Abstract
Introduction
Alternative tobacco use among adolescents who smoke cigarettes is a growing public health concern, and evidence suggests that patterns of alternative tobacco use varies with respect to cigarette consumption and frequency of cigarette use. This study aimed to examine (a) whether variations in adolescent cigarette smoking and alternative tobacco use can be explained by underlying subtypes and (b) if these subtypes differ in their demographic and psychosocial characteristics.
Methods
Using data from the 2009 National Youth Tobacco Survey, latent class analysis (LCA) was used to identify patterns of cigarette smoking and alternative tobacco use among 2746 current (past 30-day) smokers. After identification, classes were analyzed using multinomial logistic regression to examine differences based on demographics and smoking-related characteristics.
Results
Four of the six latent classes identified (non-daily light smokers, chippers, chippers-Indulgent, intermittent smokers) reflected consumption, frequency, and history of cigarette use characteristics commonly attributed to light and intermittent smokers, and the remaining two classes (daily smokers, daily smokers-Indulgent) presented cigarette use behaviors commonly attributed to daily smokers. There were clear class differences in levels of alternative tobacco product use, demographics, and psychosocial characteristics.
Conclusions
Study findings are consistent with previous work demonstrating demographic and psychosocial differences between cigarette smokers based on their alternative tobacco use. The six latent classes identified highlight the importance of including measures of alternative tobacco use when characterizing adolescent cigarette smokers as well as recognizing and tailoring interventions toward these different groups of tobacco users.
Keywords: Latent class analysis, Tobacco, Alternative tobacco, Cigarette smoking, Adolescent
1. Introduction
While cigarette smoking among U.S. adolescents may be declining, many of these young Americans are also experimenting with alternative tobacco products (ATPs) like cigars, smokeless tobacco, and waterpipe/hookah (SAMHSA, 2011; Primack et al., 2008). This experimentation may contribute to the development of nicotine dependence among adolescents, and thus may contribute to tobacco-caused morbidity and mortality (2010 Surgeon General’s Report).
Interestingly, compared to adolescents who do not smoke cigarettes, higher rates of lifetime and past month ATP use are observed among adolescent cigarette smokers. For instance, in a study of 6090 Californian adolescents (Gilpin and Pierce, 2003), about 60% of current cigarette smokers compared to only 2.1% of never smokers had ever tried smokeless tobacco, cigars, or bidis. In a study of 1123 ninth graders in Virginia (Tercyak and Audrain, 2002), adolescent cigarette smokers were about 17 times more likely than non-smokers to use ATPs in the past month. Moreover, ATP use may be especially appealing to male adolescent cigarette smokers (Bombard et al., 2008).
Among adolescent cigarette smokers, ATP use may also vary with respect to cigarettes smoked per day (CPD) and number of days on which cigarettes are smoked. ATP use rates may be higher among light or intermittent tobacco smokers (LITS) than daily cigarette smokers (Cooper et al., 2010; Tomar et al., 2010; Rae Olmsted et al., 2011). Relative to daily cigarette smokers, daily use of smokeless tobacco is more prevalent among non-daily cigarette smokers (Tomar et al., 2010) and is the highest among cigarette smokers who average 10 or fewer CPD (Peterson et al., 2007). The type of ATP used may also be related to cigarette smoking: in one study, concomitant cigarette and smokeless tobacco users averaged significantly fewer cigarettes per day than concomitant cigarette and cigar users (Rae Olmsted et al., 2011). Taken together, these studies suggest that there may be systematic variations in cigarette and ATP consumption among U.S. adolescents.
Use of ATPs among adolescent cigarette smokers is worrisome, because, at least in adults, ATP use is associated with greater levels of nicotine dependence (Timberlake, 2008). Moreover, misperceptions about the health risks of ATPs may lead adolescents to overestimate their ability to quit, thus maintaining tobacco use and contributing to dependence in adulthood. Indeed, relative to adolescents who only smoke cigarettes, adolescent cigarette smokers who also use ATPs are more likely to be tobacco users as adults (Brook et al., 2008). In addition, cigarette smokers who use ATPs report more peer and tobacco-related influences than smokers who do not use them (Gilpin and Pierce, 2003) and these influences may also be related to adult tobacco use (Gilpin et al., 2007; Brooks et al., 2008).
Clearly, adolescent cigarette smokers are at risk for use of ATPs, and some more than others may have a higher likelihood of established tobacco use and dependence later in life. Unfortunately, we know very little about the smoking patterns and characteristics of adolescent cigarette and ATP users. Even less is known about the role of perceived social norms and tobacco-related influences that may help to account for the heterogeneity in adolescent tobacco use. Thus, this study aims to determine if the co-occurrence of cigarette and ATP use can be explained by underlying classifications of adolescents into subgroups based on similar cigarette smoking patterns. A secondary aim is to understand better how variations in adolescent smoking patterns might be explained by demographics; perceived norms and health risks; exposure to smoking- and tobacco-related influences; and dependence and quit efficacy related to smoking.
2. Methods
2.1. Population and sample
This study was based on a secondary analysis of the 2009 National Youth Tobacco Survey (NYTS). The NYTS is an evaluation tool developed by the Centers of Disease Control and Prevention (CDC) to estimate the tobacco-related attitudes and behaviors of a national sample of 6th through 12th graders enrolled in both public and private schools in the United States. A comprehensive description of the 2009 NYTS survey and methodology may be found here: http://www.cdc.gov/tobacco/datastatistics/surveys/nyts/. From the 22,697 students in the 2009 NYTS, 2746 reported past 30-day (current) cigarette smoking and were included in this study.
2.2. Measures
2.2.1. Latent class indicators
The selection of smoking indicators was guided by theoretical and empirical considerations about youth cigarette smoking and dependence (Coggins et al., 2009; Fagan and Rigotti, 2009; Husten, 2009; Shiffman, 2009). Eight observed variables for cigarette smoking and the use of alternative tobacco products (ATP) were chosen for the latent class analysis. In reference to current smoking, cigarette smoking frequency (“During the past 30 days, on how many days did you smoke cigarettes?”) and cigarette consumption (“During the past 30 days, on the days you smoked, how many cigarettes did you smoke per day?”) items were treated as ordinal variables. Responses for cigarette smoking frequency had six categories: 1–2 days; 3–5 days; 6–9 days; 10–19 days; 20–29 days; and all 30 days. Cigarette consumption per day had four responses: 1 or less; 2–5; 6–10; and 11 or more. Lifetime smoking (“About how many cigarettes have you smoked in your entire life?”) was coded as a nominal variable with the following categories: Less than 100 cigarettes and 100 or more cigarettes. Smoking persistence (“Now think back to 12 months ago; at this time last year, about how much were you smoking?”) was treated as a nominal variable having five categories: I have never smoked; I have smoked in my life, but I wasn’t smoking at this time last year; I smoked on some days this time last year; I smoked on most days this time last year; and I smoked everyday this time last year. In addition to these smoking indicators, we selected for analysis four binary indicators of past month ATP use: smokeless tobacco, cigars, bidis, and clove cigarettes. Waterpipe/hookah was not assessed in the 2009 NYTS.
2.2.2. Covariates
Several demographic and smoking-related variables were examined to help explain the heterogeneity in patterns of cigarette and ATP use. Demographic variables included in this study were: age; gender; race/ethnicity (White/European American, Black/African American, Hispanic/Latino, and multiple races/ethnicities or other); and school level (middle or high school). The smoking-related covariates included: smoking norms (“Do you think smoking cigarettes makes young people cool or fit in?”); smoking risk perceptions (“Do you think it is safe to smoke for only a year or two, as long as you quit after that?”); exposure to cigarette smoking in the home (“Does anyone who lives with you now smoke cigarettes?”); and with peers (How many of your four closest friends smoke cigarettes? (none-one or more)); a proxy for tobacco dependence (“How long can you go without smoking before you feel like you need a cigarette?”); and quit efficacy (“Do you think you would be able to quit smoking now if you wanted to?”).
2.3. Data analysis
Patterns of cigarette smoking and ATP use were generated using latent class analysis (LCA). Latent Gold 4.5 (Statistical Innovations Inc., 2008) was used to classify adolescents in terms of their tobacco use patterns. Given the exploratory nature of this study, the model-building strategy involved successively increasing the number of classes until a class solution that adequately fit the data was identified. The Bayesian Information Criterion (BIC) was used as a global fit index to determine the number of classes that parsimoniously explained associations between indicator variables. In addition, the bivariate residuals (BVRs) of candidate models were inspected to determine whether the local independence assumption was violated. Missing value analysis revealed that about 80% of the 2746 current smokers had complete data on all variables, with the largest percentage of missing data on two items related to tobacco dependence (14.9–17.1%). There was little evidence of systematic bias in item non-response based on adolescents’ age, gender, and race/ethnicity. Latent Gold allows for missing data using Full Information Likelihood (FIML) estimation. Thus, missing data were retained in the models under the assumption that these data were missing at random (MAR). Interpretability of latent class solutions was also an integral part of model selection criteria. Once an appropriate model was identified, the modal class assignments of members were treated as categorical (nominal) outcomes and analyzed using multinomial logistic regression. STATA 11 (StataCorp, 2009) was used to examine differences between classes based on demographics and smoking-related characteristics, as performed previously in two-stage approach studies (e.g., Agrawal et al., 2007, 2011; Heron et al., 2011; Sutfin et al., 2009).
3. Results
3.1. Descriptive characteristics
The majority of adolescent cigarette smokers were male (55.7%), White (56.4%), and enrolled in high school (80.4%). Table 1 presents summary information on rates of ATP use by sample characteristics. Overall, more than half of adolescent smokers (51.9%) reported past 30-day ATP use, with cigars (42.6%) and smokeless tobacco (20.8%) reported as most prevalent. On average, younger adolescents were more likely to report bidis (p’s < .01) and clove cigarette (p’s < .05) use than older adolescents. Male cigarette smokers were more likely than female smokers to report past 30-day ATP use (χ2 = 147.13, p < .01). A higher percentage of male smokers than females reported current use of smokeless tobacco (χ2 = 199.13, p < .01), cigars (χ2 = 90.33, p < .01), and cloves (χ2 = 4.87, p < .001). There were no significant differences between racial/ethnic groups in terms of overall ATP use; however, these groups did differ significantly in the type of ATP used. Whites were more likely than Blacks/African Americans (χ2 = 15.55, p < .01) and Hispanic/Latinos (χ2 = 23.43, p < .01) to use smokeless tobacco. And Hispanics/Latinos and other racial/ethnic groups were more likely than Whites to report past 30-day use of cigars (p’s < 05), bidis (p’s < .05), and cloves (p’s < .05). Past 30-day use of ATPs also differed in terms of school status; middle school students reported significantly higher use of bidis (χ2 = 54.45, p < .01) and cloves (χ2 = 9.43, p < .01) than high school students.
Table 1.
Prevalence of alternative tobacco product (ATP) use among youth cigarette smokers.
| Sample characteristics | N | SLT (%) | Cigars (%) | Bidis (%) | Cloves (%) | Any ATP (%) |
|---|---|---|---|---|---|---|
| Total | 2746 | 20.8 | 42.6 | 10.9 | 11.2 | 51.9 |
| Agea | ||||||
| 12 and younger | 119 | 33.3 | 54.8 | 31.8 | 28.7 | 62.2 |
| 13 years old | 171 | 20.0 | 43.0 | 19.7 | 12.5 | 53.3 |
| 14 years old | 318 | 15.7 | 38.8 | 12.9 | 9.8 | 48.8 |
| 15 years old | 406 | 21.1 | 42.3 | 11.1 | 11.2 | 51.5 |
| 16 years old | 544 | 19.8 | 42.5 | 8.8 | 10.5 | 52.1 |
| 17 years old | 652 | 20.6 | 41.0 | 7.9 | 9.1 | 50.5 |
| 18 and older | 533 | 22.8 | 44.6 | 8.5 | 11.5 | 53.5 |
| Gendera | ||||||
| Female | 1,210 | 8.4 | 32.5 | 9.8 | 9.6 | 38.9 |
| Male | 1,526 | 28.6 | 42.8 | 22.2 | 12.4 | 62.2 |
| Racea | ||||||
| White | 1,517 | 24.2 | 39.9 | 7.6 | 10.2 | 52.2 |
| Black | 276 | 12.9 | 45.5 | 12.9 | 9.7 | 49.6 |
| Hispanic/Latino | 761 | 15.2 | 46.3 | 16.4 | 13.4 | 52.6 |
| Multiple races/other | 132 | 27.4 | 45.7 | 17.5 | 14.8 | 50.0 |
| School levela | ||||||
| Middle school | 535 | 22.6 | 44.6 | 20.0 | 14.8 | 54.5 |
| High school | 2,199 | 20.3 | 42.1 | 8.6 | 10.1 | 51.2 |
Significant differences observed between percentages of youth smokers. Some categories do not add to the total due to missing responses.
3.2. Latent class model
A series of latent class models were estimated to identify subgroups of adolescent cigarette smokers who currently use smokeless tobacco, cigars, bidis, or clove cigarettes. The overall fit of the model improved substantially from the one-class model to six-class model (37,606–31,716), but deteriorated with the seven (31,730) and eight-class models (31,742). Based on the conditional bootstrap LR results, comparing the k-class with the k-1class model, there was strong evidence of model improvement until reaching six classes. Diagnostic tests detected high residual correlations between three pairs of model indicators: number of days smoked and number of cpd (BVR = 3.92); number of cigarettes smoked in lifetime and smoking persistence (BVR = 3.76); and past 30-day smokeless tobacco use and cigar use (BVR = 6.44). To reduce local dependence among these items, the six-class model was adjusted allowing for residual dependence between these indicators (Magidson and Vermunt, 2000). Relaxing this restriction (i.e., the inclusion of a direct effect parameter) for the six-class model resulted in significant model improvement over the initial six-class model (ΔL2 − 3405.40 – 3334.58 − 70.82, p < .001) and relatively low classification error (11.34%). Considering model fit and parsimony, the six-class model with local dependence was chosen for additional analyses.
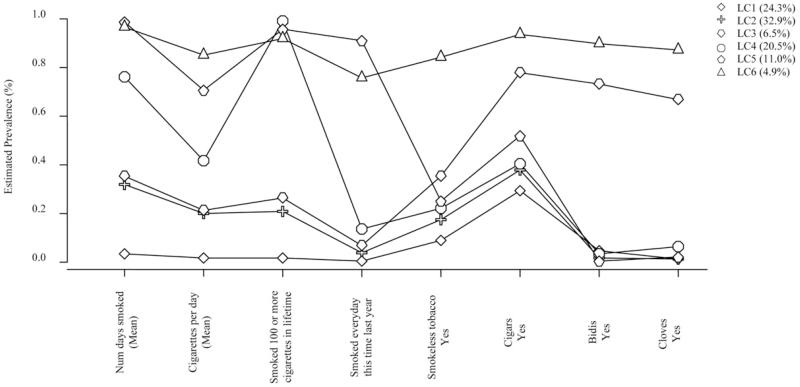
Fig. 1 presents the estimated prevalence rates for cigarette smoking and ATP use. Four of the six latent classes (LC1–LC4) reflected consumption, frequency, and history of cigarette use characteristics generally consistent with pre-defined LITS (e.g.,Shiffman, 2009). The remaining two classes (LC5 and LC6) presented behaviors attributed to daily smokers. Past 30-day ATP use was unevenly distributed across classes, with adolescents who reported more recent ATP use being assigned to LC3 and LC6 (described in more detail below).
Fig. 1.
Estimated prevalence rates for cigarette and alternative tobacco product use among adolescents.
Table 2 presents the estimated probabilities of smoking-related characteristics for each latent class. The first latent class (LC1, 24.3%) was comprised of non-daily, light smokers who reported smoking 5 or fewer cpd (99.9%) for no more than 5 days/month (98.9%). The majority of adolescents in this class were not smoking one year ago (56.2%), and the most smoked fewer than 100 cigarettes in their lifetime (98.5%). Non-daily, light smokers also reported the lowest ATP use compared to the other latent classes; however, about one-third (28.9%) of adolescent cigarette smokers assigned to this class reported past 30-day cigar use.
Table 2.
Probabilities of smoking-related characteristics by latent classes of smokers.
| Sample characteristics | LC1 non-daily light smokers (N=660) |
LC2 chippers (N = 906) |
LC3 chippers-lndulgent (N=178) |
LC4 intermittent smokers (N =564) |
LC5 daily smokers (N=303) |
LC6 daily smokers-lndulgent (N =135) |
|---|---|---|---|---|---|---|
| Class size | 24.3 | 32.9 | 6.5 | 20.5 | 11.0 | 4.9 |
| Number of days smoked | ||||||
| 1–2 days | 85.7 | 22.8 | 19.4 | <1.0 | <1.0 | <1.0 |
| 3–5 days | 13.2 | 31.2 | 29.6 | 3.4 | <1.0 | <1.0 |
| 6–9 days | <1.0 | 19.7 | 20.4 | 7.6 | <1.0 | <1.0 |
| 10–19 days | <1.0 | 17.8 | 20.3 | 24.4 | <1.0 | 1.9 |
| 20–29 days | <1.0 | 6.4 | 8.1 | 31.7 | 6.8 | 14.3 |
| All 30 days | <1.0 | 1.7 | 2.4 | 32.0 | 92.7 | 83.5 |
| Cigarettes smoked/day | ||||||
| 1 or less cigarettes | 95.8 | 45.6 | 42.8 | 12.1 | 1.4 | <1.0 |
| 2–5 cigarettes | 4.1 | 49.9 | 52.0 | 59.3 | 26.7 | 10.0 |
| 6–10 cigarettes | <1.0 | 3.9 | 4.6 | 20.2 | 31.2 | 24.1 |
| 11+ cigarettes | <1.0 | <1.0 | <1.0 | 8.3 | 40.5 | 65.5 |
| Lifetime use | ||||||
| Less than 100 cigarettes | 98.5 | 79.4 | 73.8 | 1.1 | 4.6 | 8.5 |
| 100 or more cigarettes | 1.5 | 20.6 | 26.2 | 98.9 | 95.4 | 91.5 |
| Smoking persistence | ||||||
| Never smoked (log error) | 11.8 | 3.2 | 3.7 | 3.2 | <1.0 | <1.0 |
| Smoked, but not last year | 56.2 | 29.2 | 19.2 | 15.5 | <1.0 | 5.2 |
| Some days last year | 31.6 | 53.8 | 51.1 | 30.7 | <1.0 | 3.6 |
| Most days last year | <1.0 | 10.4 | 19.6 | 37.3 | 9.0 | 12.6 |
| Every day last year | <1.0 | 3.4 | 6.4 | 13.3 | 90.7 | 75.6 |
| Past 30-day ATP use | ||||||
| Smokeless tobacco | 8.6 | 17.3 | 35.1 | 21.8 | 25.1 | 83.8 |
| Cigars | 28.9 | 37.5 | 77.5 | 40.0 | 51.7 | 93.5 |
| Bidis | 4.4 | 1.5 | 73.2 | 3.4 | <1.0 | 89.6 |
| Cloves | 1.1 | 1.3 | 66.8 | 5.9 | 1.9 | 86.9 |
| Household smoking | ||||||
| Yes | 47.6 | 52.2 | 51.5 | 57.9 | 66.6 | 68.9 |
| Peer smoking | ||||||
| 1 or more | 65.6 | 71.2 | 85.3 | 82.8 | 80.6 | 85.3 |
| Perceived smoking norms | ||||||
| Smoke to be cool/fit in | 18.1 | 22.3 | 35.6 | 17.9 | 14.4 | 50.8 |
| Perceived smoking risks | ||||||
| Okay to smoke 1–2 years | 20.1 | 27.9 | 45.9 | 29.6 | 27.4 | 48.1 |
| Tobacco dependence | ||||||
| Smoke ≤3h | <1.0 | 3.9 | 17.6 | 15.3 | 43.6 | 69.9 |
| Quit efficacy | ||||||
| Ability to stop smoking | 87.3 | 77.8 | 71.5 | 73.5 | 53.9 | 42.3 |
The second (LC2, 32.9%) and third (LC3, 6.5%) latent classes were comprised of light smokers who presented features of cigarette use similar to chippers (see Shiffman, 1989). Adolescents assigned to these classes smoked one to five cpd (LC2, 95.5%; LC3, 94.8%) on fewer than 30 days during the past month (LC2, 97.9%; LC3, 97.8%). Although the majority of youth in these classes were not established cigarette smokers as referenced by Shiffman (adult cigarette smokers; 1989), a substantial proportion of youth in each class reported smoking on some or most of the days a year earlier (LC2, 64.2%; LC3, 70.7%). In terms of past 30-day ATP use, a modest percentage of adolescent cigarette smokers assigned to LC2 reported concurrent cigar (37.5%) and smokeless tobacco use (17.3%). By contrast, a considerably higher percentage of cigarette smokers assigned to LC3 reported past 30-day ATP use: cigars (77.5%); smokeless tobacco (35.1%); bidis (73.2%); and clove cigarettes (66.8%). Considering the shared and unique cigarette and ATP use features of these classes, we have characterized LC3 as a subtype, chippers-Indulgent.
The fourth latent class (LC4, 20.5%), intermittent smokers, reported smoking 2–10 cpd (79.5%) on less than 30 days during the past month (67.1%). Virtually all adolescents assigned to this class had smoked 100 or more cigarettes in their lifetime (98.9%) with most smoking on some or most days the year prior (68.0%). More than one-third of intermittent smokers used cigars in the past month (40.0%) followed by smokeless tobacco (21.8%), bidis (3.4%) and clove cigarettes (5.9%).
The remaining two latent classes (LC5, 11.0%; LC6, 4.9%) presented cigarette consumption and frequency of use characteristics consistent with daily cigarette smokers. Adolescents assigned to these classes smoked 11 or more cpd (LC5, 40.5%; LC6, 65.5%) during all 30 days the past month (92.7% and 83.5%, respectively). In both classes, almost all adolescents were established cigarette smokers (100 or more cigarettes in lifetime: LC5, 95.4%; LC6, 91.5%) and had been for at least one year (smoked everyday last year: LC5, 90.7%; LC6, 75.6%). Despite similarities in cigarette use, adolescents assigned to LC5 and LC6 differed considerably in terms of past 30-day ATP use. There were a greater proportion of concurrent cigarette and ATP users assigned to LC6 than LC5 for smokeless tobacco (83.8% vs. 25.1%), cigars (93.5% vs. 51.7%), bidis (89.6% vs. <1.0%), and clove cigarettes (86.9% vs. 1.9%). Based on cigarette and ATP characteristics among these classes, we have characterized LC6 as a subtype, daily smokers-Indulgent.
3.3. Demographic and smoking-related covariates
Table 3 presents the multinomial regression results based on differences between latent classes for demographic and smoking-related characteristics. Theoretical perspectives on cigarette smoking and dependence (e.g., Shiffman, 2009) informed our decision to use non-daily light smokers as the reference group for the subsequent analysis. Relative to light, non-daily smokers (LC1), chippers (LC2) were more likely to be in high school (p < .01). Chippers and its subtype, chippers-Indulgent (LC3), were 1.14–1.52 times more likely than non-daily light smokers to have peers who smoked cigarettes (p’s < .01); 1.09–1.38 times more likely to perceive smoking as cool (p’s < .01); and 1.16–1.51 times more likely to perceive smoking one or two years before quitting as not risky (p’s < .01). With respect to dependence and quit efficacy, chippers and chippers-Indulgent compared to non-daily light smokers reported a shorter time between cigarettes (p’s < .05) and less confidence in their ability to quit smoking (p’s < .01).
Table 3.
Multinomial logistic regression model for latent classes by demographics and smoking-related characteristics.
| Sample characteristics | Units | LC2 chippers (N = 906) |
P ≤ | LC3 chippers-lndulgent (N =178) |
P ≤ | LC4 intermittent smokers (N=564) |
P ≤ | LC5 daily smokers (N=303) |
P ≤ | LC6 daily smokers-lndulgent (N =135) |
P ≤ |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||||
| <16 | Referent | ||||||||||
| ≥16 | Years | 1.02 (0.98,1.05) | .26 | 0.96(0.91,1.02) | .22 | 1.16(1.11, 1.20) | .01 | 1.22(1.15,1.28) | .01 | 0.99 (0.93,1.05) | .81 |
| Gender | |||||||||||
| Female | Referent | Referent | |||||||||
| Male | No/Yes | 1.11 (0.91,1.36) | .28 | 1.49(1.05, 2.12) | .03 | 1.12(0.90,1.40) | .28 | 1.49(1.13,1.96) | .01 | 2.06(1.38,3.06) | .01 |
| Race/ethnicity | |||||||||||
| White | Referent | Referent | |||||||||
| Black | No/Yes | 0.90 (0.65,1.24) | .52 | 0.81 (0.44,1.48) | .49 | 0.36 (0.24, 0.54) | .01 | 0.38 (0.23, 0.64) | .01 | 1.04 (0.55,1.98) | .88 |
| Hispanic/Latino | No/Yes | 0.80 (0.64,1.01) | .06 | 1.16(0.79,1.70) | .42 | 0.33 (0.25, 0.44) | .01 | 0.31 (0.22, 0.45) | .01 | 1.32(0.86, 2.01) | .19 |
| Multiple races/other | No/Yes | 0.92 (0.56,1.50) | .74 | 1.47(0.69,3.12) | .31 | 0.68(0.39,1.16) | .16 | 0.59 (0.30, 1.18) | .14 | 2.85(1.42, 5.70) | .01 |
| School level | |||||||||||
| Middle school | Referent | Referent | |||||||||
| High school | No/Yes | 1.36(1.07,1.72) | .01 | 0.80 (0.55,1.16) | .25 | 3.96 (2.82, 5.57) | .01 | 3.35 (2.20, 5.08) | .01 | 0.67 (0.45,1.00) | .05 |
| Smoking influences | |||||||||||
| Household smoking | No/Yes | 1.20 (0.98,1.47) | .06 | 1.13(0.80,1.61) | .46 | 1.52(1.21, 1.90) | .01 | 2.34(1.75,3.13) | .01 | 2.39(1.60,3.56) | .01 |
| Peer smoking | 0–1 | 1.14(1.07,1.21) | .01 | 1.52(1.36,1.70) | .01 | 1.53 (1.42, 1.64) | .01 | 1.62(1.48,1.78) | .01 | 1.88(1.64, 2.17) | .01 |
| Perceived smoking norms | |||||||||||
| Smoke to be cool/fit in | 0–1 | 1.09(1.00,1.18) | .03 | 1.38(1.22,1.57) | .01 | 1.00(0.91,1.10) | .92 | 0.92 (0.81,1.04) | .22 | 1.67(1.47,1.91) | .01 |
| Perceived smoking risks | |||||||||||
| Okay to smoke 1–2 years | 0–1 | 1.16(1.07,1.26) | .01 | 1.51 (1.34,1.71) | .01 | 1.19(1.09, 1.30) | .01 | 1.14(1.02,1.26) | .01 | 1.59(1.39,1.81) | .01 |
| Tobacco dependence | |||||||||||
| Less than 3 h | 0–1 | 1.16(1.00,1.35) | .05 | 1.66(1.42,1.94) | .01 | 1.58(1.38, 1.82) | .01 | 2.14(1.86, 2.46) | .01 | 2.67(2.29,3.11) | .01 |
| Quit efficacy | |||||||||||
| Ability to stop smoking | No/Yes | 0.27 (0.15, 0.50) | .01 | 0.10 (0.05, 0.20) | .01 | 0.09(0.05, 0.17) | .01 | 0.03 (0.01, 0.06) | .01 | 0.02 (0.01,0.04) | .01 |
Referent category = Non-daily, light smokers (N=660).
Intermittent smokers (LC4) were more likely than non-daily light smokers to be older (p < .01), White (p’s < .01), and enrolled in high school (p < .01). Like chippers and chippers-Indulgent, these adolescents were 1.53 times more likely than non-daily light smokers to report having more friends who smoked (p < .01). Intermittent smokers were not likely to smoke to be cool or fit in, (p > .05); however, they were significantly more likely than non-daily light smokers to perceive smoking one or two years as okay (p < .01). Intermittent smokers were less likely than non-daily light smokers to go for long periods without smoking a cigarette (p < .01) and significantly less likely to report quit efficacy (p < .01).
Daily cigarette smokers (LC5), like intermittent smokers, were more likely than non-daily light smokers to be older (p < .01), White (p’s < .01), and in high school (p < .01). Daily smokers-Indulgent (LC6), on the other hand, were 2.85 times more likely than non-daily light smokers to belong to a multi race/other ethnic group compared to White (p < .01). Compared to non-daily light smokers, daily smokers and daily smokers-Indulgent were 1.62–2.39 times more likely to report household and peer smoking (p’s < .01). Daily smokers-Indulgent were 1.67 times more likely than non-daily light smokers to perceive cigarettes as making a person look cool or fit in (p < .01); importantly, daily smokers’ perceptions did not significantly differ from non-daily light smokers (p > .05). Both daily smokers types compared to non-daily light smokers reported less time between cigarettes (p < .01) and lower confidence in their ability to quit smoking (p’s < .01).
3.4. Comparisons between chippers and daily smokers and their subtypes
Additional comparisons were performed to understand better the differences between chippers and daily smokers and their respective subtypes (Table 4). Chippers-Indulgent, compared to chippers, were less likely to be 16 years of age and older (p < .05), and less likely to be enrolled in high school grades (p < .01). With respect to smoking-related influences, chippers-Indulgent were 1.33 times more likely than chippers to have friends who smoked (p < .01). In addition, chippers-Indulgent were 1.27–1.30 times more likely than their smoking counterparts to believe smoking is cool, and to think it is okay to smoke 1–2 years before quitting (p’s < .01). In relation to tobacco dependence, chippers-Indulgent compared to chippers reported less time between cigarettes (p < .01) and less confidence in their ability to quit smoking (p < .01).
Table 4.
Logistic regression models for Chippers and Daily smoker subtypes.
| Sample characteristics | Units | LC3a chippers-lndulgent (N =178) | P ≤ | LC6b daily smokers-Indulgent (N = 135) | P ≤ |
|---|---|---|---|---|---|
| Age | |||||
| <16 | Referent | Referent | |||
| ≥16 | Years | 0.94 (0.89,1.00) | .05 | 0.81 (0.75, 0.87) | .01 |
| Gender | |||||
| Female | Referent | Referent | |||
| Male | No/Yes | 1.33 (0.94,1.89) | .09 | 1.38 (0.89, 2.13) | .14 |
| Race/ethnicity | |||||
| White | Referent | Referent | |||
| Black | No/Yes | 0.90 (0.49,1.63) | .73 | 2.71 (1.29, 5.70) | .01 |
| Hispanic/Latino | No/Yes | 1.44 (0.99, 2.10) | .06 | 4.16(2.53, 6.83) | .01 |
| Multiple races/other | No/Yes | 1.59 (0.76,3.34) | .21 | 4.75 (2.07, 10.89) | .01 |
| School level | |||||
| Middle school | Referent | Referent | |||
| High school | No/Yes | 0.58 (0.40, 0.85) | .01 | 0.20 (0.11,0.34) | .01 |
| Smoking influences | |||||
| Household smoking | No/Yes | 0.94 (0.67,1.32) | .73 | 1.01 (0.65, 1.59) | .93 |
| Peer smoking | 0–1 | 1.33(1.19,1.48) | .01 | 1.16(1.00, 1.35) | .05 |
| Perceived smoking norms | |||||
| Smoking to be cool/fit in | 0–1 | 1.27(1.12,1.43) | .01 | 1.80(1.54, 2.11) | .01 |
| Perceived smoking risks | |||||
| Okay to smoke 1–2 years | 0–1 | 1.30(1.15,1.46) | .01 | 1.39(1.21, 1.61) | .01 |
| Tobacco dependence | |||||
| Less than 3 h | 0–1 | 1.43(1.28,1.59) | .01 | 1.24(1.14, 1.36) | .01 |
| Quit efficacy | |||||
| Ability to stop smoking | No/Yes | 0.37 (0.23, 0.60) | .01 | 0.59 (0.39, 0.90) | .01 |
Referent category = LC2; chippers (N=906).
Referent category = LC5, daily smokers (N=303).
In relation to daily smokers and its subtype, daily smokers-Indulgent were less likely to be 16 years of age or older (p < .01) and to be in high school (p < .01). Compared to daily smokers, daily-Indulgent smokers were 2.71–4.75 times more likely to be a racial/ethnic minority (p’s < .01). Daily smokers-Indulgent were more likely than daily smokers to report peer smoking (p < .01), and 1.39–1.80 times more likely to perceive cigarette smoking as cool (p < .01) and believe it was okay to smoke one to two years before quitting (p’s < .01). In terms of tobacco dependence, daily smokers-Indulgent compared to daily smokers needed to smoke cigarettes more frequently during the day (p < .01) and lacked confidence in their ability to stop smoking if they wanted too (p < .01).
4. Discussion
Nationally, about 10% of adolescents (ages 12–17) report past month use of cigarettes (SAMHSA, 2011). However, only half of these smokers use cigarettes exclusively; 46.1% of adolescent cigarette smokers consume ATPs such as smokeless tobacco, cigars, bidis, and clove cigarettes (Bombard et al., 2008); water-pipe (hookah) use is also popular (e.g., Johnston et al., 2011). Few studies have investigated concurrent tobacco use in adolescence (e.g., Bombard et al., 2008; Brooks et al., 2008; Everett et al., 2000; Gilpin and Pierce, 2003; Tercyak and Audrain, 2002), and no studies have examined systematic variations in the combined use of these tobacco products. In this study, the evaluation of concomitant cigarette and ATP use has yielded important information on individual differences related to adolescents’ smoking history and smoking-related influences, norms, and perceptions. This study also provides insight on how features of dependence may be related to patterns of concurrent tobacco use in adolescence.
4.1. Prevalence of alternative tobacco use among adolescent subpopulations
Consistent with previous work, 51.9% of the adolescent cigarette smokers surveyed here used ATPs during the past month (e.g.,Gilpin and Pierce, 2003; Rigotti et al., 2000), and cigars were the most prevalent ATP used at 42.9% (e.g., Tercyak and Audrain, 2002; Gilpin and Pierce, 2003; Bombard et al., 2008). Moreover, adolescent male smokers were significantly more likely than females to report use of any ATP, smokeless tobacco alone and cigars alone (e.g., Backinger et al., 2008; Bombard et al., 2008), and Whites were significantly more likely than Blacks/African Americans and Hispanic/Latinos to use smokeless tobacco (e.g., Rigotti et al., 2000). For bidis and clove cigarettes, rates were similar to those reported previously, and relatively equal between adolescent males and females (e.g., Gilpin and Pierce, 2003). This latter finding is possibly associated with the widespread appeal of flavored tobacco and/or experimentation with novel products (e.g., Leatherdale et al., 2011; Soldz and Dorsey, 2005). Although recent legislation has banned the sale and use of bidis and clove cigarettes (Family Smoking Prevention and Tobacco Control Act, 2009), former users of these products may be attracted to ATPs with similar sensory characteristics such as roll your own (RYO), those advertised as ‘natural’ and ‘organic’, and/or waterpipes (e.g., Martinasek et al., 2011; Young et al., 2006). Importantly, use of these tobacco products, independent of concurrent cigarette smoking, likely poses substantial health risks (Aitken et al., 2009; O’Connor et al., 2007; Raad et al., 2011).
4.2. Systematic variations in the concomitant use of cigarettes and alternative tobacco products
In this study, six classes of adolescent smokers with distinct patterns of cigarette and ATP use patterns were identified. Of these six classes, four (representing 84.2% of adolescent cigarette smokers) were characterized by their light and intermittent cigarette smoking. These classifications are generally consistent with frameworks on cigarette smoking that include as defining features variables such as consumption, frequency, and history (e.g., Husten, 2009; Shiffman, 2009). Nonetheless, debate continues about the characterization of various smoker types, particularly those labeled as “light,” “chipper,” or “intermittent” (see Husten, 2009).
Up to a third of U.S. smokers maintain non-daily and/or light cigarette smoking patterns (NSDUH, 2009). Consequently, the classification of smokers primarily on the basis of cigarette consumption and frequency has been questioned. Results reported here support this idea, as there tended to be more variation within LITS and daily smoker subgroups than between these classifications. For example, probabilities for ATP use were much more disparate between chippers and chippers-Indulgent than between chippers and daily smokers (estimated probability differences ranging from 0.17–0.71 vs. 0.06–0.14, respectively). Additionally, these findings are not consistent with previous work from adults showing that rates of ATP are higher for LITS than for daily smokers (Tomar et al., 2010; Rae Olmsted et al., 2011) and among those who smoke fewer than 10 cpd (Cooper et al., 2010).
4.3. Psychosocial characteristics of latent classes of youth smokers
Relative to non-daily light smokers, all other classes were more likely to have peers who smoked, and three classes (i.e., Intermittent, daily, and daily-Indulgent smokers) were more likely to report household smoking. Peer smoking is a well-established predictor of cigarette smoking experimentation and escalation in adolescents (e.g., Alexander et al., 2001; Ali and Dwyer, 2009; Choi et al., 1997). Use of ATPs such as waterpipes (e.g., Smith-Simone et al., 2008) and smokeless tobacco (e.g., Morrell et al., 2005) has also been associated with peer use of these products. Chippers and daily smokers were more likely to believe smoking is cool compared to non-daily light smokers. Several studies among U.S. adolescents (Carpenter et al., 2009; Kandra et al., 2011) have shown a positive relationship between the perception that cigarette smoking is cool and current cigarette smoking status or smoking susceptibility. Perceptions of waterpipe smoking “coolness” have also been shown to be a predictor of current waterpipe use (Jordan and Delnevo, 2010). Overall, compared to non-daily light smokers, the most psychosocial characteristic differences were observed for the indulgent smoker groups. Furthermore, when comparing daily smoker and chipper classes to their Indulgent counterparts, results show that Indulgent individuals tended to be younger; a member of a racial/ethnic group; engaged in higher levels of ATP; and more likely to endorse risky perceptions of smoking.
4.4. Dependence among alternative tobacco users
Of primary concern is whether a greater risk of dependence is incurred when cigarette smokers also use ATPs (e.g., LC3 and LC6 subgroups). Although not directly assessed in this study, chippers-Indulgent and daily smokers-Indulgent (i.e., higher prevalence of ATP use) reported features consistent with nicotine dependence profiles. A positive association between ATP use and likelihood of nicotine dependence in both light (e.g., <1 pack/week) and heavy (e.g., ≥10 cpd) smoker types has been reported in previous studies (Donny and Dierker, 2007; Timberlake, 2008). Possible explanatory factors for this relationship include those psychosocial factors revealed here and elsewhere (e.g., number of peers who smoke;Gilpin et al., 2007; Brooks et al., 2008), as well as other factors such as increased exposure to nicotine among polytobacco users (Wetter et al., 2002). Indeed, like cigarettes, nicotine is delivered to the user by cigars (Pechacek et al., 1985), smokeless tobacco (Benowitz et al., 1988), bidis (Malson et al., 2002), kreteks (Malson et al., 2003), and waterpipe (Blank et al., 2011; Cobb et al., 2011). Thus, individuals who combine use of cigarettes and ATP may increase their exposure to nicotine relative to individuals who use only one of these tobacco products, placing themselves at greater risk for nicotine dependence. This speculation is supported by the observation that polytobacco users are less likely to attempt cessation and/or maintain abstinence compared to users of a single product (e.g., Rodu et al., 2003; Wetter et al., 2002). Together, this work highlights the importance of understanding the unique features of dependence among users of multiple tobacco products.
4.5. Study limitations
The 2009 NYTS did not assess use of some emerging tobacco products adequately (e.g., Black and Mild cigarillos) or at all (e.g., waterpipe). Adolescents commonly refer to cigarillos only by brand name (e.g., “Black and Milds”; Yerger et al., 2001), and cigar use among this population may be misreported by surveys that fail to differentiate product types (Nasim et al., 2012; Terchek et al., 2009). Tobacco smoking using a waterpipe is now especially popular among adolescents, with some college samples reporting up to 48% ever use and up to 20% past month use (e.g., Eissenberg et al., 2008; Primack et al., 2008; Sutfin et al., 2011). Moreover, many of these waterpipe users also smoke cigarettes (e.g., 52% inSutfin et al., 2011). The model modifications may well be sample dependent due to the post hoc nature of this procedure. Also, future studies may wish to explore whether concomitant tobacco use patterns are consistent across gender, race/ethnicity, and the lifespan (e.g., adolescence vs. young adulthood). Finally, the population sampled (youth who attended public or private schools) and the cross-sectional nature of this survey limit the inferences made.
4.6. Conclusions
Study findings are consistent with previous work demonstrating demographic and psychosocial differences between cigarette smokers based on their ATP use (e.g., Backinger et al., 2008; Bombard et al., 2008; Gilpin and Pierce, 2003). Together, these studies highlight the importance of including ATP in the characterization of cigarette smokers. Such an approach has implications for education (addressing misperceptions and appropriate cessation efforts) and public health (measuring nicotine/tobacco exposure comprehensively and evaluating dependence), consequently reducing the increased risk of morbidity and mortality (Accortt et al., 2002; Ferrence and Stephens, 2000) associated with concurrent tobacco use.
Acknowledgements
We would like to thank Levent Dumenci Ph.D., Associate Professor, Department of Social and Behavioral Health at Virginia Commonwealth University for his comments on this paper.
Role of funding source
Support for the first author was provided by the National Institute on Minority Health and Health Disparities (NIMHD) and the Virginia Foundation for Healthy Youth (VFHY). Additional funding support was provided by the National Cancer Institute (1R01CA120142-01A2).
Footnotes
Conflict of interest
No conflict declared.
Contributors
Author Nasim designed the study and undertook the statistical analysis. Authors Nasim and Blank wrote the first draft of the manuscript. Authors Cobb and Eissenberg provided feedback and edits to the manuscript. All authors contributed to and have approved the final manuscript.
References
- Accortt NA, Waterbor JW, Beall C, Howard G. Chronic disease mortality in a cohort of smokeless tobacco users. Am. J. Epidemiol. 2002;156:730–737. doi: 10.1093/aje/kwf106. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on alcohol and related conditions. Addiction. 2007;102:94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Scherrer JF, Pergadia ML, Lynskey MT, Madden PA, Sartor CE, Grant JD, Duncan AE, Haber JR, Jacob T, Bucholz KK, Xian H. A latent class analysis of DSM-IV and Fagerstrom (FTND) criteria for nicotine dependence. Nicotine Tob. Res. 2011;13:972–981. doi: 10.1093/ntr/ntr105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aitken CK, Fry TR, Farrell L, Pellegrini B. Smokers of illicit tobacco report significantly worse health than other smokers. Nicotine Tob. Res. 2009;11:996–1001. doi: 10.1093/ntr/ntp102. [DOI] [PubMed] [Google Scholar]
- Alexander C, Piazza M, Mekos D, Valente T. Peers, schools, and adolescent cigarette smoking. J Adol Health. 2001;29:22–30. doi: 10.1016/s1054-139x(01)00210-5. [DOI] [PubMed] [Google Scholar]
- Ali MM, Dwyer DS. Estimating peer effects in adolescent smoking behavior: A longitudinal analysis. J Adol Health. 2009;45:402–408. doi: 10.1016/j.jadohealth.2009.02.004. [DOI] [PubMed] [Google Scholar]
- Backinger CL, Fagan P, O’Connell ME, Grana R, Lawrence D, Bishop JA, Gibson JT. Use of other tobacco products among U.S. adult cigarette smokers: prevalence, trends and correlates. Addict. Behav. 2008;33:472–489. doi: 10.1016/j.addbeh.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benowitz NL, Porchet H, Sheiner L, Jacob P., III Nicotine absorption and cardiovascular effects with smokeless tobacco use: comparison with cigarettes and nicotine gum. Clin. Pharmacol. Ther. 1988;44:23–28. doi: 10.1038/clpt.1988.107. [DOI] [PubMed] [Google Scholar]
- Blank MD, Cobb CO, Kilgalen B, Austin J, Weaver MF, Shihadeh A, Eissenberg T. Acute effects of waterpipe tobacco smoking: a double-blind, placebo-control study. Drug Alcohol Depend. 2011;116:102–109. doi: 10.1016/j.drugalcdep.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bombard JM, Rock VJ, Pederson LL, Asman KJ. Monitoring polytobacco use among adolescents: do cigarette smokers use other forms of tobacco? Nicotine Tob. Res. 2008;10:1581–1589. doi: 10.1080/14622200802412887. [DOI] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Whiteman M, Cohen P, Finch SJ. Developmental trajectories of cigarette smoking from adolescence to the early thirties: personality and behavioral risk factors. Nicotine Tob. Res. 2008;10:1283–1291. doi: 10.1080/14622200802238993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks A, Larkin EMG, Kishore S, Frank S. Cigars, cigarettes, and adolescents. Am. J. Health Behav. 2008;32:640–649. doi: 10.5555/ajhb.2008.32.6.640. [DOI] [PubMed] [Google Scholar]
- Carpenter MJ, Garrett-Mayer E, Vitoc C, Cartmell K, Biggers S, Alberg AJ. Adolescent nondaily smokers: favorable views of tobacco yet receptive to cessation. Nicotine Tob. Res. 2009;11:348–355. doi: 10.1093/ntr/ntp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi WS, Pierce JP, Gilpin EA, Farkas AJ, Berry CC. Which adolescent experimenters progress to established smoking in the United States? Am J Prev Med. 1997;13:385–391. [PubMed] [Google Scholar]
- Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob. Res. 2011;13:78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coggins CR, Murrelle EL, Carchman RA, Heidbreder C. Light and intermittent cigarette smokers: a review (1989–2009) Psychopharmacology. 2009;207:343–363. doi: 10.1007/s00213-009-1675-4. [DOI] [PubMed] [Google Scholar]
- Cooper TV, Taylor T, Murray A, DeBon MW, Vander Weg MW, Klesges RC, Talcott GW. Differences between intermittent and light daily smokers in a population of U.S. military recruits. Nicotine Tob. Res. 2010;12:465–473. doi: 10.1093/ntr/ntq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Dierker LC. The absence of DSM-IV nicotine dependence in moderate-to-heavy daily smokers. Drug Alcohol Depend. 2007;89:93–96. doi: 10.1016/j.drugalcdep.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eissenberg T, Ward KD, Smith-Simone S, Maziak W. Waterpipe tobacco smoking on a U.S. college campus: prevalence and correlates. J. Adolesc. Health. 2008;42:526–529. doi: 10.1016/j.jadohealth.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett SA, Malarcher AM, Sharp DJ, Husten CG, Giovino GA. Relationship between cigarette, smokeless tobacco, and cigar use, and other health risk behaviors among U.S. high school students. J. Sch. Health. 2000;70:234–240. doi: 10.1111/j.1746-1561.2000.tb07424.x. [DOI] [PubMed] [Google Scholar]
- Fagan P, Rigotti NA. Light and intermittent smoking: the road less traveled. Nicotine Tob. Res. 2009;11:107–110. doi: 10.1093/ntr/ntn015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrence R, Stephens T. Monitoring tobacco use in Canada: the need for a surveillance strategy. Chronic Dis. Can. 2000;21:50–53. [PubMed] [Google Scholar]
- Gilpin EA, Pierce JP. Concurrent use of tobacco products by California adolescents. Prev. Med. 2003;36:575–584. doi: 10.1016/s0091-7435(02)00064-6. [DOI] [PubMed] [Google Scholar]
- Gilpin EA, White MM, Messer K, Pierce JP. Receptivity to tobacco advertising and promotions among young adolescents as a predictor of established smoking in young adulthood. Am. J. Public Health. 2007;97:1489–1495. doi: 10.2105/AJPH.2005.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron J, Hickman M, Macleod J, Munafo MR. Characterizing patterns of smoking initiation in adolescence: comparison of methods for dealing with missing data. Nicotine Tob. Res. 2011;13:1266–1275. doi: 10.1093/ntr/ntr161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husten CG. How should we define light or intermittent smoking? Does it matter? Nicotine Tob. Res. 2009;11:111–121. doi: 10.1093/ntr/ntp010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Overview of Key Findings. Institute for Social Research, The University of Michigan; Ann Arbor: 2011. 2010. Monitoring the Future: National Results on Adolescent Drug Use. [Google Scholar]
- Jordan HM, Delnevo CD. Emerging tobacco products: hookah use among New Jersey youth. Prev. Med. 2010;51:394–396. doi: 10.1016/j.ypmed.2010.08.016. [DOI] [PubMed] [Google Scholar]
- Kandra KL, Goldstein AO, Proescholdbell S. Variables associated with use and susceptibility to use of cigarettes among North Carolina adolescents: results from the 2007 statewide survey of high school students. N. C. Med. J. 2011;72:9–13. [PubMed] [Google Scholar]
- Leatherdale ST, Rios P, Elton-Marshall T, Burkhalter R. Cigar, cigarillo, and little cigar use among Canadian youth. J Prim Prev. 2011;32:161–170. doi: 10.1007/s10935-011-0248-6. [DOI] [PubMed] [Google Scholar]
- Magidson J, Vermunt JK. Latent class cluster analysis. In: Hagenaarsm JA, McCutcheon AL, editors. Applied Latent Class Analysis. Cambridge University Press; Cambridge, UK: 2000. [Google Scholar]
- Malson JL, Lee EM, Moolchan ET, Pickworth WB. Nicotine delivery from smoking bidis and an additive-free cigarette. Nicotine Tob. Res. 2002;4:485–490. doi: 10.1080/1462220021000018498. [DOI] [PubMed] [Google Scholar]
- Malson JL, Lee EM, Murty R, Moolchan ET, Pickworth WB. Clove cigarette smoking: biochemical, physiological, and subjective effects. Pharmacol. Biochem. Behav. 2003;74:739–745. doi: 10.1016/s0091-3057(02)01076-6. [DOI] [PubMed] [Google Scholar]
- Martinasek MP, McDermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Curr. Probl. Pediatr. Adolesc. Health Care. 2011;41:34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Morrell HER, Cohen LM, Bacchi D, West J. Predictors of smoking and smokeless tobacco use in college students: A preliminary study using web-based survey methodology. J Am Coll Health. 2005;54:108–115. doi: 10.3200/JACH.54.2.108-115. [DOI] [PubMed] [Google Scholar]
- Nasim A, Blank MD, Berry BM, Eissenberg T. Cigar use misreporting among youth: data from the 2009 Youth Tobacco Survey. Prev Chronic Dis. 2012 doi: http://dx.doi.org/10.5888/pcd9.110084. [PMC free article] [PubMed] [Google Scholar]
- National Survey on Drug Use and Health (NSDUH) sponsored by Department of Health and Human Services (DHHS), Substance Abuse and Mental Health Services Administration (SAMHSA), 2009.
- O’Connor RJ, McNeill A, Borland R, Hammond D, King B, Boudreau C, Cummings KM. Smokers’ beliefs about the relative safety of other tobacco products: findings from the ITC collaboration. Nicotine Tob. Res. 2007;9:1033–1042. doi: 10.1080/14622200701591583. [DOI] [PubMed] [Google Scholar]
- Pechacek TF, Folsom AR, de Gaudermaris R, Jacobs DR, Luepker RV, Gillum RF, Blackburn H. Smoke exposure in pipe and cigar smokers: serum thiocyanate measures. JAMA. 1985;254:3330–3332. [PubMed] [Google Scholar]
- Peterson AL, Severson HH, Andrews JA, Gott SP, Cigrang JA, Gordon JS, Hunter CM, Martin GC. Smokeless tobacco use in military personnel. Mil. Med. 2007;172:1300–1305. doi: 10.7205/milmed.172.12.1300. [DOI] [PubMed] [Google Scholar]
- Primack BA, Sidani J, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann. Behav. Med. 2008;36:81–86. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raad D, Gaddam S, Schunemann HJ, Irani J, Abou Jaoude P, Honeine R, Akl EA. Effects of water-pipe smoking on lung function: a systematic review and meta-analysis. Chest. 2011;139:764–774. doi: 10.1378/chest.10-0991. [DOI] [PubMed] [Google Scholar]
- Rae Olmsted KL, Bray RM, Reyes Guzman CM, Williams J, Kruger H. Overlap in use of different types of tobacco among active duty personnel. Nicotine Tob. Res. 2011;13:691–698. doi: 10.1093/ntr/ntr060. [DOI] [PubMed] [Google Scholar]
- Rigotti NA, Lee JE, Wechsler H. U.S. college students’ use of tobacco products. JAMA. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Rodu B, Stegmayr B, Nasic S, Cole P, Asplund K. Evolving patterns of tobacco use in Northern Sweden. J. Int. Med. 2003;253:660–665. doi: 10.1046/j.1365-2796.2003.01143.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Tobacco “chippers” - individual differences in tobacco dependence. Psychopharmacology. 1989;97:539–547. doi: 10.1007/BF00439561. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Light and intermittent smokers: background and perspective. Nicotine Tob. Res. 2009;11:122–125. doi: 10.1093/ntr/ntn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-Simone SY, Curbow BA, Stillman FA. Differing psychosocial risk profiles of college freshmen waterpipe, cigar, and cigarette smokers. Addict. Behav. 2008;33:1619–1624. doi: 10.1016/j.addbeh.2008.07.017. [DOI] [PubMed] [Google Scholar]
- Soldz S, Dorsey E. Youth attitudes and beliefs toward alternative tobacco products: cigars, bidis, and kreteks. Health Educ. Behav. 2005;32:549–566. doi: 10.1177/1090198105276219. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. NSDUH Series H-41. HHS Publication No. (SMA) 11-4658. [Google Scholar]
- Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115:131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutfin EL, Reboussin BA, McCoy TP, Wolfson M. Are college student smokers really a homogeneous group? A latent class analysis of college student smokers. Nicotine Tob. Res. 2009;11:444–454. doi: 10.1093/ntr/ntp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tercyak KP, Audrain J. Psychosocial correlates of alternate tobacco product use during early adolescence. Prev. Med. 2002;35:193–198. doi: 10.1006/pmed.2002.1060. [DOI] [PubMed] [Google Scholar]
- Terchek JJ, Larkin EMG, Male ML, Frank SH. Measuring cigar use in adolescents: Inclusion of a brand-specific item. Nicotine Tob Res. 2009;11:842–846. doi: 10.1093/ntr/ntp074. [DOI] [PubMed] [Google Scholar]
- Timberlake DS. A latent class analysis of nicotine-dependence criteria and use of alternative tobacco. J. Stud. Alcohol Drugs. 2008;69:709–717. doi: 10.15288/jsad.2008.69.709. [DOI] [PubMed] [Google Scholar]
- Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among U.S. males: findings from national surveys. Tob. Control. 2010;19:104–109. doi: 10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, McClure JB, de Moor C, Cofta-Gunn L, Cummings S, Cinciripini PM, Gritz ER. Concomittant use of cigarettes and smokeless tobacco: prevalence, correlates, and predictors of tobacco cessation. Prev. Med. 2002;34:638–648. doi: 10.1006/pmed.2002.1032. [DOI] [PubMed] [Google Scholar]
- Yerger V, Pearson C, Malone RE. When is a cigar not a cigar? African American youths’ understanding of “cigar” use. Am J Public Health. 2001;91:316–317. doi: 10.2105/ajph.91.2.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young D, Borland R, Hammond D, Cummings KM, Devlin E, Yong HH, O’Connnor RJ. Prevalence and attributes of roll-your-own smokers in the international tobacco control (ITC) four country survey. Tob. Control. 2006;15(Suppl. 3):76–82. doi: 10.1136/tc.2005.013268. [DOI] [PMC free article] [PubMed] [Google Scholar]