Abstract
Background:
Fractures of the distal femur comprise 4% to 6% of all femoral fractures. Elderly patients are predisposed to low-energy fractures due to osteoporosis. Treatment of these fractures in the elderly group remains a challenge. Our hypothesis is that locking plates inserted with minimally invasive plate osteosynthesis (MIPO) techniques will produce better results compared to those inserted by open technique. The objective of this study is to evaluate the clinical outcomes of MIPO technique using locking plates in the elderly patients.
Materials and Methods:
A total of 24 elderly patients (mean age 73 years) with distal femur fractures treated using the MIPO technique (2007-2010) were reviewed retrospectively. Parameters analyzed included classification of fracture, time to fracture union, knee range of motion, functional knee score (Knee Society Score—Functional) at 6 months, and other significant complications. One patient was lost to follow-up.
Results:
In all, 88% of the fractures were extraarticular. The mean time to union was 13.48 (range: 8-28) weeks. Mean range of motion achieved at 6 months and beyond was 100° ranging from 0 to 30 (extension) to 90 to 140 (flexion). Functional knee scores at 6 months from fixation were satisfactory (mean score 88.8). There were no cases of implant failure, nonunion, and infection. In all, 6 (25%) patients developed deep vein thrombosis (DVT) in the early postoperative period, all of which were below the level of the knee joint.
Conclusion:
Locking plates inserted using MIPO techniques in elderly patients with distal femur fractures appear to be promising based on clinical outcome measurements. However, there was a high incidence of DVT noted.
Keywords: distal femur fracture, geriatric population, locking plates, minimally invasive
Introduction
Fractures of the distal femur comprise 4% to 6% of all femoral fractures.1 Although, they are 10 times less common than the proximal femur fractures,2 they represent the second most frequent fracture of the femur in the elderly patients.3 Operative treatment is usually necessary to permit early rehabilitation and mobilization. The presence of osteoporosis, comminution, and intraarticular extension often makes it challenging to use intramedullary fixation. Hence, extramedullary implants such as 95°condylar screw plate, 95° Angle Blade Plate (ABP), and locking Condylar Plate are more favorable in such cases. Although open reduction, combined with stable internal fixation, is achievable in some cases, a wide surgical exposure particularly in the complex fracture patterns risks nonunion and infection due to the compromise in fixation stability and the local blood supply.
The concept of bridge plating with locking plates has enabled a minimally invasive approach and indirect reduction techniques, with the aim of circumventing the above-mentioned problems.4 Our hypothesis is that locking plates inserted with minimally invasive plate osteosynthesis (MIPO) technique will produce better results compared to those inserted by open technique. The objective of this study is to evaluate the surgical outcomes of MIPO using anatomical locking plates as a surgical option in elderly patients with osteoporotic fractures. To our knowledge, there has been no study describing the clinical outcomes of this specific fracture type in older patients using locking plates with MIPO techniques.
Materials and Methods
A retrospective case series study was performed in a busy, level I trauma academic center. All patients aged 55 years and older with closed distal femoral fractures were included in the study. Patients who were medically unfit to undergo surgery (due to high risk of anesthesia) or opted for nonsurgical management were excluded from the study.
A total of 25 patients met our inclusion criteria. All patients were treated between January 2007 and December 2010. One patient was lost to follow–up, leaving 24 patients to analyze. All patients had low-energy injuries secondary to falls. In all cases, these were solitary injuries. According to the (AO/Orthopaedic Trauma Association [OTA]) classification, majority (20) of the patients had type A, 3 had type B, and 1 had type C fractures. All patients underwent surgery within 2 weeks from the time of the injury. Preoperatively, a Robert Jones dressing was applied to all patients including a posterior plaster slab or light skin traction. Based on our hospital protocol, all patients received mechanical thromboprophylaxis with thrombo embolic deterrent (TED) stockings and mechanical calf pumps. There was no routine use of pharmacological prophylaxis. A lower limb duplex scan was performed in all patients to rule out deep vein thrombosis (DVT) on day 5 postinjury.
Surgically, a small incision over the distal lateral thigh was made initially, and locking anatomical plate (Synthes LISS or Zimmer Periarticular Plate, Singapore) was introduced submuscularly. To achieve articular reduction in complex cases, the incision was deepened and extended intra-articularly. An additional small incision was made proximally to localize and centralize the plate over the lateral cortex. The distal femur fragments were reduced with clamps and K-wires based on fracture configuration. With manual traction, satisfactory length and rotation were achieved, and the plate was secured to the bone with distal and proximal wires. This was followed by screw fixation distally and proximally under image intensifier guidance to confirm the position. Lag screws were used when required to reduce the fracture in relation to the plate and followed by the locking screw insertion sequentially on either side to hold the plate to the bone.
Postoperatively, the patients were treated with continuous passive knee movement until more than 70° flexion was achieved. The patients were also routinely subjected to TED stockings and calf palms immediately postoperatively till the day of discharge. All patients that received physiotherapy beginning on postoperative day 1 were allowed to full weight bear as tolerated. Patients were followed-up at the outpatient clinic at regular intervals of 3, 6, and 9 months and 1 and 2 years postoperatively. Parameters analyzed included demographics, type of fracture pattern, time to radiographic fracture union, knee range of motion, and functional knee score (Knee Society Score) at 6 months. The scoring was performed during the outpatient follow-up review. Any related clinical complications were recorded.
Results
The mean age of the population was 73.08 (57-94) years. There was, as expected, a predominance of females (22 patients) with a mean age of 73.41 years. The mean age for the 2 males was 69.5 (67 and 72) years. In all, 15 fractures were on the right side and 9 on the left. No patient had bilateral fractures. The mean time to surgery was 4.5 (1-11) days. Based on the AO/OTA classification system, 88% (21) of the patients had extra-articular fractures. The majority (62.5%) of the fractures were type A1.
Radiographic presence of trabeculae across the fracture site with the absence of pain on palpation and weight bearing was defined as union. The mean time to union was 13.48 (8-24) weeks, and none required a reoperation. The mean time to follow-up was 15.3 (8-24) months. The functional range at 6 months was encouraging, as all patients achieved a minimum flexion of 90° (90-140; mean, 113.4°). The range of extension deficit recorded was up to a maximum of 30° (0-30; mean, 4.8°). There were no cases with hyperextension. Based on the Knee Society Scoring system, the mean knee score was 88.8 (76-97), and the mean functional score was 76 (45-100). Based on the grading of knee scores, less than 20% of the patients had poor results (Table 1).
Table 1.
Functional Outcome.
| Age, Years | Range of Movement | AO Classification | Functional Knee Score | DVT |
|---|---|---|---|---|
| 94 | 0-130 | A1 | 45 | |
| 57 | 10-140 | A1 | 90 | |
| 67 | 10-130 | A1 | 70 | |
| 62 | 30-90 | A3 | 55 | |
| 78 | 10-90 | C1 | 75 | |
| 64 | 20-120 | A1 | 80 | |
| 93 | 10-110 | A3 | 45 | |
| 62 | 0-120 | A1 | 90 | |
| 64 | 0-100 | A3 | 80 | + ve |
| 79 | 0-110 | B1 | 75 | |
| 62 | 0-120 | A1 | 80 | |
| 60 | 5-120 | A2 | 90 | |
| 77 | 10-100 | A1 | 90 | |
| 83 | 0-100 | A1 | 80 | + ve |
| 69 | 10-120 | A1 | 90 | |
| 58 | 10-100 | A1 | 100 | |
| 78 | 10-100 | A1 | 55 | |
| 84 | 0-120 | A1 | 70 | |
| 78 | 10-110 | A1 | 75 | |
| 83 | 0-100 | A2 | 65 | |
| 92 | 10-120 | C1 | 80 | + ve |
| 77 | 10-120 | C3 | 75 | + ve (above knee) |
| 72 | 0-90 | A1 | 75 | + ve |
| 61 | 0-120 | A1 | 90 |
Abbreviations: DVT, deep vein thrombosis; +ve, positive.
There were no reported cases of implant loosening, cutout, or failure. All wounds healed well with no evidence of infection. All received 48 hours of intravenous antibiotics postoperatively based on our hospital protocol. There were no mortalities reported. The routine duplex scan of the lower limb revealed a high prevalence of DVT. The DVT was positive in 5 (20.8%) patients. Four had DVT confined to veins below the level of the knee, and the other had a proximal extension involving the superficial femoral vein. All were subjected to pharmacological treatment upon review by the hematologist. None had a preceding history of DVT or any other compounding factors to suggest an increased risk. Although not statistically significant, the prevalence is considerably significant. None had clinical signs of pulmonary embolism as a complication. The other complications noted were urinary tract infection (1 patient) and pneumonia (1 patient), which resolved with antimicrobial treatment.
Discussion
Fractures involving the femur in older adults are reasonably common. Distal femur fractures in this age group can be quite challenging. Some important concerns from the surgeon’s point of view include bone quality, healing potential, and achieving a good functional outcome. Locked plates and the MIPO technique has to a certain extent helped to address these challenges.
Locked plates are increasingly used for indirect reduction in diaphyseal/metaphyseal fractures in osteoporotic bones and when bridging severely comminuted fractures.5 A biologically friendly approach can improve early and long-term outcomes in trauma care.6 Locking plates with angular stable screws have shown effectiveness in maintaining fracture reduction and stability.7 The anatomical locking plates are designed to be placed on the lateral aspect of the distal femur with adequate screws for secure fixation in a locking mode. The primary goal of surgery with locking plates is to achieve union with bridging callus through relative stability which allows movement at the fracture gap. The biomechanical principle of relative stability allows a relative dynamic deformation,8 which induces secondary callus formation when compared to primary callus formation in absolute stability. Hence, the difference in the fixation stability (absolute or relative) stimulates a different mechanobiologic process for fracture healing altogether.9 Compared to other fixation modalities (nailing, conventional plates, and dynamic compression screw), the anatomical locking plates provide improved distal fixation at the expense of reduced movement at the fracture site.10 This feature makes the locking plate a reasonable implant of choice in the elderly patients with osteoporosis.
The MIPO techniques complement locking plate technology. Careful tissue handling helps to maintain tissue viability. Equally important is to preserve the periosteal blood supply to maximize healing potential. Minimally invasive approach allows fixation of a bone through smaller surgical incisions. It allows positioning of the plate in the submuscular plane thus reducing iatrogenic injury to the periosteum. Less surgical trauma to tissues can lead to further improvements in clinical results.11 Minimally invasive surgical methods may be biologically more advantageous than the traditional method,12 as it improves the rate of fracture healing, decreases the need for bone grafting, and lowers the incidence of infection and other complications.1 A recent study has validated the clinical advantages of MIPO technique with locking plates in treatment of distal femur periprosthetic fractures.13 In our study, there were no complications of infection, wound breakdown, or nonunion resulting from surgical approach, technique, and choice of implant. The complications seen in our population were urinary tract infection and pneumonia, which resolved with treatment. We had no mortalities during the 2-year follow-up, though reports have shown mortality rates of up to 0.05% (1 month), 16% (6 months), and 20% (12 months) after distal femur fractures in the elderly patients.14 Mortality rates in this group of patients have also been shown to increase in the presence of medical complications.15
Plate breakage can result from delayed union or nonunion in the presence of loading. Nevertheless, reoperation for plate breakage and nonunion in distal femur fractures stabilized with locking plates with a minimally invasive approach in the elderly population has been reported to be low.16 In our study, all fractures united without reoperation. We attributed to the use of a long spanning plate in a locking mode that promotes callus formation by relative stability (Figures 1 and 2). Nevertheless, loading is needed to stimulate the healing process. A recent study in Asia reported cases of failures when short locking plates were used.17 The use of long plates theoretically increases the plate’s working length and hence improves the number of cycles it can withstand load until failure.18 This fixation principle in our elderly population allowed early loading (full weight bearing as tolerated) even in the presence of delayed union (>12 weeks) without subsequent implant failure or screw loosening. The added advantage of allowing early mobilization and ambulation is of paramount importance particularly in the elderly patients to prevent complication of prolonged immobility such as DVT, pneumonia, urinary tract infection, bed sores, and joint contractures among other possible medical complications that could lead to an increased incidence of mortality.
Figure 1.

Long spiral distal femur fracture.
Figure 2.

Union at 6 months following a locking plate (minimally invasive plate osteosynthesis technique).
In our study, the functional outcome was good at 6 months with satisfactory range of motion. All patients had a minimum of 90° flexion, with the maximum range of flexion achieved being 140°. Extension deficit (inability to achieve full extension) of 5° to 10° was present in 12 patients and a lack of 30° in 2 patients. This may represent a reflection of the patient’s preinjury functional range of motion. Furthermore, an older patient’s ability to comprehend and comply with physiotherapy may be a challenge to the rehabilitation efforts. This may be another factor contributing to the failure of achieving full extension postoperatively (14 patients). There was also a considerable delay to surgery (mean time to surgery of 4.5 days) due logistic concerns and delay in getting consent from the patients. This could have further contributed to the deficits in knee motion. However, all patients were able to achieve full extension when passively ranged with no presence of hyperextension. This reflects an absence of malreduction in the sagittal plane. There was no clinical evidence of rotational and coronal malalignment with equal limb lengths. The mean arc of knee flexion in a study of distal femur fractures (mean age of 52, n = 99) treated with locking plates has been reported to be 1°to 109°.19 Similarly, the elderly population cohort from our study achieved a comparable result, with the mean arc of knee flexion being 4.8° to 113.3°. These results are promising considering that the mean age of our study population (73.08) was almost 20 years. Furthermore, it was interesting to note that more than 80% of the patients in our study achieved a fair to excellent grade based on the Knee Society Functional Scores (Figure 3). The functional ability will influence mobility and hence can potentially reduce the risk of developing postoperative thrombosis and other complications related to immobility.
Figure 3.
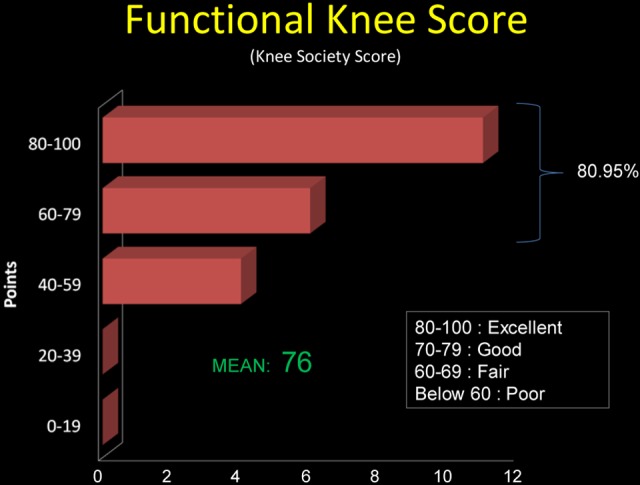
Graph 1: functional knee score grading.
Clinical complications in our study were rare. Although the functional outcomes in our study were favorable, there was a high prevalence of DVT (5 patients) with risk factors for the lower limb fracture and advanced age. A study in Canada has shown an overall 28% incidence of clinically occult DVT in fractures distal to the hip of which 40% involved the femoral shaft and 43% involving the tibial plateau.20 The value of giving chemoprophylaxis in the elderly patients with distal femur fracture in our Asian population cohort is controversial, hence it was not routine in our practice. Many reports have shown that the incidence of DVT in Asian population is significantly low,21-22 and hence chemoprophylaxis may not be justified in isolated upper or lower extremity fractures. Nevertheless, there are studies in the Asian population which suggest the need for mechanical or pharmacological prophylaxis for major orthopedic surgeries, as the incidence is comparable to Western populations.23-24 Although routine use of pharmacological thromboprophylaxis preoperatively was not practiced in our setting, all patients in our study received mechanical prophylaxis preoperatively and postoperatively. Five patients diagnosed to have DVT in our study were given appropriate pharmacological treatment after consultation with a hematologist. Lower limb venous thrombosis is a known complication in complex, high-velocity knee injuries; however, there has been no such reports in low-velocity distal femur fractures in the elderly patients. The guidelines by the American College of Chest Physicians clearly recommend chemoprophylaxis for major orthopedic surgeries (total hip replacement, total knee surgery, and hip fracture surgery); however, it is not recommended for injuries distal to the knee.25 The findings from our study highlight the importance of having a high index of suspicion for occult DVT in low-velocity distal femur fractures in the elderly patients. Besides mechanical thromboprophylaxis, there may be a significant role for the use of chemoprophylaxis in low velocity distal femur fractures in the elderly patients in the absence of relative or absolute contraindications. To be certain of the prophylaxis regimen, additional studies are necessary to determine the role of DVT prophylaxis in the management of distal femur fractures in the elderly patients.
Limitations
Sample size was a limiting factor in our study. Another limitation is the lack of a control group treated during the same time period. Furthermore, we had no data concerning comorbidities and osteoporosis, which may have a significant effect on the outcome of elderly patients.
Conclusions
The MIPO technique combined with distal femur locking plates resulted in favorable outcomes in our small case series of older adults. The technique appears to be useful and safe. All patients treated with this technique healed and had satisfactory functional outcomes with no mortalities and few postoperative complications. However, a 20% incidence of DVT was noted and suggests the need for routine chemoprophylaxis therapy in this elderly patients with distal femur fracture. Additional study is needed to confirm these findings.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the less invasive stabilization system (LISS): the technique and early results. Injury. 2001;32(suppl 3):SC32–SC47 [DOI] [PubMed] [Google Scholar]
- 2. Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. Epidemiology of fractures of the distal femur. Injury. 2000;31(suppl 3):C62–C63 [DOI] [PubMed] [Google Scholar]
- 3. Arneson TJ, Melton LJ III, Lewallen DG, O'Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res. 1988;(234):188–194 [PubMed] [Google Scholar]
- 4. Frigg R, Appenzeller A, Cristensen R, Frenk A, Gilbert S, Schavan R, The development of the distal femur less invasive stabilization system (LISS). Injury. 2001;32(suppl 3): SC24–SC31 [DOI] [PubMed] [Google Scholar]
- 5. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18(8):488–493 [DOI] [PubMed] [Google Scholar]
- 6. Tejwani NC, Wolinsky P. The changing face of orthopaedic trauma: locked plating and minimally invasive techniques. Instr Course Lect. 2008;57:3–9 [PubMed] [Google Scholar]
- 7. Weight M, Collinge C. Early results of the less invasive stabilization system for mechanically unstable fractures of the distal femur (AO/OTA types A2, A3, C2, and C3). J Orthop Trauma. 2004;18(8):503–508 [DOI] [PubMed] [Google Scholar]
- 8. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84(8):1093–1110 [DOI] [PubMed] [Google Scholar]
- 9. Claes L. Biomechanical principles and mechanobiologic aspects of flexible and locked plating. J Orthop Trauma. 2011;25(suppl 1):S4–S7 [DOI] [PubMed] [Google Scholar]
- 10. Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma. 2004;18(8):494–502 [DOI] [PubMed] [Google Scholar]
- 11. Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 2000;8(4):211–216 [DOI] [PubMed] [Google Scholar]
- 12. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13(6):401–406 [DOI] [PubMed] [Google Scholar]
- 13. Ehlinger M, Adam P, Di Marco A, Arlettaz Y, Moor BK, Bonnomet F. Periprosthetic femoral fractures treated by locked plating: feasibility assessment of the mini-invasive surgical option. A prospective series of 36 fractures. Orthop Traumatol Surg Res. 2011;97(6):622–628 [DOI] [PubMed] [Google Scholar]
- 14. Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality After Distal Femur Fractures in Elderly Patients. Clin Orthop Relat Res. 2011;469(4):1188–1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kammerlander C, Riedmüller P, Gosch M, et al. Functional outcome and mortality in geriatric distal femoral fractures. Injury. 2012;43(7):1096–1101 [DOI] [PubMed] [Google Scholar]
- 16. El-Zayat BF, Ruchholtz S, Efe T, et al. NCB-plating in the treatment of geriatric and periprosthetic femoral fractures. Orthop Traumatol Surg Res. 2012;98(7):765–772 [DOI] [PubMed] [Google Scholar]
- 17. Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop. 2005;29(2):117–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoffmeier KL, Hofmann GO, Mückley T. Choosing a proper working length can improve the lifespan of locked plates. a biomechanical study. Clin Biomech (Bristol, Avon). 2011;26(4):405–409 [DOI] [PubMed] [Google Scholar]
- 19. Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509–520 [DOI] [PubMed] [Google Scholar]
- 20. Abelseth G, Buckley RE, Pineo GE, Hull R, Rose MS. Incidence of deep-vein thrombosis in patients with fractures of the lower extremity distal to the hip. J Orthop Trauma. 1996;10(4):230–235 [DOI] [PubMed] [Google Scholar]
- 21. White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009;123(suppl 4):S11–S17 [DOI] [PubMed] [Google Scholar]
- 22. Kanchanabat B, Stapanavatr W, Meknavin S, Soorapanth C, Sumanasrethakul C, Kanchanasuttirak P. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98(10):1356–1364 [DOI] [PubMed] [Google Scholar]
- 23. Lu Y, Ma B, Guo R, et al. Deep vein thrombosis in trauma: a prospective study of lower limb orthopedic trauma patients in Tianjin Hospital, China. Int Angiol. 2007;26(2):165–170 [PubMed] [Google Scholar]
- 24. Sen RK, Tripathy SK, Singh AK. Is routine thromboprophylaxis justified among Indian patients sustaining major orthopedic trauma? a systematic review. Indian J Orthop. 2011;45(3):197–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery Patients. antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(suppl 2):e278S–e325S [DOI] [PMC free article] [PubMed] [Google Scholar]


