydder (1997). Advanced MR imaging techniques, 1st edn. Mosby year book, pp 143–162
- 23.Johnson DBS, Toland BJ, O’Dwyer AJ. Magnetic resonance imaging in the evaluation of cerebrospinal fluid fistulae. Clin Radiol. 1996;51:837–841. doi: 10.1016/S0009-9260(96)80079-1. [DOI] [PubMed] [Google Scholar]
- 24.Shetty PG, Shroff MM, Sahani DV, et al. Evaluation of high-resolution CT and MR cisternography in the diagnosis of cerebrospinal fluid fistula. Am J Neuroradiol. 1998;19:633–639. [PMC free article] [PubMed] [Google Scholar]
- 25.Gammal TE, Sobol W, Wadlington VR. cerebrospinal fluid fistula: detection with MR cisternography. Am J Neuroradiol. 1998;19:627–631. [PMC free article] [PubMed] [Google Scholar]
- 26.EL Jamel MS, Pidgeon CN, Toland J, et al. MR cisternography and the localization of CSF fistulae. Br J Neurosurg. 1994;8:433–437. doi: 10.3109/02688699408995111. [DOI] [PubMed] [Google Scholar]
- 27.Nachtigal D, Frenkiel S, Yoskovitch A, Mohr G. endoscopic repair of cerebrospinal fluid rhinorrhea: is it the treatment of choice? Otolaryngo. 1999;28:129–133. [PubMed] [Google Scholar]
- 28.Hubbard JL, McDonald TJ, Pearson BW, Laws ER. Spontaneous cerebrospinal fluid rhinorrhea: evolving concepts in diagnosis and surgical management based on the Mayo Clinic experience from 1970 through 1981. Neurosurgery. 1985;16:314–321. doi: 10.1227/00006123-198503000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Aarabi B, Leibrock LG. Neurosurgical approaches to cerebrospinal fluid rhinorrhea. Ear Nose Throat J. 1992;71:300–305. [PubMed] [Google Scholar]


