Abstract
Objective
To examine the course of health risk behaviors (HRBs) during a 3-year period after a parent’s death in bereaved youth compared with nonbereaved youth (control subjects).
Design
A longitudinal population-based study.
Setting
Bereaved families were recruited through coroner records and by advertisement. Control families were recruited using random-digit dialing and by advertisement.
Participants
Two hundred forty parentally bereaved offspring were compared with 183 nonbereaved control offspring.
Main Exposure
Sudden parental death due to accident, suicide, or sudden disease-related (natural) death.
Main Outcome Measures
The sum of the total number of HRBs at a clinically significant frequency threshold assessed 9, 21, and 33 months after the parent’s death.
Results
The bereaved group showed a higher number of HRBs over time compared with the nonbereaved group (univariate effect sizes, 0.22–0.52; P<.04), even after taking into account correlates of bereavement and of HRBs, such as youth aggression, as well as antisocial and anxiety disorders of the deceased parent.
Conclusions
Parental bereavement is associated with higher HRBs in youth over time, even after controlling for other covariates associated with bereavement and HRBs. Clinicians should be aware that bereaved youth may be vulnerable to HRBs. Further work is warranted on interventions to attenuate the negative effect of bereavement on HRBs.
Loss of a parent is one of the most stressful events that a child can experience. Cross-sectional and longitudinal studies1–4 have shown an increased risk in depression, posttraumatic stress disorder (PTSD), alcohol and substance use, and behavioral problems in parentally bereaved children. Although the negative effect of family adversity on health and health risk behaviors (HRBs) is increasingly well documented,5–7 less is known about the specific effect of parental bereavement on HRBs. Because HRBs, such as risky sexual behavior, physical inactivity, weapon carrying, fighting, and not wearing seat belts, make a significant contribution to the mortality and morbidity of young people, this aspect of the potential effect of parental bereavement on their children has important public health implications.
In a previous report8 on parental bereavement, no significant increase in the rates of individual HRBs 9 months after the death was observed, although there were nonsignificant trends toward higher rates of not wearing seat belts and of fighting in parentally bereaved youth. There are reasons to expect that parentally bereaved youth might be at increased risk for the development of these behaviors. As noted, family and social adversity are associated with HRBs.7,9–11 In addition, bereavement may leave the surviving caregiver impaired and less able to supervise the bereaved child.1,12,13 The increased risk in child psychiatric diagnoses, specifically depression and PTSD, is also associated with HRBs. Exposure to traumatic death and, specifically, exposure to suicide may lead to an increase in HRBs.14 Finally, youth who are parentally bereaved often come from families at high psychosocial risk due to several familial and personal psychopathologic factors, discord, divorce, and other family adversities that antedate the parental death all of which might increase the risk for HRBs.1,15–17
In light of the increase in psychopathologic characteristics in youth after loss of a parent and the association between those characteristics, family adversity, and HRBs,18–21 one might expect that parental bereavement would be associated with a higher risk of undesirable health behaviors over time. Weextended the initial crosssectional study8 of HRBs in parentally bereaved youth to examine the course of HRBs during the 3-year period after the parent’s death compared with behaviors in nonbereaved youth (controls). We hypothesized that bereaved youth would show more HRBs over time compared with nonbereaved youth. We also hypothesized that the deceased parent’s psychiatric disorder, if present, in addition to the child’s psychopathologic characteristics and coping as well as the caregiver’s functioning, would affect bereaved youths’ HRBs.
METHODS
SAMPLE
The sample included 154 bereaved and 99 nonbereaved families. The bereaved families consisted of 240 offspring who lost a parent resulting from accidental death (n=57), sudden diseaserelated (natural) death (n=100), or suicide (n=83) and 149 adult caregivers, with 183 youths and 99 adult caregivers included in the nonbereaved group. Five bereaved families did not have an adult caregiver because the offspring in those families were 18 years or older and were living independently at the time of the death (n=3), the parent who died was single (n=1), or the surviving parent was estranged from the family (n=1). Deceased probands were between the ages of 30 and 60 years, had biological offspring between the ages of 7 and 25 years, and died within 24 hours after suicide, accidental death, or sudden natural death. Families in which there were multiple deaths or injuries were excluded. The most common causes of accidental and sudden natural death were motor vehicle crash and myocardial infarction. In the bereaved families, the caretaking parent was almost always female (82.8%) and the biological parent of the child (91.3%). The nonbereaved offspring had 2 living biological parents, lived in the home of at least one of them, and had no first-degree relatives who had died within the previous 2 years. During the follow-up in this study, 4 offspring from 2 control families experienced the loss of a parent and so were excluded from the analyses in this follow-up report. Table 1 summarizes the demographic, clinical, and psychological characteristics of the bereaved and nonbereaved groups; differences between the groups were similar to those in previous reports.1
Table 1.
Baseline Demographic, Clinical and Psychological Characteristics by Bereavement status§
| Offspring | Bereaved 240 | Control 183 | |||
|---|---|---|---|---|---|
| Antecedent | Test | df | P | ||
| Gender, N (% female) | 118 (49.2) | 92 (50.3) | χ2=0.05 | 1 | .82 |
| Age, (M± SD) | 13.6±3.7 | 12.9±3.2 | t=2.03 | 416.08 | .04 |
| Race, N (Caucasian %) | 190 (79.2) | 155 (84.7) | χ2 =2.11 | 1 | .15 |
| Socio-economic status, | 35.6±8.3 | 37.8±7.3 | t=−1.67 | 160 | .10 |
| Previous history of | 26 (10.9) | 1 (0.6) | χ2 | 1 | <.001 |
| Characteristics | |||||
| Depression, N (%) | 52(23.1) | 11(6.0) | χ2 | 1 | <.001 |
| PTSD, N (%) | 22 (9.3) | 0 (0.0) | FET | - | <.001 |
| Functional Impairment | 75.9 ±12.1 | 82.5±10.0 | t=−6.10 | 417.58 | <.001 |
| Self-reported | |||||
| Depression** | 0.4 ±1.1 | −0.1±0.9 | t=4.70 | 386.76 | <.001 |
| Anxiety** | 0.3±1.1 | 0.04±0.9 | t=2.22 | 390.09 | .03 |
| PTSD | 5.8±7.5 | 1.1±3.2 | t=6.91 | 249.80 | <.001 |
| Suicidal Ideation | 23.0±12.0 | 19.8±9.6 | t=2.90 | 383.83 | .004 |
| Health Risk Behaviors** | 0.2±1.1 | −0.03±0.9 | t=2.03 | 345.75 | .04 |
| Psychological | |||||
| Self Esteem | 13.8±5.8 | 12.6±5.2 | t=2.29 | 389.80 | .02 |
| Aggression | 72.1±23.3 | 66.2±20.1 | t=2.65 | 389 | .008 |
| Social Support** | −0.2 ±1.0 | 0.1± 0.9 | t=−2.83 | 388 | .005 |
| Physical or Sexual | 21 (8.8) | 3 (1.6) | χ2 =9.87 | 1 | .002 |
| Adult Caregiver | 149 (59.6) | 101 (40.4) | |||
| Previous History of | 70 (47.0) | 33 (33.0) | χ2 =4.82 | 1 | .03 |
| Previous History of | 49 (32.9) | 15 (14.9) | χ2 | 1 | .001 |
| New Onset Diagnosis* | |||||
| New Onset Depression, | 53 (39.6) | 9 (10.3) | χ2 | 1 | <.001 |
| New Onset PTSD, N (%) | 38 (26.0) | 2 (2.3) | χ2 | 1 | <.001 |
| Functional impairment | 73.8 ±12.5 | 82.0±9.2 | t=−5.76 | 220.95 | .001 |
| Depression | 66 (43.1) | 32 (33.0) | χ2 =2.56 | 1 | .11 |
| Bipolar Disorder | 20 (13.0) | 3 (3.0) | χ2 =7.23 | 1 | .007 |
| Alcohol or Substance | 95 (62.1) | 42 (42.4) | χ2 =9.37 | 1 | .002 |
| Any Axis II Disorder | 27 (17.5) | 3 (3.0) | χ2=12.13 | 1 | <.001 |
Only significant results included.
New onset since the death
Standardized scores
RECRUITMENT
Bereaved families were recruited through coroner’s records (49.7%) and by newspaper advertisement (50.3%). Details on recruitment procedures were described previously.8
The demographic characteristics of probands who died of suicide and accidents were similar to those of all people who died of suicide and accidents in AlleghenyCounty (metropolitan Pittsburgh, Pennsylvania), and there were no significant demographic differences as a function of method of recruitment. The rate of participation for eligible bereaved families was 71.0%. Control families were recruited using random-digit dialing and by advertisement. Of those who were eligible, 55.0% agreed to participate. This study was approved by the University of Pittsburgh Institutional Review Board. After a complete description of the study, caregivers’ consent was obtained for their participation, as well as the assent or consent of their offspring.
ASSESMENT
Participants were interviewed on 3 occasions—9, 21, and 33 months after the death—with parallel timing for the nonbereaved controls. Retention for the study was 89.5% and 73.9% for 21 and 33 months, respectively. Participants lost to follow-up were more likely to be bereaved compared with those retained (74.4% vs 25.6%; X12=6.1; P=.002). Within the bereaved group, the highest rate of attrition was within the sudden natural death group (25.0%); the difference with the other types of death was not statistically significant. In addition, the caregivers of families lost to follow-up were more functionally impaired, as assessed by the Global Assessment Scale29 (mean [SD] score, 69.8 [13.9] vs 77.7 [11.4]; t392=3.4; P<.001), and had a lower socioeconomic status shown on the Hollingshead Scale27 (30.5 [8.8] vs 36.8 [8.1]; t262= −3.04; P=.03). There were no significant differences associated with attrition in other demographic, psychiatric, or psychological characteristics.
The Youth Risk Behavior (YRB) questionnaire is an adaptation of the Youth Risk Behavior Survey,31 which inquires about HRBs that contribute to unintentional injury, violence, and risky sexual behavior that the Centers for Disease Control and Prevention has prioritized for surveillance. The HRBs assessed in this study were not wearing a seat belt, being in a vehicle during the past 30 days with a driver who has been drinking alcohol, carrying a weapon, and being in a physical fight during the past 12 months. The child version for those aged 8 to 12 years includes 14 questions assessing safety and physical violence; the adolescent/adult version for those 13 years or older includes 6 additional questions related to sexual risk behaviors. Both versions include qualitative and quantitative items ranging from never (1)to always (5)or from zero times (1) to 12 or more times (8). Responses were dichotomized as sometimesor higher for the qualitative items and 1 or more times for the quantitative items. The total scores were computed as a count of endorsed questions and were standardized to combine the child and adolescent/young adult versions. The Cronbach α value, a measure of the internal consistency of this questionnaire, was 0.97 for the child version and 0.84 for the adolescent/adult version. A previous report8 on HRBs 9 months after the parent’s death reported the rates of individual HRBs. Because we are examining the change in the YRB scores over time in the present study and because of the YRB’s high internal consistency, we summed the number of different HRBs and treated the YRB as a continuous measure. We compared the scores on the YRB if we changed the cutoff point from 1 to 2 and found that the revised scores were highly correlated with YRB scores using the original8 cutoff point both in the child (r=0.92;P<.001) and adolescent/adult (r=0.98; P<.001) versions. We conducted analyses separately on the 2 age groups, and, since the results were consistent, we standardized the measure and present pooled findings, controlling for age.
The Schedule for Affective Disorders and Schizophrenia for School Age Children–Present and Lifetime Version32 was used to assess children younger than 18 years, and the structured interview for Diagnostic and Statistic Manual of Mental Disorders (Fourth Edition) (DSM-IV) Axis I disorders was used for assessment of adult offspring and caregivers.33 Psychiatric assessment of the proband was conducted using a psychological autopsy procedure.34 Functional status was determined using the Children’s Global Assessment Scale28 or the Global Assessment Scale for adults.29 In both of these scales, a lower score is associated with a higher level of impairment.
A battery of self-reported instruments was administered to assess the severity of symptoms, social support, coping, and history of family adversity. Self-reported depression, anxiety, and suicidal ideation were assessed in children younger than 18 years using the Mood and Feelings Questionnaire,35 the Screen for Child Anxiety Related Emotional Disorders,36 and the Suicide Ideation Questionnaire–Jr.37 For adult offspring, depression and anxiety inventories by Beck et al 38,39 and the Adult Suicidal Ideation Questionnaire40 were used. The severity of DSM-IV PTSD symptoms was assessed using the Child PTSD Symptom Scale41 interview for children and the parallel PTSD Symptom Scale42 interview for adults.
Intercurrent life events were assessed using the Life Events Checklist in children younger than 18 years43 and the Social Readjustment Rating Scale44 in offspring 18 years or older. Social support and coping style were evaluated using the Survey of Children’s Social Support45 and the Kidcope,46 respectively, in children younger than 18 years. The Multidimensional Scale of Perceived Social Support30 and the Ways of Coping Questionnaire47 were used in adult offspring. The Abuse Dimensions Inventory48 was used to obtain information on abuse history, including physical and sexual abuse. When different measures were used for offspring who were younger or older than 18 years, scores from these measures were standardized.
DATA ANALYSIS
We compared demographic, clinical, and psychological characteristics 9 months after the parent’s death (referred to as base-line) between the bereaved and nonbereaved groups using standard unpaired, 2-tailed, univariate statistics (eg, X2 and t tests). The α value was set at .05.
We then examined whether there was a differential change in HRBs over time between bereaved and nonbereaved participants by using mixed-effects regression models with HRBs as the outcome and with the main effects of bereavement, time, and a bereavement, time interaction. Similarly, we examined the relationship of demographic characteristics, antecedent characteristics to the death (referred to as antecedent), and other correlates assessed at baseline and YRB by using mixed-effects regression models with the main effects of correlates, time, and Correlates X time interaction.
We next examined the relationship of correlates assessed longitudinally at 21 and 33 months after the death (referred to as longitudinal), thus varying over time and HRBs. Time was included as a random effect. The time of baseline and follow-up assessments in relation to the time of death varied by participants and, as such, a logarithmic transformation was used. We also included proband (ie, family) as a random effect to take into account the correlation between siblings. A mixed-effects regression model was fitted with amain effect of bereavement, age, race, and sex, as well as with antecedent, baseline, and longitudinal correlates that were significantly associated with HRBs either as a main effect or as an interaction with time.
RESULTS
HRBs AND BEREAVEMENT
At baseline and at each of the subsequent time points, the bereaved youth showed a higher number of HRBs compared with nonbereaved youth. The standardized differences in the number of HRBs in the bereaved group at baseline and the 2 subsequent evaluation time points were 0.22 (SE, 0.11; t345.7=2.03; P=.04), 0.25 (SE, 0.12; t273.0=2.17; P=.03), and 0.52 (SE, 0.13; t164.9=4.13; P<.001). We examined changes in HRBs and the effect of bereavement on the changes in HRBs using a mixedeffects regression model, with HRBs as the outcome with bereavement and time as main effects, and bereavement × time interaction. We found a decrease in HRBs over time (β= −0.14; z= −2.50; P=−.001), but no significant bereavement (β= −0.001; z= 0.005; P>.99) or bereavement × time interaction (β=0.11; z=1.40; P=.16) was observed. Looking at individual HRBs, 2 different HRBs showed a pattern of persistent elevation in the bereaved group compared with the controls: the main effects of not wearing a seat belt when riding in a car driven by someone else (β= −0.56; z= −2.71; P=.007) and of physical fights during the past year (β=0.48; z=2.13; P=.03). At baseline, 12.4% of the bereaved youth did not wear a seat belt at least sometimes compared with 4.8% of the nonbereaved youth (X12=6.30; P=.01). Similarly, 28.1% of bereaved youth fought at least sometimes compared with 19.2% of the nonbereaved youth (X12=3.87; P=.049).
Within the bereaved group, we compared the HRBs over time among the 3 types of death and found no effect of time (P=.96), type of death (P=.40), or their interaction (P=.41).
ANTECEDENT AND BASELINE CORRELATES OF HRBs
We then examined the baseline correlates associated with changes in HRBs over time. We conducted mixed effects regression models for HRBs with a main effect of correlate (1 model for each correlate), time, and a correlate time interaction (Table 2). Interactions with time were found with proband bipolar disorder (β= −0.52; z= −2.94; P=.003), offspring aggression (β= −0.005; z= −2.61; P=.009), and offspring frequency of use of less adaptive coping methods (β= −0.10; z= −2.17; P=.03). Specifically, HRBs showed a slower decline among offspring of bipolar probands, as well as in offspring with higher aggression and less-adaptive coping scores.
Table 2.
Antecedent*** and Baseline*** and Longitudinal*** Correlates’ Main Effects and Interactions with Time on HRBs*
| β | Time | P | β | Covariate | P | β | Covariate by Time | P | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SE | Z | SE | Z | SE | Z | |||||||
| Offspring | ||||||||||||
| Antecedent Characteristics | ||||||||||||
| Gender (Male) | −0.10 | 0.06 | −1.74 | 0.08 | −0.40 | 0.23 | −1.77 | 0.08 | 0.04 | 0.08 | 0.46 | 0.65 |
| Age | 0.13 | 0.19 | 0.67 | 0.50 | 0.07 | 0.04 | 1.74 | 0.08 | −0.02 | 0.02 | −1.08 | 0.28 |
| Race (Caucasian) | −0.09 | 0.10 | −0.86 | 0.39 | −0.55 | 0.31 | −1.77 | 0.08 | 0.01 | 0.11 | 0.09 | 0.93 |
| Previous History of Behavioral | −0.06 | 0.04 | −1.56 | 0.12 | 1.71 | 0.60 | 2.84 | 0.005 | −0.41 | 0.23 | −1.76 | 0.08 |
| Characteristics Following the Death | ||||||||||||
| Bereavement | −0.14 | 0.06 | −2.50 | 0.01 | 0.00 | 0.24 | 0.00 | >0.99 | 0.11 | 0.08 | 1.40 | 0.16 |
| Functional Impairment | −0.40 | 0.29 | −1.37 | 0.17 | −0.03 | 0.01 | −2.78 | 0.005 | 0.00 | 0.00 | 1.11 | 0.27 |
| Self-Reported Symptoms | ||||||||||||
| Depression | −0.08 | 0.04 | −1.85 | 0.07 | 0.26 | 0.11 | 2.34 | 0.02 | −0.06 | 0.04 | −1.52 | 0.13 |
| Suicidal ideation | 0.03 | 0.09 | 0.33 | 0.74 | 0.02 | 0.01 | 2.29 | 0.02 | −0.01 | 0.00 | −1.46 | 0.14 |
| Hopelessness | −0.08 | 0.04 | −1.86 | 0.06 | 0.22 | 0.11 | 2.05 | 0.04 | −0.05 | 0.04 | −1.42 | 0.16 |
| Aggression | 0.26 | 0.13 | 1.97 | 0.05 | 0.03 | 0.00 | 5.25 | <0.001 | −0.01 | 0.002 | −2.61 | 0.00 |
| Social support | −0.07 | 0.04 | −1.62 | 0.11 | −0.26 | 0.11 | −2.27 | 0.02 | 0.03 | 0.04 | 0.62 | 0.53 |
| Negative coping | −0.07 | 0.04 | −1.53 | 0.13 | 0.33 | 0.13 | 2.60 | 0.009 | −0.10 | 0.05 | −2.17 | 0.03 |
| Adult Caregiver | ||||||||||||
| New Onset PTSD | −0.09 | 0.04 | −1.95 | 0.05 | 0.70 | 0.35 | 2.01 | 0.04 | −0.01 | 0.12 | −0.09 | 0.93 |
| Offspring, Longitudinal | ||||||||||||
| Functional Impairment | −0.76 | 0.19 | −4.08 | <0.00 | −0.03 | 0.01 | −3.83 | <0.001 | 0.01 | 0.00 | 3.76 | <0.00 |
| Aggression | 0.03 | 0.13 | 0.27 | 0.79 | 0.02 | 0.00 | 3.88 | <0.001 | 0.00 | 0.00 | −0.74 | 0.46 |
| Adult Caregiver, Longitudinal | ||||||||||||
| Functional Impairment | −0.42 | 0.29 | −1.47 | 0.14 | −0.03 | 0.01 | −2.82 | 0.005 | 0.00 | 0.00 | 1.17 | 0.24 |
| Proband Psychiatric History | ||||||||||||
| Anxiety | −0.04 | 0.05 | −0.94 | 0.35 | 0.85 | 0.28 | 3.07 | <0.001 | −0.16 | 0.10 | −1.70 | 0.09 |
| Bipolar Disorder | −0.05 | 0.04 | −1.25 | 0.21 | 1.77 | 0.50 | 3.54 | <0.001 | −0.52 | 0.18 | −2.94 | <0.00 |
| Anti Social Personality | −0.08 | 0.04 | −1.86 | 0.06 | 0.93 | 0.40 | 2.31 | 0.02 | −0.03 | 0.14 | −0.23 | 0.82 |
Only significant main effects and/or interaction with time are present.
Includes Conduct, Oppositional Defiant, and Attention Deficit Hyperactivity Disorders.
Antecedent: prior death; Baseline: from death to 9 months after; Longitudinal: greater that 9 months after death.
Table 3 presents the most parsimonious set of antecedent and baseline predictors and correlates after controlling for age of offspring. A bereavement X time interaction was found (β=0.16; 95% CI, −0.01 to 0.32; z=1.89; P=.06), with the bereaved group showing a slower rate of decrease in HRBs than the nonbereaved group. In addition, main effects of proband antisocial personality (β=0.67; 95% CI, 0.39 to 0.95; z=4.71; P<.001), proband anxiety disorders (β=0.42; 95% CI, 0.23 to 0.60; z=4.35; P<.001), offspring sex (β= −0.30; 95% CI, −0.44 to −0.15; z= −4.04; P<.001), race (β= −0.43; 95% CI, −0.65 to −0.21; z= −3.91; P<.001), and aggression (β=0.01; 95% CI, 0.01 to 0.02; z=6.75; P<.001) were significant.
Table 3.
The Most Parsimonious Antecedents and Baseline Predictors when Controlling for Age of Offspring
| YRB | β | SE | z | P | 95% CI | |
|---|---|---|---|---|---|---|
| Bereavement | −0.22 | 0.23 | −0.99 | 0.32 | −0.67 | 0.22 |
| Time | −0.14 | 0.06 | −2.54 | 0.01 | −0.25 | −0.03 |
| Bereavement by Time | 0.16 | 0.08 | 1.89 | 0.06 | −0.01 | 0.32 |
| Offspring | ||||||
| Gender | −0.30 | 0.07 | −4.04 | <0.001 | −0.44 | −0.15 |
| Race | −0.43 | 0.11 | −3.91 | <0.001 | −0.65 | −0.21 |
| Age | 0.02 | 0.01 | 1.35 | 0.18 | −0.01 | 0.04 |
| Aggression | 0.01 | 0.002 | 6.75 | <0.001 | 0.01 | 0.02 |
| Proband Lifetime | ||||||
| Anxiety | 0.42 | 0.10 | 4.35 | <0.001 | 0.23 | 0.60 |
| Antisocial Personality | 0.67 | 0.14 | 4.71 | <0.001 | 0.39 | 0.95 |
LONGITUDINAL CORRELATES OF HRBs
After controlling for age of offspring, an interaction with time was found with offspring functional impairment (β=0.008; 95% CI, 0.004–0.01; z=3.55; P<.001). Offspring who were functionally impaired showed a slower decrease in HRBs over time compared with those with better functioning (Table 4).
Table 4.
The Most Parsimonious Longitudinal Predictors when Controlling for Age of Offspring.
| YRB | β | SE | z | P | 95% CI | |
|---|---|---|---|---|---|---|
| Bereavement | −0.18 | 0.24 | −0.77 | 0.44 | −0.65 | 0.28 |
| Time | −0.80 | 0.20 | −4.05 | <0.001 | −1.19 | −0.41 |
| Bereavement by Time | 0.16 | 0.08 | 1.92 | 0.06 | −0.003 | 0.32 |
| Offspring | ||||||
| Functional Impairment | −0.03 | 0.008 | −3.61 | <0.001 | −0.05 | −0.01 |
| Functional Impairment by Time | 0.008 | 0.002 | 3.55 | <0.001 | 0.004 | 0.01 |
| Age | 0.02 | 0.01 | 1.66 | 0.10 | −0.005 | 0.05 |
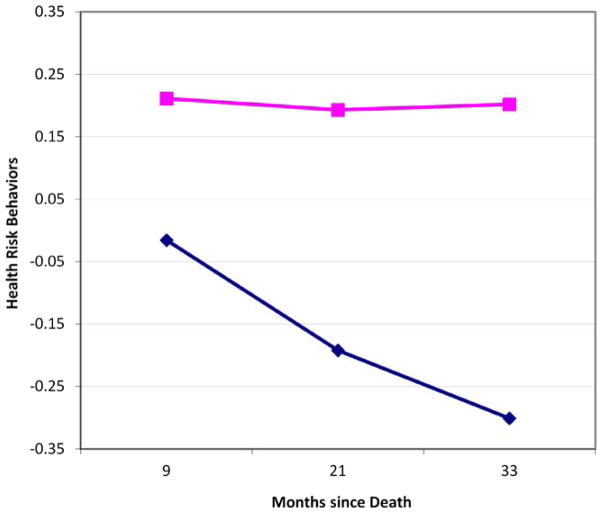
Controlling simultaneously for antecedent, baseline, and longitudinal correlates of HRBs, the bereavement × time interaction with respect to HRBs was significant (β=0.18;95% CI, 0.01 to 0.34; z=2.13; P=.03) (Table 5). As depicted in the Figure, HRBs declined more sharply in the nonbereaved control group. Offspring sex (β= −0.30; 95% CI, −0.45 to −0.16; z= −4.11; P<.001), race (β= −0.41; 95% CI, −0.63 to 0.19; z= −3.70; P<.001), and aggression (β=0.01; 95% CI, 0.007 to 0.01; z=6.10; P<.001) were significant predictors of HRBs. In addition, proband antisocial personality (β=0.67; 95% CI, 0.39 to 0.95; z=4.70; P<.001) and proband anxiety disorders (β=0.41; 95% CI, 0.22 to 0.59; z=4.26; P<.001) were also significant predictors of HRBs.
Table 5.
The Most Parsimonious Antecedent, Baseline and Longitudinal Predictors when Controlling Age of Offspring.
| YRB | β | SE | z | P | 95% CI | |
|---|---|---|---|---|---|---|
| Bereavement | −0.31 | 0.23 | −1.32 | 0.19 | −0.76 | 0.15 |
| Time | −0.47 | 0.20 | −2.38 | 0.02 | −0.85 | −0.08 |
| Bereavement by Time | 0.18 | 0.08 | 2.13 | 0.03 | 0.01 | 0.34 |
| Offspring | ||||||
| Gender | −0.30 | 0.07 | −4.11 | <0.001 | −0.45 | −0.16 |
| Age | 0.02 | 0.01 | 1.32 | 0.19 | −0.01 | 0.04 |
| Race | −0.41 | 0.11 | −3.70 | <0.001 | −0.63 | −0.19 |
| Aggression | 0.01 | 0.002 | 6.10 | <0.001 | 0.007 | 0.01 |
| Functional impairment | −0.01 | 0.008 | −1.80 | 0.07 | −0.03 | 0.001 |
| Functional impairment by Time | 0.004 | 0.002 | 1.74 | 0.08 | −0.001 | 0.01 |
| Proband Lifetime | ||||||
| Anxiety | 0.40 | 0.10 | 4.26 | <0.001 | 0.22 | 0.59 |
| Antisocial Personality | 0.67 | 0.14 | 4.70 | <0.001 | 0.39 | 0.95 |
Figure.
Effect of Bereavement over HRBs over Time
COMMENT
The purpose of this study was to examine the course of HRBs during 3 years after the parent’s death in bereaved youth compared with nonbereaved controls. Over time, the bereaved group showed higher numbers of HRBs compared with the nonbereaved group, even after controlling for antecedent, baseline, and longitudinal correlates that affected the trajectory of HRBs. In addition, several antecedents, correlates, and sequelae of bereavement were found to be associated with HRBs. These variables included proband antisocial personal and anxiety disorders as well as offspring characteristics (eg, race, sex, functioning, and aggression). We discuss the implications of these findings and place them in the context of the extant literature after discussing the limitations and strengths of the study.
This study is one of the few population-based, controlled, longitudinal investigations of parental bereavement and one of the few studies of child bereavement to examine HRBs. Retention was relatively good; however, there was differential attrition, with greater loss of participants in the bereaved than in the control group, as well as of those whose caregivers showed higher levels of functional impairment. We believe that this attrition biases the study toward the null hypothesis, since our findings indicate that this population, if retained, would have shown higher HRBs. This study was also limited insofar as the first assessment was performed 9 months after the death, with the possibility of retrospective bias. In particular, we have no measure of the HRB frequency before the parent’s death. Although the relationship between caregiver function and offspring behavior is expected and has been well documented,49,50 we do not have more fine-grained data on the parental discipline and positive parenting that might shed light on the mechanism of this association.
In this longitudinal study, we demonstrated that parentally bereaved youth show persistently higher levels of HRBs compared with nonbereaved youth. Although a previous report8 found no significant differences in individual HRBs between bereaved and nonbereaved youth 9 months after a parent’s death, in this study we treated the number of HRBs in those same groups as a continuous measure, which provided a more sensitive measure of HRBs over time.51 This association between HRBs and bereavement is consistent with the view that a broad range of family adversities, bereavement among them, can lead to increased HRBs. Although it is difficult to compare across studies, the univariate risk of HRBs associated with bereavement appears to be as large, or larger, than the effects of living in a single-parent household.52 In addition to the effect of bereavement on HRBs, offspring levels of aggression and overallfunctional impairment were also significantly associated with the HRBs. These latter associations are consonant with the role of inappropriate aggression and poor assessment of consequences of behavior in the genesis of some HRBs.
Bereavement may predispose youth to HRBs because bereaved youth have greater loading for parental psychopathologic factors, including antisocial personality disorder, that increase the risk for violent behavior and psychiatric impairment in offspring.1 Specifically, parental antisocial personality disorder predisposed the parent to premature death and increased the likelihood that surviving offspring had increased numbers of HRBs. Although the design of this study cannot disentangle genetic and environmental influences of parental antisocial behavior, there is broad evidence53 for both pathways to be operative. In addition, bereavement disrupts the usual support networks and parental monitoring, and this disruption in turn has been found to be associated with a greater level of offspring aggression.2,54 These results give clues as to which youth are at the highest risk to experience HRBs and what vulnerabilities might be targets for prevention or amelioration.
In summary, we found that parentally bereaved youth have a pattern of higher frequencies of HRBs over time compared with nonbereaved youth, even after adjusting for other correlates that predispose to HRBs. Clinicians who care for bereaved youth should assess them for HRBs. Further work on the development of preventive interventions to attenuate the effects of bereavement on HRBs may be indicated.
Acknowledgments
Funding/Support: This study work was supported by an R01 grant (MH65368, Dr Brent), a K01 grant (MH077930, Dr Melhem), and a T32 grant (MH18951, Dr Brent) from the National Institute of Mental Health, and by the Binational Commission of Exchange Visitor Country, US Department of State (Fulbright Scholars) (Dr Hamdan).
Role of Sponsors: The National Institute of Mental Health did not participate in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Additional Contributions: Emily Hogan, MS, and William McKenna, BS (Western Psychiatric Institute and Clinic), assisted in the acquisition of data for this study, for which they received compensation. Wethank the families for their participation.
Author Contributions: Dr Hamden and Mr Mazariegos contributed equally to this work. Drs Hamdan, Melhem, and Brent had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Hamdan, Melhem, and Brent. Acquisition of data: Hamdan, Melhem, Walker Payne, and Brent. Analysis and interpretation of data: Hamdan, Mazariegos, Melhem, Porta, Walker Payne, and Brent. Drafting the manuscript:Hamdan and Brent. Critical revision of the manuscript for important intellectual content: Hamdan, Mazariegos, Melhem, Porta, Walker Payne, and Brent. Statistical Analysis: Hamdan, Mazariegos, Melhem, Porta, and Brent. Obtaining funding: Hamdan, Melhem, and Brent. Administrative, technical, and material support: Hamdan, Walker Payne, and Brent. Study supervision: Hamdan, Melhem, Walker Payne, and Brent.
Financial Disclosure: Dr Brent has received research support from the National Institute of Mental Health, receives royalties from Guilford Press, and serves as an editor for UpToDate Psychiatry.
References
- 1.Melhem NM, Walker M, Moritz G, Brent DA. Antecedents and sequelae of sudden parental death in offspring and surviving caregivers. Arch Pediatr Adolesc Med. 2008;162(5):403–410. doi: 10.1001/archpedi.162.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brent D, Melhem N, Donohoe MB, Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. Am J Psychiatry. 2009;166(7):786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dowdney L. Childhood bereavement following parental death. J Child Psychol Psychiatry. 2000;41(7):819–830. [PubMed] [Google Scholar]
- 4.Kaplow JB, Saunders J, Angold A, Costello EJ. Psychiatric symptoms in bereaved versus nonbereaved youth and young adults: a longitudinal epidemiological study. J Am Acad Child Adolesc Psychiatry. 2010;49(11):1145–1154. doi: 10.1016/j.jaac.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herrenkohl TI, Kosterman R, Mason WA, Hawkins JD, McCarty CA, McCauley E. Effects of childhood conduct problems and family adversity on health, health behaviors, and service use in early adulthood: tests of developmental pathways involving adolescent risk taking and depression. Dev Psychopathol. 2010;22(3):655–665. doi: 10.1017/S0954579410000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dodge KA, Greenberg MT, Malone PS Conduct Problems Prevention Research Group. Testing an idealized dynamic cascade model of the development of serious violence in adolescence. Child Dev. 2008;79(6):1907–1927. doi: 10.1111/j.1467-8624.2008.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Muñiz-Cohen M, Melhem NM, Brent DA. Health risk behaviors in parentally bereaved youth. Arch Pediatr Adolesc Med. 2010;164(7):621–624. doi: 10.1001/archpediatrics.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker EA, Gelfand A, Katon WJ, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999;107(4):332–339. doi: 10.1016/s0002-9343(99)00235-1. [DOI] [PubMed] [Google Scholar]
- 10.Henry DB, Tolan PH, Gorman-Smith D. Longitudinal family and peer group effects on violence and nonviolent delinquency. J Clin Child Psychol. 2001;30 (2):172–186. doi: 10.1207/S15374424JCCP3002_5. [DOI] [PubMed] [Google Scholar]
- 11.Herrenkohl TI, Guo J, Kosterman R, Hawkins JD, Catalano RF, Smith BH. Early adolescent predictors of youth violence as mediators of childhood risks. J Early Adolesc. 2001;21(4):447–469. 1177/02724316010210004004. [Google Scholar]
- 12.Stroebe MS, Folkman S, Hansson RO, Schut H. The prediction of bereavement outcome: development of an integrative risk factor framework. Soc Sci Med. 2006;63(9):2440–2451. doi: 10.1016/j.socscimed.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 13.Bonanno GA, Wortman CB, Lehman DR, et al. Resilience to loss and chronic grief: a prospective study from preloss to 18-months postloss. J Pers Soc Psychol. 2002;83(5):1150–1164. doi: 10.1037//0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- 14.Cerel J, Roberts TA. Suicidal behavior in the family and adolescent risk behavior. J Adolesc Health. 2005;36(4):352e9–352e16. doi: 10.1016/j.jadohealth.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Grunbaum JA, Kann L, Kinchen SA, Ross J, Hawkins J, Lowry R. Youth risk behavior surveillance—United States, 2003. MMWR Surveill Summ. 2004;53 (2):1–96. [PubMed] [Google Scholar]
- 16.Eaton DK, Kann L, Kinchen S, et al. Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57(4):1–131. [PubMed] [Google Scholar]
- 17.Sells CW, Blum RW. Morbidity and mortality among US adolescents: an overview of data and trends. Am J Public Health. 1996;86(4):513–519. doi: 10.2105/ajph.86.4.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korhonen T, Levälahti E, Dick DM, et al. Externalizing behaviors and cigarette smoking as predictors for use of illicit drugs: a longitudinal study among Finnish adolescent twins. Twin Res Hum Genet. 2010;13(6):550–558. doi: 10.1375/twin.13.6.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Testa CR, Steinberg L. Depressive symptoms and health-related risk-taking in adolescence. Suicide Life Threat Behav. 2010;40(3):298–305. doi: 10.1521/suli.2010.40.3.298. [DOI] [PubMed] [Google Scholar]
- 20.Schilling EA, Aseltine RH, Gore S. The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Soc Sci Med. 2008;66(5):1140–1151. doi: 10.1016/j.socscimed.2007.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl. 2007;31(3):211–229. doi: 10.1016/j.chiabu.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Weinberger DA. Distress and self-restraint as measures of adjustment across the life span: confirmatory factor analyses in clinical and nonclinical samples. Psychol Assess. 1997;9(2):132–135. doi: 10.1037/1040-3590.9.2.132. [DOI] [Google Scholar]
- 23.Perry-Jenkins M, Gillman S. Parental job experiences and children’s well being: the case of two-parent and single-mother working-class families. J Fam Econ Issues. 2000;21:123–147. [Google Scholar]
- 24.Buss AH, Perry MP. The Aggression Questionnaire. J Pers Soc Psychol. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- 25.Buss AH, Warren WL. The Aggression Questionnaire Manual. Los Angeles, CA: Western Psychological Services; 2000. [Google Scholar]
- 26.Dubow EF, Ullman DG. Assessing social support in elementary school children: the Survey of Children’s Social Support. J Clin Child Psychol. 1989;18:52–64. [Google Scholar]
- 27.Hollingshead A. Four-Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 28.Shaffer D, Gould MS, Brasic J, et al. A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 29.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33(6):766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 30.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 31.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 Youth Risk Behavior Survey questionnaire. J Adolesc Health. 2002;31(4):336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 32.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-age Children—Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 34.Hawton K, Appleby L, Platt S, et al. The psychological autopsy approach to studying suicide: a review of methodological issues. J Affect Disord. 1998;50(2–3):269–276. doi: 10.1016/s0165-0327(98)00033-0. [DOI] [PubMed] [Google Scholar]
- 35.Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res. 1995;5:237–249. [Google Scholar]
- 36.Birmaher B, Khetarpal S, Brent D, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 37.Reynolds WM. Suicidal ideation and depression in adolescents: assessment and research. In: Lovibond P, Wilson P, editors. Clinical and Abnormal Psychology. Amsterdam, the Netherlands: Elsevier Science; 1989. pp. 125–135. [Google Scholar]
- 38.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 39.Beck AT, Epstein N, Brown G, Steer RA. An inventory formeasuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 40.Reynolds WM. Psychometric characteristics of the Adult Suicidal Ideation Questionnaire in college students. J Pers Assess. 1991;56(2):289–307. doi: 10.1207/s15327752jpa5602_9. [DOI] [PubMed] [Google Scholar]
- 41.Foa EB, Johnson KM, Feeny NC, Treadwell KR. The Child PTSD Symptom Scale: a preliminary examination of its psychometric properties. J Clin Child Psychol. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- 42.Foa E, Johnson KM, Feeny NC. Reliability and validity of a brief instrument for assessing post traumatic stress disorder. J Trauma Stress. 1993;6:459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- 43.Brand AH, Johnson JH. Note on reliability of the Life Events Checklist. Psychol Rep. 1982;50:1274. [Google Scholar]
- 44.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 45.Dubow EF, Ullman DG. Assessing social support in elementary school children: the Survey of Children’s Social Support. J Clin Child Psychol. 1989;18(1):52–64. 10.1207s15374424jccp1801_7. [Google Scholar]
- 46.Spirito A, Stark LJ, Williams C. Development of a brief coping checklist for use with pediatric populations. J Pediatr Psychol. 1988;13(4):555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- 47.Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55(3):234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Chaffin M, Wherry JN, Newlin C, Crutchfield A, Dykman R. The Abuse Dimensions Inventory: initial data on a research measure of abuse severity. J Interpers Violence. 1997;12(4):569–589. doi: 10.1177/088626097012004006. [DOI] [Google Scholar]
- 49.Haine RA, Wolchik SA, Sandler IN, Millsap RE, Ayers TS. Positive parenting as a protective resource for parentally bereaved children. Death Stud. 2006;30(1):1–28. doi: 10.1080/07481180500348639. [DOI] [PubMed] [Google Scholar]
- 50.Kwok OM, Haine RA, Sandler IN, Ayers TS, Wolchik SA, Tein JY. Positive parenting as amediator of the relations between parental psychological distress and mental health problems of parentally bereaved children. J Clin Child Adolesc Psychol. 2005;34(2):260–271. doi: 10.1207/s15374424jccp3402_5. [DOI] [PubMed] [Google Scholar]
- 51.Abdelnoor A, Hollins S. The effect of childhood bereavement on secondary school performance. Educ Psychol Pract. 2004;20(1):43–54. [Google Scholar]
- 52.Blum RW, Beuhring T, Shew ML, Bearinger LH, Sieving RE, Resnick MD. The effects of race/ethnicity, income, and family structure on adolescent risk behaviors. Am J Public Health. 2000;90(12):1879–1884. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moffitt TE. The new look of behavioral genetics in developmental psychopathology: gene-environment interplay in antisocial behaviors. Psychol Bull. 2005;131(4):533–554. doi: 10.1037/0033-2909.131.4.533. [DOI] [PubMed] [Google Scholar]
- 54.Windle M, Brener N, Cuccaro P, et al. Parenting predictors of early-adolescents’ health behaviors: simultaneous group comparisons across sex and ethnic groups. J Youth Adolesc. 2010;39(6):594–606. doi: 10.1007/s10964-009-9414-z. [DOI] [PubMed] [Google Scholar]