In summary, it has become evident that multiple factors can affect sperm counts and quality. Most reports indicate that there has not been a worldwide decrease in sperm counts over the past 20 or 50 years, and the validity of the endocrine disruptor hypothesis or testicular dysgenesis syndrome with respect to sperm counts is highly questionable.
Background
My research program in the 1970–1990 period was primarily focused on the chemistry, toxicology and mechanisms of action of highly persistent organochlorine environmental contaminants including the polychlorinated biphenyls (PCBs), dibenzofurans and dibenzo-p-dioxins (Figure 1). Since environmental samples and human residues of these organohalogen compounds (OCs) (or persistent organic pollutants) are complex mixtures of PCB, polychlorinated dibenzofuran and polychlorinated dibenzo-p-dioxin isomers and congeners, my laboratory initially focused on structure–activity and quantitative structure–activity relationships among these compounds.1,2,3 2,3,7,8-tetrachlorodibenzo-p-dioxin was identified as the most toxic OC, and Poland and co-workers4,5 initially hypothesized and demonstrated that 2,3,7,8-tetrachlorodibenzo-p-dioxin and related compounds induce their toxic responses through activation of the aryl hydrocarbon receptor (AHR). Our quantitative structure–activity relationship studies contributed to development of the toxic equivalence factor approach for hazard assessment of OC mixtures which has been adopted by the World Health Organization and regulatory agencies worldwide to regulate and decrease emissions of OCs from multiple sources.1,2,3,6,7 In the early 1990s, we began to investigate the molecular biology and toxicology of AHR-mediated inhibition of estrogen receptor (ER) signalling and the complex mechanisms of inhibitory AHR–ER cross-talk were determined.8,9,10,11,12 These studies were an example of antiestrogenic endocrine disruption by AHR agonists.
Figure 1.
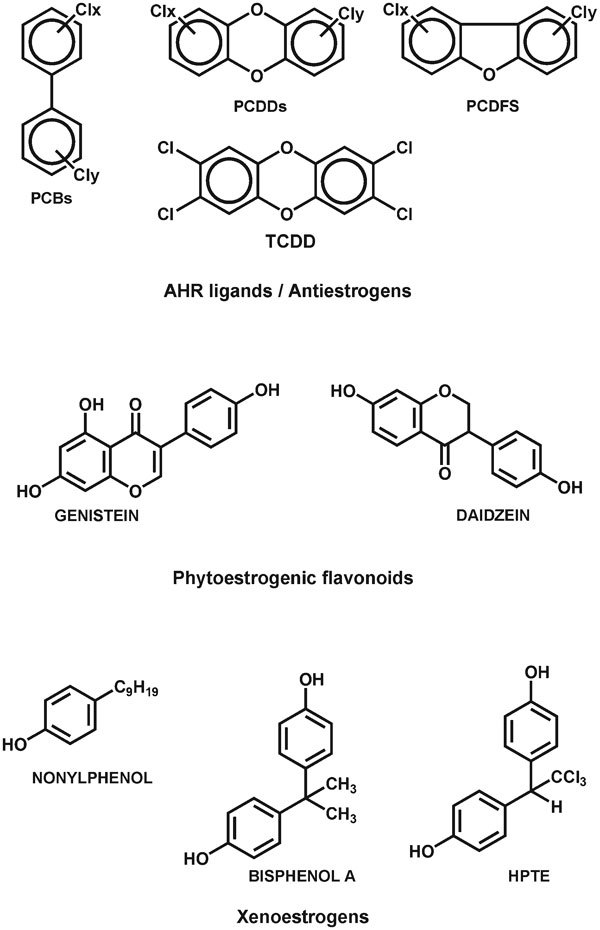
Structures of diverse endocrine disruptors that modulate estrogen signaling. AHR, aryl hydrocarbon receptor; HPTE, 2,2-bis(p-hydroxyphenyl)-1,1,1-trichloroethane; PCB, polychlorinated biphenyl; PCDD, polychlorinated dibenzo-p-dioxin; PCDF, polychlorinated dibenzofuran; TCDD, 2,3,7,8-tetrachlorodibenzo-p-dioxin.
The endocrine disruptor hypothesis
On the basis of this background of studies on environmental antiestrogens coupled with the reported chemoprotective effects of flavonoids which exhibit estrogenic and potential antiestrogenic activity, I was intrigued by the new hypotheses on the potential adverse health effects of endocrine-disrupting compounds (EDCs). Sharpe and Skakkebaek13 published a hypothesis in Lancet entitled ‘Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract' in 1993 and the major basis for this hypothesis was the meta-analysis which reported that among 14 947 men included in 61 studies published between 1938 and 1991, there was a 40% decrease in mean sperm counts from 113×106 to 66×106 ml−1.14
In addition, this hypothesis was also linked to other disorders of the male reproductive such as testicular cancer, cryptorchidism and hypospadias which were also increasing and it was suggested that ‘these abnormalities and reduced sperm counts may have a common etiology'.13 Support for this statement was derived, in part, from the devastating effects of the potent estrogenic drug diethylstilbestrol which was prescribed for pregnant women and resulted in multiple adverse effects on the reproductive tracts of male and female offspring.15,16,17 The observations with diethylstilbestrol led to the hypothesis that ‘the increasing incidence of reproductive tract abnormalities in the human male may be related to increased oestrogen exposure in utero'.13 This hypothesis was extended to breast cancer since two small studies showed that levels of PCB or 1,1-bis(p-chlorophenyl)ethylene (DDE) were increased in breast cancer patients vs. controls.18,19 The breast cancer hypothesis implicating estrogenic EDCs as causal agents20 was less specific with respect to the timing of estrogen exposure but was supported by the fact that a woman's lifetime exposure to estrogens is a known risk factor for this disease.
Under the subheading ‘male sexual development in a sea of oestrogen', there were several letters published in the July 10 issue of Lancet which provided support for the EDC hypothesis and one letter pointing out that we also live in a sea of potential antiestrogens which include not only the OC environmental contaminants but also polynuclear aromatic hydrocarbons and ‘natural products in foods such as flavonoids and indole-derived compounds which bind the AHR probably also show antoestrogenic activity'.21 The estrogenic endocrine disruptor hypothesis was supported by many scientists and was strengthened by environmental studies which showed the estrogenization of male fish in many river systems, the decreased penis size of alligators in Lake Apopka and the identification of an increasingly large number of industrial and cosmetic (personal care) products or chemicals including bisphenol-A (BPA) that were estrogenic.22,23,24,25 Popular magazines such as the New Yorker, scientific books such as Our Stolen Future and television programs in Europe and North America warned the population of the impending crisis, and, on the basis of the diminished size of alligator penises, a US Congressional committee was informed that we are not half the men our fathers were!
Involvement in the EDC controversies
My involvement in the EDC hypothesis was primarily focused on monitoring results of a myriad of studies focused on testing or confirming the hypothesis that environmental (and dietary) estrogens were playing a role in the increased incidence of male reproductive tract problems and breast cancer among women. I wrote several review articles26,27,28,29,30 and attended many symposia on EDCs as the dissenting or sceptical voice and also initiated several research projects in this field. My initial research on the possible role of xenoestrogens and flavonoids as tissue-specific selective estrogen receptor modulators (SERMs) (i.e., ER agonists or antagonists) was funded by the Chemical Manufacturers' Association (CMA) (now the American Chemistry Council) and later by the National Institutes for Environmental Health Sciences. The CMA funding during the mid-1990s supported some of our early research31 and, although ‘consulting' money was not provided, the source of the funds was later used in attempts to discredit my impartiality as a critic of the EDC hypothesis. The CMA leadership and their employees never influenced my research or its interpretation and I naively believed at the time that for scientists, the source of funding was not a factor. There are now many examples of how funding sources have influenced the science and I always indicate possible conflicts and contribute my infrequent consulting money to Texas A&M University. My research on EDCs has continued to the present day and has primarily been focused on demonstrating that industrial and dietary estrogenic compounds are SERMs and predicting their tissue-specific ER agonist or antagonist activities can only be ascertained by doing the experiments.32,33,34,35,36,37 Assays determining ER binding or transactivation are useful but do not predict SERM-like activity, and our results actually support, in part, the EDC hypothesis where it can be hypothesized that a so-called ‘weak' estrogen such as BPA may be more potent in some tissues during specific periods of development. In collaboration with Drs Kevin Gaido (Chemical Industry Institute of Toxicology), Donald McDonnell (Duke University) and Ken Korach (National Institutes for Environmental Health Sciences), we also showed that interactions of several environmental estrogens were additive38,39 and this refuted a paper in Science claiming ‘synergistic' interactions of environmental estrogens.40 This discovery of synergistic activity for some estrogenic EDCs was covered by the news media worldwide; however, our results and the subsequent retraction of the Science paper were barely mentioned in the press.
EDCs and male reproductive tract problems
The publication of the meta-analysis study14 prompted similar retrospective studies on sperm counts and sperm quality in many countries and regions, and one of the first studies analyzed sperm counts from a sperm bank in Paris. Sperm concentrations from 1351 donors (to a sperm bank) decreased from 89×106 to 60×106 ml−1 from 1973 to 1992, suggesting a downward trend.41 However, a subsequent study using similar methods of analysis showed that from 1977 to 1992, sperm concentrations in the Toulouse area were 83.12×106 ml−1 and did not vary over the time period.42 Subsequent studies in multiple locations showed both decreases in sperm counts or no change, and it was clear that the high variability was due to many factors, including sampling and measurement techniques, seasonal variability, body mass index of the donors and many other lifestyle or personal factors that can affect sperm counts. One of the most striking variables that could not be addressed in the 1992 meta-analysis study was body mass index where it has now been shown that high or low body mass has remarkable effects on sperm counts and quality.43,44 Another important variable that was also not accounted for was the regional differences in sperm counts which were observed in Europe and North America. Fisch and co-workers45 investigated sperm concentrations from vasectomy clinics in New York, Minnesota and California, and mean sperm counts were 131.5×106, 100.8×106 and 72.7×106 ml−1 respectively, and these values were not significantly changed over the 1970–1994 period of collection Regional variability was also observed in sperm concentrations from 11 different clinics across Canada where sperm counts ranged from 51×106 to 121×106 ml−1 in 1984 and 43×106 to 137×106 ml−1 in 1996.46 Handelsman47 also reported high variability in sperm concentrations (142×106–63×106 ml−1) from five different groups of volunteers in the area of Sydney Australia taken over an 8-year span (1987–1994). These patients were volunteers and were not vasectomy patients or sperm donors, and Handelsman47 concluded that ‘this highlights the invalidity of extrapolating such findings on sperm output of self-selected volunteers to the general male community from which the volunteers originated'. The concern regarding the global decrease in sperm counts espoused by Skakkebaek and some of his collaborators in Denmark has spurred studies to understand what is happening by examining Danish military recruits. Among the five thousand 18- to 20-year-old men who provided semen samples from 1996 to 2010, sperm concentrations exhibited median values from 50×106 to 45×106 ml−1 and there was no evidence for significant variations over the 15-year period.48 Similar results were observed in a Swedish study,49 whereas a decrease in sperm counts was observed in a sample of 858 Finnish men during 1998–2006.50 The series of three Scandinavian studies have been controversial with personal and professional undertones which have been accompanied by letters to the editor and commentaries. The large cohort and duration of the Danish study strongly suggest that exposures to EDCs 18–20 years prior to 1996–2010 have not changed over the 15 years of the study and this does not support the hypothesis that sperm counts are decreasing. While the Finnish studies are interesting and the effects appear to be localized or regionalized, the conclusions of Jorgensen, Skakkebaek and their co-workers, namely that ‘these simultaneously and rapidly occurring adverse trends suggest that the underlying causes are environmental and, as such, preventable'50 is not scientifically justified nor consistent with similar trends in environmental contaminant levels in Finland or the other Scandinavian countries.
One of the key missing ingredients in the endocrine disruptor hypothesis has been the lack of any correlations between sperm count changes and in utero exposure to estrogenic compounds. It was also hypothesized that the antiandrogen DDE might also be an important contributor to male reproductive tract problems.51 However, the increasing incidence of testicular cancer in Scandinavia and other Western countries is inversely correlated with DDE levels (in breast milk) which have decreased dramatically owing to banning or use restrictions in most countries.52 Results of twin studies showing higher rates of testicular cancer in dizogytic than monozygotic twins correlate with higher maternal (and in utero) levels of estrogen and support a role for estrogen as a risk factor for testicular cancer.53 However, a study with singletons, di- and monozygotic twins did not show any differences in their sperm counts in these groups of men.54 It was concluded that ‘higher prenatal concentrations of oestrogen are not related to reduced sperm counts in adulthood'.54 These results do not support a role for in utero exposure to steroidal-type estrogens in mediating a decrease in sperm counts but do not exclude the possibilities that some, as yet unidentified SERM, may be involved. However, on the basis of historical and more recent data, it seems unlikely that there is a worldwide decrease in sperm counts although it is possible that some regional problems with unknown etiologies may exist. While it is known that estrogens are a risk factor for hypospadias and cryptorchidism, it is also unclear if these reproductive tract disorders are increasing. For example, a study on international trends for both problems showed large regional variability and increases in hypospadias ‘leveled off in many systems after 1985' and since 1985 the incidence of cryptorchidism has ‘declined in most systems'.55 Thus, with the exception of testicular cancer, the temporal increase in male reproductive tract problems is questionable and correlations with ‘environmental exposures' are minimal to non-existent.
Conclusions and surprises
The initial endocrine disruptor hypothesis which suggested a link between in utero exposures to estrogens and decreased sperm counts is not supported by most studies but is still championed by Skakkebeck and some of his co-workers who now refer to it as the ‘testicular dysgenesis syndrome'56 and they recently suggested that ‘we may have reached a tipping point'.57 The role of OC estrogens such as PCBs and DDE in breast cancer has largely been resolved by several studies including a detailed examination of women on Long Island. It was concluded by the authors that ‘these findings, based on the largest number of samples analyzed to date among primarily white women, do not support the hypothesis that organochlorines increase breast cancer risk among Long Island women'.58 Despite some resolution of the sperm count and breast cancer issues, the endocrine disruptor hypothesis has now morphed into the developmental origins of health and disease where there is an ongoing controversy regarding the adverse health effects of endocrine disruptors. BPA and related industrial estrogens are among the chemicals of concern and it has been suggested by some scientists that exposure to BPA may play a role in ‘the increase in prostate and breast cancer, uro-genital abnormalities in male babies, a decline in semen quality in men, early onset of puberty in girls, metabolic disorders including insulin resistant (type 2) diabetes and obesity, and neurobehavioral problems such as attention-deficit hyperactivity disorder'.59
Thus, the claims and controversies regarding EDCs have continued for almost 20 years and there are no signs of resolution. It is noteworthy that two preeminent reproductive biologists who have made highly significant contributions to this field have developed scepticism on the claimed effects for BPA. Ryan and co-workers60 showed that BPA did not alter sexually dimorphic behaviour, puberty, fertility or anatomy of female Long–Evans rats, which contradicted prior results or conclusions drawn by other groups. In a commentary, Sharpe,61 a coauthor of the initial endocrine disruptor hypothesis, clearly answered in the affirmative the title of his highlight ‘Is it time to end concerns over the estrogenic effects of BPA?'. On the basis of the exchange of letters on this article, it is apparent that the issue of endocrine disruptors and their adverse health effects is far from settled among scientists, and it is possible and very unfortunate that this may not be resolved in the next 20 years. In times of decreased funding for academic research, it is critical that reasonable scientists and regulators come to a consensus regarding specific EDCs that should be further investigated or regulated and address more pressing scientific problems and opportunities.
References
- Safe S. Polychlorinated biphenyls (PCBs) and polybrominated biphenyls (PBBs): biochemistry, toxicology, and mechanism of action. Crit Rev Toxicol. 1984;13:319–95. doi: 10.3109/10408448409023762. [DOI] [PubMed] [Google Scholar]
- Safe S. Polychlorinated biphenyls (PCBs), dibenzo-p-dioxins (PCDDs), dibenzofurans (PCDFs), and related compounds: environmental and mechanistic considerations which support the development of toxic equivalency factors (TEFs) Crit Rev Toxicol. 1990;21:51–88. doi: 10.3109/10408449009089873. [DOI] [PubMed] [Google Scholar]
- Safe SH. Polychlorinated biphenyls (PCBs): environmental impact, biochemical and toxic responses, and implications for risk assessment. Crit Rev Toxicol. 1994;24:87–149. doi: 10.3109/10408449409049308. [DOI] [PubMed] [Google Scholar]
- Poland A, Glover E, Kende AS. Stereospecific, high affinity binding of 2,3,7,8-tetrachlorodibenzo-p-dioxin by hepatic cytosol. Evidence that the binding species is receptor for induction of aryl hydrocarbon hydroxylase. J Biol Chem. 1976;251:4936–46. [PubMed] [Google Scholar]
- Poland A, Knutson JC. 2,3,7,8-tetrachlorodibenzo-p-dioxin and related halogenated aromatic hydrocarbons: examination of the mechanism of toxicity. Annu Rev Pharmacol Toxicol. 1982;22:517–54. doi: 10.1146/annurev.pa.22.040182.002505. [DOI] [PubMed] [Google Scholar]
- van den Berg M, Birnbaum L, Bosveld AT, Brunstrom B, Cook P, et al. Toxic equivalency factors (TEFs) for PCBs, PCDDs, PCDFs for humans and wildlife. Environ Health Perspect. 1998;106:775–92. doi: 10.1289/ehp.98106775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg M, Birnbaum LS, Denison M, de Vito M, Farland W, et al. The 2005 World Health Organization reevaluation of human and Mammalian toxic equivalency factors for dioxins and dioxin-like compounds. Toxicol Sci. 2006;93:223–41. doi: 10.1093/toxsci/kfl055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romkes M, Safe S. Comparative activities of 2,3,7,8-tetrachlorodibenzo-p-dioxin and progesterone as antiestrogens in the female rat uterus. Toxicol Appl Pharmacol. 1988;92:368–80. doi: 10.1016/0041-008x(88)90177-9. [DOI] [PubMed] [Google Scholar]
- Romkes M, Piskorska-Pliszczynska J, Safe S. Effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin on hepatic and uterine estrogen receptor levels in rats. Toxicol Appl Pharmacol. 1987;87:306–14. doi: 10.1016/0041-008x(87)90292-4. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Safe S. Polychlorinated biphenyls (PCBs), dibenzo-p-dioxins (PCDDs), and dibenzofurans (PCDFs) as antiestrogens in MCF-7 human breast cancer cells: quantitative structure-activity relationships. Toxicol Appl Pharmacol. 1993;120:55–61. doi: 10.1006/taap.1993.1086. [DOI] [PubMed] [Google Scholar]
- Krishnan V, Porter W, Santostefano M, Wang X, Safe S. Molecular mechanism of inhibition of estrogen-induced cathepsin D gene expression by 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) in MCF-7 cells. Mol Cell Biol. 1995;15:6710–9. doi: 10.1128/mcb.15.12.6710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safe S, Wormke M. Inhibitory aryl hydrocarbon receptor-estrogen receptor alpha cross-talk and mechanisms of action. Chem Res Toxicol. 2003;16:807–16. doi: 10.1021/tx034036r. [DOI] [PubMed] [Google Scholar]
- Sharpe RM, Skakkebaek NE. Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract. Lancet. 1993;341:1392–5. doi: 10.1016/0140-6736(93)90953-e. [DOI] [PubMed] [Google Scholar]
- Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305:609–13. doi: 10.1136/bmj.305.6854.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusti RM, Iwamoto K, Hatch EE. Diethylstilbestrol revisited: a review of the long-term health effects. Ann Intern Med. 1995;122:778–88. doi: 10.7326/0003-4819-122-10-199505150-00008. [DOI] [PubMed] [Google Scholar]
- Newbold R. Cellular and molecular effects of developmental exposure to diethylstilbestrol: implications for other environmental estrogens. Environ Health Perspect. 1995;103 Suppl 7:83–7. doi: 10.1289/ehp.95103s783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stillman RJ. In utero exposure to diethylstilbestrol: adverse effects on the reproductive tract and reproductive performance and male and female offspring. Am J Obstet Gynecol. 1982;142:905–21. doi: 10.1016/s0002-9378(16)32540-6. [DOI] [PubMed] [Google Scholar]
- Falck F, Jr, Ricci A, Jr, Wolff MS, Godbold J, Deckers P. Pesticides and polychlorinated biphenyl residues in human breast lipids and their relation to breast cancer. Arch Environ Health. 1992;47:143–6. [PubMed] [Google Scholar]
- Wolff MS, Toniolo PG, Lee EW, Rivera M, Dubin N. Blood levels of organochlorine residues and risk of breast cancer. J Natl Cancer Inst. 1993;85:648–52. doi: 10.1093/jnci/85.8.648. [DOI] [PubMed] [Google Scholar]
- Davis DL, Bradlow HL, Wolff M, Woodruff T, Hoel DG, et al. Medical hypothesis: xenoestrogens as preventable causes of breast cancer. Environ Health Perspect. 1993;101:372–7. doi: 10.1289/ehp.93101372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safe S. Male sexual development in “a sea of oestrogen”. Lancet. 1993;342:125. [PubMed] [Google Scholar]
- Desbrow C, Routledge EJ, Brighty GC, Sumpter JP, Waldock M. Identification of estrogenic chemicals in STW effluent. 1. Chemical fractionation and in vitro biological screening. Environ Sci Technol. 1998;32:1549–58. [Google Scholar]
- Allen Y, Scott AP, Matthiessen P, Haworth S, Thain JE, et al. Survey of estrogenic activity in United Kingdom estuarine and coastal waters and its effects on gonadal development of the flounder Platichthys flesus. Environ Toxicol Chem. 1999;18:1791–800. [Google Scholar]
- Guillette LJ, Jr, Gross TS, Masson GR, Matter JM, Percival HF, et al. Developmental abnormalities of the gonad and abnormal sex hormone concentrations in juvenile alligators from contaminated and control lakes in Florida. Environ Health Perspect. 1994;102:680–8. doi: 10.1289/ehp.94102680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiper GG, Carlsson B, Grandien K, Enmark E, Haggblad J, et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors alpha and beta. Endocrinology. 1997;138:863–70. doi: 10.1210/endo.138.3.4979. [DOI] [PubMed] [Google Scholar]
- Safe S. Dietary and environmental estrogens and antiestrogens and their possible role in human disease. Environ Sci Pollut Res. 1994;1:29–33. doi: 10.1007/BF02986921. [DOI] [PubMed] [Google Scholar]
- Safe S.Male reproductive capacity and exposure to environmental chemicals.In: Eisenbrand G, editor. Hormonally Active Agents in Food: Symposium Weinheim; John Wiley-VCH; 1998p253–9. [Google Scholar]
- Safe SH. Endocrine disruptors and human health—is there a problem? An update. Environ Health Perspect. 2000;108:487–93. doi: 10.1289/ehp.00108487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safe S. Endocrine disruptors and human health: is there a problem. Toxicology. 2004;205:3–10. doi: 10.1016/j.tox.2004.06.032. [DOI] [PubMed] [Google Scholar]
- Safe S. Environmental estrogens: roles in male reproductive tract problems and in breast cancer. Rev Environ Health. 2002;17:253–62. doi: 10.1515/reveh.2002.17.4.253. [DOI] [PubMed] [Google Scholar]
- Safe SH. Environmental and dietary estrogens and human health: is there a problem. Environ Health Perspect. 1995;103:346–51. doi: 10.1289/ehp.95103346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon K, Pellaroni L, Ramamoorthy K, Gaido K, Safe S. Ligand structure-dependent differences in activation of estrogen receptor alpha in human HepG2 liver and U2 osteogenic cancer cell lines. Mol Cell Endocrinol. 2000;162:211–20. doi: 10.1016/s0303-7207(99)00261-0. [DOI] [PubMed] [Google Scholar]
- Yoon K, Pallaroni L, Stoner M, Gaido K, Safe S. Differential activation of wild-type and variant forms of estrogen receptor alpha by synthetic and natural estrogenic compounds using a promoter containing three estrogen-responsive elements. J Steroid Biochem Mol Biol. 2001;78:25–32. doi: 10.1016/s0960-0760(01)00070-x. [DOI] [PubMed] [Google Scholar]
- Gaido KW, Leonard LS, Maness SC, Hall JM, McDonnell DP, et al. Differential interaction of the methoxychlor metabolite 2,2-bis-(p-hydroxyphenyl)-1,1,1-trichloroethane with estrogen receptors alpha and beta. Endocrinology. 1999;140:5746–53. doi: 10.1210/endo.140.12.7191. [DOI] [PubMed] [Google Scholar]
- Gaido KW, Maness SC, McDonnell DP, Dehal SS, Kupfer D, et al. Interaction of methoxychlor and related compounds with estrogen receptor alpha and beta, and androgen receptor: structure-activity studies. Mol Pharmacol. 2000;58:852–8. [PubMed] [Google Scholar]
- Wu F, Safe S. Differential activation of wild-type estrogen receptor alpha and C-terminal deletion mutants by estrogens, antiestrogens and xenoestrogens in breast cancer cells. J Steroid Biochem Mol Biol. 2007;103:1–9. doi: 10.1016/j.jsbmb.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Wu F, Khan S, Wu Q, Barhoumi R, Burghardt R, et al. Ligand structure-dependent activation of estrogen receptor alpha/Sp by estrogens and xenoestrogens. J Steroid Biochem Mol Biol. 2008;110:104–15. doi: 10.1016/j.jsbmb.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramamoorthy K, Wang F, Chen IC, Safe S, Norris JD, et al. Potency of combined estrogenic pesticides. Science. 1997;275:405–6. doi: 10.1126/science.275.5298.405. [DOI] [PubMed] [Google Scholar]
- Ramamoorthy K, Wang F, Chen IC, Norris JD, McDonnell DP, et al. Estrogenic activity of a dieldrin/toxaphene mixture in the mouse uterus, MCF-7 human breast cancer cells, and yeast-based estrogen receptor assays: no apparent synergism. Endocrinology. 1997;138:1520–7. doi: 10.1210/endo.138.4.5056. [DOI] [PubMed] [Google Scholar]
- Arnold SF, Klotz DM, Collins BM, Vonier PM, Guillette LJ, Jr, et al. Synergistic activation of estrogen receptor with combinations of environmental chemicals. Science. 1996;272:1489–92. doi: 10.1126/science.272.5267.1489. [DOI] [PubMed] [Google Scholar]
- Auger J, Kunstmann JM, Czyglik F, Jouannet P. Decline in semen quality among fertile men in Paris during the past 20 years. N Engl J Med. 1995;332:281–5. doi: 10.1056/NEJM199502023320501. [DOI] [PubMed] [Google Scholar]
- Bujan L, Mansat A, Pontonnier F, Mieusset R. Time series analysis of sperm concentration in fertile men in Toulouse, France between 1977 and 1992. BMJ. 1996;312:471–2. doi: 10.1136/bmj.312.7029.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, et al. Impact of body mass index values on sperm quantity and quality. J Androl. 2006;27:450–2. doi: 10.2164/jandrol.05124. [DOI] [PubMed] [Google Scholar]
- Jensen TK, Andersson AM, Jorgensen N, Andersen AG, Carlsen E, et al. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril. 2004;82:863–70. doi: 10.1016/j.fertnstert.2004.03.056. [DOI] [PubMed] [Google Scholar]
- Fisch H, Goluboff ET, Olson JH, Feldshuh J, Broder SJ, et al. Semen analyses in 1,283 men from the United States over a 25-year period: no decline in quality. Fertil Steril. 1996;65:1009–14. doi: 10.1016/s0015-0282(16)58278-8. [DOI] [PubMed] [Google Scholar]
- Younglai EV, Collins JA, Foster WG. Canadian semen quality: an analysis of sperm density among eleven academic fertility centers. Fertil Steril. 1998;70:76–80. doi: 10.1016/s0015-0282(98)00118-6. [DOI] [PubMed] [Google Scholar]
- Handelsman DJ. Sperm output of healthy men in Australia: magnitude of bias due to self-selected volunteers. Hum Reprod. 1997;12:2701–5. doi: 10.1093/humrep/12.12.2701. [DOI] [PubMed] [Google Scholar]
- Bonde JP, Ramlau-Hansen CH, Olsen J. Trends in sperm counts: the saga continues. Epidemiology. 2011;22:617–9. doi: 10.1097/EDE.0b013e318223442c. [DOI] [PubMed] [Google Scholar]
- Axelsson J, Rylander L, Rignell-Hydbom A, Giwercman A. No secular trend over the last decade in sperm counts among Swedish men from the general population. Hum Reprod. 2011;26:1012–6. doi: 10.1093/humrep/der045. [DOI] [PubMed] [Google Scholar]
- Jorgensen N, Vierula M, Jacobsen R, Pukkala E, Perheentupa A, et al. Recent adverse trends in semen quality and testis cancer incidence among Finnish men. Int J Androl. 2011;34:e37–48. doi: 10.1111/j.1365-2605.2010.01133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe RM. Reproductive biology. Another DDT connection. Nature. 1995;375:538–9. doi: 10.1038/375538a0. [DOI] [PubMed] [Google Scholar]
- Ekbom A, Wicklund-Glynn A, Adami HO. DDT and testicular cancer. Lancet. 1996;347:553–4. doi: 10.1016/s0140-6736(96)91190-3. [DOI] [PubMed] [Google Scholar]
- Swerdlow AJ, de Stavola BL, Swanwick MA, Maconochie NE. Risks of breast and testicular cancers in young adult twins in England and Wales: evidence on prenatal and genetic aetiology. Lancet. 1997;350:1723–8. doi: 10.1016/s0140-6736(97)05526-8. [DOI] [PubMed] [Google Scholar]
- Storgaard L, Bonde JP, Ernst E, Andersen CY, Kyvik KO, et al. Effect of prenatal exposure to oestrogen on quality of semen: comparison of twins and singleton brothers. BMJ. 2002;325:252–3. doi: 10.1136/bmj.325.7358.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ. International trends in rates of hypospadias and cryptorchidism. Environ Health Perspect. 1999;107:297–302. doi: 10.1289/ehp.99107297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skakkebaek NE, Rajpert-De Meyts E, Main KM. Testicular dysgenesis syndrome: an increasingly common developmental disorder with environmental aspects. Hum Reprod. 2001;16:972–8. doi: 10.1093/humrep/16.5.972. [DOI] [PubMed] [Google Scholar]
- Andersson AM, Jorgensen N, Main KM, Toppari J, Rajpert-De Meyts E, et al. Adverse trends in male reproductive health: we may have reached a crucial ‘tipping point'. Int J Androl. 2008;31:74–80. doi: 10.1111/j.1365-2605.2007.00853.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gammon MD, Wolff MS, Neugut AI, Eng SM, Teitelbaum SL, et al. Environmental toxins and breast cancer on Long Island. II. Organochlorine compound levels in blood. Cancer Epidemiol Biomarkers Prev. 2002;11:686–97. [PubMed] [Google Scholar]
- vom Saal FS, Akingbemi BT, Belcher SM, Birnbaum LS, Crain DA, et al. Chapel Hill bisphenol A expert panel consensus statement: integration of mechanisms, effects in animals and potential to impact human health at current levels of exposure. Reprod Toxicol. 2007;24:131–8. doi: 10.1016/j.reprotox.2007.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan BC, Hotchkiss AK, Crofton KM, Gray LE., Jr In utero and lactational exposure to bisphenol A, in contrast to ethinyl estradiol, does not alter sexually dimorphic behavior, puberty, fertility, and anatomy of female LE rats. Toxicol Sci. 2010;114:133–48. doi: 10.1093/toxsci/kfp266. [DOI] [PubMed] [Google Scholar]
- Sharpe RM. Is it time to end concerns over the estrogenic effects of bisphenol A. Toxicol Sci. 2010;114:1–4. doi: 10.1093/toxsci/kfp299. [DOI] [PubMed] [Google Scholar]


