Abstract
Meningioma is the most common nonglial intracranial neoplasm, arising from meningocytes (arachnoid cap cells) of arachnoid granulation tissue and constitutes 15–20 % of all intracranial tumors. Approximately 6–17 % of all meningiomas can be found in extracranial or extra spinal sites. The head and neck is the most frequent location of extraneuraxial meningiomas, commonly seen as an extension of primary intracranial tumor (secondary extracranial meningioma). Less than 2 % of all meningiomas arise at a primary ectopic site (primary extracranial meningioma). Meningioma of nose and paranasal sinuses is a very rare tumor. The overall incidence is about 0.1 % of all tumors in the nose and sinuses. To date, very few cases of this primary extracranial meningioma of paranasal sinuses have been reported. In this report we are going to present three rare cases of primary extracranial meningioma of paranasal sinuses operated in our department over a period of 22 years (1986–2008).
Keywords: Meningioma, Tumor, Paranasal sinuses
Introduction
Meningiomas are considered to be one of the most common tumors of the central nervous system. Meningioma is the most common nonglial intracranial neoplasm, arising from meningocytes (arachnoid cap cells) of arachnoid granulation tissue and constitutes 15–20 % of all intracranial tumors [1]. These tumors are rarely found extra cranially, primarily in the head and neck region. Less than 2 % of all meningiomas arise at a primary ectopic site (primary extracranial meningioma) [2]. Farr et al. [3] reviewed 405 meningiomas and found that the most frequent location of extracranial meningiomas associated with an intracranial mass was the orbital cavity. Extracranial meningiomas have also been found in the ear, nose, paranasal sinuses, parotid, neck, pharynx, mandible, and skin [4].
Primary extracranial meningiomas can be defined as those not connected with an underlying meningioma of the neuraxis. Due to their rarity, one must exclude an extension from a central meningioma. The pathogenesis of primary extracranial meningioma is not completely established. It is postulated that meningocytes may become entrapped during closure of midline structures (fusion line inclusion), similar to the development of meningoceles [5]. Meningocytes can also be found around foramina of the skull or along perineural sheaths of cranial nerves and were found to have a predilection for areas of dural penetration by cranial nerves I, III, VII, IX, X, XI, and XII. In sites that are distant from cranial nerves and fusion lines, meningiomas might arise from metaplasia of undifferentiated mesenchymal cells [6].
Case 1
A 13 years female presented with swelling over medial canthus of Right (Rt) eye, proptosis and double vision of 2 months duration. She had complaints of nasal obstruction and rhinorrhoea, but no epistaxis. There was no complaint of diminished vision.
She was operated twice at Ahmedabad in a gap of 6 months duration and her last operation 8 months back for complaints of double vision, diminished vision, Rt eye proptosis with swelling above medial canthus of Rt eye. Histopathological examination showed the tumor to be meningioma. She had recurrence of tumor 4–5 months after each operation.
On examination, Rt eye proptosis with downward and outward shift was found. Also non-tender firm swelling of 1 cm size was found above and medial to medial canthus of Rt eye. Rt eye movements were restricted in superior and medial direction with diplopia, but with normal vision. Examination of nose, oral cavity and neck did not reveal any abnormality.
Rt frontoethmoidectomy was performed under general anesthesia. Tumor tissue was present in Rt and Lt frontal sinus and Rt ethmoid sinus. There was no evidence of intracranial extension or connection. Histopathological examination showed the structure of meningioma. The post operative recovery was normal. There were no complaints of diplopia and proptosis after 3 months of postoperative period. On follow up after 1 year no recurrence was seen and the patient is asymptomatic.
Case 2
Female, 45 years, presented with complaints of nasal obstruction of 3 years duration, initially unilateral, progressing to bilateral obstruction. Rt nasal mass with purulent foul smelling nasal discharge, spontaneous epistaxis, diminished vision on Rt side and Rt frontal headache. For last 7 months she noticed swelling over bridge of nose, nasolabial region with proptosis.
Examination of nose revealed an irregular mass occluding the whole nasal cavity with displacement of septum to opposite side with no nasopharyngeal extension and purulent foul smelling discharge. Examination of face showed a soft cystic swelling over Rt medial canthus of eye, extending over interpupillary line with skin hyper pigmentation. Rt eye was pushed laterally and outwards. Rt eye vision was 6/12. Rt ear showed changes of secretory otitis media. Examination of oral cavity and neck did not reveal any abnormality.
Erosion of medial wall of Rt maxillary sinus was seen along with destruction of Rt ethmoid labyrinth on radiological examination.
Biopsy from nasal mass was reported as meningioma.
On performing lateral rhinotomy under general anesthesia, tumor was seen occupying whole Rt nasal cavity, Rt ethmoid labyrinth, erosion of medial wall of Rt antrum, anterior wall of Rt sphenoid sinus (posterior wall was intact), nasal bones and erosion of medial wall of Rt orbit was found. Also posterosuperior part of nasal septum with a part of hard palate was eroded (the mucosa was free). There was no evidence of intracranial connection or extension.
The post operative recovery was normal. On follow up after 15 days, Rt eye was seen to be in normal position but the skin hyper pigmentation persisted.
On 8 months follow up, no recurrence was seen. The skin hyper pigmentation was markedly less. Otherwise the patient is asymptomatic.
Case 3
A 23 years female presented with painless swelling over left cheek since 1 year. It was insidious in onset and gradually increasing in size. There were no complaints of nasal obstruction or nasal discharge or epistaxis. There was history of some surgery done for the same complaint in Ujjain 4 months back (details were not available). Swelling was reduced initially, but recurred within a month. There was no complaint pertaining to vision.
On examination there was a 3 × 3 cm swelling present over left side of cheek extending from the inferior margin of left orbit up to the angle of mouth, laterally up to the zygoma. The swelling was bony hard in consistency, immobile, nontender, smooth surface with ill defined margins. On oral cavity examination there was bulge in the upper gingivobuccal sulcus on left side, with a scar over it. Anterior rhinoscopy examination revealed no abnormality. Ophthalmic examination was within normal limits. On telescopic examination of nose, no abnormality was detected.
Contrast enhanced CT Scan of paranasal sinuses was done. There was a large 5 × 4.5 × 3.4 cm hypo dense well enhancing lesion with thin bony wall noted in connection with root of premolars and canine on left side. Lesion expands into left maxillary sinus causing expansion of sinus wall as well. There is minimal extension of enhancing soft tissue into subcutaneous region just below the inferior orbital margin on left side. Post operative bone gap seen in anterior wall of maxillary sinus. Left frontal and ethmoidal sinuses revealed inflammatory opacification. Rt sided frontal, ethmoid, maxillary and sphenoid sinuses were clear. There was no intracranial extension of mass anywhere. Possibility of ameloblastoma, odontogenic keratocyst, dentigerous cyst were suggested (Fig. 1).
Fig. 1.
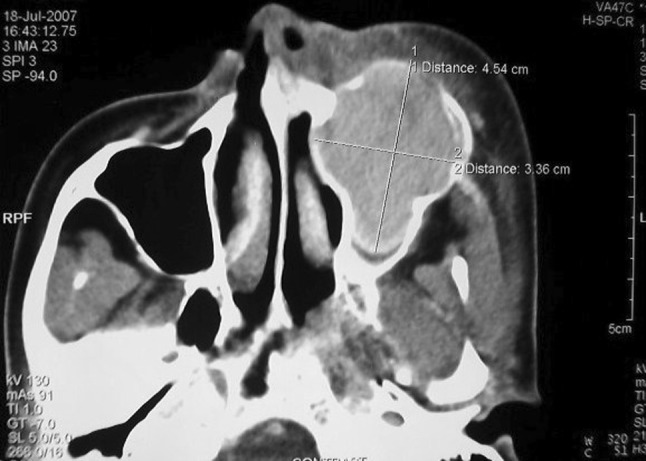
Pre-operative CT scan showing the extent of the tumor
Biopsy was taken by sublabial incision after knowledge about extension.
Histopathological study showed the histology of Meningioma.
Excision of the tumor was done by left lateral rhinotomy approach.
Tumor reached and separated from the surrounding tissue and periosteum through blunt dissection. Swelling was easily separable from the surrounding tissue, except on the inferolateral aspect where fibrous adhesions were present. Tumor was removed in toto and sent for histopathology (Fig. 2).
Fig. 2.

Excised tumor mass
Her postoperative period was uneventful. Postoperatively there was no visible swelling. The healing was good. The histopathological report of the final excised specimen was reported as a fibroblastic meningioma. Six months after on routine follow up there was no evidence of recurrence.
Discussion
The tumor can occur in patients with age group ranging from 2nd to 7th decade. Patients usually presents with nasal obstruction, nasal mass, proptosis, epiphora, pain and occasionally epistaxis. The common sites of primary origin described are nose [7], maxillary sinus [7] and frontal sinus [7]. The ethmoid sinus can also be involved but sphenoid sinus involvement is uncommon. The precise site of origin varies, many tumors take origin in the orbit or intracranial cavity. The primary orbital tumor and intracranial tumors may extend into the antrum or into the ethmoid sinuses.
Atherio et al. [8] classified extracranial meningiomas into four groups:
Primary extracranial meningiomas extending from the skull.
Extracranial meningioma arising from arachnoid cell rests of cranial nerve sheaths.
Meningiomas having no demonstrable connection with foramina or cranial nerves.
Metastasis of malignant intracranial meningiomas.
No particular cause of these tumors has been identified. Ultra- structural studies have demonstrated similarity between the so called meningothelial cells and the normal arachnoid cells which confirms the concept of arachnoid origin but Schmidtman has postulated possible endothelial origin. Atherio et al. [8] describe the intracranial origin with subsequent extension of these tumors, while Lopez [5] believes that primary meningiomas in nose and sinuses arise from arachnoid cells that have migrated in the nerve sheaths and even become detached during development. Some believe the origin of these tumors is from the multipotent meningothelial cell with ectodermal and mesodermal characteristics with ability to produce collagen.
These tumors are of rubbery consistency and may appear like simple polyps.
Histologically, meningiomas are divided into different histological subtypes according to the predominant cellular morphology, such as meningothelial (syncytial), fibrous (fibroblastic), psammomatous, angiomatous (angioblastic), and transitional (mixed). The majority of extracranial meningiomas of the paranasal sinuses have been syncytial [9].
The syncytial type consists of polyhedral cells with “endothiliomatous” pattern. The transitional type consists of whorls of spindle cells surrounded by fibrous tissue. These whorls may have central vessels or hyalinized or calcified collagen producing psammoma bodies. The fibroblastic form is composed of bundles of spindle cells with intervening collagen with psammoma bodies. The angioblastic form resembles hemangiopericytoma. So it may be excluded from meningioma group (Fig. 3).
Fig. 3.
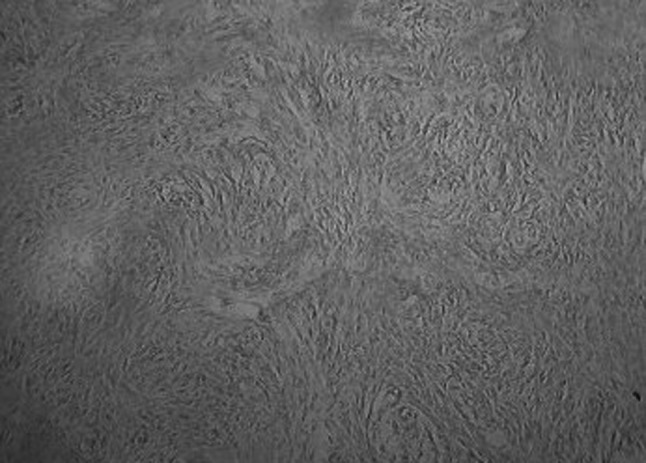
Histopathology of the excised tissue showing the microscopic features of meningioma
The ultra structure of meningioma shows two types of cells with rounded or oral and elongated nuclei in spindle type. Immunohistochemical studies are indispensable in the differential diagnosis of primary extracranial meningiomas from other benign tumors of peripheral nerve origin. The positive expression of EMA and vimentin antigen demonstrates the dual epithelial and mesenchymal characteristics of the cells found in these tumors.
Treatment of primary extracranial meningioma is surgical excision because meningiomas are known to be radio resistant and recurrence is very rare following adequate surgical resection [10].
Most meningiomas are benign with no tendency to metastasize but they can cause pressure erosion and spread from one cavity to another. Malignant change is rare. Cases have been reported as surviving up to 30 years. It is important to watch for evidence of intracranial involvement which may give rise to epilepsy.
References
- 1.Leestma JE. Brain tumors. Am J Pathol. 1980;100:239–316. [PMC free article] [PubMed] [Google Scholar]
- 2.Friedmann CD, Costantino PD, Tietelbaum B, et al. Primary extracranial meningiomas of the head and neck. Laryngoscope. 1990;100:41–48. doi: 10.1288/00005537-199001000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Farr HW, Gray GF, Jr, Vrana M, Panio M. Extracranial meningioma. J Surg Oncol. 1973;5:411–420. doi: 10.1002/jso.2930050503. [DOI] [PubMed] [Google Scholar]
- 4.Landini G, Kitano M. Meningioma of the mandible. Cancer. 1992;69:2917–2920. doi: 10.1002/1097-0142(19920615)69:12<2917::AID-CNCR2820691209>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 5.Lopez DA, Silvers DN, Helwig EB. Cutaneous meningiomas: a clinicopathological study. Cancer. 1974;32:728–744. doi: 10.1002/1097-0142(197409)34:3<728::AID-CNCR2820340332>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 6.Papini MA, Chantelli R, Contini D, et al. Nasal meningioma: report of a case. Acta Otorhinolaryngol Belg. 1988;42:40–44. [PubMed] [Google Scholar]
- 7.Friedmann I, Osborn DA (1982) Pathology of granulomas and neoplasms of the nose and paranasal sinuses. Churchill Livingstone, Edinburgh, pp 118–132
- 8.Atherio CCT, Garcia R, Lopes LJ. Ectopic meningioma of the nose and paranasal sinuses (report of a case) J Laryngol Otol. 1985;99:1161–1166. doi: 10.1017/S0022215100098340. [DOI] [PubMed] [Google Scholar]
- 9.Ho K. Primary meningioma of the nasal cavity and paranasal sinuses. Cancer. 1980;46:1442–1447. doi: 10.1002/1097-0142(19800915)46:6<1442::AID-CNCR2820460625>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 10.Perzin KH. Nonepithelial tumors of the nasal cavity, paranasal sinuses and nasopharynx. XIII: meningiomas. Cancer. 1984;54:1860–1869. doi: 10.1002/1097-0142(19841101)54:9<1860::AID-CNCR2820540916>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]


