Abstract
Background
Black patients tend to receive more life-prolonging care at the end of life (EOL) than White patients. This study aimed to evaluate whether differences in patient-physician communication contribute to Black-White disparities in EOL care.
Methods
Multi-institutional prospective longitudinal cohort study of 261 White and 71 Black advanced cancer patients. Main outcome measures were Black-White differences in relationships between EOL discussions, communication goals (terminal illness awareness, treatment preferences, DNR orders), and EOL care outcomes (life-prolonging care, hospice care, receipt of care consistent with preferences).
Results
EOL discussions between physicians and their White patients were associated with less life-prolonging EOL care (adjusted odds ratio (AOR) .11, P=.04). However, more Black patients than White patients received life-prolonging care (20% versus 7%, P=.001) despite similar rates of EOL discussions (35% versus 38%, P=.65). EOL discussions were associated with attainment of some communication goals among Blacks, including placement of DNR orders (AOR 4.25, P=.04), but these communication goals were not consistently associated with EOL care received by Black patients. For example, Black patients with DNR orders were no less likely than Blacks without DNR orders to receive life-prolonging care (AOR 1.57, P=.58).
Conclusions
EOL discussions and communication goals appear to assist White patients in receiving less life-prolonging care at the EOL. Black patients, however, do not experience the same benefits of EOL discussions. Instead, Black patients tend to receive life-extending measures at the EOL even when they have DNR orders or state a preference for symptom-directed care.
Introduction
Black patients receive more life-prolonging measures and less comfort-directed care at the end of life (EOL) than White patients.1–4 Previous studies have documented higher rates of resuscitation,2, 4 intensive care unit4, 5 and feeding tube use at the EOL among Black patients,1, 4 and decreased use of hospice care relative to White patients.3, 6, 7 Although Black patients are also more likely than Whites to desire life-prolonging measures,8–10 receipt of life-prolonging care at the EOL is associated with greater distress and poorer quality of life.11 These findings raise the concern that Black patients receive inferior EOL care, a possibility underscored by Black-White disparities in certain objective care measures such as pain management.12–14
A number of explanations have been proposed for differences in care received by Black and White patients at the EOL. Black patients’ tendency to prefer life-prolonging care is one likely factor influencing disparities in EOL care.8–10 Some have argued that impaired trust between Black patients and their physicians may lead Black patients to request life-prolonging measures that they perceive as being denied them at the EOL.8, 15–17 Others have suggested that this preference reflects social, religious, and cultural values for care.18
Of note, however, previous literature has shown that Black patients have more limited baseline knowledge about advance directives than White patients.19 This finding raises the question of whether Blacks who are fully informed about the risks and benefits of life-prolonging therapy would still be more likely than Whites to request it. In addition, Black patients have been shown to be less likely to have discussions with their physicians about their preferences for resuscitation even though they often wish to have such discussions.20 Blacks tend to receive less information in their interactions with physicians21 than Whites, and family members of Black patients who have died describe more communication problems at the EOL than families of White decedents.22 Black-White differences in preferences might therefore be a function of discrepancies in patient-physician communication rather than in inherent racial differences in values for care.
Most prior research has examined discrete aspects of EOL decision-making as potential sources of disparities in EOL care. For example, studies have examined Black-White differences in care preferences,8–10 trust of clinicians,15–17 and rates of feeding tube use at the EOL1 as isolated outcomes. We used the Structural Influence Model (SIM) of Health Communication23 to conceptualize pathways from physician-patient communication to the receipt of EOL care. The SIM specifies that social factors24, 25 influence EOL communication. As depicted in Figure 1, EOL discussions lead to communication goals that then predict subsequent clinical outcomes.
Figure 1.
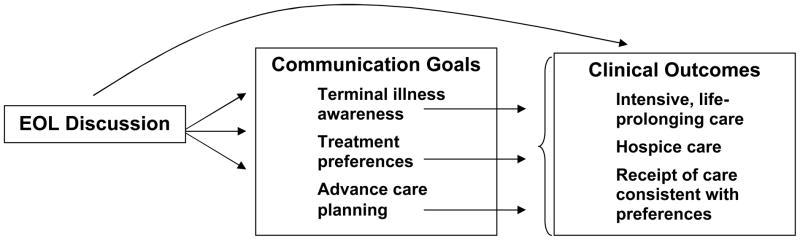
Structural Influence Model of Health Communication: The effects of EOL discussions on communication goals and clinical outcomes. Please note that the complete model, including social determinants of communication, can be found in reference number 23.
We report here findings from a multi-institutional study of 261 White and 71 Black patients with advanced cancer. We have previously reported associations between race, preferences, and intensive EOL care in this cohort,24, 25 but without evaluating mechanisms for disparities as part of an integrated model of EOL communication, and without considering a full spectrum of EOL care outcomes. This study was designed to evaluate the extent to which racial differences in the effects of EOL discussions on communication goals account for established Black-White differences in EOL care. For this study, we focused on patient communication goals rather than caregiver goals, based on our finding that patient, not caregiver, goals are most closely associated with clinical outcomes.26
We hypothesized that Blacks and Whites differ in the extent to which EOL communication relates to communication goals, including patient recognition that the illness is terminal, formulation of preferences for care, and documentation of those preferences as do-not-resuscitate (DNR) orders. EOL discussions between Black patients and their physicians, for example, might not be associated with the greater terminal illness awareness and preferences for less intensive care that we observed previously in our predominantly White cohort of advanced cancer patients.11 In addition, we hypothesized that communication goals affect clinical outcomes, such as receipt of life-prolonging care and hospice services, to differing degrees in Blacks and Whites.
Methods
Subjects were recruited as part of the Coping with Cancer Study, a multi-institutional longitudinal cohort study of advanced cancer patients and their primary caregivers.11, 27 The 332 patients included in the present study identified themselves as non-Hispanic White or Black, were recruited between October 2002 and September 2007, and died during the course of the study. Participating sites included Yale Cancer Center (New Haven, CT), Veterans’ Affairs Connecticut Healthcare System Comprehensive Cancer Clinics (West Haven, CT), Memorial Sloan-Kettering Cancer Center (New York, NY), Simmons Comprehensive Cancer Care Center (Dallas, TX), Parkland Hospital Palliative Care Service (Dallas, TX), Massachusetts General Hospital and Dana-Farber Cancer Institute (Boston, MA), and New Hampshire Oncology-Hematology (Hooksett, NH).
Patients were eligible to participate if they had cancer with distant metastases and with failure of first-line chemotherapy, were 20 years of age or older, spoke English or Spanish, were able to identify an unpaid caregiver, and had adequate stamina to complete the interview. Patient-caregiver dyads were excluded if the patient or caregiver met criteria for dementia or delirium by neurobehavioral cognitive status examination.28 All study participants provided written informed consent. Of 983 eligible patients, 691 enrolled in the full cohort study (70.3%).
Patients were asked to participate in a baseline 45-minute interview in English or Spanish; a $25 payment was provided. Interviews covered topics including sociodemographic information, quality of life,11 mental health,29, 30 coping style, religiousness,31 therapeutic alliance with the physician,32 as well as the variables described below. Chart review at enrollment and after death was used to ascertain comorbidity at enrollment, location of death, and use of invasive measures at the end of life. A post-mortem questionnaire was administered within 2 weeks of death to a caregiver (paid healthcare provider or family member) who had cared for the patient during his or her last week of life.
The institutional review boards of participating institutions approved study procedures.
Measures used in analysis are described below.
Social determinants of EOL care
Race and ethnicity
Identified through patient self-report.
Other socio-demographic characteristics
Identified through self-report of gender, age, marital status, income, health insurance status, religion, and highest grade completed in school.
Medical determinants of EOL care
Time from baseline assessment to death
Dates of death documented in medical records were used to determine survival time from baseline assessment.
Karnofsky performance status.33
Determined by the research interviewer at the time of enrollment in consultation with the treating physician.
Symptom burden
Measured using the physical symptom subscale of the McGill Quality of Life Questionnaire (MQOL).34, 35
EOL communication
EOL discussions
Patients were asked in “yes/no” format whether they and their physician had discussed any wishes about the care they would want to receive if they were dying.
Communication goals
Terminal illness awareness
Patients were asked, “Describe your current health status,” with response options of “relatively healthy,” “seriously but not terminally ill,” and “seriously and terminally ill.” Patients who described themselves as “seriously and terminally ill” were considered to be aware of their terminal illness.
Treatment preferences
Patients were asked, “if you could choose, would you prefer (1) a course of treatment that focused on extending life as much as possible, even if that meant more pain and discomfort, or (2) a plan of care that focused on relieving pain and discomfort, even if that meant not living as long?” Patients who chose the former were designated as preferring life-extending care, and those who chose the latter were designated as preferring symptom-directed care. This question has been used previously, including in the SUPPORT study.36 Patients’ informal caregivers were also asked an analogous question about patient preferences.
DNR orders
Patients were asked if they had a do-not-resuscitate order.
EOL care outcomes
Receipt of life-extending care
Defined as use of mechanical ventilation, resuscitation, or ICU care in the last week of life; determined through chart review and caregiver interviews.
Hospice care
Determined through chart review. We used receipt of hospice care for more than one week as our outcome measure, based on our previously reported finding that more than one week of hospice care was associated with better patient quality of life.11
Receipt of care consistent with preferences
Defined as concordance between baseline preferences (as defined above) and actual EOL care received. Patients who desired and received life-extending measures were designated as having received care consistent with their preferences, as were patients who desired symptom-directed care and who did not receive life-extending measures.
Statistical methods
We first examined differences in social and medical factors between Black and White patients. Differences between proportions were compared using chi-squared tests, and distributions of continuous variables were compared using t-tests.
Second, we evaluated associations between EOL discussions and our pre-defined communication goals, including terminal illness awareness, treatment preferences, and DNR orders. Logistic regression was used to determine associations in bivariable and multivariable analyses. Tables present both the unadjusted (bivariable) odds ratios from binary logistic regression, and the adjusted (multivariable) odds ratios. Adjusted models include the following confounders: patient age, gender, marital status, education, insurance, survival time, and performance status.
Third, we evaluated associations between EOL discussions, communication goals, and EOL care outcomes, defined as receipt of life-prolonging care, use of hospice care, and receipt of care consistent with preferences. Bivariable and multivariable analyses were performed as described above. Of note, we did not assess associations between preferences for care and receipt of care consistent with preferences, because of endogeneity of the predictor and outcome.
All analyses were conducted using the SAS statistical package, version 9.1.
Results
Black-White differences in sociodemographic characteristics
Black and White patients were similar with respect to gender, cancer diagnosis, performance status, symptom burden, and length of survival from baseline assessment (Table 1). However, Black patients were younger on average (P=.002), were less likely to be married (P<.0001) and insured (P<.0001), and had fewer mean years of education (P<.0001) than their White counterparts.
Table 1.
Demographic, health, and EOL care attributes among Black and White patients.
| Demographic characteristics: | Black patients (N=71) | White patients (N=261) | P value |
|---|---|---|---|
| Age in years, mean (SD) | 55.6 (11.1) | 60.5 (11.9) | .002 |
| Male gender, N(%) | 39 (55) | 146 (56) | .88 |
| Married, N(%) | 22 (31) | 164 (64) | <.0001 |
| Education in years, mean (SD) | 11.3 (3.2) | 13.9 (3.0) | <.0001 |
| Insured, N(%) | 23 (33) | 201 (79) | <.0001 |
| Religious preference, N (%) | |||
| Catholic | 4 (6) | 101 (39) | <.0001 |
| Protestant | 13 (18) | 55 (21) | |
| Baptist | 34 (48) | 22 (8) | |
| Other | 19 (27) | 68 (26) | |
| None | 1 (1) | 15 (6) | |
| Health characteristics: | |||
| Cancer type, N(%) | |||
| Lung | 19 (27) | 59 (23) | .17 |
| Colon | 12 (17) | 32 (13) | |
| Breast | 7 (10) | 21 (8) | |
| Pancreas | 2 (3) | 32 (13) | |
| Other* | 30 (43) | 111 (44) | |
| Karnofsky performance status, mean (SD) | 65.5 (14.8) | 63.5 (19.3) | .36 |
| McGill symptom burden, mean (SD) | 5.6 (1.7) | 5.5 (1.3) | .41 |
| Survival time from baseline, mean days (SD) | 191 (180) | 189 (192) | .92 |
| EOL care attributes: | |||
| EOL discussions | 24 (35) | 89 (38) | .65 |
| Terminal illness awareness | 21 (32) | 121 (41) | .15 |
| Preference for symptom-directed care, N(%) | 43 (63) | 180 (78) | .01 |
| DNR order, N(%) | 21 (31) | 115 (50) | .005 |
| Receipt of life-prolonging care, N(%) | 14 (20) | 18 (7) | .001 |
| Use of hospice care for more than one week, N(%) | 37 (52) | 157 (60) | .21 |
| Receipt of EOL care consistent with preferences, N(%) | 43 (63) | 181 (78) | .01 |
Cancer types that constituted less than 5% of the sample were designated as “Other”. Missing data: marital status (3), health insurance (10), cancer type (8), Karnofsky performance status (14), McGill symptom burden (2), EOL discussion (32), terminal illness awareness (41), hospice care (1), receipt of care consistent with preferences (32)
Black-White differences in EOL discussions, communication goals, and EOL care
Black and White patients reported similar rates of EOL discussions (35% versus 38%, respectively, P=.65) and awareness of their terminal illness (32% versus 41%, P=.15). White patients who reported having EOL discussions with their physicians tended to have worse performance status (mean Karnofsky score 56 versus 66, P=.0001) and a shorter survival time from baseline (mean days 136 versus 223, P=.0004) than Whites who had not had EOL discussions. Blacks with more years of education (mean years 12.0 versus 10.8, P=.06) were marginally more likely to report having had EOL discussions.
Despite similar rates of EOL discussions, White patients were more likely than Blacks to prefer symptom-directed therapy over life-extending care (78% versus 63%, P=.01) and to have DNR orders in place (50% versus 31%, P=.005). Whites were also less likely to receive life-prolonging care in their last week of life (7% versus 20%, P=.001, Table 1).
The Structural Influence Model (SIM) of health communication in White patients
EOL discussions in White patients were associated with several communication goals and EOL care outcomes. For example, Whites who reported EOL discussions with their physicians were more likely to be aware that they were terminally ill (adjusted odds ratio (AOR) 3.06, P=.0006, Table 2), to prefer symptom-directed over life-extending care (AOR 2.23, P=.05), and to have DNR orders in place (AOR 2.82, P=.001) than patients who had not had such discussions. EOL discussions were also directly associated with EOL care, such that White patients who reported EOL discussions were less likely to receive life-prolonging care (OR .11, P=.04, Table 3), more likely to use hospice care (AOR 1.99, P=.04), and more likely to receive care that was consistent with their baseline preferences (AOR 2.59, P=.02) than those who had not had EOL discussions. Finally, communication goals of EOL discussions were associated with some EOL care outcomes (Table 4). For example, Whites who had DNR orders were less likely to receive life-prolonging care (AOR .15, P=.02) and more likely to receive EOL care that was consistent with their baseline preferences (AOR 4.91, P<.0001) than Whites without DNR orders. Whites who were aware that they were terminally ill were also less likely to receive life-prolonging care (AOR .26, P=.05).
Table 2.
Relationships between EOL discussions and communication goals in Black and White patients.
| EOL discussions All patients | EOL discussions Black patients | EOL discussions White patients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||
| Communication goals | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p |
| Terminal illness awareness | 3.24 [1.98, 5.30] | <.0001 | 2.96 [1.72, 5.09] | <.0001 | 2.01 [.70, 5.83] | .20 | 2.46 [.60, 10.14] | .21 | 3.76 [2.14, 6.60] | <.0001 | 3.06 [1.62, 5.80] | .0006 |
| Preference for symptom-directed care | 2.30 [1.27, 4.15] | .006 | 2.63 [1.36, 5.10] | .004 | 3.17 [1.00, 10.00] | .05 | 3.85 [.93, 15.87] | .06 | 2.13 [1.14, 3.96] | .02 | 2.23 [.99, 4.99] | .05 |
| DNR order | 3.53 [2.15, 5.81] | <.0001 | 2.92 [1.70, 5.01] | <.0001 | 2.88 [.99, 8.37] | .05 | 4.25 [1.10, 16.45] | .04 | 3.87 [2.17, 6.89] | <.0001 | 2.82 [1.50, 5.31] | .001 |
Note: Odds ratios represent the odds of the communication goals when the patient reported that an EOL discussion took place. Adjusted models account for sex, age, survival time from baseline assessment, performance status, educational level, marital status, and insurance status.
Table 3.
Relationships between EOL discussions and care received in Black and White patients.
| EOL discussions All patients | EOL discussions Black patients | EOL discussions White patients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||
| EOL care received | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p |
| Receipt of life-prolonging care (ventilator, resuscitation, or death in the ICU) | .23 [.08, .67] | .007 | .27 [.09, .82] | .02 | .43 [.11, 1.72] | .23 | .29 [.06, 1.39] | .12 | .10 [.01, .75] | .03 | .11 [.01, .90] | .04 |
| Use of hospice care for more than one week | 2.08 [1.27, 3.43] | .004 | 1.87 [1.10, 3.17] | .02 | 1.67 [.60, 4.60] | .32 | 2.15 [.67, 6.83] | .20 | 2.22 [1.25, 3.94] | .006 | 1.99 [1.05, 3.77] | .04 |
| Receipt of EOL care consistent with preferences | 1.97 [1.11, 3.50] | .02 | 2.01 [1.07, 3.75] | .03 | 1.26 [.44, 3.58] | .67 | 1.61 [.46, 5.68] | .45 | 2.37 [1.16, 4.83] | .02 | 2.59 [1.15, 5.85] | .02 |
Adjusted models account for sex, age, survival time from baseline assessment, performance status, educational level, marital status, and insurance status.
Table 4.
Relationships between communication goals and EOL care received in Black and White patients.
| All patients | Black patients | White patients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||
| Relationships between terminal illness awareness and EOL care | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p | OR [95% CI] | p |
| Receipt of life-prolonging care (ventilator, resuscitation, or death in the ICU) | .45 [.19, 1.06] | .07 | .39 [.16, 1.00] | .05 | 1.45 [.41, 5.11] | .57 | .60 [.11, 3.41] | .57 | .23 [.07, .85] | .03 | .26 [.07, 1.01] | .05 |
| Use of hospice care | 1.61 [1.00, 2.59] | .05 | 1.65 [.97, 2.81] | .06 | 1.42 [.49, 4.09] | .51 | 3.42 [.83, 14.22] | .09 | 1.62 [.94, 2.78] | .08 | 1.33 [.71, 2.48] | .38 |
| Receipt of EOL care consistent with preferences | 1.61 [.93, 2.78] | .09 | 1.76 [.96, 3.23] | .07 | .90 [.31, 2.62] | .84 | 1.30 [.29, 5.91] | .74 | 1.78 [.93, 3.41] | .08 | 2.14 [.99, 4.62] | .05 |
| Relationships between preference for symptom-directed care and EOL care | ||||||||||||
| Receipt of life-prolonging care (ventilator, resuscitation, or death in the ICU) | .31 [.14, .68] | .003 | .36 [.15, .85] | .02 | .50 [.15, 1.65] | .25 | .23 [.04, 1.30] | .10 | .28 [.10, .82] | .02 | .31 [.10, 1.00] | .05 |
| Use of hospice care | 1.75 [1.03, 2.96] | .04 | 1.60 [.91, 2.83] | .10 | 3.32 [1.19, 9.29] | .02 | 4.53 [1.23, 16.71] | .02 | 1.31 [.69, 2.46] | .41 | 1.16 [.57, 2.34] | .69 |
| Relationships between DNR orders and EOL care | ||||||||||||
| Receipt of life-prolonging care (ventilator, resuscitation, or death in the ICU) | .32 [.13, .78] | .01 | .41 [.16, 1.03] | .06 | 1.32 [.38, 4.56] | .66 | 1.57 [.31, 7.90] | .58 | .13 [.03, .56] | .007 | .15 [.03, .75] | .02 |
| Use of hospice care | 1.33 [.83, 2.13] | .23 | 1.17 [.70, 1.96] | .55 | 1.56 [.55, 4.45] | .41 | 2.92 [.78, 11.00] | .11 | 1.22 [.72, 2.09] | .46 | 1.02 [.56, 1.86] | .95 |
| Receipt of EOL care consistent with preferences | 3.13 [1.76, 5.56] | .0001 | 3.15 [1.69, 5.88] | .0003 | 1.24 [.42, 3.66] | .70 | 1.17 [.30, 4.60] | .82 | 3.99 [1.99, 8.01] | .0001 | 4.91 [2.22, 10.83] | <.0001 |
Adjusted models account for sex, age, survival time from baseline assessment, performance status, educational level, marital status, and insurance status.
The SIM in Black patients
As in White patients, EOL discussions were associated with attainment of some communication goals among Blacks. For example, Blacks who reported EOL discussions with their physicians were more likely to prefer symptom-directed care (AOR 3.85, P=.06, Table 2) and to have DNR orders in place (AOR 4.25, P=.04). However, unlike relationships seen in Whites, EOL discussions were not directly associated with EOL care outcomes among Black patients (Table 3), and attainment of communication goals was not consistently associated with EOL care (Table 4). Although a preference for symptom-directed care was associated with a higher likelihood that Black patients used hospice care in the last week of life (AOR 4.53, P=.02), DNR orders neither decreased the likelihood that Black patients received life-prolonging measures (AOR 1.57, P=.58) nor increased the likelihood that Blacks received care consistent with their preferences (AOR 1.17, P=.82).
To evaluate this finding further, we examined baseline preferences of Black patients’ informal caregivers, to assess whether family preferences for life-extending care might account for the use of such care despite DNR orders. Although some (N=5) caregivers of Black patients did express a preference for life-extending care when the patient preferred symptom-directed care, none of these patients ultimately received life-prolonging measures.
Discussion
White patients with advanced cancer who engage in EOL discussions with their physicians are less likely to receive intensive, life-prolonging care at the EOL, an effect that appears to work through resultant patient awareness that their illness is terminal, preferences for symptom-directed care, and the documentation of preferences with DNR orders. Black patients, however, tend to receive life-prolonging care at the EOL despite similar rates of EOL discussions to those reported by Whites, and even despite important potential goals of those discussions, such as DNR orders and preferences for symptom-directed care.
Previous literature suggests that more frequent receipt of life-prolonging care at the EOL by Blacks may be a reflection of preferences for such care.8–10 Blacks in our study did express a preference for life-prolonging care more often than Whites. However, our results do not appear to be fully explained by differing preferences; even when Blacks had DNR orders, they were no less likely to receive mechanical ventilation, CPR, or ICU care in the last week of life than Blacks without DNR orders. Similarly, Blacks who had DNR orders were no more likely than other Black patients to receive EOL care that reflected their preferences. Although EOL discussions and communication goals assist White patients in receiving less burdensome, life-prolonging care at the EOL, Black patients tend to receive more aggressive care regardless of their preferences.
The Structural Influence Model of Health Communication allows us to consider some possible etiologies for the observed disparities. For example, previous work suggests that disparities in communication may be a major underlying force driving Black-White differences in care received.19, 21, 22, 37 In our study, EOL discussions were not associated with heightened terminal illness awareness among Black patients. It is possible that sustained effects of EOL communication are mediated in part through recognition of one’s terminal illness, such that Black patients who do not recognize that their illness is terminal may ultimately be more likely to receive life-prolonging EOL care. In addition, other unmeasured communication attributes, such as the timing of EOL communication relative to diagnosis, the content of conversations, or the extent to which physicians returned to such conversations over time, may explain why Black patients would experience communication goals of EOL discussions in the short term, but not the EOL care outcomes months later. Future research should consider the extent to which the nature of EOL discussions differs between Blacks and Whites.
Our findings also raise the possibility that wider issues within the health care system, beyond patient-physician communication, could explain the major disparity we have identified--the translation of preferences into care. Whites may have greater continuity of providers and sites of care, for example, making DNR orders and known or documented preferences available at every encounter. Alternatively, racial bias on the part of providers about patient preferences could play a role.
Although we have found that the communication goals of EOL discussions have a limited impact on EOL care among Black patients with advanced cancer, an important exception is the increased use of hospice care at the EOL among Blacks who reported a preference for symptom-directed care. This is a potentially significant outcome given evidence that hospice care is underutilized among Black patients at the EOL.3, 7 This finding, and our finding of communication goals of EOL discussions among Blacks, suggest that EOL discussions remain an important aspect of care of all advanced cancer patients, regardless of race. Nonetheless, more work is needed to identify ways to help Black patients receive the same benefits of such discussions as White patients.
Alternative explanations for our findings deserve consideration. Importantly, months elapsed between ascertainment of baseline preferences and the patient’s death. It is possible that Black patients’ preferences were more likely than Whites’ to change over time. Previous literature has documented that Black patients are more likely to leave hospice care before death in order to pursue life-prolonging care,38, 39 and to rescind DNR orders than Whites.20 However, the latter study also documented communication problems between Blacks and their physicians, with Blacks more likely to want to discuss preferences for CPR with their physicians than Whites and less likely to have such discussions.20 Although similar numbers of White and Black patients in our study reported EOL discussions, these findings raise the question of whether communication problems experienced by Black patients underlie changes in preferences for care over time.
In addition, because we measured attributes of care in the last week of life, surrogate decision-makers may have played a role in deciding about the patient’s care during that period. Although we did find discordance between patient and caregiver preferences for care among Blacks, these familial differences were not associated with increased use of life-prolonging EOL care.
Our study has several limitations. Most importantly, our study included relatively small numbers of Black patients. Many of the relationships studied in Blacks had odds ratios in similar directions to those of Whites, although often with attenuated magnitude. A larger study would enable us to determine whether some of the non-significant results we have found among Black patients are true negative relationships.
In addition, we have evaluated markers of life-prolonging care, but a broad array of attributes may define a patient’s experience of quality EOL care. Future research should continue to evaluate the best ways to measure patient experiences of care at the EOL. We have also posited a model of EOL communication in which discussions lead to communication goals and thereby affect care received. However, we do not know whether EOL discussions cause the examined outcomes, or whether patient-level differences account for the associations observed. We also used patient reports of EOL discussions, but we do not know the extent to which patient reports of discussions reflect actual discussions and their content. Future research using additional tools such as direct observation or audiotaping is needed to determine discrepancies between what is said and what is heard and whether this varies by race. Finally, psychometric data for our questionnaire items are not available by race. It is possible that patients of different races interpreted questions differently or considered different issues important, and this could account for some of our findings.
Both Black and White patients appear to benefit from EOL discussions in terms of development and documentation of care preferences. Why Blacks do not ultimately experience care that consistently reflects those preferences is unclear. We have considered explanations for our findings, such as Black-White disparities in the effects of EOL communication and broad differences in the ways health care systems support Black and White patients at the EOL. These issues should remain a topic of ongoing research and a priority for physicians who care for patients at the EOL. Although the reasons for our findings are not fully understood, White patients appear to have undefined advantages when it comes to receiving EOL care that reflects their values. Care of dying Black patients must be brought to the same standard.
Acknowledgments
This research was supported in part by the following grants to Dr. Prigerson: MH63892 from the National Institute of Mental Health and CA106370 from the National Cancer Institute; a Fetzer Religion at the End-of-Life Grant; the Center for Psycho-Oncology and Palliative Care Research, Dana-Farber Cancer Institute. Dr. Mack was supported by an American Cancer Society Mentored Research Scholar Grant.
References
- 1.Mitchell SL, Teno JM, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. Jama. 2003 Jul 2;290(1):73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 2.Goodlin SJ, Zhong Z, Lynn J, et al. Factors associated with use of cardiopulmonary resuscitation in seriously ill hospitalized adults. Jama. 1999 Dec 22–29;282(24):2333–2339. doi: 10.1001/jama.282.24.2333. [DOI] [PubMed] [Google Scholar]
- 3.Virnig BA, Kind S, McBean M, Fisher E. Geographic variation in hospice use prior to death. J Am Geriatr Soc. 2000 Sep;48(9):1117–1125. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- 4.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009 Mar 9;169(5):493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnato AE, Chang CC, Saynina O, Garber AM. Influence of race on inpatient treatment intensity at the end of life. J Gen Intern Med. 2007 Mar;22(3):338–345. doi: 10.1007/s11606-006-0088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haas JS, Earle CC, Orav JE, et al. Lower use of hospice by cancer patients who live in minority versus white areas. J Gen Intern Med. 2007 Mar;22(3):396–399. doi: 10.1007/s11606-006-0034-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greiner KA, Perera S, Ahluwalia JS. Hospice usage by minorities in the last year of life: results from the National Mortality Followback Survey. J Am Geriatr Soc. 2003 Jul;51(7):970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 8.Blackhall L, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes toward life sustaining technology. Soc Sci Med. 1999;48:1779–1789. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 9.Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009 Jun;24(6):695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phipps E, True G, Harris D, et al. Approaching the end of life: attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. J Clin Oncol. 2003 Feb 1;21(3):549–554. doi: 10.1200/JCO.2003.12.080. [DOI] [PubMed] [Google Scholar]
- 11.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Jama. 2008 Oct 8;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. Jama. 1998 Jun 17;279(23):1877–1882. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 13.Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group Minority Outpatient Pain Study. Ann Intern Med. 1997 Nov 1;127(9):813–816. doi: 10.7326/0003-4819-127-9-199711010-00006. [DOI] [PubMed] [Google Scholar]
- 14.Morrison RS, Wallenstein S, Natale DK, Senzel RS, Huang LL. “We don’t carry that”--failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. N Engl J Med. 2000 Apr 6;342(14):1023–1026. doi: 10.1056/NEJM200004063421406. [DOI] [PubMed] [Google Scholar]
- 15.Gordon HS, Street RL, Jr, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol. 2006 Feb 20;24(6):904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 16.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004 Apr;7(2):247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 17.Matthews AK, Sellergren SA, Manfredi C, Williams M. Factors influencing medical information seeking among African American cancer patients. J Health Commun. 2002 May-Jun;7(3):205–219. doi: 10.1080/10810730290088094. [DOI] [PubMed] [Google Scholar]
- 18.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. Jama. 2000 Nov 15;284(19):2518–2521. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 19.Murphy ST, Palmer JM, Azen S, Frank G, Michel V, Blackhall LJ. Ethnicity and advance care directives. J Law Med Ethics. 1996 Summer;24(2):108–117. doi: 10.1111/j.1748-720x.1996.tb01843.x. [DOI] [PubMed] [Google Scholar]
- 20.Borum ML, Lynn J, Zhong Z. The effects of patient race on outcomes in seriously ill patients in SUPPORT: an overview of economic impact, medical intervention, and end-of-life decisions. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000 May;48(5 Suppl):S194–198. doi: 10.1111/j.1532-5415.2000.tb03132.x. [DOI] [PubMed] [Google Scholar]
- 21.Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors’ information-giving and patients’ participation. Cancer. 2006 Sep 15;107(6):1313–1320. doi: 10.1002/cncr.22122. [DOI] [PubMed] [Google Scholar]
- 22.Welch L, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005;53(7):1145–1153. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 23.Viswanath K, Ramanadhan SR, Kontos EZ. Mass Media and Population Health: A Macrosocial View. In: Galea S, editor. Macrosocial Determinants of Population Health. Springer; 2007. pp. 275–294. [Google Scholar]
- 24.Trice Loggers E, Maciejewski PK, Paulk E, Desanto-Madeya S, Nilsson M, Viswanath K, Wright AA, Balboni TA, Temel J, Stieglitz H, Block S, Prigerson HG. Racial Differences in Predictors on Intensive End-of-Life Care in Advanced Cancer Patients. Journal of Clinical Oncology. 2009 doi: 10.1200/JCO.2009.22.4733. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008 Sep 1;26(25):4131–4137. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright A, Mack JW, Balboni T, Massaro A, Matulonis U, Block S, Prigerson H. Influence of Patients’ Preferences and Treatment Site on Cancer Patients’ End-of-Life Care. 2009 doi: 10.1002/cncr.25217. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mack JW, Nilsson M, Balboni T, et al. Peace, Equanimity, and Acceptance in the cancer experience (PEACE): validation of a scale to assess acceptance and struggle with terminal illness. Cancer. 2008 Apr 21; doi: 10.1002/cncr.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiernan RJ, Mueller J, Langston JW, Van Dyke C. The Neurobehavioral Cognitive Status Examination: a brief but quantitative approach to cognitive assessment. Ann Intern Med. 1987 Oct;107(4):481–485. doi: 10.7326/0003-4819-107-4-481. [DOI] [PubMed] [Google Scholar]
- 29.Morina N, Rudari V, Bleichhardt G, Prigerson HG. Prolonged grief disorder, depression, and posttraumatic stress disorder among bereaved Kosovar civilian war survivors: A preliminary investigation. Int J Soc Psychiatry. 2009 Jul 10; doi: 10.1177/0020764008101638. [DOI] [PubMed] [Google Scholar]
- 30.Zhang B, Mitchell SL, Bambauer KZ, Jones R, Prigerson HG. Depressive symptom trajectories and associated risks among bereaved Alzheimer disease caregivers. Am J Geriatr Psychiatry. 2008 Feb;16(2):145–155. doi: 10.1097/JGP.0b013e318157caec. [DOI] [PubMed] [Google Scholar]
- 31.Phelps AC, Maciejewski PK, Nilsson M, et al. Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. JAMA. 2009 Mar 18;301(11):1140–1147. doi: 10.1001/jama.2009.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009 Jul 15;115(14):3302–3311. doi: 10.1002/cncr.24360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karnofsky DA. Determining the extent of the cancer and clinical planning for cure. Cancer. 1968 Oct;22(4):730–734. doi: 10.1002/1097-0142(196810)22:4<730::aid-cncr2820220407>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 34.Cohen SR, Mount BM, Bruera E, Provost M, Rowe J, Tong K. Validity of the McGill Quality of Life Questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med. 1997 Jan;11(1):3–20. doi: 10.1177/026921639701100102. [DOI] [PubMed] [Google Scholar]
- 35.Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995 Jul;9(3):207–219. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 36.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 37.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003 Feb;18(2):146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kapo J, MacMoran H, Casarett D. “Lost to follow-up”: ethnic disparities in continuity of hospice care at the end of life. J Palliat Med. 2005 Jun;8(3):603–608. doi: 10.1089/jpm.2005.8.603. [DOI] [PubMed] [Google Scholar]
- 39.Johnson KS, Kuchibhatla M, Tanis D, Tulsky JA. Racial differences in hospice revocation to pursue aggressive care. Arch Intern Med. 2008 Jan 28;168(2):218–224. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]


