Abstract
Objective
To examine the relationship between adolescents’ cigarette smoking experiences and alternative tobacco product (ATP) use.
Methods
Multiple indicators and multiple causes (MIMIC) models estimated simultaneously the relationship between cigarette smoking experiences and ATP use among high school students (N=1827) completing the 2009 Virginia Youth Tobacco Survey.
Results
Overall, ATP use was associated with adolescents’ ever use of cigarettes, early onset of cigarette smoking, cigarettes smoked per day, and peer smoking; however, important model differences between racial/ethnic groups were observed.
Conclusions
Prevention and cessation programs might reduce adolescent ATP use by targetting specific characterstics of cigarette smoking.
Keywords: adolescents, cigarette smoking, alternative tobacco product use, polytobacco
Adolescents frequently experiment with cigarette smoking before trying other forms of tobacco like cigars, smokeless tobacco (SLT), bidis/clove cigarettes, and waterpipe tobacco smoking (WTS).1-3 Still, by the end of adolescence, nearly 90% of adolescent cigarette smokers have tried an alternative tobacco product (ATP);4 and between 46 and 50% of adolescent cigarette smokers have used an ATP in the past month.5,6 In fact, concomitant use of multiple tobacco products may be the norm among many adolescent populations.3,4
Only a handful of studies have examined cigarette smoking and ATP use in adolescence,4,5,7,8 and they suggest that cigarette use is a major risk factor for ATP use in this population. For instance, earlier studies on adolescent tobacco use reveal that ever smokers (ie, tried cigarette smoking) and current smokers (ie, past-month use of cigarettes) are more likely than never smokers and noncurrent smokers (ie, no past-month use) to report current ATP use.4,7 These findings are corroborated by more recent studies on national youth samples that show current smokers are more likely than their coevals to use cigars, SLT, and bidis/cloves in the past month.8
Nonetheless, the extent to which smoking characteristics such as cigarette smoking frequency (ie, number of days smoked) and consumption (ie, cigarettes smoked per day; cpd) influnce adeloscent ATP use is not fully understood. This issue is of significant importance because individual differences in cigarette smoking frequency and consumption predict ATP use and dependence in adults. Specifically, adult smoker characteristics to include established cigarette smoking (100+ cigarettes in lifetime);9 cigarette smoking of higher frequency (eg, daily versus intermittent smoking),10 and lower cigarette smoking intensity (ie, < 10 versus > 10 cpd)11 are associated with ATP use and greater severity of nicotine dependence.12
Interestingly, only one study has explored the relationship between smoking characteristics related to cigarette frequency and consumption and ATP use in adolescence.5 In this study of 2800 adolescents (aged 12 to 18), both low-frequency/low intensity and high-frequency/high-intensity cigarette smoking was associated with cigar, SLT, and bidis/cloves use. Although informative, this work did not address likely variations in smoking characteristics and ATP use due to racial/ethnic group affliation. National data on high school students reveal that white/European American adolescents are more likely than black/African Americans to report smoking more days per month and more cpd as well as 100 or more cigarettes in their lifetime.13,14 Considering ATP use trends among adult cigarette smokers, smoking characteristics related to frequency, consumption, and lifetime use (ie, established smoking) may predict differentially the ATP behaviors of white/European American and black/African American adolescents.
In addition to smoking characteristics, the extent to which adolescents’ exposure to familial and peer smoking influnces is related to ATP use also is largely understudied. Adolescents’ first experiences with tobacco occur typically with family and peers who smoke cigarettes,15-17 and exposure to familial and peer smoking influnces is related to ATP use.4,18 However peer cigarette smoking to increase the likelihood of adolescent ATP use by 3-fold,7 whereas others report familial smoking exposure to be of lesser importance than peer smoking affiliations.2,19 Importantly, these studies considered the influnce of environmental tobacco smoking on any ATP use and did not observe the impact of familial and peer smoking on specific ATPs (eg, SLT, cigars, and WTS). Environmental smoking influnces may differentially impact adolescents’ susceptibility to some forms of tobacco compared to others (eg, cigars 20), and this differential impact may be especially relevant among racial/ethnic minority adolescents.21,22 Whether adolescents’ smoking experiences (ie, cigarette smoking characteristics and related influnces) increase uniformly the risk of consuming other tobacco products has not been determined.
The current study uses a model of adolescent ATP use to (1) describe the relationship between adolescents’ cigarette smoking experiences and their current use of popular ATPs (ie, cigars, SLT, and WTS), (2) examine whether these associations are similar across racial/ethnic groups, and (3) determine if certain experiences with cigarette smoking are more closely associated with use of some ATPs than others. Findings will inform tobacco prevention and cessation programs about characteristics of adolescent cigarette smoking most influential in the initiation and maintenance of other tobacco use behaviors.
METHODS
Research Design and Procedures
This study tested a multiple indicators and multiple causes (MIMIC) model using secondary data from the 2009 Virginia Youth Tobacco Survey (YTS), an ongoing, statewide monitoring and surveillance survey of tobacco use conducted by the Virginia Foundation for Healthy Youth (formerly the Virginia Tobacco Settlement Foundation; VTSF), Centers for Disease Control and Prevention (CDC), and the Survey and Evaluation Research Laboratory (SERL) at Virginia Commonwealth University (VCU). A total of 100 Virginia public schools (50 middle schools and 50 high schools) were randomly selected to participate in the 2009 Virginia YTS. A 2-stage cluster sample design (school and class level) was used to produce a representative sample of students enrolled in public middle schools and high schools. The overall response rate for the 2009 Virginia YTS was 60.9%. The 2009 Virginia YTS results were weighted by the CDC to account for selection bias differential nonresponse rates and demographics to include race, gender, and grade. Additional information about the 2009 Virginia YTS research design and procedures may be found here: http://healthyyouthva.org/vtsf/data/youth-tobacco-survey.asp.
The current study focused on students enrolled in high school grades. Of the 50 high schools randomly selected to take part in the study, 36 (72%) agreed to participate. About 82% of students (N=1827 of 2232) in selected high school classrooms returned usable surveys. This study draws from this representative sample of high school students (N=1827) who completed the 2009 Virginia YTS. The current study used public access secondary data that did not contain identifying information and were deemed exempt from review by the VCU Institutional Review Board (IRB).
Measures
Cigarette smoking experiences
Respondents reported whether they ever tried cigarette smoking (no/yes), age of first cigarette (< 13 years old or older), lifetime number of cigarettes (0-100 or more), frequency of past-month cigarette use (0 days, 1-2 days, 3-5 days; 6-10 days, 11-19 days, 20-29 days, all 30 days), number of cigarettes smoked per day (cpd; None, fewer than 1, 1, 2-5, 6-10, 11-20, more than 20), if they had ever smoked daily (no/yes), household smoking (no/yes), and peer smoking (0-1 or more).
ATP use
Respondents completed items on past-month use of cigars (eg, cigars, little cigars, and cigarillos), SLT (eg, chewing tobacco, snuff, and dip), and WTS (eg, shisha and hookah). Importantly, the 2009 YTS included additional items on novel, brand-specific tobacco products such as snus (Swedish snuff; moist powdered tobacco packaged in a small pouch) and a brand-specific cigar product (ie, Black & Mild cigarillos). Respondents indicating past-month use of Snus were coded as having used an SLT product, and those reporting past-month use of Black & Mild cigarillos were coded as having used a cigar product.
Demographics
Age (11 and younger; 12-17; 18 and older), gender (female/male), Hispanic descent person (yes/no), race/ethnicity (American Indian or Alaskan Native, African American, Asian, and white), grade (9th-12th), and discretionary income (none, less than $1 to $5, $6 to $10, $11 to $20, more than $20) were assessed.
Data Analysis
Using PASW Statistics 18, we examined each of the study variables and their bivariate relationships. Those younger than 14 years of age (N=14; 0.8%) were dropped, yielding a final sample of 1813 adolescents. Missing values ranged from 0.1 to 8.6% of the data due to participant nonresponse to tobacco use items. Importantly, other studies using national youth survey data report similar or higher nonresponse rates to tobacco-related items.5 A missing-value analysis revealed that the highest percentage of nonresponses was on the cpd and SLT items. There was little evidence of systematic bias in item nonresponse based on adolescents’ age, gender, and race/ethnicity. Guided by well-established multiple imputation procedures,23,24 we corrected for bias due to nonresponses in an effort to ensure the data most accurately reflected youth populations in Virginia.
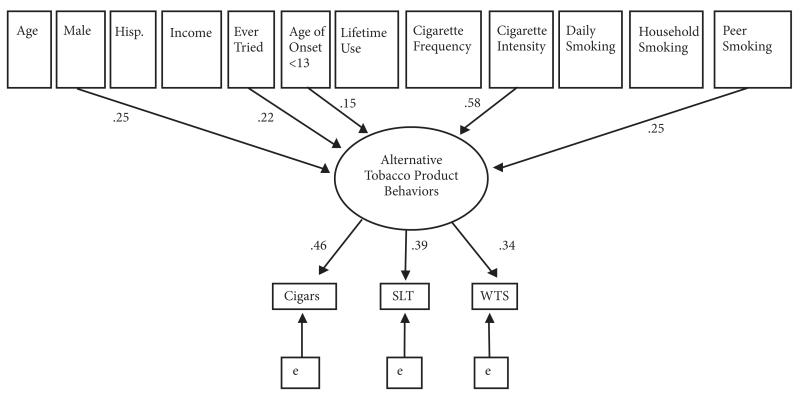
Amos 16.025 was used to test the MIMIC model. The MIMIC modeling technique was selected for this study because it estimates simultaneously the effect of the indicators (SLT, cigars, and WTS) on the latent variable (ATP use) and the direct effects of observed variables (smoking experiences) on the latent variable. Figure 1 presents the one-factor MIMIC model estimated for this study. The bottom half of the model (ie, measurement model) diagrams the relationship between the individual ATP-use items and the latent construct. The top half of the model (ie, regression model) presents the study variables (ie, cigarette smoking experiences) hypothesized to have an effect on the latent construct. Covariates (ie, age, gender, Hispanic descent, and discretionary income) were included in the model to provide adjusted estimates.
Figure 1. Multiple Indicators and Multiple Causes (MIMIC) Model.
Note.
Covariances in the model are not shown.
Hisp. = of Hispanic descent; SLT = smokeless tobacco; WTS = waterpipe tobacco smoking
MIMIC model comparisons between racial/ethnic groups were performed following structural equation modeling (SEM) procedures outlined by Schumacker and Lomax.26 This allowed for testing significant differences between certain group parameters in the MIMIC model; in this case, comparing parameters (eg, ever smoked cigarettes → ATP use) across racial/ethnic minority groups. The parameters for cigarette smoking experiences and ATP use were set equal across groups to allow pairwise comparisions of standardized coefficients. Critical ratios (CR) for differences tests were computed to examine differences between racial/ethnic groups on all direct effect parameters in the MIMIC model. CR values meeting or exceeding ± 1.96 were considered statistically significant.
Several indexes were used to determine adequate fit of the MIMIC models: the chi-square/degrees of freedom ratio (χ2min/df <3),27 the comparative fit index (CFI; ≥ .95), the Tucker Lewis Index (TLI; ≥ .95),28 and the root mean square error of approximation (RMSEA; < .08).26 Biased-corrected bootstrap 95% confidence intervals (BC 95% CIs) were computed for individual indirect effects in the MIMIC model to determine the influence of cigarette smoking experiences on individual ATP use. Bootstrapped estimates were based on 2000 bootstrap samples. Evidence of a significant indirect effect was noted by confidence intervals that did not overlap zero.
RESULTS
Sample Characteristics
Table 1 presents demographic information and prevalence rates for adolescents’ cigarette and ATP use. The median age of adolescents was 16 years. Males (51.1%) and females (48.8%) were equally represented in the final sample. The majority of adolescents were of non-Hispanic descent (91.7%). White/European American adolescents (60.6%) constituted the majority of the sample followed by black/African Americans (29.9%). Most adolescents reported a weekly discretionary income of more than 20 dollars (57.3%). Less than half (44.0%) of all adolescents reported having tried cigarettes in their lifetime (not presented in table). About 20% of youth were current smokers (ie, past 30-day use of cigarettes): 11.8% were established smokers (ie, smoked 100 or more cigarettes), and 14.2% indicated daily smoking during their life-time (not presented in table). In terms of ATP use, adolescents reported using cigars (20.5%) more than SLT (10.7%) and WTS (8.9%).
Table 1. Demographic Characteristics of High School Students in Virginia,2009 (Weighted Data).
| Sample Characteristics | % (95%CI) |
|---|---|
| Age | |
| 14 | 14.6 (13.2, 16.1) |
| 15 | 26.4 (24.2, 28.7) |
| 16 | 25.7 (23.4, 28.0) |
| 17 | 24.0 (21.7, 26.2) |
| 18 and older | 9.0 (7.5, 10.5) |
| Gender | |
| Female | 48.8 (46.3, 51.4) |
| Male | 51.1 (48.5, 53.6) |
| Hispanic Descent | |
| No | 91.7 (90.4, 93.1) |
| Yes | 8.2 (6.8, 9.5) |
| Race | |
| White | 60.6 (58.1, 63.0) |
| Black | 29.9 (27.5, 32.2) |
| Multiple race groups | 9.4 (8.0, 10.7) |
| Grade | |
| 9th | 26.5 (24.6, 28.4) |
| 10th | 25.0 (22.5, 27.5) |
| 11th | 24.3 (22.1, 26.6) |
| 12th | 24.0 (21.8, 26.2) |
| Income | |
| None to < $1 | 10.4 (8.9, 11.9) |
| $1 to $5 | 5.6 (4.4, 6.7) |
| $6 to $10 | 7.7 (6.4, 9.0) |
| $11 to $20 | 18.8 (16.8, 20.9) |
| $21 or more | 57.3 (54.8, 59.8) |
| Tobacco Use Behaviors | |
| Cigarettes | 19.3 (17.2, 21.4) |
| Cigars | 20.5 (18.3, 22.7) |
| Smokeless tobacco (SLT) | 10.7 (9.0, 12.4) |
| Waterpipe (hookah/ shisha) | 8.9 (7.4, 10.4) |
|
| |
| Total Sample (N=1813) | |
Multiple Indicators and Multiple Causes (MIMIC) Model: The Overall Sample
Confirmatory factor analysis showed that past 30-day use of cigars (B=.62), SLT (B=.56), and WTS (B = .41) were good reflective indicators of the measurement model. The fully saturated MIMIC model showed adequate fit χ2 min/df = 2.10; CFI=.99; TLI=.98; RMSEA = .03 (.02, .04). Nonsignificant paths were set to zero (ie, constrained model); and the fit of the model was improved, χ2min/df = 2.05; CFI=.99; TLI=.99; RMSEA=.02 (.01, .03). Simultaneous effects for demographic and smoking experiences were estimated in the regression model (Figure 1). Adolescent males (B=.25, p < .001) were more likely than females to report ATP use. Those who tried cigarettes were more susceptible to ATP use than were adolescents who had not smoked cigarettes (B=.22, p < .001), and adolescents who attempted cigarette smoking before the age of 13 were particularly vulnerable (B=.15, p < .001). The number of cigarettes smoked per day was related to ATP use such that adolescents who smoked more cpd were more likely to engage in ATP use (B=.58, p < .001). Adolescents with one or more peers who smoked cigarettes were more likely to report ATP use than were youth with peers who did not smoke (B=.25, p < .001).
Probing the influences of cigarette smoking experiences on individual ATP use showed the indirect effect of having ever smoked cigarettes on cigar smoking, B=.10 (0.06, 0.14), was slightly larger than SLT, B=.08 (0.05, 0.12), and WTS, B=.07 (0.04, 0.10) (Table 2). There were similar associations between age of smoking onset and adolescents’ ATP use. The indirect effect of number of cigarettes smoked per day on cigar smoking, B=.27 (0.20, 0.33), was larger than SLT, B=.23 (0.17, 0.29), and WTS, B=.19 (0.14, 0.25). In addition, the indirect effect of peer smoking was larger for cigar smoking, B=.12 (0.06, 0.17), followed by SLT, B=.10 (0.06, 0.14), and WTS, B=.08 (0.05, 0.12).
Table 2. Standardized Indirect Effects of Adolescent Smoking Experiences on ATP Use.
| Alternative Tobacco Products (ATPs) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cigars |
Smokeless |
Waterpipe |
|||||||
| Smoking Experiences | b | 95% CI | p ≤ | b | 95% CI | P≤ | b | 95% CI | p ≤ |
| Ever smoked | .10 | (.06, .14) | .01 | .08 | (.05, .12) | .01 | .07 | (.04, .11) | .01 |
| Age of onset | .07 | (.01, .12) | .01 | .06 | (.01, .11) | .01 | .05 | (.01, .09) | .01 |
| Cigarettes per day | .27 | (.20, .33) | .01 | .23 | (.17, .29) | .01 | .19 | (.14, .25) | .01 |
| Peer smoking | .12 | (.06, .17) | .01 | .10 | (.06, .14) | .01 | .08 | (.05, .12) | .01 |
MIMIC Model Comparisons Across Racial/Ethnic Groups
Multiple group comparisons were conducted to test significant differences in the relationship between cigarette smoking experiences and ATP use for white/European American (60% of the total sample) and black/African American (about 30% of the total sample) adolescents. Stated another way, MIMIC models were compared across race/ethnicity to determine differences in the direct effect parameters. The multiple group chi-square statistic (χ2 min/df = 2.39) supported the configural invariance of the MIMIC model across white/European American and black/African American subsamples. For white/European American adolescents, gender (male; B=.28, p < .001), discretionary income (B=.11, p < .05), ever use of cigarettes (B=.17, p < .05), cigarettes smoked per day (B=.49, p < .001), and peer smoking (B=.26, p < .001) were associated significantly with ATP use. For black/African American adolescents, early smoking onset (B=.38, p < .001), cigarette smoking frequency (B=.40, p < .05), and peer smoking predicted (B=.29, p < .001) ATP use.
Table 3 presents the critical ratios (CR) for differences for direct effect parameters among white/European American and black/African American adolescents. White/European American and black/African American youth were statistically equivalent on most coefficients in the MIMIC model with 2 notable exceptions. Early smoking onset was a stronger predictor of ATP use for black/African Americans than for white/European adolescents (z = 3.58; p < .001); and this effect significantly explained black/African Americans’ early cigarette smoking onset on their use of cigars, b = .17 (.06, .25); SLT, b = .15 (.04, .26); and WTS, b = .14(.04, .25). There was also a statistically significant difference between white/European American and black/African American youth in the relationship between cigarette smoking frequency and ATP, such that cigarette smoking frequency was a stronger predictor for black/African American adolescents than for white/European youth (z = 2.78; p < .001). However, specific ATP use (ie, cigars, SLT, and WTS) among black/African American adolescents was not adequately explained by cigarette smoking frequency (ie, 95% CIs for indirect effects overlapped zero).
Table 3. Critical Ratiosa (CR) for Differences Between Smoking Experiences and ATP Use Among White and African American Adolescents.
| Parameters | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Ever tried cigs | −0.51 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 2. Age of onset < 13 years | 0.00 | 3.58 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 3. Lifetime >100 cigs | 0.00 | 0.00 | −1.47 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 4. Number of days smoked | 0.00 | 0.00 | 0.00 | 2.77 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5. Cigarettes per day | 0.00 | 0.00 | 0.00 | 0.00 | −1.44 | 0.00 | 0.00 | 0.00 |
| 6. Daily smoking | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | −1.05 | 0.00 | 0.00 |
| 7. Household smoking | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | −0.19 | 0.00 |
| 8. Peer smoking | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.12 |
Note.
CR values meeting or exceeding ±1.96 were considered statistically significant (p < .05).
DISCUSSION
Using innovative modeling techniques, this study sought to determine the simultaneous impact of various cigarette smoking experiences (smoking patterns, environmental influences) on ATP use among a representative, statewide sample of high school students. In addition, this survey incorporated assessment of novel tobacco products, like Snus and bran-specific cigarillos, the use of which has not been examined in previous statewide or national tobacco surveillance surveys. Study results support past work with adults in that early experience with cigaretteseg, 29 and peer smokingeg, 7 predicted adolescent ATP behaviors.
Findings also revealed that experiences with cigarette smoking influences adolescents’ susceptibility to some ATPs more so than others. That is, experiences such as ever trying cigarettes, early initiation, cpd, and peer smoking were associated with adolescents’ use of cigars to a greater extent than SLT use and WTS. Accessibility to tobacco products is associated with ever trying and early initiation of smoking,19,30 and cigars may be more readily accessible than other tobacco products. Moreover cigars, especially little cigars and cigarillos (eg, Black and Milds), are most similar to cigarettes in terms of product features and considerably less expensive compared to other ATPs (to include SLT and waterpipe).31,32 Little cigars and cigarillos are also less expensive than cigarettes33 and thus may be a preferred alternative and/or supplemental tobacco product among adolescents who consume cigarettes regularly.32 Importantly, products that are restricted to youth in terms of affordability and/or access may promote reductions in use.34,35
Tobacco dependence also may play a role in these findings and may explain the weak to moderate relationship between cigarette smoking experiences and SLT. That is, heavier cigarette smokers (eg, 11+ cpd) may be less likely to use SLT than are nondaily, light cigarette smokers.11, 36; but see 5 Additionally, concomitant cigarette and SLT users have been observed to smoke, on average, significantly fewer cpd than do concomitant cigarette and cigar users.10 As for WTS, distinct social and cultural features may appeal to adolescents who are not attracted to cigarette smoking.37 In fact, among some college samples, 45% of waterpipe smokers are not current cigarette smokers; and 22% have never tried a cigarette.38 Nonetheless, these and other behaviors remain understudied despite the high prevalence of ATP use among sampled populations.8
Although cigarette smoking experiences were rather robust predictors of adolescent ATP use, there were differences in this relationship between white/European American and black/African American adolescents. For instance, early initiation of cigarette smoking was a stronger predictor of ATP use among black/African American adolescents than white/European American youth. Moreover, whereas cpd predicted ATP use for white/European American adolescents, the number of days smoked during the past month was an important predictor for black/African Americans. As suggested above, these factors may tap into issues of access to and affordability of specific ATPs such as cigars.
Of course, study inferences may be limited by the population sampled, high school students of Virginia, and the cross-sectional nature of the survey employed. Recall bias may also limit study findiings, though previous work demonstrates the reliability and validity of self-report data among adolescents.39,40 Despite these limitations, this study provides additional evidence on the complex relationship between cigarette smoking and ATP use in adolescence. Such evidence is necessary given the dramatic shifts in tobacco prevalence and sales observed over the past decade; cigarette rates have decreased while cigarette prices have increased and vice versa for ATPs.33, Importantly, study findings support the idea that tobacco prevention and intervention programs, at least in Virginia, should consider use of ATPs in combination with cigarette smoking.
Acknowledgments
All work was performed at Virginia Commonwealth University. The National Institute on Minority Health and Health Disparities (NIMHD), Virginia Foundation for Healthy Youth (VFHY; formerly the Virginia Tobacco Settlement Foundation), and the National Cancer Institute (1R01CA120142-01A2) provided support for this study.
Footnotes
There are no conflict of interest to report.
Contributor Information
Aashir Nasim, Virginia Common-wealth University, Institute for Drug and Alcohol Studies, Department of Psychology, Richmond, VA.
Melissa D. Blank, Moffitt Cancer Center, Tobacco Research & Intervention Program, Tampa, FL.
Caroline O. Cobb, Virginia Commonwealth University, Department of Psychology, Richmond, VA.
Thomas Eissenberg, Virginia Common-wealth University, Institute for Drug and Alcohol Studies, Department of Psychology, Richmond, VA.
REFERENCES
- 1.Kopstein A. Tobacco Use in America: Findings from the 1999 National Household Survey on Drug Abuse. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2001. Analytic Series: A-15, DHHS Publication No. SMA 02-3622. [Google Scholar]
- 2.Asfar T, Ward KD, Eissenberg T, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to water-pipe between beginning and established smokers. BMC Public Health. 2005;5:19. doi: 10.1186/1471-2458-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rigotti NA, Lee JE, Wechsler H. U.S. college students’ use of tobacco products: results from a national survey. JAMA. 2000;284(6):699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- 4.Gilpin EA, Pierce JP. Concurrent use of tobacco products by California adolescents. Prev Med. 2003;36:575–584. doi: 10.1016/s0091-7435(02)00064-6. [DOI] [PubMed] [Google Scholar]
- 5.Nasim A, Blank MD, Cobb CO, Eissenberg T. Patterns of alternative tobacco use among adolescent cigarette smokers. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2011.11.022. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bombard JM, Peterson LL, Koval JJ, O’Hegarty M. How are lifetime polytobacco users different from cigarette-only users? Results from a Canadian young adult population. Addict Behav. 2009;34(12):1069–1072. doi: 10.1016/j.addbeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Tercyak KP, Audrain J. Psychosocial correlates of alternate tobacco product use during early adolescence. Prev Med. 2002;35:193–198. doi: 10.1006/pmed.2002.1060. [DOI] [PubMed] [Google Scholar]
- 8.Bombard JM, Rock VJ, Pederson LL, Asman KJ. Monitoring polytobacco use among adolescents: Do cigarette smokers use other forms of tobacco? Nicotine Tob Res. 2008;10(11):1581–1589. doi: 10.1080/14622200802412887. [DOI] [PubMed] [Google Scholar]
- 9.Tomar SL, Giovino GA. Incidence and predictors of smokeless tobacco use among US youth. Am J Public Health. 1998;88:20–26. doi: 10.2105/ajph.88.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rae Olmsted KL, Bray RM, Reyes Guzman CM, et al. Overlap in use of different types of tobacco among active duty personnel. Nicotine Tob Res. 2011;13(8) doi: 10.1093/ntr/ntr060. [DOI] [PubMed] [Google Scholar]
- 11.Peterson AL, Severson HH, Andrews JA, et al. Smokeless tobacco use in military personnel. Mil Med. 2007;172(12):1300–1305. doi: 10.7205/milmed.172.12.1300. [DOI] [PubMed] [Google Scholar]
- 12.Timberlake DS. A latent class analysis of nicotine-dependence criteria and use of alternative tobacco. J Stud Alcohol Drugs. 2008;69:709–717. doi: 10.15288/jsad.2008.69.709. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Youth Risk Behavior Surveillance — United States, 2009. Surveillance Summaries. MMWR. 2010;59(SS-5) [PubMed] [Google Scholar]
- 14.Marshall L, Schooley M, Ryan H, et al. Youth Tobacco Surveillance --- United States, 2001—2002. MMWR Surveill Summ. 2006 May 19;55(3):1–56. [PubMed] [Google Scholar]
- 15.Bricker JB, Peterson AV, Andersen MR, et al. Parents’ and older siblings’ smoking during childhood: changing influences on smoking acquisition and escalation over the course of adolescence. Nicotine Tob Res. 2007;9(9):915–926. doi: 10.1080/14622200701488400. [DOI] [PubMed] [Google Scholar]
- 16.Jackson C, Henriksen L. Do as I say: parent smoking, antismoking socialization, and smoking onset among children. Addict Behav. 1997;22(1):107–114. doi: 10.1016/0306-4603(95)00108-5. [DOI] [PubMed] [Google Scholar]
- 17.Rothwell E, Larmarque J. The use of focus groups to compare tobacco attitudes and behaviors between youth in urban and rural settings. Health Promot Pract. 2011;12(4):551–560. doi: 10.1177/1524839909349179. [DOI] [PubMed] [Google Scholar]
- 18.Tomar SL, Giovino GA. Incidence and predictors of smokeless tobacco use among US youth. Am J Public Health. 1998;88(1):20–26. doi: 10.2105/ajph.88.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyle RG, Claxton AJ, Forster JL. The role of availability social influences and tobacco on adolescent smokeless tobacco use. J Adolesc Health. 1997;20(4):279–285. doi: 10.1016/S1054-139X(96)00272-8. [DOI] [PubMed] [Google Scholar]
- 20.Brooks A, Larkin EMG, Kishore S, Frank S. Cigars, cigarettes, and adolescents. Am J Health Behav. 2008;32(6):640–649. doi: 10.5555/ajhb.2008.32.6.640. [DOI] [PubMed] [Google Scholar]
- 21.Soldz S, Huyser DJ, Dorsey E. Characteristics of users of cigars, bidis, and kreteks and the relationship to cigarette use. Prev Med. 2003;37(3):250–258. doi: 10.1016/s0091-7435(03)00121-x. [DOI] [PubMed] [Google Scholar]
- 22.Frazier AL, Fisher L, Camargo CA, et al. Association of adolescent cigar use with other high-risk behaviors. Pediatrics. 2000;106(2):E26. doi: 10.1542/peds.106.2.e26. [DOI] [PubMed] [Google Scholar]
- 23.Little RJA, Rubin DB. Statistical Analysis with Missing Data. Wiley; New York: 1987. [Google Scholar]
- 24.Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons, Inc.; New York: 1987. [Google Scholar]
- 25.Arbuckle JL. Amos 16.0 User’s Guide. SPSS; Chicago: 2007. [Google Scholar]
- 26.Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. Lawerence Erlbaum; Mahwah, NJ: 2004. pp. 61–122. [Google Scholar]
- 27.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 3rd ed. Harper Collins; New York: 1996. [Google Scholar]
- 28.Hu Mc, Bentler PM. Cutoff criteria for fit indices in co-variance structure analysis: conventional criteria versus new alternative. Struct Equ Model. 1999;6:1–55. [Google Scholar]
- 29.Gerlach KK, Cummings KM, Hyland A, et al. National Cancer Institute . Cigars: Health Effects and Trends. Smoking and Tobacco Control Monograph 9. U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health; Bethesda, MD: 1998. Trends in cigar consumption and smoking prevalence. NIH pub. no. 98-4302. [Google Scholar]
- 30.Doubeni CA, Li W, Fouayzi H, DiFranza JR. Perceived accessibility as a predictor of youth smoking. Ann Fam Med. 2008;6(4):323–330. doi: 10.1370/afm.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Delnevo CD. Smokers’ choice: what explains the steady growth of cigar use in the U.S.? Public Health Rep. 2006;121:116–121. doi: 10.1177/003335490612100203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soldz S, Dorsey E. Youth attitudes and beliefs toward alternative tobacco products: cigars, bidis, and kreteks. Health Educ Behav. 2005;32:549–566. doi: 10.1177/1090198105276219. [DOI] [PubMed] [Google Scholar]
- 33.Connolly GN, Alpert HR. Trends in the use of cigarettes and other tobacco products, 2000-2007. JAMA. 2008;299(22):2629–2630. doi: 10.1001/jama.299.22.2629. [DOI] [PubMed] [Google Scholar]
- 34.DiFranza JR, Savageau JA, Fletcher KE. Enforcement of underage sales laws as a predictor of daily smoking among adolescents – a national study. BMC Public Health. 2009;9:107. doi: 10.1186/1471-2458-9-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ross H, Blecher E, Yan L, Hyland A. Do cigarette prices motivate smokers to quit? New evidence from the ITC survey. Addiction. 2011;106(3):609–619. doi: 10.1111/j.1360-0443.2010.03192.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among U.S. males: findings from national surveys. Tob Control. 2010;19:104–109. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacol Biochem Behav. 2005;80(1):173–179. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 38.Sutfln EL, McCoy TP, Reboussin BA, et al. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115(1-2):131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brener ND, Kann L, McManus T, et al. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31:336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 40.Zullig KJ, Pun S, Patton JM, Ubbes VA. Reliability of the 2005 middle school youth risk behavior survey. J Adolesc Health. 2006;39(6):856–860. doi: 10.1016/j.jadohealth.2006.07.008. [DOI] [PubMed] [Google Scholar]