Abstract
This study investigated the effect of treatment with the proprietary standardized, water-soluble extract of the root of the Malaysian plant, Eurycoma longifolia Jack, which is thought to enhance male fertility with regard to higher semen volumes, sperm concentrations, the percentage of normal sperm morphology and sperm motility in male partners of sub-fertile couples with idiopathic infertility. A total of 350 patients were given 200 mg of the extract daily and follow-up semen analyses were performed every 3 months for 9 months. Of these 350 patients, 75 patients completed one full cycle of 3 months. Follow-up semen analyses in these patients showed significant improvement in all semen parameters. The proprietary extract of Eurycoma longifolia Jack significantly improved the sperm quality in these patients, allowing for 11 (14.7%) spontaneous pregnancies.
Keywords: male infertility, medicinal herbs, semen
Introduction
Male infertility is a multifactorial disease, with numerous factors contributing to both reduced spermatogenesis and the production of dysfunctional sperm, which are the most prevalent underlying characteristics found in cases of idiopathic male infertility 1. A meta-analysis of 61 studies worldwide reported a downward trend in sperm count and semen volume over the past 50 years 2, 3. Among the causes of male infertility,the prominent ones namely idiopathic infertility,followed with varicocele, maldescended testes,infections, hormonal causes and gebetic effects. Given its etiologic heterogeneity, successful treatment of male infertility is quite challenging .
Eurycoma longifolia Jack, locally known as Tongkat ali, is a common shrub found along the slopes in hilly terrains of the Malaysian rainforest. A water decoction of the root of Tongkat ali is a well-known traditional supplement for the enhancement of sexuality and fertility and is also used as an anti-aging tonic 4, 5, 6, 7, 8. This aqueous extract contains, among other things, tannins, high-molecular-weight polysaccharides, glycoprotein, mucopolysaccharides and quassinoid alkaloids, which exhibit anti-malarial, anti-ulcer, anti-tumor, anti-parasitic and anti-pyretic activities 5, 6, 7, 8, 9, 10, 11.
Animal studies have shown that the anti-cancer, pro-fertility and aphrodisiac properties of this extract are mediated by its glycoprotein components 12, 13. Recent human trials have proven its testosterone-enhancing and anti-stress or anti-aging effects, which are accompanied or mediated, respectively, by normalized serum growth hormone concentrations and elevated concentrations of superoxide dismutase (SOD), an important anti-oxidant 14, 15, 16, 17, 18, 19. Therefore, this study aimed to investigate the fertility-enhancing effects of Tongkat ali. We hypothesized that a standardized extract of the Eurycoma longifolia Jack root may prove useful in treating men with idiopathic infertility; namely, men with low sperm concentration with or without low motility and a decreased percentage of sperm showing normal morphology. The secondary aim was to investigate a possible increase in the pregnancy rate during treatment.
Materials and methods
Between early 2004 and late 2007, a total of 350 male partners from sub-fertile couples attending the Wellmen Clinic, Damai Service Hospital, Kuala Lumpur, Malaysia, were identified as having idiopathic infertility, in the setting of low sperm concentration, decreased motility and abnormal sperm morphology. Out of the 350 patients initially recruited, a total of 75 male patients with an average age of 32.7 years and a history of infertility of 5.3 years fulfilled the inclusion criteria and were treated with two capsules of 100 mg of a proprietary standardized water-soluble extract of Eurycoma longifolia Jack root (US Patent: US7, 132,117B2 from Phytes Bioteks, Biotropics Malaysia, Berhad, Malaysia), taken orally twice daily after eating. The dose of 200 mg daily was determined by an earlier dosing study 18, 19. Follow-up examinations were conducted every 3 months for three cycles. In each of these examinations, a semen analysis according to World Health Organization (WHO) guidelines 20 and determination of the testicular volume (based on Prader's orchidometer) were performed. The principal parameter to be evaluated was improvement in the sperm parameters (sperm concentration, motility and morphology). The secondary parameter was achievement of pregnancy in the female partner. There was a drop in the patients' compliance from the second to the third follow-up examination owing to dropout and pregnancies of the female partner.
The data were analyzed using SPSS version 12 (SPSS Inc., Chicago, IL, USA). After confirming normal distribution using the Kolmogorov–Smirnov test, data were expressed as mean ± SE, with trends plotted on line graphs. Paired t-tests were used to assess whether there were any significant differences between the means of the parameters between the baseline and each of the treatment cycles; a P-value of less than 0.05 (two-sided) was considered significant.
Results
There was improvement in the seminal parameters in all 75 men who completed the supplement in each of the follow-up cycles. Results are expressed as mean ± SE for each parameter in Table 1. Statistically significant differences between each cycle and baseline are indicated in Table 1. The changes in the means of sperm concentration, percentage of sperm with normal morphology and semen volume over the three cycles of treatment are also illustrated in Figures 1 2 3. In Figure 1, the sperm concentration (million per mL) significantly increased from the baseline to the first cycle. It went down at the second cycle and peaked at the third cycle. When paired comparison performed using paired t-test, the mean differences were 5.4, 5.5 and 14.9 million per ml at each of the paired comparison (data not shown) that is at the baseline and at the first cycle, at the baseline and at the second cycle, at the baseline and at third cycle. Each pair differed significantly with their P values of 0.007, < 0.001 and 0.007 respectively. Even though in Figure 1, the pattern of the increase is not uniform, it indicates improvement of the sperm concentration at each of the cycle when compared to the baseline sperm concentration. In Figure 2, it shows the mean percentage of sperm with normal morphology also generally increased consistently except in the last cycle, cycle 3 where it dipped slightly. There were statistically significant improvements in sperm concentration and sperm morphology from baseline to each cycle of treatment (Table 1). The mean sperm concentration and percentage of sperm with normal morphology increased from baseline by 65.5% and 94.9%, respectively, at the third cycle of treatment. An upward trend in semen volume was also seen, although this failed to reach statistical significance (Figure 3). The mean sperm motility at the first cycle of treatment was significantly increased from baseline (P = 0.037); no further changes were observed over the subsequent cycles (Table 1).
Table 1. Seminal parameters evaluated at baseline and each cycle of treatment.
| Seminal parameter | Baseline (n = 75) | Cycle 1 (n = 75) | Cycle 2 (n = 49) | Cycle 3 (n = 17) |
|---|---|---|---|---|
| Semen volume (mL) | 2.95 ± 0.14 | 2.96 ± 0.13 | 3.14 ± 0.21 | 3.52 ± 0.35 |
| Sperm concentration (million per mL) | 10.59 ± 2.06 | 16.32 ± 1.99a | 12.52 ± 2.03b | 17.53 ± 5.04a |
| Normal sperm morphology (%) | 5.28 ± 0.66 | 8.94 ± 1.02b | 10.41 ± 1.28b | 10.29 ± 2.52c |
| Sperm motility (%) | 44.68 ± 2.44 | 49.99 ± 2.81d | 46.33 ± 2.58 | 40.24 ± 4.40 |
All values are mean ± SE.
aP = 0.007;
bP < 0.001;
cP = 0.003;
dP = 0.037; compared with baseline (paired t-test).
Figure 1.
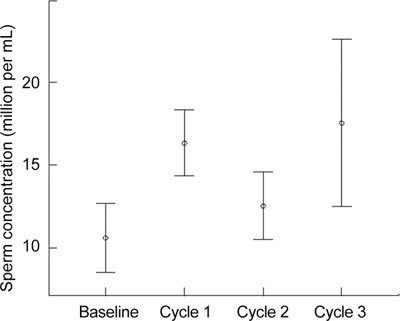
Increase in seminal sperm concentration after treatment with a 100 mg twice daily dose of the proprietary standardized water-soluble extract of Eurycoma longifolia Jack root. A distinct continuous increase in sperm concentration after the treatment can be seen from baseline to the first, second and third cycles. All values are mean ± SE.
Figure 2.
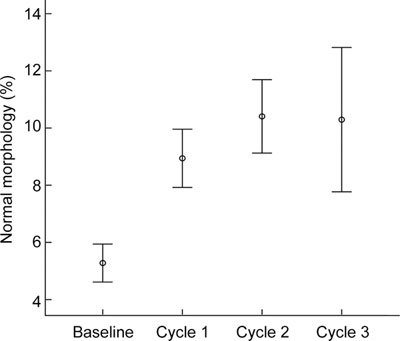
Increase in the percentage of sperm with normal morphology after treatment with a 100 mg twice daily dose of the proprietary standardized water-soluble extract of Eurycoma longifolia Jack root. A significant improvement in sperm morphology after the treatment can be seen from the baseline to the first, second and third cycles. All values are mean ± SE.
Figure 3.
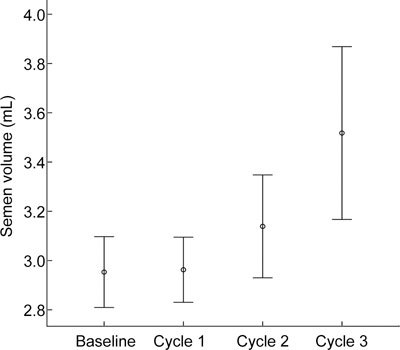
Increase in seminal volume after treatment with a 100 mg twice daily dose of the proprietary standardized water-soluble extract of Eurycoma longifolia Jack root. A distinct, continuous increase in seminal volume after treatment can be seen from baseline to the first, second and third cycles. All values are mean ± SE.
In all, 75 men completed at least one cycle of treatment, 49 men completed two cycles and 17 men completed three cycles. There were 11 (14.7%) spontaneous pregnancies during this time, 6 of which were achieved at completion of the first cycle of treatment and 5 of which were achieved at completion of two cycles of treatment. The semen parameters of male patients whose partner conceived are shown in Table 2. There were no differences in the mean semen volume at baseline (3.50 mL), in the first (2.83 mL) or in the second (3.38 mL) follow-up examination. In addition, there were also no marked differences in the mean sperm concentration at baseline (28.47 million per mL), in the first (27.57 million per mL) or in the second (33.60 million per mL) follow-up examination.
Table 2. Semen parameters of those men whose female partners became spontaneously pregnant.
| Number | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Baseline semen volume (mL) | 11 | 2.20 | 4.50 | 3.50 | 0.73 |
| Baseline sperm concentration (million/mL) | 11 | 3.00 | 68.00 | 28.47 | 24.77 |
| Baseline sperm motility (%) | 11 | 20.00 | 70.00 | 44.00 | 14.97 |
| Baseline sperm morphology (%) | 11 | 2.00 | 18.00 | 10.36 | 5.39 |
| Semen volume at cycle 1 (mL) | 11 | 1.00 | 5.00 | 2.83 | 1.15 |
| Sperm concentration at cycle 1 (million/mL) | 11 | 8.30 | 55.00 | 27.57 | 16.19 |
| Sperm motility at cycle 1 (%) | 11 | 11.00 | 90.00 | 56.00 | 23.34 |
| Sperm morphology at cycle 1 (%) | 11 | 6.00 | 32.00 | 16.54 | 7.98 |
| Semen volume at cycle 2 (mL) | 5 | 2.50 | 5.00 | 3.38 | 0.96 |
| Sperm concentration at cycle 2 (million/mL) | 5 | 5.00 | 63.00 | 33.60 | 24.49 |
| Sperm motility at cycle 2 (%) | 5 | 35.00 | 80.00 | 58.60 | 19.87 |
| Sperm morphology at cycle 2 (%) | 5 | 3.00 | 25.00 | 16.00 | 9.00 |
However, in those men whose female partners became pregnant, sperm motility increased significantly from the initial examination (44.00%) to the first follow-up (56.00%) and the second follow-up (58.60%). A similar trend was seen for the percentage of sperm with normal morphology, which improved from 10.36% at the time of baseline examination to 16.54% at the first follow-up and 16.00% at the second follow-up examination. After completion of this study, those patients whose partner failed to conceive were given the option of using assisted reproduction (ART), at which point 60% underwent intra-uterine insemination (IUI), 20% underwent in vitro fertilization (IVF) and 5.3% were treated with IVF/intracytoplasmic sperm injection technique (ICSI).
Discussion
This study clearly shows an improvement in the main seminal parameters in infertile patients treated with the proprietary standardized water-soluble extract of Eurycoma longifolia Jack, with significant increases in sperm concentration and the percentage of sperm with normal morphology after each treatment cycle. The exact mechanism of action of this extract at the level of the reproductive cell remains unknown. However, the beneficial effect may be attributed to its testosterone-enhancing effect and antioxidant properties, which have been well documented in the previous studies 14, 15, 16, 17, 18, 19. Eurycoma longifolia Jack was reported to contain a bioactive peptide, which has been shown to increase the testosterone levels in rat Leydig cells 13. Recent human trials also showed that the extract of Eurycoma longifolia Jack enhanced total testosterone and dihydroepiandrosterone levels 14, 15, 16, 17, 18, 19. The same studies also showed that the Eurycoma longifolia Jack extract contains SOD activity. Considering that the antioxidant supplementation is thought to improve male reproductive functions 21, 22, 23, these properties may contribute to the improvement in sperm concentration and sperm morphology.
A large number of men are infertile owing to abnormalities in sperm production, especially severe defects in sperm morphology, which render the sperm dysfunctional and greatly reduce the partner's chances of pregnancy 24. Therefore, infertile couples have to rely on costly techniques such as ART (for example, IVF). Sperm morphology and concentration have been shown to be significantly associated with the fertilization rate in vitro and have been deemed to be decisive factors in the selection of appropriate ART techniques to treat infertile couples efficiently 25, 26. Consequently, it is noteworthy that 11 (14.7%) spontaneous pregnancies were achieved after the treatment of infertile men presenting with idiopathic infertility in the setting of decreased sperm concentration, poor sperm motility and abnormal sperm morphology, using the proprietary standardized water-soluble extract of Eurycoma longifolia Jack. Semen parameters of those patients whose partners achieved pregnancy showed increased percentages of normal sperm morphology and motility following treatment with this herbal extract. It is also intriguing to observe that the herbal extract significantly improved sperm concentration and sperm morphology in patients whose partners did not become pregnant. In these cases, other parameters, such as poor chromatin condensation or sperm DNA fragmentation, might have been the limiting factors that prevented fertilization 27. Nonetheless, the increase in sperm concentration and morphologically normal sperm allowed couples a chance of natural conception, or to forgo IVF and undergo less invasive and less expensive ART options, such as IUI, instead. In total, 60% of the patients in this study underwent IUI based on their seminal parameters after treatment with the extract of Eurycoma longifolia Jack. Before treatment, seminal parameters did not permit this possibility in any case, meaning that these patients would have been forced to opt for a more invasive and expensive ART treatment, such as IVF. Thus, the results of this study indicate that sperm quality can be improved by treating men with traditional remedies, which in turn can improve the pregnancy rates.
Conclusion
The results of this study suggest that treatment with the proprietary standardized extract of Eurycoma longifolia Jack significantly improves semen volume, sperm concentration, sperm motility and the percentage of morphologically normal sperm in men with idiopathic infertility. As spontaneous pregnancies were achieved in 14.7% of couples in our study and the use of a less invasive, cheaper variety of ART became possible in another 60%, the treatment of such patients with Eurycoma longifolia Jack might be an option in the management of male infertility.
In light of the encouraging results of the present study, further studies in a larger group of patients, with follow-up of the outcomes of the ART procedures, are required to elucidate the potential role of Eurycoma longifolia Jack in the treatment of male infertility.
Conflict of interest
The authors declare no competing commercial interests in relation to the company that produced the Standardized Water-soluble extract of Eurycoma longifolia. We have not received grant support from the company.
References
- Mahdi AA, Bano F, Singh R, Singh RK, Siddiqui MS, et al. Seminal plasma superoxide dismutase and catalase activities in infertile men. Med Sci Res. 1999;27:201–3. [Google Scholar]
- Bano F, Singh RK, Singh R, Siddiqui MS, Mahdi AA. Seminal plasma lipid peroxide levels in infertile men. J Endocrinol Reprod. 1999;3:20–8. [Google Scholar]
- Sikka SC. Relative impact of oxidative stress on male reproductive function. Curr Med Chem. 2001;8:851–62. doi: 10.2174/0929867013373039. [DOI] [PubMed] [Google Scholar]
- Burkill IH, Hanif M. Malay village medicine, prescriptions collected. Gardens Bulletin Strait Settlements. 1930;6:176–7. [Google Scholar]
- Ali JM, Saad JM.Biochemical effect of Eurycoma Longifolia Jack on the sexual behavior, fertility, sex hormone and glycolysis [Dissertation]Department of Biochemistry, University of Malaya. 1993
- Ang HH, Sim MK. Eurycoma longifolia increases sexual motivation in sexually naive male rats. Arch Pharm Res. 1998;21:779–81. doi: 10.1007/BF02976776. [DOI] [PubMed] [Google Scholar]
- Ang HH, Sim MK. Eurycoma longifolia Jack and orientation activities in sexually experienced male rats. Biol Pharm Bull. 1998;21:153–5. doi: 10.1248/bpb.21.153. [DOI] [PubMed] [Google Scholar]
- Ang HH, Sim MK. Eurycoma Longifolia Jack increases sexual motivation in sexually naive male rats. Archives of Pharmacal Research. 1998;21:778–81. doi: 10.1007/BF02976776. [DOI] [PubMed] [Google Scholar]
- Kuo PC, Damu AG, Lee KH, Wu TS. Cytotoxic and antimalarial constituents from the roots of Eurycoma longifolia. Bioorg Med Chem. 2004;12:537–44. doi: 10.1016/j.bmc.2003.11.017. [DOI] [PubMed] [Google Scholar]
- Jiwajinda S, Santisopasri V, Murakami A, Sugiyama H, Gasquet M, et al. In vitro anti-tumor promoting and anti-parasitic activities of the quassinoids from Eurycoma longifolia, a medicinal plant in Southeast Asia. J Ethnopharmacol. 2002;82:55–8. doi: 10.1016/s0378-8741(02)00160-5. [DOI] [PubMed] [Google Scholar]
- Hamzah S, Yusof A. The ergogenic effects of Tongkat Ali (Eurycoma Longifolia) Br J Sports Med. 2003;37:465–66. [Google Scholar]
- Asiah O, Nurhanan MY, Ilham MA. Determination of bioactive peptide (4.3 kDa) as an aphrodisiac marker in six Malaysia plants. J Tropical Forest Sci. 2007;19:61–3. [Google Scholar]
- Sambandan TG, Rha C, Kadir AA, Aminudim N, Saad JM.Bioactive fraction of Eurycoma longifoliaUS Patent: US7, 132,117 B2 2006.
- Tambi MI.Glycoprotein water-soluble extract of Eurycoma Longifolia Jack as a health supplement in management of Health aging in aged menIn: Lunenfeld B, editor. Abstracts of the 3rd World Congress on the Aging Male, February 7–10, 2002, Berlin, Germany. Aging Male 2002; 6. [Abstract].
- Tambi MI.Water soluble Extract of Eurycoma Longifolia in enhancing testosterone in malesIn: Proceeding of International Trade Show and Conference, Supply Side West, The Venetian, Las Vegas, Nevada, USA. 2003 Oct 1–3.
- Tambi MI.Standardized water soluble extract of Eurycoma Longifolia (LJ100) on men's healthIn: Abstracts of the 8th International Congress of Andrology, 12–16 June 2005, Seoul, Korea. Int J Androl 200528Suppl 12715679618 [Google Scholar]
- Tambi MI.Standardized water soluble extract of Eurycoma Longifolia LJ100 maintains healthy aging in manIn: Lunenfeld B, editor. Abstracts of the 5th World Congress on the Aging Male. February 9-12, 2006, Salzburg, Austria. Aging Male 20069Abstract]
- Tambi MI. Eurycoma Longifolia jack: a potent adaptogen in the form of water-soluble extract with the effect of maintaining men's health. Asian J Androl. 2006;8 Suppl 1:49–50. [Google Scholar]
- World Health Organization (WHO)Laboratory Manual for the Examination of Human Semen and Sperm–Cervical Mucus InteractionNew York: Cambridge University Press; 1999
- Lenzi A, Picardo M, Gandini L, Dondero F. Lipids of the sperm plasma membrane: from polyunsaturated fatty acids considered as markers of sperm function to possible scavenger therapy. Hum Reprod Update. 1996;2:246–56. doi: 10.1093/humupd/2.3.246. [DOI] [PubMed] [Google Scholar]
- Lenzi A, Lombardo F, Sgro P, Salacone P, Caponecchia L, et al. Use of carnitine therapy in selected cases of male factor infertility: a double-blind crossover trial. Fertil Steril. 2003;79:292–300. doi: 10.1016/s0015-0282(02)04679-4. [DOI] [PubMed] [Google Scholar]
- Kefer JC, Agarwal A, Sabanegh E. Role of antioxidants in the treatment of male infertility. Int J Urol. 2009;16:449–57. doi: 10.1111/j.1442-2042.2009.02280.x. [DOI] [PubMed] [Google Scholar]
- Kruger TF, Coetzee K. The role of sperm morphology in assisted reproduction. Hum Reprod Update. 1999;5:172–8. doi: 10.1093/humupd/5.2.172. [DOI] [PubMed] [Google Scholar]
- Burr RW, Siegberg R, Flaherty SP, Wang XJ, Matthews CD. The influence of sperm morphology and the number of motile sperm inseminated on the outcome of intrauterine insemination combined with mild ovarian stimulation. Fertil Steril. 1996;65:127–32. doi: 10.1016/s0015-0282(16)58039-x. [DOI] [PubMed] [Google Scholar]
- Mortimer D, Menkveld R. Sperm morphology assessment—historical perspectives and current opinions. J Androl. 2001;22:192–205. [PubMed] [Google Scholar]
- Henkel R, Maaß G, Bödeker RH, Scheibelhut C, Stalf T, et al. Sperm function and assisted reproduction technology. Reprod Med Biol. 2005;4:7–30. doi: 10.1111/j.1447-0578.2005.00087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


