Abstract
Nasal turbinate hypertrophy is a major cause of nasal airway obstruction that affects up to 20% of the European general population. This study aims to determine the efficacy of radiofrequency treatment as perceived by patients during a 2-years period. From 2007 to 2009, an observational study was conducted on 36 patients who consecutively underwent temperature-controlled radiofrequency tissue volume reduction. A questionnaire was administered to each patient in order to collect demographic data, lifestyle habits, health status and visual analogue scale (VAS) score of perceived symptoms. Mean VAS scores of nasal obstruction, headache, rhinorrhoea and anosmia after treatment were significantly lower than that at baseline. Urban residence and allergic rhinitis were significantly associated with lower mean improvement (2.9 vs. 5.6; P = 0.04 and 2.3 vs. 5.3; P = 0.01, respectively). A non significant association with scarce nasal obstruction improvement was present in older aged patients, in patients other than students and in active and passive smokers. Our data enrich the general knowledge on radiofrequency treatment of turbinate hypertrophy identifying the rate of long-term efficacy of radiofrequency treatment as perceived by patients and focusing on several risk factors involved in patient prognosis after treatment.
Keywords: Turbinate, Radiofrequency, Nasal obstruction, Tissue reduction
Introduction
Nasal turbinate hypertrophy is a major cause of nasal airway obstruction that affects up to 20% of the European general population [1]. Although vasomotor deregulation may be an important factor in its pathogenesis, turbinate hypertrophy can be strictly associated to allergic or not allergic rhinitis [2, 3]. The blockage of nasal breathing is usually the main symptom but people may also experience sleep apnea, rhinorrhoea, headache, anosmia and discomfort. Moreover, its medical therapy only slightly improves the health status of patients and chronic therapy exposes to high risk of undesirable iatrogenic effects due to local consumption of decongestants [1]. When conservative medical therapy is not effective in controlling nasal obstruction, surgical reduction can be considered an alternative method to open nasal airway. At date, a large variety of surgical procedures are available but none of these achieve a worldwide consensus and have proved to be effective long-term [4–6]. During the last decade, temperature-controlled radiofrequency tissue volume reduction (TCRFTVR) has been introduced and promoted for the treatment of turbinate hypertrophy [7]. The aim of this study was to determine the rate of long-term efficacy of radiofrequency treatment as perceived by patients, identifying factors involved in a positive prognosis.
Methods
The study was conducted during a 2-years period on 36 patients who consecutively underwent TCRFTVR at the Otorhinolaryngoiatric Clinic of the University of Palermo. All enrolled patients had turbinate hypertrophy, symptoms or signs of nasal obstruction and were non responders to medical therapy. Patients with previous nasal surgery, septal deformity, nasal polyposis or sinusitis or history of cancer of upper respiratory tract were excluded from the study. A questionnaire was developed and validated in order to standardize the data recording. During the study period (from 2007 to 2009) the implemented questionnaire was submitted to each participant. The questionnaire was structured by considering three main sections. A first part of the questionnaire investigated demographic data (profession, sex, age and residence), lifestyle habits (active and passive smoking, oral contraceptive consumption and history of nasal decongestants consumption) and health status (diabetes, hypertension and allergic rhinitis). In a second section of the questionnaire, a series of questions (n = 18) were asked regarding the main symptoms perceived by patients. Symptom investigation assessed nasal obstruction, rhinorrhoea, anosmia and headache. Moreover, nasal obstruction was investigated by arbitrarily distinguishing between obstruction experienced during day-time (from 8 am to 22.00 pm) and during night-time (from 23.00 pm to 7.00 am). In order to determine the intensity of each symptom, a standard visual analogue scale (VAS) ranging from zero (no symptom) to ten (the most severe symptom) was used in the questionnaire. Patients were asked to position a cross on a line corresponding to their own perception of each symptom. Questionnaire data were collected before treatment, immediately after intervention (approximately after 1 month) and, finally, at the end of 2 years following the TCRFTVR. All data were validated in order to guaranty the accuracy of requested information. Validation was conducted by assessing the concordance between obtained measures and medical history reported on the sanitary cartel of subjects included in the study. Data with evident discrepancies were discarded and not considered for statistical analysis. According to international literature [8], a reduction of nasal obstruction lesser than 0.7 cm was considered as absence of clinically important improvement in health status (treatment failure). Moreover, after completion of questionnaire, a surgeon not involved in treatment endoscopically graded turbinate hypertrophy as absent, mild, moderate or severe. Hypertrophy was classified in four grades by using the percentage of engorgement of nasal fossa: mild (when 25% of the nasal fossa was occupied), moderate (when 50% of the nasal fossa was occupied) and severe (75% or more of the nasal fossa was occupied). These latter data were included in the third section of the questionnaire.
TCRFTVR was performed using a radiofrequency generator (Surgitron, Ellman International, Inc., Hewlett, NY) set at bipolar coagulation mode and producing high frequency current (4 MHz) but low temperature energy. No vasocostrictive agent was used topically or by injection to avoid turbinate shrinkage. The bipolar radiofrequency electrode was inserted submucosally and the energy was delivered to three different sites of each turbinate (to the anterior, middle and posterior portions). The energy delivery was stopped once whitening the applied region of the mucosa. No packaging was used, and no antibiotic therapy.
All the statistical analysis were performed by using R statistical software package 2.8.1 version. P-value lesser than 0.05 was considered statistically significant. Categorical variables were expressed as number and percentages and were analyzed using the Pearson χ2 test or Fisher’s exact test if the number of observations per cell was <5. Continuous data were presented as mean ± standard deviation and comparison between groups were performed with the Student t test. Continuous repeated measures obtained at baseline, 1 month and 2 years were compared with the paired Student t test or with one-way ANOVA for repeated measures.
Results
Table 1 presents the sociodemographic characteristics, lifestyle habits and health status of patients who underwent to radiofrequency treatment. Men (n = 18) and women (n = 18) were equally distributed. The two groups showed a similar average age they were not significantly different in terms of urban residence (50 vs. 61.1%), profession (33.3 vs. 16.7% were students), active smoking (27.8 vs. 27.8%), passive smoking (11.1 vs. 27.8%), diabetes (0 vs. 5.6%), allergic rhinitis (44.4 vs. 44.4%) and hypertension (5.6 vs. 5.6%).
Table 1.
Sociodemographic characteristics, lifestyle habits and health status of patients who underwent to radiofrequency treatment
| Men (n = 18) | Women (n = 18) | P-value | |
|---|---|---|---|
| Mean age ± SD (in years) | 38.7 ± 19.7 | 39.7 ± 16 | 0.86 |
| Urban residence (%) | 9 (50.0) | 11 (61.1) | 0.73 |
| Profession: student (%) | 6 (33.3) | 3 (16.7) | 0.44 |
| Active smoking (%) | 5 (27.8) | 5 (27.8) | 1 |
| Passive smoking (%) | 2 (11.1) | 5 (27.8) | 0.40 |
| Diabetes (%) | 0 (0) | 1 (5.6) | 1 |
| Allergic rhinitis (%) | 8 (44.4) | 8 (44.4) | 1 |
| Hypertension (%) | 1 (5.6) | 1 (5.6) | 1 |
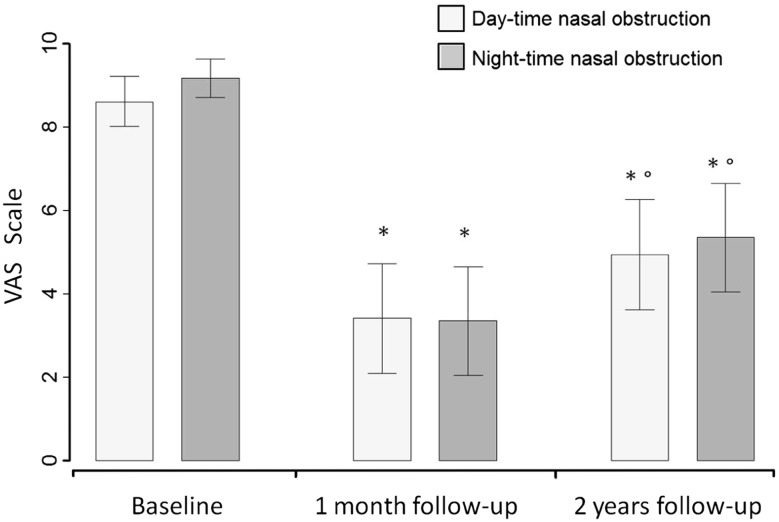
Figure 1 depicts the trend of day-time and night-time VAS score of nasal obstruction recorded at three different times. At 1 month, a significant reduction was evident in both day-time and night-time VAS scores with respect to baseline (3.4 vs. 8.6; P < 0.001 and 3.3 vs. 9.2; P < 0.001, respectively). Similarly, also at 2 years means VAS values were significantly lower than at baseline (4.9 vs. 8.6; P < 0.001 during the day and 5.3 vs. 9.2; P < 0.001 during the night). Moreover, a slight significant increase in VAS scores was present at 2 years versus 1 month in both daytime (4.9 vs. 3.4; P < 0.05) and night-time (5.3 vs. 3.4; P < 0.01).
Fig. 1.
Average VAS and 95% CIs of the degree of day-time and night-time nasal obstruction at baseline, 1 month follow-up and 2 years follow-up. *P < 0.01 with respect to baseline. °P < 0.05 with respect to 1 month follow-up
Table 2 summarizes statistical associations between VAS score nasal obstruction improvement and variables examined by questionnaire. Urban residence and allergic rhinitis were significantly associated with lower mean improvement (2.9 vs. 5.6; P = 0.04 and 2.3 vs. 5.3; P = 0.01, respectively).
Table 2.
Univariate statistical analysis between VAS score nasal obstruction improvement and variables examined by questionnaire
| Variable | VAS score nasal obstruction improvementa | P-value |
|---|---|---|
| Age in years | ||
| ≤30 | 4.4 | 0.89 |
| 31–60 | 3.8 | |
| >61 | 3.6 | |
| Sex | ||
| Males | 4.0 | 0.98 |
| Females | 4.0 | |
| Residence | ||
| Urban | 2.9 | 0.04 |
| Others | 5.6 | |
| Profession | ||
| Students | 5.7 | 0.14 |
| Others | 3.4 | |
| Active smoking | ||
| Yes | 3.5 | 0.63 |
| No | 4.2 | |
| Passive smoking | ||
| Yes | 3.7 | 0.82 |
| No | 4.1 | |
| Allergic rhinitis | ||
| Yes | 2.3 | 0.01 |
| No | 5.3 | |
aVAS score nasal obstruction at baseline minus VAS score nasal obstruction at 2 years follow-up
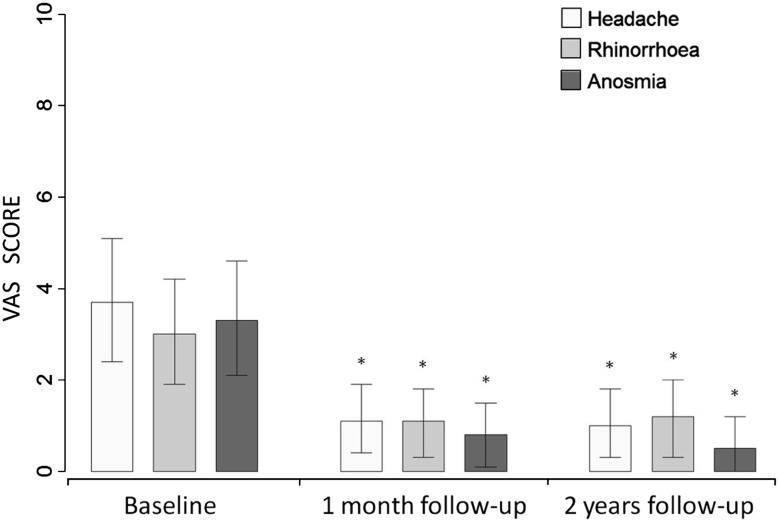
A non significant association with scarce nasal obstruction improvement has been shown in older aged patients (3.6 in older than 60 years vs. 3.8 in 31–60 years old vs. 4.4 in younger than 30 years old), in not students (3.4 vs. 5.7) and in active and passive smokers (3.5 vs. 4.2 and 3.7 vs. 4.1, respectively). None difference was attributable to sex. Moreover, considering 0.7 cm as the minimal clinically evident improvement at 2 years, 10 out from 36 patients (27.8%) did not modify their preoperative conditions (data not shown). Mean VAS scores and their 95% CI of headache, rhinorrhoea and anosmia at baseline, 1 month and 2 years are showed in Fig. 2. All these symptoms have been characterized by mean VAS values strongly lower then that observed in day-time and night-time nasal obstruction.
Fig. 2.
VAS average and 95% CIs of the degree of headache, rhinorrhoea and anosmia at baseline, 1 month follow-up and 2 years follow-up. *P < 0.01 with respect to baseline
Significant decreases from baseline to 1 month were present in both headache (3.7 vs. 1.1; P < 0.001) and rhinorrhoea (3 vs. 1.1; P < 0.001) and anosmia (3.3 vs. 0.8; P < 0.001).
The early postoperative conditions were also maintained at 2 years and none significant difference was observed with respect to 1 month after treatment.
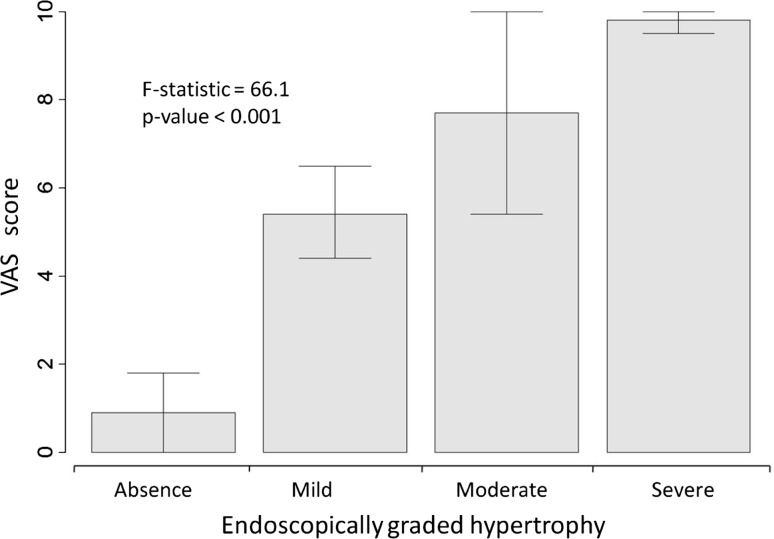
Finally, the relation between VAS score nasal obstruction and hypertrophy endoscopically graded at 2 years is depicted in Fig. 3.
Fig. 3.
VAS average and 95% CIs of the degree of nasal obstruction stratified by endoscopically graded hypertrophy
As evident, higher VAS score nasal blockage was strictly and significantly associated (F-statistic = 66.1, P < 0.001) with growing endoscopic grades of turbinate hypertrophy (0.9 when absent, 5.4 when mild, 7.7 when moderate and 9.8 when severe).
Discussion
The present study was mainly designed to assess the efficacy of radiofrequency treatment in reducing patient disease perception over 2 years after treatment. As suggested by international literature [1, 9], our results showed that nasal airway obstruction represented the main symptom experienced by patients as consequence of turbinate hypertrophy. Patients with important day-time nasal blockage were more likely to be affected by similar night-time nasal blockage, showing a high correlation between two symptoms. Moreover, an evident and statistically significant postoperative improvement in feeling of both day-time and night-time nasal obstruction was evident in our study. A reduction of nasal obstruction after treatment was already reported by other authors [7, 9–11] but modestly lower percentage of patients with clinically relevant nasal obstruction improvement was reported in our experience than in previous studies.
This modest difference in postoperative evolution may be explained by considering the different prevalence of risk factors in populations from different geographic areas. In this way, our data suggest that nasal obstruction improvement, as perceived by patients, is statistically significantly affected by allergic rhinitis and urban residence. The presence of these risk factors is well linked to worse prognosis in nasal blockage improvement but also age or smoke exposition could be interested in similar consideration. These last risk factors did not reach significance but older patients and active or passive smokers had lower VAS score improvements after treatment. Unfortunately, the population study size was not larger enough in order to exhaustively investigate all risk factors involving with post-operative symptom perception.
Among lesser common symptoms, headache, rhinorrhoea and anosmia showed VAS scores lower than those reported for breathing obstruction.
Finally, the major limitations of the present study are its small size and a large use of self-reported data. However, several authors [12, 13] reported that more objective measures of the nasal obstruction improvement, such as rhinomanometry, have often been inconsistent with subjective assessment and that the success of treatment is primarily based on patient’s feelings and satisfaction. In addition, the surprising linkage of endoscopically graded turbinate hypertrophy and nasal obstruction VAS score suggests a larger and objective validity of subjective observations. Our experience may be of scientific interest suggesting future investigations on a topic still not well-known, assessing the influence of several risk factors involved in patient prognosis after treatment. These last variables could have an important predictive role in choosing patients for whom radiofrequency treatment would truly be of benefit. In this way, our data enrich the general knowledge on radiofrequency treatment of turbinate hypertrophy focusing on patient point of view as the main responsible of the surgical intervention.
Key Messages
A large variety of surgical procedures are available to reduce nasal turbinate hypertrophy but none of these achieve a worldwide consensus and have proved to be effective long-term.
An evident and statistically significant postoperative improvement in feeling of both day-time and night-time nasal obstruction was evident in our study.
Modestly lower percentage of patients with clinically relevant nasal obstruction improvement was reported in our experience than in previous studies.
Several risk factors may be useful in identifying patients at particularly high risk of treatment failure.
Acknowledgments
Conflict of interest
None declared.
Footnotes
All authors have equally contributed to this paper and approved the manuscript.
References
- 1.Cavaliere M, Mottola G, Iemma M. Comparison of the effectiveness and safety of radiofrequency turbinoplasty and traditional surgical technique in treatment of inferior turbinate hypertrophy. Otolaryngol Head Neck Surg. 2005;133(6):972–978. doi: 10.1016/j.otohns.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Lippert BM, Werner JA. Nd:YAG laser light-induced reduction of nasal turbinates. Laryngorhinootologie. 1996;75:523–528. doi: 10.1055/s-2007-997626. [DOI] [PubMed] [Google Scholar]
- 3.Ottaviani F, Capaccio P, Cesana BM, Manzo R, Peri A. Argon plasma coagulation in the treatment of nonallergic hypertrophic inferior nasal turbinates. Am J Otolaryngol. 2003;24:306–310. doi: 10.1016/S0196-0709(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 4.Friedman M, Tanyeri H, Lim J, Landsberg R, Caldarelli D. A safe, alternative technique for inferior turbinate reduction. Laryngoscope. 2000;109:1834–1837. doi: 10.1097/00005537-199911000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Jackson LE, Koch RJ. Controversies in the management of inferior turbinate hypertrophy: a comprehensive review. Plast Reconstr Surg. 1999;103:300–312. doi: 10.1097/00006534-199901000-00049. [DOI] [PubMed] [Google Scholar]
- 6.Sapci T, Sahin B, Karavus A, Akbulut UG. Comparison of the effects of radiofrequency tissue ablation, CO2 laser ablation, and partial turbinectomy applications on nasal mucociliary functions. Laryngoscope. 2003;13(3):514–519. doi: 10.1097/00005537-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Coste A, Yona L, Blumen M, Louis B, Zerah F, Rugina M, et al. Radiofrequency is a safe and effective treatment of turbinate hypertrophy. Laryngoscope. 2001;111:894–899. doi: 10.1097/00005537-200105000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Powell NB, Zonato AI, Weaver EM, Li K, Troell R, Riley RW, Guilleminault C. Radiofrequency treatment of turbinate hypertrophy in subjects using continuous positive airway pressure: a randomized, double-blind, placebo-controlled clinical pilot trial. Laryngoscope. 2001;111(10):1783–1790. doi: 10.1097/00005537-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Harsten G. How we do it: radiofrequency-turbinectomy for nasal obstruction symptoms. Clin Otolaryngol. 2005;30(1):64–66. doi: 10.1111/j.1365-2273.2004.00941.x. [DOI] [PubMed] [Google Scholar]
- 10.Li KK, Powell NB, Riley RW, Troell R, Guilleminault C. Radiofrequency volumetric tissue reduction for the treatment of turbinate hypertrophy: a pilot study. Otolaryngol Head Neck Surg. 1998;119(6):569–573. doi: 10.1016/S0194-5998(98)70013-0. [DOI] [PubMed] [Google Scholar]
- 11.Rhee CS, Kim DY, Won TB, Lee HJ, Park SW, Kwon TY, et al. Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. Laryngoscope. 2001;111:153–158. doi: 10.1097/00005537-200101000-00026. [DOI] [PubMed] [Google Scholar]
- 12.Utley DS, Goode RL, Hakim I. Radiofrequency energy tissue ablation for the treatment of nasal obstruction secondary to turbinate hypertrophy. Laryngoscope. 1999;109:683–686. doi: 10.1097/00005537-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Kim CS, Moon BK, Jung DH. Correlation between nasal obstruction symptoms and objective parameters of acoustic rhinometry and rhinomanometry. Auris Nasus Larynx. 1998;25:45–48. doi: 10.1016/S0385-8146(97)10011-6. [DOI] [PubMed] [Google Scholar]