Summary
Chronic hepatitis C infection is associated with hypolipidaemia that resolves with viral clearance. Lipid levels in a subgroup of patients rebound to levels that may increase the risk of coronary heart disease. The impact of acute hepatitis C infection and its clearance on lipid levels is unknown. We undertook a retrospective evaluation of subjects with acute hepatitis C infection evaluating lipid levels before, during and following acute infection. Thirty-eight subjects with acute hepatitis C infection had lipid levels available. Twelve patients had pre-infection and intra-infection lipid levels available. Cholesterol (197.8–152.4 mg/dL, P = 0.025), low-density lipoprotein (LDL) (116.1–76.3 mg/dL, P = 0.001) and non-high-density lipoprotein (non-HDL) cholesterol (164.0–122.7 mg/dL, P = 0.007) decreased dramatically during acute hepatitis C virus infection. Nineteen patients who achieved viral clearance had lipid levels available during infection and following resolution of infection. In these patients, cholesterol (145.0–176.0 mg/dL, P = 0.01), LDL (87.0–110.1 P = 0.0046) and non-HDL cholesterol (108.6–133.6 mg/dL, P = 0.008) increased significantly. No change was seen in patients who developed chronic infection. Four patients had lipid levels before, during and following resolution of infections and had increased postinfection LDL, cholesterol and non-HDL cholesterol from pre-infection levels, indicating acute infection may be associated with an increase in postinfection lipid levels and may confer an increased risk of coronary heart disease. Acute hepatitis C infection results in hypolipidaemia with decreased LDL, cholesterol and non-HDL cholesterol levels that increase following infection resolution. Levels may increase above pre-infection baseline lipid levels and should be monitored.
Keywords: cholesterol, hepatitis C, low-density lipoprotein, non-HDL cholesterol
Replication of the hepatitis C virus (HCV) involves several important host lipid interactions. Hepatitis C virions complex with host lipoproteins to form lipoviroparticles in the host circulation [1]. Lipoviroparticles may then use low-density lipoprotein (LDL) receptors on hepatocytes as one mechanism of cell entry [2,3]. In addition, the HCV envelope glycoprotein E2 has been demonstrated in vitro to bind to lipoproteins and lead to enhanced LDL receptor and CD81 binding [4]. Once inside the hepatocyte, HCV replication requires geranylgeranylation of the host protein FBL2, a process dependent on the host cholesterol synthesis pathway [5]. Interruption of this pathway results in dissolution of the HCV replication complex [6]. Further, HCV secretion appears to be tied to host apolipoprotein B secretion [7,8].
Interaction between HCV and host lipids has been shown in clinical studies. Lower serum cholesterol and LDL levels are found in patients infected with hepatitis C when compared with patients with hepatitis B or without infection [9–11]. Recently, we demonstrated that chronic hepatitis C infection is associated with a decrease in cholesterol and LDL when compared with matched control subjects. We also found that this hypolipidaemia resolves with treatment-induced viral clearance, while patients without response to therapy remain hypolipidaemic [12]. Further, we demonstrated that in patients who achieve viral clearance, LDL and cholesterol often rebound to levels that may confer increased risk of cardiovascular disease and require treatment with lipid-lowering therapy.
To strengthen the association between HCV infection and alterations in serum lipids, we sought to evaluate the impact of acute HCV infection on serum lipid levels. Acute HCV infection is a unique form of hepatitis C infection that presents symptomatically, thus bringing patients to clinical attention and allowing approximation of the date of infection. The ability to determine the time point of infection allows for the evaluation of lipid levels prior to infection and comparison of these levels to levels during and following infection. We hypothesized that, similar to chronic hepatitis C infection, acute infection would result in a lowering of LDL and cholesterol levels from baseline levels and rebound in those who cleared the infection but not in those who went on to develop a chronic infection. Further, we hypothesized that clearance of HCV would be associated with a rebound in LDL and cholesterol above pre-infection levels. In addition, we hypothesized that non-high-density lipoprotein (non-HDL) cholesterol levels, derived by subtracting HDL cholesterol from total cholesterol levels and increasingly recognized as an important risk factor for coronary heart disease (CHD) [13], would decrease with acute infection and rebound with resolution of infection.
Methods
We performed a retrospective evaluation of patients who presented to the Massachusetts General Hospital with acute hepatitis C infection between 1999 and 2008. Nineteen patients were prospectively enrolled into a registry of patients with acute hepatitis C and had serum stored on which lipid panels were retroactively performed. The remaining patients had lipid panels measured as part of routine care by the same methodology and were available in the electronic medical record. Acute hepatitis C was defined by seroconversion to anti-hepatitis C antibody (anti-HCV) in the setting of acute hepatitis, negative antibody and positive HCV RNA or positive antibody in the setting of acute hepatitis, positive HCV RNA and elevated ALT with a history of recent HCV exposure. In addition, patients with a documented seroconversion of their antibody in the past 12 months with a positive HCV RNA in the absence of documented symptoms or elevated transaminases could be included. All subjects had fasting serum lipid panels available before and during their acute infection, during and following their acute infection or at all three time points.
The primary outcomes of interest were mean LDL, cholesterol, HDL, non-HDL cholesterol and triglyceride levels before, during and following acute infection in patients who achieved spontaneous clearance, treatment-induced clearance and those who developed chronic hepatitis C infection. Non-HDL cholesterol was calculated by subtracting HDL from total cholesterol levels.
Statistical analysis was performed using SAS software, version V.9.13 (SAS Institute, Cary, NC, USA). Continuous variables were analysed using a student's t-test or paired t-test, while categorical variables were analysed using a chi-square test. Multivariate modelling was performed to determine what effect pre-infection and intra-infection lipids had on hepatitis C outcome.
This study was approved by the Partners Human Research Committee.
Results
Baseline characteristics of patients with acute hepatitis C
Thirty-eight patients with acute hepatitis C infection met entry criteria and were included in this study. Fifty per cent were women with a mean age of 36.3 years. Subjects were predominantly Caucasian (76.3%), with 10.5% Hispanic and 7.9% African American. Genotype 1 predominated (68.4%) as did intravenous drug abuse as the identified risk factor for acquiring HCV (61.5%). (Table 1). There was no significant difference in mean age, genotype, risk factor or race between subjects who had treatment-induced or spontaneous clearance and those with chronic disease or non-response to therapy. In addition, no difference in any baseline variable was seen when the spontaneous clearers were compared to those with treatment-induced clearance, nonresponders or untreated patients who developed chronic disease.
Table 1. Baseline characteristics of the acute hepatitis C virus (HCV)-infected patients.
| Number of subjects | 38 |
|---|---|
| Gender (%) | |
| Women | 19 (50.0) |
| Men | 19 (50.0) |
| Mean age (SD) | 36.3 (13.2) |
| Race (%) | |
| White | 29 (76.3) |
| Hispanic | 4 (10.5) |
| Black | 3 (7.9) |
| Other | 2 (5.3) |
| Mode of transmission (%) | |
| Intravenous drug use | 24 (61.5) |
| Sexual | 6 (15.4) |
| Unknown | 4 (10.6) |
| Other | 5 (12.8) |
| Genotype (%) | |
| 1 (%) | 26 (68.4) |
| 2 (%) | 1 (2.6) |
| 3 (%) | 5 (10.6) |
| Unknown (%) | 4 (10.4) |
| HCV RNA (SD) | 934 887 (1 786 543) |
Twelve patients had lipid panels available before and during their acute infection. Of these patients, eight had lipid levels also available either following infection resolution (n = 4) or after the development of chronic infection (n = 4). In addition, there were 15 unique patients who had spontaneous clearance or treatment-induced clearance and had lipid panels during and after infection. Twelve patients who did not clear virus (either untreated or failed treatment) had lipids available during infection and after the development of chronic infection (defined as 6 months or more after the diagnosis of infection).
Acute hepatitis C results in decreased LDL and cholesterol from baseline
Twelve patients had lipid panels available for evaluation prior to the diagnosis of acute hepatitis C infection (Table 2). Lipid panels were drawn a mean of 2.6 years before acute infection. Eleven patients had LDL values available before and during infection and all 11 experienced a decline in LDL. The mean pre-infection LDL was 116.1 mg/dL, which fell to 76.3 mg/dL with the development of acute hepatitis C infection (P = 0.001). Eleven patients had cholesterol levels before and during their acute infection, and 10 of 11 experienced a decline in cholesterol from a mean pre-infection level of 197.8–152.4 mg/dL (P = 0.025).
Table 2. Lipid levels before and during acute hepatitis C infection (Group 1, n = 12).
| |||
|---|---|---|---|
|
| |||
| Lipids levels | Prior to acute infection | During infection | P value |
| Cholesterol (SD) | 197.8 (45.2) | 152.4 (42.9) | 0.025 |
| LDL (SD) | 116.1 (33.6) | 76.3 (32.1) | 0.001 |
| Triglycerides (SD) | 98.9 (62.9) | 114.5 (49.2) | 0.54 |
| HDL (SD) | 46.5 (11.3) | 36.3 (22.1) | 0.26 |
| Non-HDL Cholesterol (SD) | 164.0 (49.0) | 122.7 (28.3) | 0.007 |
Note: 10 of 11 had decline in cholesterol (one did not have cholesterol reported). Eleven of 11 had decline in LDL (one did not have LDL reported).
In addition, we evaluated mean levels of non-HDL cholesterol. We found non-HDL levels significantly declined from pre-infection levels, mean 164.0–122.7 mg/dL during acute infection (P = 0.007). No significant change was seen in triglyceride or HDL levels.
LDL and cholesterol levels rebound with viral clearance
Thirty-five patients had lipid panels performed during their infection and either following resolution of their infection (spontaneous, n = 7 or treatment induced, n = 12) or after the development of chronic infection. Nineteen patients achieved either spontaneous or treatment-induced viral clearance and had lipid panels available during a mean of 1.6 years following diagnosis of their infection. (Table 3). Seventeen of these patients experienced an increase in their cholesterol level following infection compared to their cholesterol levels during infection (145.0 vs 176.4 mg/dL, P = 0.01). In addition, 17 patients had an increase in LDL levels from 87.0 mg/dL during infection to 110.1 mg/dL following clearance of viraemia (P = 0.0046). Non-HDL cholesterol levels also increased significantly from intra-infection levels of 108.3–133.6 mg/dL following resolution of infection (P = 0.008). No change in mean HDL or triglyceride levels was seen.
Table 3. Lipid levels during and following acute hepatitis C infection.
| ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Spontaneous and treatment induced clearance (n = 19) | Chronic infection/nonresponders (n = 16) | |||||
|
|
|
|||||
| During infection | Postacute infection | P value | During infection | Postacute infection | P value | |
| Cholesterol (SD) | 145.0 (40.0) | 176.4 (50.8) | 0.01 | 163.0 (33.0) | 155.3 (31.7) | 0.50 |
| LDL (SD) | 87.0 (30.7) | 110.1 (41.5) | 0.0046 | 84.9 (33.1) | 87.7 (26.8) | 0.8 |
| Triglycerides (SD) | 133.5 (59.9) | 161.2 (78.2) | 0.23 | 108.7 (46.2) | 97.6 (41.4) | 0.50 |
| HDL (SD) | 38.1 (9.7) | 42.4 (18.6) | 0.19 | 48.8 (15.1) | 42.4 (13.2) | 0.23 |
| Non-HDL Cholesterol (SD) | 108.6 (27.7) | 133.6 (48.1) | 0.008 | 114.7 (29.9) | 112.9 (30.7) | 0.88 |
Sixteen patients developed chronic hepatitis C infection either following failed treatment (n = 4) or did not receive treatment (n = 12). These patients had lipid levels a mean of 2.6 years following the diagnosis of their infection. These patients experienced no change during and postinfection in cholesterol (163.0 vs 155.3 mg/dL, P = 0.5), LDL (84.9 vs 87.8 mg/dL, P = 0.85) or non-HDL cholesterol levels (114.7 vs 112.9 mg/dL, P = 0.88). In addition, as in those who achieved viral clearance, no changes in mean HDL or triglyceride levels were noted.
LDL and cholesterol levels increase from pre-infection levels
Eight patients had lipid levels before, during and following acute infection; four patients who achieved viral clearance and four who developed chronic infection and allow for direct evaluation of postviral clearance rebound hyperlipidaemia. The four patients who achieved viral clearance all experienced a decline in LDL, cholesterol and non-HDL cholesterol during acute infection. All patients experienced a rebound in lipid levels following resolution of infection with three patients experiencing a rebound to levels above pre-infection lipid levels. The four patients who went on to develop chronic infection had sustained decreases in their lipid levels (Figs 1–3).
Fig. 1.
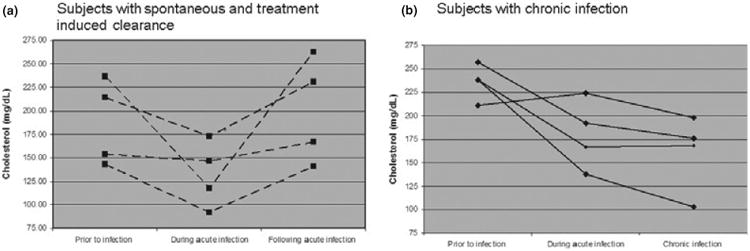
Cholesterol levels before, during and following acute infection.
Fig. 3.
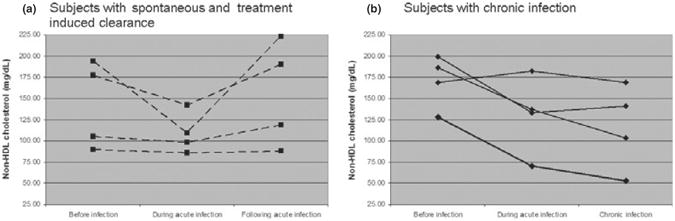
Non-HDL cholesterol levels before, during and following acute infection.
Predictors of viral clearance
Neither pre-infection nor intra-infection levels of cholesterol, triglyceride, HDL or LDL were found to be predictors of spontaneous or treatment-induced viral clearance. There was a trend of lower pre-infection LDL levels in patients achieving clearance with pre-infection LDL level of 107.1 mg/dL compared to 140.0 mg/dL in those who went on to develop chronic infection (P = 0.16).
Discussion
This study further strengthens the association between HCV infection and decreased LDL and cholesterol by demonstrating that the hepatitis C viraemia results in a profound decrease in LDL and cholesterol levels from pre-infection levels, which rebound once clearance occurs but which persist in chronic infection. In addition, our study is the first to examine the dynamic effects of acute HCV infection on non-HDL cholesterol, a strong predictor of CHD. Our study is unique in demonstrating that acute hepatitis C infection is associated with hypolipidaemia that resolves with viral clearance but persists with chronic infection. In addition, our study is the first to compare pre-infection levels of cholesterol, LDL and non-HDL cholesterol levels with intra-and postinfectious levels, providing strong evidence that HCV infection itself is the direct cause of hypolipidaemia in these patients.
Our findings are consistent with our previous study of lipid levels in chronic hepatitis C as well as other published cohorts that have demonstrated that hepatitis C is uniquely associated with decreased LDL and cholesterol [9,10,12,14]. As we have previously suggested, we posit that this may be driven by the virus interference with the mevalonate pathway leading to decreased cholesterol production and compensatory upregulation of LDL receptors leading to decreased LDL levels, akin to the mechanism of HMG-CoA reductase inhibitors. In addition, hepatitis C has been associated with reduced levels of microsomal triglyceride transferase protein (MTTP), the enzyme responsible for the production of VLDL whose inhibition results in decreased circulating LDL and cholesterol levels [15]. Thus, the decrease in non-HDL cholesterol levels, a composite of principally VLDL and LDL, could reflect viral inhibition of MTTP. Evaluation of hepatitis C infection on directly measured VLDL levels will be helpful in clarifying this possibility.
We demonstrated that LDL, cholesterol and non-HDL cholesterol levels increase from pre-infection levels following viral clearance. Patients with lipid panels available before, during and following infection demonstrated a 10.7 mg/dL increase in LDL and a 13.7 mg/dL increase in total cholesterol levels. LDL and total cholesterol levels are associated with a continuous, graded increase in the risk of cardiovascular disease [16]. A 10-point increase in LDL is clinically significant as it is associated with a 12% increased risk of cardiovascular disease [17]. Similarly, a cholesterol increase from 186.75–200.5 mg/dL confers a >40% increased risk of cardiovascular disease [16]. Non-HDL cholesterol is strongly associated with an increased risk of CHD. A recent metaanalysis demonstrated that a 1% decrease in non-HDL cholesterol levels is associated with a 1% decrease in CHD risk over 4.5 years. The patients in this study experienced a 25% decrease in non-HDL cholesterol levels with acute infection, which in persistent infection would be associated with a 25% decrease in the risk of developing CHD. Likewise, our patients who achieved viral clearance and had lipid values available before, during and following resolution had a 9.5% increase in non-HDL cholesterol from pre-infection levels. If these increases are sustained, this would infer a nearly 10% increase risk of CHD over 4.5 years. Currently, our group is evaluating the incidence of cardiovascular disease in patients with chronic hepatitis C who achieve treatment-induced sustained virologic response compared with those who failed to respond to therapy to evaluate the long-term implications of virally mediated alterations in lipid levels and to determine whether viral clearance is associated with increased risk of CHD.
Our finding of lower pre-infection LDL levels in patients who achieve viral clearance is worthy of further evaluation. Hepatitis C has been noted to complex with LDL in the circulation and use LDL receptors as one form of cell entry. In addition, therapy with HMG-CoA reductase inhibitors has been associated with increased rates of sustained virologic response in patients undergoing hepatitis C therapy [18,19]. Our study was limited by a small number of patients with pretreatment levels available and thus did not reach statistical significance. However, further evaluation is warranted to determine whether pretreatment LDL levels can be used as predictors of spontaneous or treatment-induced viral clearance in patients with acute infection or whether pretreatment lipid-lowering therapy could serve as an adjunct to antiviral therapy.
The small numbers of patients with hepatitis C who present acutely limit our study. Only four subjects who achieved viral clearance had lipid levels documented at all time points: before, during and after infection. However, these patients amply illustrate the phenomenon of viral-induced hypolipidaemia and reinforce the findings in the entire cohort that demonstrate a decrease in mean LDL and cholesterol during infection and resolution following viral clearance. These four subjects also suggest the possibility of rebound hyperlipidaemia above pretreatment levels. Long-term follow-up of these subjects will be important to assess whether the hyperlipidaemia is lasting.
In conclusion, this study adds to accumulating evidence that hepatitis C infection results in reduced LDL and cholesterol levels that rebound following the resolution of infection. Further study is needed to determine whether pre-infection lipid levels are predictive of viral clearance and can be used to guide management. In addition, the impact of viral infection and clearance on long-term cardiovascular outcomes is necessary and underway.
Fig. 2.
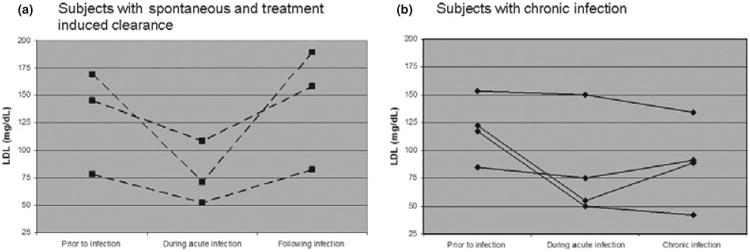
LDL levels before, during and following acute infection. Note: One patient did not have an LDL included as part of their lipid panel.
Acknowledgments
This study was funded in part by a grant from the NIDDK 1F32DK083252-01 (Corey).
Abbreviations
- CHD
coronary heart disease
- HCV
hepatitis C virus
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- SVR
sustained virologic response
Footnotes
Disclosure: The authors have no personal interests to disclose.
References
- 1.Andre P, Komurian-Pradel F, Deforges S, et al. Characterization of low-and very-low-density hepatitis C virus RNA-containing particles. J Virol. 2002;76(14):6919–6928. doi: 10.1128/JVI.76.14.6919-6928.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agnello V, Abel G, Elfahal M, Knight GB, Zhang QX. Hepatitis C virus and other flaviviridae viruses enter cells via low density lipoprotein receptor. Proc Natl Acad Sci U S A. 1999;96(22):12766–12771. doi: 10.1073/pnas.96.22.12766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acuna-Alonzo V, Flores-Dorantes T, Kruit JK, et al. A functional ABCA1 gene variant is associated with low HDL-cholesterol levels and shows evidence of positive selection in Native Americans. Hum Mol Genet. May 11; doi: 10.1093/hmg/ddq173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wunschmann S, Muller HM, Stipp CS, Hemler ME, Stapleton JT. In vitro interaction between hepatitis C virus (HCV) envelope glycoprotein E2 and serum lipoproteins (LPs) results in enhanced cellular binding of both HCV E2 and LPs. J Infect Dis. 2006;194(8):1058–1067. doi: 10.1086/507647. [DOI] [PubMed] [Google Scholar]
- 5.Wang C, Gale M, Jr, Keller BC, et al. Identification of FBL2 as a geranyl-geranylated cellular protein required for hepatitis C virus RNA replication. Mol Cell. 2005;18(4):425–434. doi: 10.1016/j.molcel.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Guthery SL, Pohl JF, Bucuvalas JC, et al. Bone mineral density in long-term survivors following pediatric liver transplantation. Liver Transpl. 2003;9(4):365–370. doi: 10.1053/jlts.2003.50071. [DOI] [PubMed] [Google Scholar]
- 7.Nahmias Y, Goldwasser J, Casali M, et al. Apolipoprotein B-dependent hepatitis C virus secretion is inhibited by the grapefruit flavonoid naringenin. Hepatology. 2008;47(5):1437–1445. doi: 10.1002/hep.22197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diaz O, Delers F, Maynard M, et al. Preferential association of hepatitis C virus with apolipoprotein B48-containing lipoproteins. J Gen Virol. 2006;87(Pt 10):2983–2991. doi: 10.1099/vir.0.82033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabris C, Federico E, Soardo G, Falleti E, Pirisi M. Blood lipids of patients with chronic hepatitis: differences related to viral etiology. Clin Chim Acta. 1997;261(2):159–165. doi: 10.1016/s0009-8981(97)06532-7. [DOI] [PubMed] [Google Scholar]
- 10.Marzouk D, Sass J, Bakr I, et al. Metabolic and cardiovascular risk profiles and hepatitis C virus infection in rural Egypt. Gut. 2007;56(8):1105–1110. doi: 10.1136/gut.2006.091983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Floris-Moore M, Howard AA, Lo Y, Schoenbaum EE, Arnsten JH, Klein RS. Hepatitis C infection is associated with lower lipids and high-sensitivity C-reactive protein in HIV-infected men. AIDS Patient Care STDS. 2007;21(7):479–491. doi: 10.1089/apc.2006.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corey KE, Kane E, Munroe C, Barlow LL, Zheng H, Chung RT. Hepatitis C virus infection and its clearance alter circulating lipids: implications for long-term follow-up. Hepatology. 2009;50(4):1030–1037. doi: 10.1002/hep.23219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arsenault BJ, Rana JS, Stroes ES, et al. Beyond low-density lipoprotein cholesterol: respective contributions of non-high-density lipoprotein cholesterol levels, triglycerides, and the total cholesterol/high-density lipoprotein cholesterol ratio to coronary heart disease risk in apparently healthy men and women. J Am Coll Cardiol. 2009;55(1):35–41. doi: 10.1016/j.jacc.2009.07.057. [DOI] [PubMed] [Google Scholar]
- 14.Dai CY, Chuang WL, Ho CK, et al. Associations between hepatitis C viremia and low serum triglyceride and cholesterol levels: a community-based study. J Hepatol. 2008;49(1):9–16. doi: 10.1016/j.jhep.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Mirandola S, Realdon S, Iqbal J, et al. Liver microsomal triglyceride transfer protein is involved in hepatitis C liver steatosis. Gastroenterology. 2006;130(6):1661–1669. doi: 10.1053/j.gastro.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 16.Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT) JAMA. 1986;256(20):2823–2828. [PubMed] [Google Scholar]
- 17.Howard BV, Robbins DC, Sievers ML, et al. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: the Strong Heart Study. Arterioscler Thromb Vasc Biol. 2000;20(3):830–835. doi: 10.1161/01.atv.20.3.830. [DOI] [PubMed] [Google Scholar]
- 18.Bader T, Xxxxx M, Rizvi S. Retrospective analysis of the effect of taking a statin along with peginterferon and ribavirin (PI+R) on SVR. Gastroenterology. 2007;132(4):A–788. [Google Scholar]
- 19.Bader T, Xxxxx MM, Rizvi A, Seres K, Fazili J. Statins improve ALT values in chronic hepatitis C patients with abnormal values. Gastroenterology. 2007;4:A–775. [Google Scholar]


