Abstract
The aim of the study is to compare the subjective (relief of symptoms) and objective (endoscopic visualization of ostium patency at the time of syringing) outcomes at the end of two procedures—Endonasal DCR versus External DCR with Mitomycin C and to assess the role of Mitomycin C in maintaining patency of nasolacrimal drainage system. Prospective randomized comparative study was performed. Thirty-five patients were enrolled in each endoscopic and external dacryocystorhinostomy groups with Mitomycin C (MMC) application. The 37 eyes underwent endonasal DCR (28 unilateral primary eyes + 1 bilateral primary eyes + 5 unilateral revision eyes + 1 bilateral revision eye) while 35 eyes underwent external DCR (34 unilateral primary eyes + 1 unilateral revision eye). Mitomycin C 0.2 mg/ml was applied intra-operatively for 5 min to the ostium site at the end of endonasal or external DCR procedure. Objective assessment by syringing at the end of 1 year in the endonasal group showed 35 eyes (94%) were patent, 1 (3%) was partially blocked and 1(3%) was completely blocked; while in external group all 35 eyes (100%) were patent. Endoscopic visualization of the ostium at the time of syringing showed only one eye (3%) in the endonasal group was blocked while all the other eyes in both groups were patent. Both groups had a mean follow-up of 6–36 months. No complications were associated with use of Mitomycin C. In conclusion, intra-operative use of Mitomycin C in both endoscopic DCR and external DCR is safe and effective in increasing the success rate.
Keywords: Chronic dacryocystitis, External dacryocystorhinostomy, Endonasal endoscopic dacryocystorhinostomy, Mitomycin C
Introduction
Dacryocystorhinostomy (DCR) is widely accepted as the procedure of choice for surgical correction of lacrimal drainage system obstruction distal to common canaliculus [1]. It can be done via external approach or endonasal endoscopic approach. Endonasal DCR has now come of age and the success of endonasal DCR compares favorably with that of external DCR. The advantages of endoscopic DCR include maintenance of lacrimal pump function, decreased operative time and avoidance of cutaneous scar. The main problems of endonasal DCR are doubts about long term patency and osteotomy closure by granulation tissue [2, 3]. Addeo Totti first described the external DCR in 1904 [4]. Bouget and Dupuy-Dutemps later described mucosal anastomosis with suturing of the mucosal flaps [4]. This procedure is carried on till this day with minor modifications. Failures in external DCR are attributed to position and size of the ostium or scarring within the anastomosis. The success rate of external DCR has been reported to be 80–99% depending on the surgeon’s experience. Endoscopic DCR has a reported success rate of around 77–95% [3].
Mitomycin C is derived from streptomyces caespitosus, an alkylating agent with anticancer property. It reduces fibroblast collagen synthesis by inhibiting DNA-dependant RNA synthesis and can suppress cellular proliferation in any period of the cell cycle [2, 3]. In order to prevent excessive scar formation Mitomycin C has been used as a surgical adjuvant in glaucoma filtration surgery and pterygium excision. More recently its use has been described in primary lacrimal drainage surgery [5, 6]. The beneficial effect of Mitomycin C (MMC) as a surgical adjuvant is thought to be related to its potent inhibition of fibroblast proliferation [5, 6]. Intraoperative use of Mitomycin C in both endoscopic and external DCR procedures may possibly improve the success rates over the traditional dacryocystorhinostomy procedures. Mitomycin C in external DCR when used in appropriate doses minimizes post operative fibrosis and granulations thereby maintaining a bigger post op ostium throughout the post operative period [2].
The aim of this study is to assess the ostium patency and to compare the success rate in both endonasal and external DCR groups following Mitomycin C application.
Materials and Methods
The patients attending ENT & Ophthalmic outpatient department in KLES Dr. Prabhakar Kore Hospital and Medical Research Centre (MRC), Belgaum presenting with watering of eye and/or swelling in the medial canthal region are the subjects for this study. The patients with post-saccal stenosis of primary and revision cases were confirmed by syringing. The duration of the study was from Aug 2008 to Aug 2011. Exclusion criteria were patients with presaccal obstruction, noticeable lower lid laxity, age under 15 years, suspicion of malignancy, radiation therapy to the head and neck area, post-traumatic bony deformity or bone diseases affecting the nose and orbit. Institutional ethical clearance was obtained.
Seventy patients (72 eyes) who consented for the study were randomized into two groups. The 37 eyes underwent endonasal DCR (28 unilateral primary eyes + 1 bilateral primary eyes + 5 unilateral revision eyes + 1 bilateral revision) while 35 eyes underwent external DCR (34 unilateral primary eyes + 1 unilateral revision eyes). In bilateral cases, each side was considered as separate eye.
All patients who underwent endonasal DCR were performed under local anasthesia. The operated side of the nasal cavity was packed with ribbon gauge soaked with 4% xylocaine and adrenaline 1:100,000 prior to surgery for surface anasthesia and vasoconstriction. Later, the mucosa of lateral wall of nose was infiltrated with 2% xylocaine with adrenaline. Using 00 endoscope and a sickle knife, 1 cm2 incision was made in the lateral wall of nose starting just anterior to the axilla of the middle turbinate. The 2 mm Kerrison’s punch was used to remove the frontal process of maxilla and the lacrimal bone. The lacrimal sac was identified, using sickle knife the medial wall of the sac was incised vertically and excised with Kerrison’s punch or cauterized. Any abnormality of the septum or middle turbinate likely to increase the risk of failure due to occlusion of the ostium or synechiae formation were corrected endoscopically. In revision cases membranectomy, osteotomy enlargement and synechiae release was done as required. At the end of the procedure, mitomycin C 0.2 mg/ml was applied at the rhinostomy site for 5 min soaked in gelfoam and washed with saline later. The lacrimal syringing was done to confirm the free flow of saline. Nasal packing was done with medicated ribbon gauze for 24 h.
In the patients who underwent external DCR, ribbon gauge soaked with 4% xylocaine and adrenaline 1:100,000 was used to pack nasal cavity and surgery was performed under local anasthesia. All cases were done by a single ophthalmologist using the technique of Dupuy-Dutemps and Bourguet. A straight incision of ~2 cm in length was made medial to the medial canthus, starting at the level of the medial canthal ligament. The orbicularis muscle fibers were separated with blunt dissection and cats paw retractors were used to retract the wound. The periosteum overlying the anterior lacrimal crest was exposed. The periosteum incision was made just medial and inferior to the bony insertion of the medial canthal tendon. The osteotomy measuring approximately 12 mm in diameter was created with Citelli’s punch. The lacrimal sac and nasal mucosa were opened in a longitudinal fashion to form anterior and posterior flaps. The anterior and posterior flaps were sutured separately with 6-0 Vicryl sutures. Mitomycin C 0.2 mg/ml was applied over the anastomosed flaps and osteotomy site for 5 min soaked in gelfoam and washed with saline later. Subcuticular sutures were put to close the wound.
The subjective assessment was done by questionnaire about symptoms. The objective assessment was done by endoscopic visualization of ostium patency at the time of syringing. These assessments were done at the end of 1 week, 4 weeks, 6 months and 1 year. Endoscopic suction clearance was done as when required for patients who underwent endoscopic DCR. The overall success rates were calculated for both endoscopic DCR and external DCR.
The statistical analyzes were performed using SPSS 12 statistical software. Success rates and other categorical variables were tested with Yates corrected Chi-Square test. P values greater than 0.05 was regarded as not significant.
Results
Of the 70 patients, there were 19 males and 51 females; the male to female ratio in the endonasal group was 1:3 while in external group was 1:2. The mean age in the endonasal group was 45.62 years while in the external group was 45.74 years. The majority of the patients, i.e. 78.5% (55/70) were from poor socio economic background. In this study disease involvement was equal on both sides. In both groups, epiphora was the main symptom in 75% eyes (54/72) while epiphora with discharge was seen in 25% eyes (18/72). The 49 eyes of chronic dacryocystitis, 22 eyes of mucocoele and one eye of lacrimal abscess were diagnosed before surgery. The four cases of gross deviated nasal septum (DNS) were found in the disease side of endonasal DCR group and all of them underwent endoscopic septoplasty. Only one case of gross DNS was found in external DCR group on the same side of disease and underwent conventional septoplasty. In the endoscopic DCR group, 5 had middle turbinate hypertrophy and only 1 was subjected to anterior middle turbinate resection. The distended sac was found in 6 eyes of endonasal DCR group and in 12 eyes of external DCR group; one sac was found to be cicatrized in the external DCR group. The 59% of cases in the endonasal DCR group were completed within 60 min while 63% of cases were performed within 60–90 min in the external DCR group. All 37 eyes in the endonasal DCR group were found to have mild to moderate bleeding. In the external DCR group, there was one eye with severe bleeding, 3 eyes of angular vessel bleeding and 2 eyes with delayed wound healing.
In the revision endoscopic DCR eyes, ostium enlargement was done in 2 eyes, while membranectomy was done in 4 eyes and synechiae release was done in one eye. Only one case of revision external DCR was present in this study which underwent synechiae release and refashioning of mucosal anastomosis.
Subjective evaluation in the endonasal DCR group, at the end of 4 weeks, 27 eyes (73%) were asymptomatic, 8 eyes (22%) showed significant improvement, 2 eyes (5%) showed slight improvement; while at the end of 6 months and 1 year, 27 eyes (73%) were asymptomatic, 7 eyes (19%) showed significant improvement, 2 eyes (5%) showed slight improvement and one eye (3%) remained the same. In the external DCR group, at the end of 4 weeks, 34 eyes were asymptomatic, one eye showed significant improvement; while at the end of 6 months and 1 year the results remained the same as at the end of 4 weeks. The comparison of subjective assessment of both endonasal and external DCR groups at the end of 4 weeks, 6 months and 1 year were found to be statistically significant (Tables 1, 2).
Table 1.
Subjective assessment of symptoms at the end of 4 weeks
| Period | Endonasal DCR 37 eyes |
External DCR 35 eyes |
P value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Asymptomatic | 27 | 73 | 34 | 97 | 0.028 (P < 0.05), statistically significant |
| Significant improvement | 8 | 22 | 1 | 3 | 0.011 (P < 0.05), statistically significant |
| Slight improvement | 2 | 5 | 0 | 0 | |
| Same | 0 | 0 | 0 | 0 | |
Table 2.
Subjective assessment of symptoms at the end of 1 year
| Period | Endonasal DCR 37 eyes |
External DCR 35 eyes |
P value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Asymptomatic | 27 | 73 | 34 | 97 | 0.028 (P < 0.05), statistically significant |
| Significant improvement | 7 | 19 | 1 | 3 | 0.011 (P < 0.05), statistically significant |
| Slight improvement | 2 | 5 | 0 | 0 | |
| Same | 1 | 3 | 0 | 0 | |
Objective assessment by endoscopic visualization of ostium patency at the time of syringing at the end of 6 months, in the endonasal group showed 35 eyes (94%) were patent, one eye (3%) was partially blocked and one eye (3%) was completely blocked; while in the external group all 35 eyes (100%) were patent. The results were the same at the end of 1 year for both endonasal and external DCR groups. Endoscopic visualization of the ostium showed only one eye (3%) in the endonasal group was found to be blocked while all the other eyes in both groups were patent (Fig. 1).
Fig. 1.
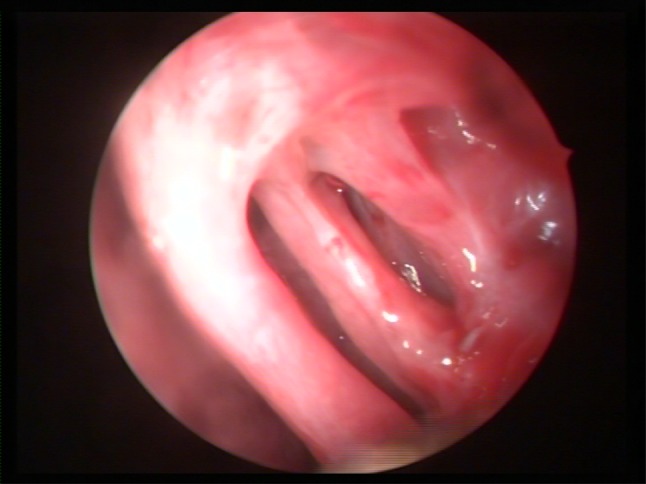
The endoscopic visualization of ostium patency at the time of syringing
The overall success rate was 97% in the endonasal DCR group while it was 100% in the external DCR group (Table 3). The comparative overall success rate between the endonasal and external DCR groups was not statistically significant (P = 0.168).
Table 3.
Overall success rate
| Results | Endonasal DCR group | External DCR group | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Success | 36 | 97 | 35 | 100 |
| Failure | 1 | 3 | 0 | 0 |
*Success rate: Group A and Group B did not differ significantly (P = 0.168)
Discussion
Chronic dacryocystitis had been observed to be more common in women of low-socio economic group due to their poor personal hygiene, long duration of exposure to smoke in the kitchen and dust in the external environment. The other possible cause could be congenital anatomical narrowing of naso-lacrimal drainage system in females as compared to the males [7].
The majority of the patients in our study were in the age group 31–40 years (28.5%), youngest being 19 years and oldest being 72 years. There was a declining trend towards both extremes of age. This may be due to the fact that lacrimal secretion is less in extremes of age.
In present study both sides had equal disease involvement, while other studies had observed predominant left side disease.
The osteotomy site will be compromised by fibrous tissue growth, scarring and granulation tissue formation during the healing process and thereby leading to surgical failure [6]. Lindberg et al. [8] showed that an appropriately large osteotomy made during surgery can narrow down to a final size of approximately 2 mm due to tissue growth and scarring . Hence, the use of Mitomycin C enables to reduce fibrous proliferation and vascular ingrowth at the osteotomy site and at the anastomosed flaps.
In present study, there were no complications associated with the use of Mitomycin C in the endonasal DCR group while there were 2 cases of delayed wound healing in the external DCR group probably due to Mitomycin C. The other complications like abnormal nasal bleeding, mucosal necrosis, infection or atrophic rhinitis were absent. The complications reported with the use of Mitomycin C (MMC) in pterygium surgery have included corneal perforation, cataract, secondary glaucoma and scleral calcification [9]. Hypotony-related maculopathy, infection and endophthalmitis have complicated the use of MMC in glaucoma surgery [10]. No complications from Mitomycin C use in lacrimal surgery were reported by Liao et al. [11] and Liu et al. [12]. The application of MMC in the nasolacrimal duct appears to be safe.
The optimal dosage and exposure time of Mitomycin C is controversial. In the present study, 0.2 mg/ml was applied for 5 min, but in the study by You and Fang published in 2001 [13], they have compared the two Mitomycin C groups, one in which 0.2 mg/ml was applied in 16 patients while in the other group of 16 patients, 0.5 mg/ml was applied topically at the osteotomy site and found that there was no statistically significant difference between the two MMC groups. There is need for further randomized studies involving various dosage regimens and long term follow up visits would help to elucidate the optimum drug regimen.
The success rate in this study in the endonasal DCR group with Mitomycin C application was 97%. The reported success rates of DNA-dependant RNA synthesis with Mitomycin C varied between 77.3% and 99.2%. Our results in the endonasal DCR group are comparable to the studies of Camara (2000) [14] and Dolmetsch (2010) [15]. The success rate in this study in the external DCR group with Mitomycin C application was 100% while similar studies performed by Kao et al. (1997) [16] was 100% and Liao et al. (2000) [11] was 95.5%. This present study is the only randomized comparative study in which benefit of Mitomycin C application was assessed in both endonasal and external DCR groups.
In summary, intra-operative use of Mitomycin C in both endonasal DCR and external DCR is safe and effective in increasing the success rate and as a useful adjunct in DCR surgery. The use of Mitomycin C also enables endonasal DCR to have success rates almost comparable to external DCR.
References
- 1.Roozitalab MH, Amirahmadi M, Namazi MR. Results of the application of intraoperative Mitomycin C in dacryocystorhinostomy. Eur J Ophthalmology. 2004;14(6):461–463. doi: 10.1177/112067210401400602. [DOI] [PubMed] [Google Scholar]
- 2.Deka A, Bhattacharjee K, Bhuyan SK, et al. Effect of mitomycin C on ostium in dacryocystorhinostomy. Clin Experiment Ophthalmology. 2006;34:557–561. doi: 10.1111/j.1442-9071.2006.01265.x. [DOI] [PubMed] [Google Scholar]
- 3.Ugurbas SH, Zilelioglu G, Sargon MF, et al. Histopathologic effects of Mitomycin C on endoscopic transnasal dacryocystorhinostomy. Ophthalmic Surg Lasers. 1997;28:300–304. [PubMed] [Google Scholar]
- 4.Adrien S, Geetha T. External dacryocystorhinostomy—an end of an era. Br J Ophthalmol. 1997;81:716–717. doi: 10.1136/bjo.81.9.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosh S, Roychoudhury A, Roychaudhuri BK. Use of Mitomycin C in Endo–DCR. Indian J Otolaryngol. 2006;58(4):368–369. doi: 10.1007/BF03049597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zilelioglu G, Ugurbas SH, Anadolu Y, et al. Adjunctive use of mitomycin C on endoscopic lacrimal surgery. Br J Ophthalmol. 1998;82:63–66. doi: 10.1136/bjo.82.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh M, Jain V, et al. Intranasal endoscopic DCR (End-DCR) in cases of dacryocystitis. Indian J Otolaryngol. 2004;56(3):177–183. doi: 10.1007/BF02974345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linberg JV, Anderson RL, Bumsted RM, et al. Study of intranasal ostium in external dacryocystorhinostomy. Arch Ophthalmol. 1982;100:1758–1762. doi: 10.1001/archopht.1982.01030040738005. [DOI] [PubMed] [Google Scholar]
- 9.Rubinfield RS, Pfister RR, Stein RM, et al. Serious complications of topical mitomycin C after pterygium surgery. Ophthalmology. 1992;99:1647–1654. doi: 10.1016/s0161-6420(92)31749-x. [DOI] [PubMed] [Google Scholar]
- 10.Megevand GS, Salmon JF, Scholts RP, Murray AD. The effect of reducing the exposure time of Mitomycin C in glaucoma filtering surgery. Ophthalmology. 1995;102:84–90. doi: 10.1016/s0161-6420(95)31049-4. [DOI] [PubMed] [Google Scholar]
- 11.Liao SL, Kao SCS, et al. Results of intraoperative mitomycin C application in dacryocystorhinostomy. Br J Ophthalmol. 2000;84(8):903–906. doi: 10.1136/bjo.84.8.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu D, Bosley TM. Silicone nasolacrimal intubation with mitomycin C. A prospective, randomized, double-masked study. Ophthalmology. 2003;110:306–310. doi: 10.1016/S0161-6420(02)01751-7. [DOI] [PubMed] [Google Scholar]
- 13.You YA, Fang CT. Intraoperative mitomycin C in dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2001;17:172–177. doi: 10.1097/00002341-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Camara JG, Bengzon AU, Henson RD. The safety and efficacy of Mitomycin C in endonasal endoscopic laser-assisted dacryocystorhinostomy. Ophtal Plast Reconstr Surg. 2000;16:114–118. doi: 10.1097/00002341-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Dolmetsch AM. Nonlaser Endoscopic endonasal dacryocystorhinostomy with adjunctive Mitomycin C in nasolacrimal duct obstruction in adults. Ophthalmology. 2010;117:1037–1040. doi: 10.1016/j.ophtha.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 16.Kao SCS, Liao SL, et al. Dacryocystorhinostomy with intraoperative Mitomycin C. Ophthalmology. 1997;104:86–91. doi: 10.1016/S0161-6420(97)30357-1. [DOI] [PubMed] [Google Scholar]


