Abstract
3K3A-APC is a recombinant analog of activated protein C (APC) which is an endogenous protease with multiple functions in the body. Compared to APC, 3K3A-APC has reduced anticoagulant activity but preserved cell signaling activities. In the brain, 3K3A-APC exerts neuroprotective effects after an acute or chronic injury. 3K3A-APC is currently under clinical assessment as a neuroprotective agent following acute ischemic stroke. Whether 3K3A-APC can influence post-ischemic neurogenesis and improve neurological outcome by promoting brain repair remains unknown. Here we show that murine 3K3A-APC 0.8 mg/kg intraperitoneally given at 12 h, 1, 3, 5 and 7 days after permanent distal middle cerebral artery occlusion (dMCAO) in mice compared to vehicle improves significantly sensorimotor and locomotor activity 7 and 14 days after stroke, reduces infarct and edema volumes 7 days after stroke by 43% (P<0.05) and 50% (P<0.05), respectively, increases the number of newly formed neuroblasts in the subventricular zone, corpus callosum and the peri-infarct area 7 days after stroke by 2.2-fold, 2.3-fold and 2.2-fold (P<0.05), respectively, and increases the cortical width index 14 days after stroke by 28% (P<0.05). Functional outcome in 3K3A-APC-treated group, but not in vehicle-treated group, correlated inversely with the reductions in the infarct volume, and positively with the number of neuroblasts migrating in the peri-infarct area and the cortical width index. The effects of 3K3A-APC on neuroprotection, neurogenesis and brain repair were lost in protease activated receptor 1 (PAR1) deficient mice. Thus, late therapy with 3K3A-APC is neuroprotective and promotes stroke-induced neurogenesis and repair through PAR1 in mice.
Keywords: 3K3A-APC, Stroke, Neurogenesis, Neuroprotection, Protease activated receptor 1
1. Introduction
Activated protein C (APC) is an endogenous circulating serine protease with multiple functions in the body that are regulated chiefly by its anticoagulant and/or cell-signaling activities (Zlokovic and Griffin, 2011). The protease activated receptor 1 (PAR1) is a key receptor involved in APC-mediated cell-signaling in various types of cells in the central nervous system (CNS) and periphery (Mosnier et al., 2004). Within the neurovascular unit, APC activates vasculoprotective, neuroprotective and anti-inflammatory pathways in brain endothelium, neurons and microglia, respectively, protecting CNS after acute or chronic types of injury (Zlokovic and Griffin, 2011; Zlokovic, 2011). Besides CNS, APC exerts beneficial effects in multiple injury models in peripheral organs including heart, lung, kidney and liver (Griffin et al., 2012).
In the circulation, APC interacts with blood factors Va and VIIIa which involves its enzymatic active site region and the residues called exosites (Mosnier et al., 2004). Mutations in the APC exosites generate APC analogs with diminished anticoagulant activity but preserved cell signaling activity such as 3K3A-APC or 5 A-APC (Gale et al., 2002; Mosnier et al., 2007, 2004). These APC mutations ultimately reduce the risk of serious bleeding caused by APC’s anticoagulant activity which is especially important for treating CNS disorders. Studies in rodent models of stroke (Guo et al., 2009a; Wang et al., 2012, 2009), traumatic brain injury (Walker et al., 2010), amyotrophic lateral sclerosis (Zhong et al., 2009) and bacterial sepsis (Kerschen et al., 2010, 2007), have revealed that APC variants with reduced anticoagulant activity have beneficial effects that were equivalent to, and sometimes greater than, the wild type (wt) recombinant APC (wt-APC).
Wt-APC and 3K3A-APC exert strong anti-apoptotic activity in injured neurons by inhibiting both the intrinsic, caspase-9 and p53-mediated apoptotic pathway, and the extrinsic, caspase-8-mediated apoptotic pathway (Cheng et al., 2006; Guo et al., 2009a, 2009b, 2004; Liu et al., 2004; Wang et al., 2009). The anti-apoptotic effects of APCs in neurons are mediated mainly by PAR1, but according to some studies may also require the additional participation of PAR3 (Guo et al., 2009a, 2004) or endothelial protein C receptor (Cheng et al., 2003; Gorbacheva et al., 2009) wt-APC has been shown to potentiate subependymal proliferation of neural progenitor cells after ischemic (Thiyagarajan et al., 2008) or traumatic (Petraglia et al., 2010) CNS injury. Whether 3K3A-APC, which is currently under clinical assessment as a neuroprotective agent following acute ischemic stroke (Williams et al., 2012), can improve neurological outcome after stroke by promoting neurogenesis and cerebral cortical repair in addition to its direct neuroprotective effects is not known. It is also unknown whether the major APC receptor PAR1 (Mosnier et al., 2007; Zlokovic and Griffin, 2011) is required for 3K3AAPC effects in the CNS in vivo. To address these questions we studied functional recovery, neuropathological outcome, neurogenesis and cortical post-ischemic expansion in F2r+/+ mice encoding PAR1 and F2r−/− mice lacking PAR1 both subjected to permanent distal middle cerebral artery occlusion (dMCAO) and treated with late systemic multiple dose 3K3A-APC therapy or vehicle.
2. Results
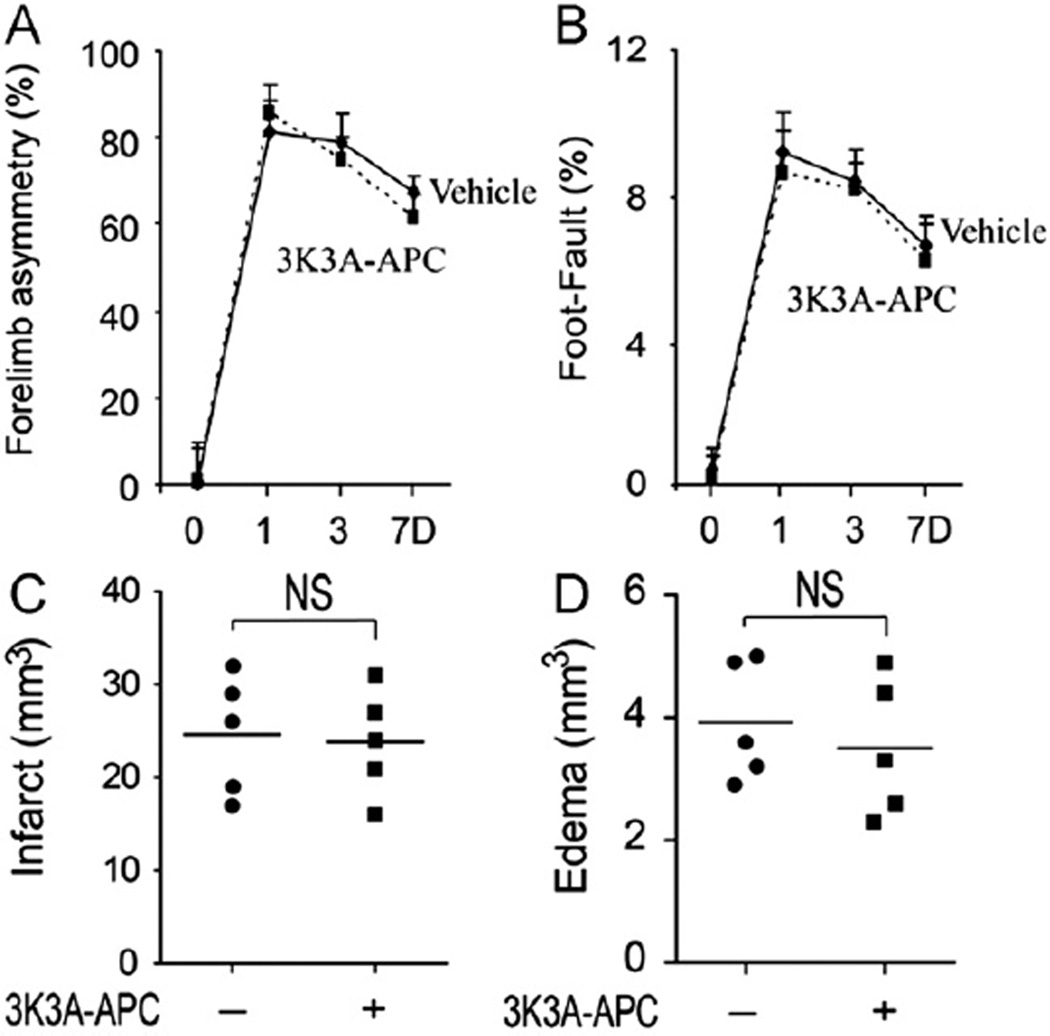
2.1. Sensorimotor activity and locomotor assessment
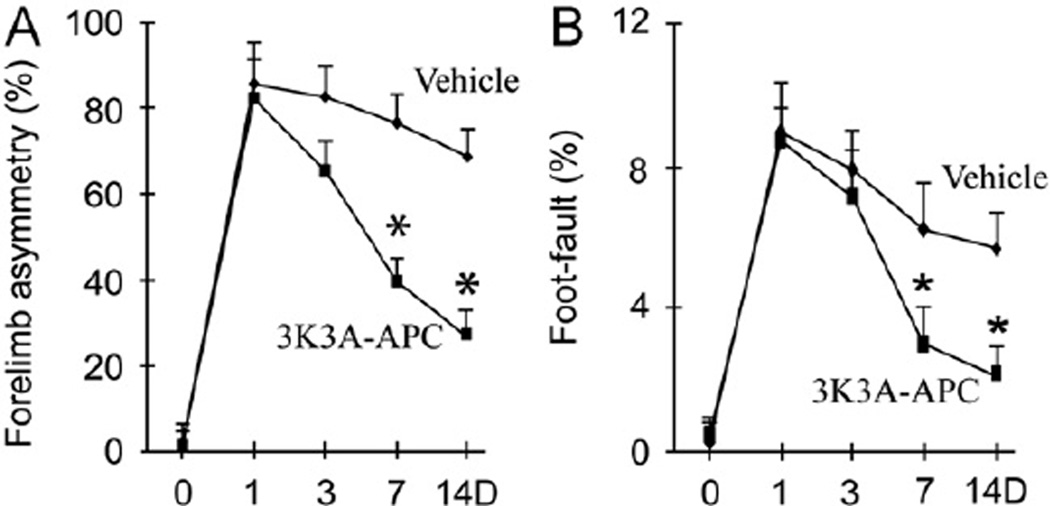
A series of tests were performed at days 1, 3, 7 and 14 after dMCAO to evaluate the effects of multiple dose 3K3A-APC treatment on sensorimotor activity by forelimb use asymmetry test (Schallert and Whishaw, 1984; Wang et al., 2009; Zlokovic et al., 2005) and locomotor assessment by foot-fault test (Gong et al., 2004; Wang et al., 2009; Zlokovic et al., 2005). As shown in Fig. 1A–B, 3K3A-APC significantly improved performance on both tests at day 7 and day 14 after stroke, but did not have an effect on functional outcome at day 1 and day 3 after stroke.
Fig. 1.
Effects of murine 3K3A-APC late multiple dose therapy on functional recovery within 14 days of permanent dMCAO. Forelimb use asymmetry test (A) and foot-fault test (B) were performed within 14 days after stroke in F2r+/+ C57Bl6 mice treated with vehicle (saline) or multiple dose 3K3A-APC (0.8 mg/kg intraperiotoneally) administered at 12 h, 1, 3, 5 and 7 days after onset of ischemia. Mean±SEM, n = 10 mice/group for functional tests in A–B within 7 days; n = 5 mice/group for functional tests at 14 days. *, **P<0.05.
2.2. 3K3A-APC reduces the volume of brain injury
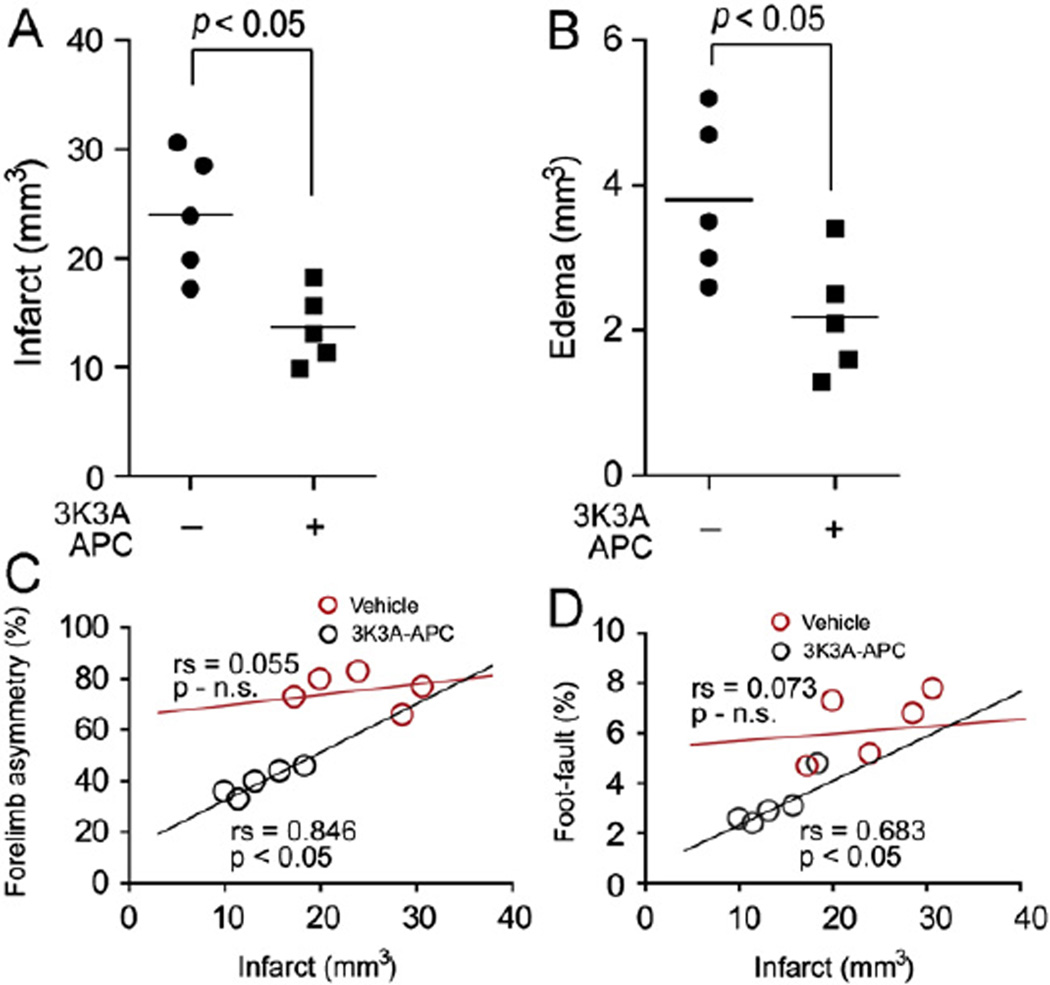
We next studied the effects of 3K3A-APC mutiple dose therapy on neuropathological outcome in relation to improvements observed in functional recovery within 7 days of stroke. Our data show that 3K3A-APC reduces the infarct and edema volumes by 43% and 50%, respectively (Fig. 2A and B). Interestingly, the observed neurological improvements in 3K3A-APC-treated group, but not in vehicle-treated group, correlated inversely with the reduction in the infarct volume 7 days after stroke (Fig. 2C–D).
Fig. 2.
Effects of murine 3K3A-APC late multiple dose therapy on neuropathological outcome after permanent dMCAO. Infarct volume (A), brain swelling (edema) (B) and regression analysis of functional outcome on forelimb use asymmetry test (C) and foot-fault test (D) versus the infarct volume at day 7 after dMCAO. Vehicle or multiple dose 3K3A-APC treatment (0.8 mg/kg intraperitoneally) were administered to F2r+/+ C57Bl6 mice at 12 h, 1, 3, 5 and 7 days after onset of ischemia. Mean±SEM, n = 5 mice/group. Pearson correlation coefficient (rs) and significance are indicated in panels C–D.
Although it is not exactly clear why we did not observe the correlation between infarct size and behavioral deficits in control mice subjected to permanent dMCAO model, it is interesting to note that regions most frequently affected after permanent dMCAO in control mice typically involve M1 (open field, rotarod, foot fault), S1FL (adhesive removal, forelimb placing test, forelimb asymmetry) and S1HL (hind limb placing test) regions, and in case of relatively larger infarctions also S2 (elevated body swing) and AuD and AuV, secondary auditory cortex dorsal and ventral (auditory startling), regions (not shown). Therefore, it is possible that permanent occlusion of the M1 distal portion of the left MCAO in the present study had a comparable effect on foot fault and forelimb asymmetry tests irrespective of the relative increase in infarct size as M1, S1FL and S1HL regions which coordinate performances of these two tests, respectively (Zlokovic et al., 2005; Wang et al., 2009), are most consistently affected by the procedure. However, to confirm this hypothesis, future studies should use a larger battery of tests including elevated body swinging and auditory startling and coordinate findings in individual animals with the precise topography of infarction.
2.3. 3K3A-APC stimulates post-ischemic neurogenesis
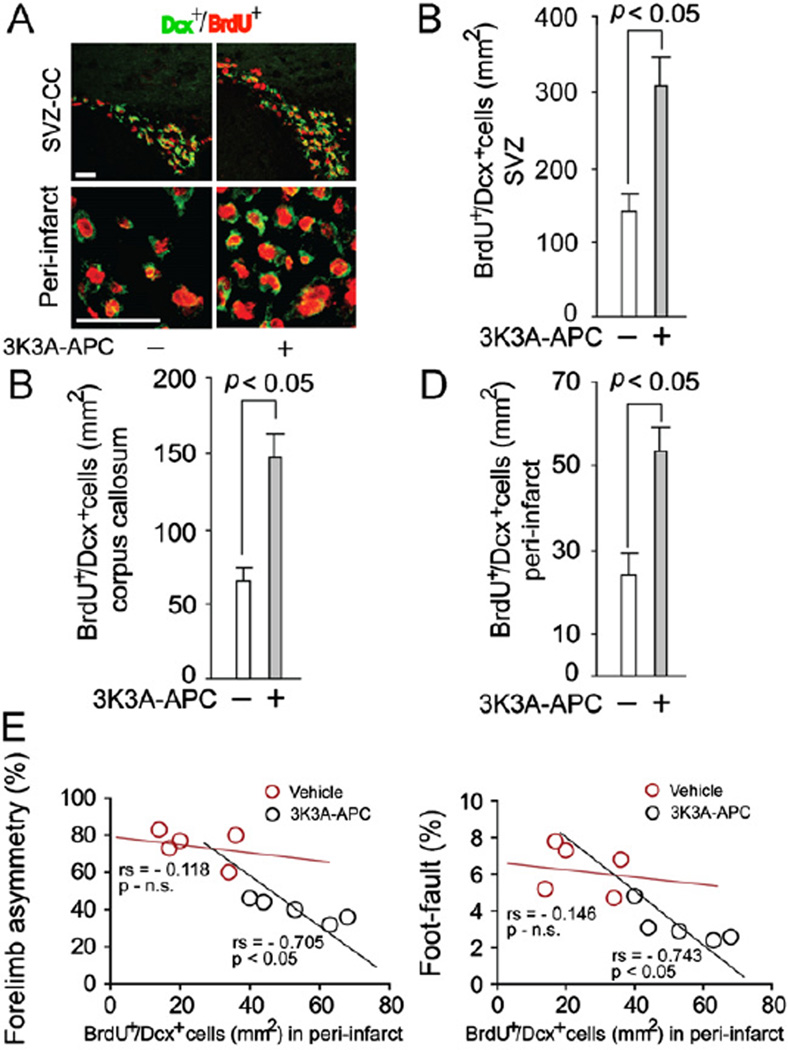
To determine the effects of 3K3A-APC multiple dose therapy on neurogenesis we studied migration of newly formed Dcx+/BrdU+ neuroblasts from SVZ to the peri-infarct area along the corpus callosum, and determined the number of newly formed neuroblasts in the SVZ region, corpus callosum and peri-infarct region within 7 days of stroke. Fig. 3A–C shows that 3K3A-APC treatment compared to vehicle increased by 2.2, 2.3 and 2.2-fold, respectively, the number of Dcx+/BrdU+ neuroblasts in the SVZ, corpus callosum and per-infarct area, within 7 days of stroke. Importantly, functional improvements on forelimb use asymmetry test and foot-fault test correlated positively with the increasing number of newly formed neuroblasts in the peri-infarct area (Fig. 3E–F).
Fig. 3.
Effects of murine 3K3A-APC latemultiple dose therapy on newly formed neuroblasts 7 days after permanent dMCAO. (A) Dcx+/BrdU+ neuroblasts migrating from the subventricular zone (SVZ) to the corpus callosum (upper panels; scale bar 50 µm), and Dcx+/BrdU+ neuroblasts in the peri-infarct region (lower panels; scale bar 50 µm) 7 days after permanent dMCAO. F2r+/+ C57Bl6 mice were treated with a multiple dose 3K3A-APC (0.8 mg/kg intraperitoneally at 12 h, 1, 3, 5 and 7 days after ischemia onset) or vehicle. Graphs show effect of 3K3A-APC multiple dose therapy as in (A) on the number of Dcx+/BrdU+ cells in the SVZ region (B) corpus callosum (C) and peri-infarct area (D). Regression analysis of functional outcome on forelimb use asymmetry test (E) and foot-fault test (F) versus the number of Dcx+/BrdU+ neuroblasts in the peri-infarct area at day 7. Mean±SEM, n = 5 mice/group. Pearson correlation coefficient (rs) and significance are indicated in panels D–E.
2.4. 3K3A-APC induces cerebral cortex expansion following ischemic stroke
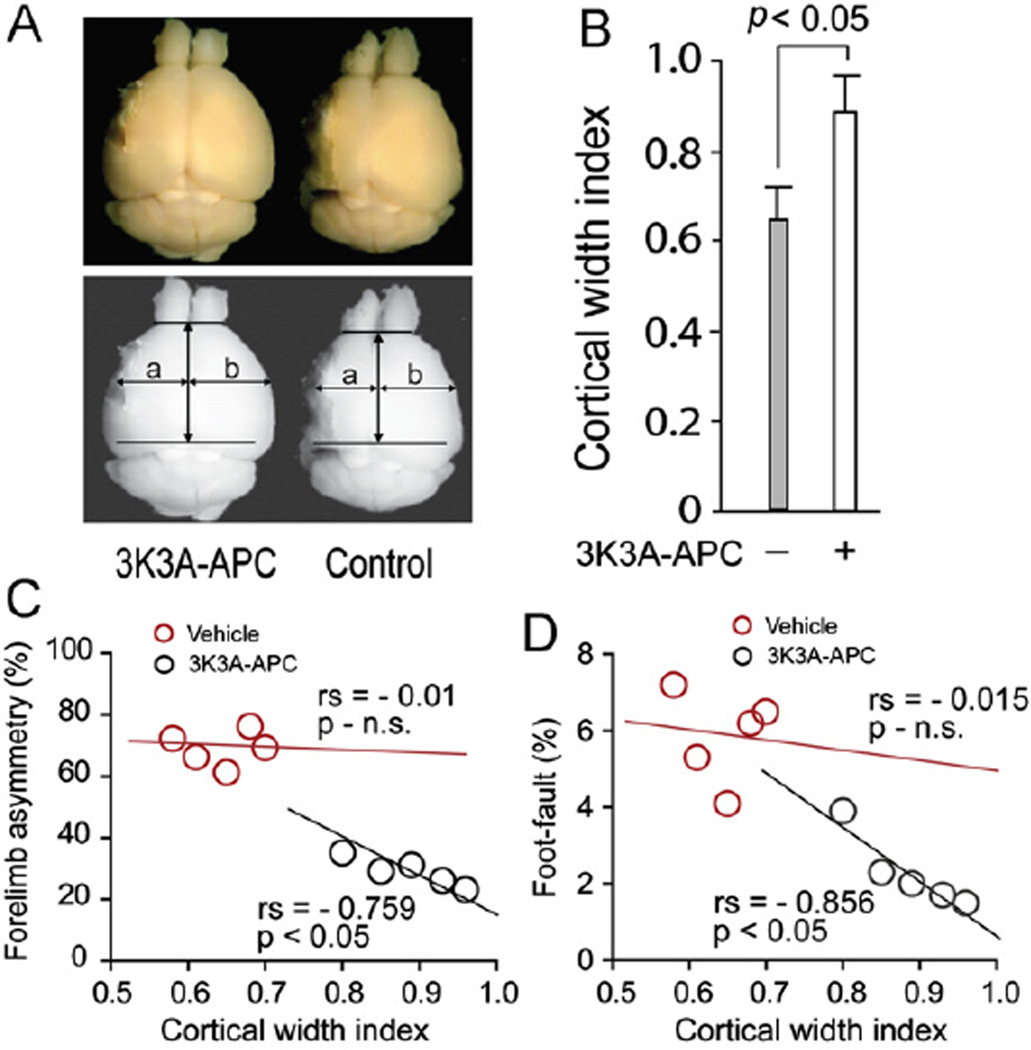
To determine the effects of 3K3A-APC multiple dose therapy on cerebral cortical expansion, the cortical width index was utilized as previously described (Taguchi et al., 2004; Zhao et al., 2006). Fig. 4A–B shows that the cortical width index was significantly increased by 3K3A-APC treatment compared to vehicle-treated controls within 14 days post-stroke. The improvements in functional outcome determined 14 days after stroke correlated positively with the cortical width index (Fig. 4C–D).
Fig. 4.
Effects of 3K3A-APC late multiple dose therapy on the cortical width index 14 days after permanent dMCAO. (A) Cortical cavitation (upper panels) and cortical width index measured using NIH Image J software (lower panels): a, maximum width from midpoint to edge of infarcted hemisphere; b, maximum edge from midpoint edge of noninfarcted hemisphere. F2r+/+ C57Bl6 mice treated with a multiple dose 3K3A-APC (0.8 mg/kg intraperitoneally at 12 h, 1, 3, 5 and 7 days after ischemia onset) or vehicle. (B) Cortical width index in mice treated with 3K3A-APC as above or vehicle. Regression analysis of forelimb use asymmetry test (C) and foot-fault test (D) versus the cortical width index at day 14. Mean±SEM, n = 5 mice/group. Pearson correlation coefficient (rs) and significance are indicated in panels C–D.
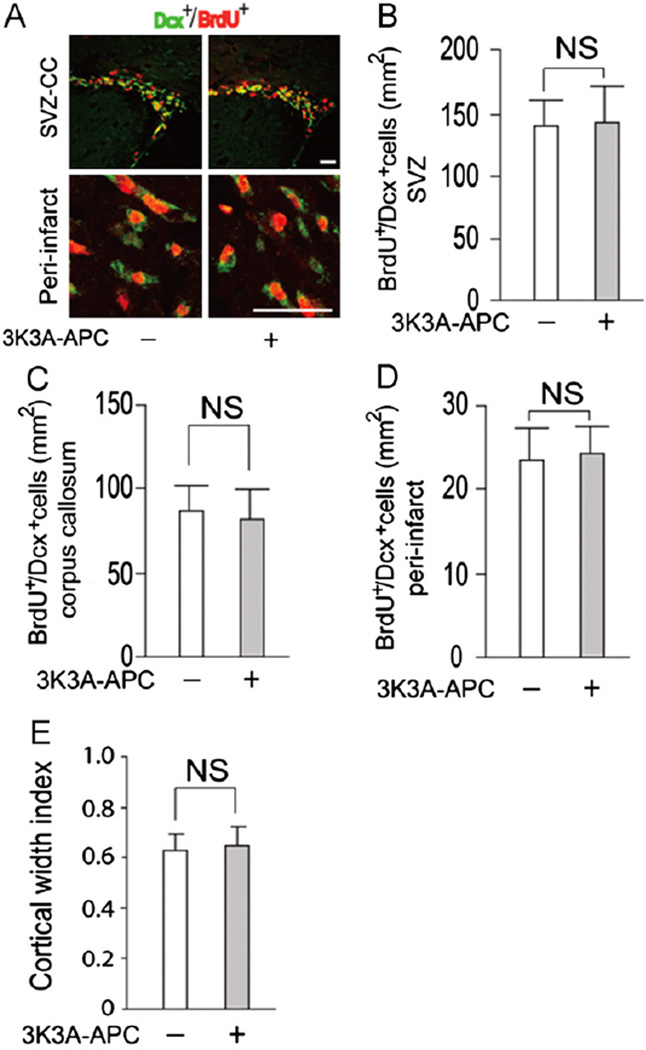
2.5. Loss of 3K3A-APC beneficial effects in F2r−/− mice
3K3A-APC multiple dose therapy in F2r−/− mice compared to vehicle did not have any significant effect on the functional outcome (i.e., forelimb use asymmetry and foot-fault tests) (Fig. 5A–B) or infarction and edema volumes (Fig. 5C and D). Moreover, 3K3A-APC therapy in F2r−/− mice compared to vehicle did not have any effect on the number of newly formed neuroblasts in the SVZ, corpus callosum and the peri-infarct region (Fig. 6A–D), nor did it have any effect on the cortical width index (Fig. 6E).
Fig. 5.
Effects of 3K3A-APC late multiple dose therapy on functional recovery and infarct volume in F2r−/− mice within 7 days of dMCAO. Forelimb use asymmetry test (A), foot-fault test (B), infarct volume (C) and edema volume (D) in F2r−/− mice on C57Bl6 background treated with 3K3A-APC (0.8 mg/kg intraperitoneally at 12 h, 1, 3, 5 and 7 days after onset of ischemia) or vehicle. Mean±SEM, n = 5 mice/group.
Fig. 6.
Effects of 3K3A-APC late multiple dose therapy on newly formed neuroblasts and the cortical width index in F2r−/− mice after dMCAO. (A) Dcx+/BrdU+ neuroblasts migrating from the subventricular zone (SVZ) to the corpus callosum (CC) (upper panels; scale bar 50 µm) and the peri-infarct region (lower panels, scale bar 50 µm) 7 days after dMCAO. Graphs showing the number of Dcx+/BrdU+ neuroblasts in the SVZ (B), corpus callosum (C) and peri-infarct area (D) 7 days after dMCAO. (E) Cortical width index 14 days after dMCAO. F2r−/− mice on C57Bl6 background were treated with a multiple dose 3K3A-APC (0.8 mg/kg intraperitoneally at 12 h, and at 1, 3, 5 and 7 days after ischemia onset) or vehicle. Mean±SEM, n = 5 mice/group.
3. Discussion
Previous studies have demonstrated that 3K3A-APC is directly neuroprotective after ischemic stroke and traumatic brain injury in rodents if administered within 4 or 6 h after injury, respectively (Guo et al., 2009a; Walker et al., 2010). In this study the dose of 3K3A-APC was increased from 0.2 mg/kg intravenously (Guo et al., 2009a) to 0.8 mg/kg intraperitoneally, which yields approximately 25–30% higher APC concentration in plasma based on 180 min areas under the curve of the integrated APC plasma concentrations (Thiyagarajan et al., 2008; Zhong et al., 2009) This moderate increase in 3K3A-APC dose did not result, however, in a greater brain protection compared to a previous report (Guo et al., 2009a). Interestingly, late multiple dose 3K3A-APC therapy beginning 12 h after stroke was still able to reduce the infarction and edema volumes by salvaging the peri-infarct area, but did not improve functional performance within first 3 days of stroke, in contrast to an earlier treatment when 3K3A-APC was given within first 4 h of stroke (Guo et al., 2009a). These data suggest that factors other than direct neuronal protection might be critical for functional improvement observed with the late 3K3A-APC treatment.
3K3A-APC significantly increased the number of post-ischemic newly formed neuroblasts in the SVZ region, corpus callosum and the peri-infract area indicating increased migration of neuroblasts from the SVZ to the site of ischemic injury. These data are in agreement with previous findings showing similar effect of wt-APC therapy on post-ischemic neurogenesis (Thiyagarajan et al., 2008). Several brain ischemia studies using agents such as sildenafil (Zhang et al., 2002), tadalfil (Zhang et al., 2006), statins (Chen et al., 2003), and erythropoietin (Wang et al., 2004; Wen and Wang, 2012) have reported that enhanced neurogenesis correlates well with the functional improvements, although delayed administration of these agents did not reduce cerebral infarction. Because delayed administration of 3K3A-APC did not improve functional outcome within the first 3 days of stroke, but only at days 7 and 14 after stroke, it is likely that neurological improvements seen with 3K3A-APC in this study can be attributed, at least in part, to its pro-neurogenic effects. Earlier findings have demonstrated that increased rate of neurogenesis, as for example in the dentate gyrus, may translate into an enhanced performance on a hippocampal-dependent tasks, whereas a decreasing rate of neurogenesis may be correlated with impairment of these tasks (Shors et al., 2001; Can Praag et al., 1999a, 1999b). Future studies should evaluate whether APC treatment also increases neurogenesis in the absence of prior ischemia.
3K3A-APC significantly increased cerebral cortical width index suggesting that in addition to increasing neurogenesis 7 days after stroke it increases cortical expansion as determined 14 days after stroke. Moreover, functional improvements in the 3K3A-APC-treated group, but not in the vehicle-treated group, correlated with the increasing number of neuroblasts in the peri-infarct area and the extent of cortical hyperplasia measured by the cortical width index, indicating that 3K3A-APC promotes brain repair which likely contributes in an important way to recovery of neurological functions. Interestingly, late 3K3A-APC treatment also reduced the infarction and edema volume within 7 days of stroke. Delayed administration of some agents such as wt-APC (Thiyagarajan et al., 2008), vascular endothelial growth factor (Sun et al., 2003), magnesium (Heath and Vink, 1999), cyclooxygenase-2 inhibitors (Candelario-Jalil et al., 2002), P53 inhibitor (Luo et al., 2009) and chondroitinase ABC (Soleman et al., 2012), have been also shown to reduce cerebral infarction similar to 3K3A-APC. The exact contributions of enhanced neurogenesis and brain repair versus direct protection of the peri-infarct tissue to the observed functional improvements seen with 3K3A-APC is difficult to assess based on the present findings. Future studies initiating 3K3A-APC treatment 3 days after stroke when its direct neuroprotection is likely eliminated as shown for example with wt-APC (Thiyagarajan et al., 2008), should be able to address this question. As wt-APC has been shown to promote post-ischemic angiogenesis (Thiyagarajan et al., 2008), it would be interesting to find out whether 3K3A-APC also retains the pro-angiogenic properties of wt-APC. In addition, future studies should examine the effects of 3K3A-APC therapy on the blood-brain barrier permeability and post-ischemic angiogenesis that can importantly influence brain repair and cortical expansion, as well as whether the presently observed effects are reproducible in older mice.
In this study we also show that the effects of 3K3A-APC on neuroprotection, neurogenesis and brain repair were lost in PAR1-deficient F2r−/− mice suggesting that PAR1 is critical for the observed beneficial 3K3A-APC effects. The present study using permanent dMCAO model did not find, however, any evidence suggesting that lack of PAR1 per se influences the neurological or neuropathological outcome in F2r−/− mice subjected to stroke compared to control F2r+/+ mice. These data indicate that under the present experimental conditions PAR1 deletion does not affect stroke evolution without the drug which is consistent with a previous report showing that lack of PAR1 does not influence the development of N-methyl-d-aspartate-induced excitotoxic brain lesions in mice (Guo et al., 2004). However, an earlier study using F2r−/− mice and neuropathological evaluations within 24 h of a transient MCAO, has shown that lack of PAR1 is protective when the period of MCA occlusion is limited to 30 min followed by 24 h of reperfusion, but is not protective when the period of MCA occlusion is extended to 60 min followed by 24 h reperfusion (Junge et al., 2003). Therefore, it is possible that lack of PAR1 might influence positively some processes occurring rapidly after periods of short-term ischemia followed by reperfusion, but does not have, on the other hand, any effect on ischemic mechanisms after longer periods of ischemia/reperfusion or permanent MCAO.
3K3A-APC has been manufactured for patients with acute ischemic stroke and other neurological disorders (Williams et al., 2012) as a new neuroprotective agent with direct vasculoprotective, blood-brain barrier enhancing, neuroprotective, and anti-inflammatory properties (Zlokovic and Griffin, 2011; Zlokovic, 2011). Our results support that 3K3AAPC can also potentially be considered as a potential neuroregeneration therapy. Given significant species-related differences between murine and human APC systems in terms of coagulation and cell signaling (Guo et al., 2009b), future studies should establish whether human 3K3A-APC can exert pro-neurogenic effects on human neural progenitor cells in culture as part of the process for a first step in translating the present findings from mice to humans.
4. Experimental procedures
4.1. Reagents
Murine 3K3A-APC (KKK191-193AAA) was prepared by ZZ Biotech using a stable cell line generated in Chinese hamster ovary (CHO) cells (Guo et al., 2009a) and procedures as reported (Fernández et al., 2003; Gale et al., 2002; Mosnier et al., 2004) with modifications (Guo et al., 2009a; Wang et al., 2009). The cells were maintained in suspension in CD Opti-CHO medium (Invitrogen, Carlsbad, CA) containing 2 mM CaCl2, 10 µg/ml vitamin K and 2 mM GlutaMAX (Invitrogen). For production, the cells were grown in the same medium in a 10 L Biowave bioreactor (5 L working volume) and fed with CD CHO Efficient Feed™ A (Invitrogen, Carlsbad, CA). A fourstep purification procedure was used: capturing PC using FFQ resin (GE Healthcare, Piscataway, NJ), further purification of 3K3A-PC using Uno Q column (BioRad, Richmond, CA), activation with recombinant human thrombin (ZymoGenetics, Seattle,WA), and removal of thrombin using a Uno Q column. The purity of 3K3A-APC was determined by reduced SDS-PAGE/silver staining. There was no detectable thrombin in the purified APC preparations based on thrombin time clotting assays using purified fibrinogen.
For immunostaining, the following primary antibodies were used: rat monoclonal anti-BrdU (1:100; AbD SeroTech, Oxford, UK) and rabbit polyclonal anti-human doublecortin (Dcx) which cross reacts with mouse Dcx (1:100; Cell Signaling Tech. Inc., Danvers, MA). The following secondary antibodies were used: anti-rat IgG Cy3 conjugate (1:200; Jackson ImmunoResearch Laboratories) and anti-rabbit IgG-fluorescein isothiocynate (FITC) conjugate (1:200; Jackson ImmunoResearch Laboratories, West Grove, PA).
4.2. Permanent distal middle cerebral artery occlusion (dMCAO)
All procedures were approved by the Institutional Animal Care and Use Committee at the University of Rochester. Male 2–3-month-old F2r+/+ C57Bl/6 mice (The Jackson Laboratory) and male 2–3-month-old F2r−/− mice on 97% C57BL/6 background obtained from Dr. S. Coughlin, University of California, San Francisco, San Francisco, CA (Connolly et al., 1996), were used (total of 40 mice). The mice were anaesthetized intraperitoneally with 100 mg/kg body weight ketamine and 10 mg/kg body weight xylazine. The physiological parameters were monitored as described previously (Wang et al., 2009). Briefly, animals were allowed to breathe spontaneously. Rectal temperature was maintained between 36.5 and 37.0 °C using a feedback-controlled heating system. The right femoral artery was cannulated for continuous monitoring of blood pressure and blood analysis including pO2, pCO2 and pH.
Permanent distal middle cerebral artery occlusion (dMCAO) was performed as we previously described (Wang et al., 2009). In brief, under the surgical microscope the left common carotid artery was isolated through a neck incision and ligated using a 5-0 silk (Roboz surgical instrument Co.). A skin incision was made between the left orbit and tragus. The zygomatic arch was removed and temporal muscle retracted laterally. The mandible was retracted downward. The MCA was visible through the temporal semitranslucent surface of the skull. A 2-mm burr hole was made with a high-speed micro-drill through the outer surface of the semitranslucent skull over the visually identified MCA. The dura was carefully opened and the M1 branch of the MCA exposed and coagulated using a cauterizer producing permanent dMCAO. The wound was sutured, and rectal temperature was controlled until mice regained full consciousness.
All studies were perfomed in a blind fashion. Male C57BL/6 F2r+/+ mice and F2r−/− mice were randomly assigned to the vehicle-treated group and 3K3A-APC-treated group. 3K3AAPC (0.8 mg/kg at 12 h, and at 1, 3, 5 and 7 days after stroke) or vehicle (saline) were administered intraperitoneally.
4.3. Functional tests
The following behavioral tests were performed in mice at 0, 1, 3, 7 and 14 days after stroke: (i) forelimb use asymmetry test, for sensorimotor activity (Wang et al., 2009; Zlokovic et al., 2005); and (ii) foot-fault test, for locomotor assessment (Cheng et al., 2003; Gong et al., 2004; Liu et al., 2004).
4.4. Neuropathological analysis
4.4.1. Infarct volume and swelling
Mice were sacrificed 7 days after dMCAO under anesthesia as above (4.4.2) and the brains removed and rapidly frozen in CO2 snow. Brains were cut into serial 20 µm cryostat sections. Every 10th section was stained with cresyl-violet and the lesion area determined using the NIH Image J analysis system (Bethesda, MD, USA). Infarct volume and brain swelling (edema) were determined as previously described (Wang et al., 2005; Zlokovic et al., 2005).
4.4.2. Assessment of cerebral cortical expansion
Mice anesthetized as above (4.4.2) were perfusion fixed with paraformaldehyde 14 days after stroke and the brains were removed. Whole brain images were captured using a microscopic digital camera system coupled to a dissecting stereomicroscope (AxioCam, Zeiss). Images were analyzed by the NIH Image J system (Bethesda, MD, USA). The distance from midline to the edge of brain on the ischemic hemisphere was divided by the distance from midline to the lateral edge on the contralateral side to calculate the cortical width index as previously described (Taguchi et al., 2004; Zhao et al., 2006).
4.5. Analysis of neurogenesis
4.5.1. 5-Bromo-2′-deoxyuridine labeling (BrdU) in vivo
BrdU labeling in combination with doublecortin (Dcx) was used to study newly formed neuroblasts in the SVZ region, in the corpus callosum during their migration from SVZ to the peri-infarct regions, and in the peri-infarct regions. BrdU (Sigma, St. Louis, MO), 50 mg/kg in saline intraperitoneally, was given at 8 h intervals twice daily for 6 days, beginning at 24 h after dMCAO.
4.5.2. Immunohistochemistry
Coronal cryostat sections (20 µm) were mounted on slides, post-fixed with methanol, and stored at −20 °C until immunostaining. Brain sections were initially prepared for BrdU staining as previously described (Thiyagarajan et al., 2008), and incubated with primary antibodies to BrdU and Dcx followed by incubation with their respective secondary antibodies (anti-rat IgG-Cy3 to detect BrdU, and anti-rabbit IgGFITC to detect Dcx). All secondary antibodies were incubated for 1 h at 37 °C. Confocal laser-scanning microscopy (LSM510 META; Carl Zeiss MicroImaging) was used to acquire images from immunostained sections. An Argon laser (excitation 488 nm; emission 500–550 nm) and a helium-neon laser (excitation 543 nm; emission 560–615 nm) were used to excite FITC and Cy3, respectively.
4.5.3. Quantification of BrdU+/Dcx+ cells
Three regions of interest (1 mm2) per section (20 µm) within the SVZ, peri-infarct area and corpus callosum, and three sections per animal (200 µm apart), were counted blindly under ×25 objective (LSM510, Zeiss). BrdU+/Dcx+ cells were quantified as the average number of BrdU and Dcx double-positive cells per mm2/section. Data were presented as mean±SEM.
4.6. Statistics
Data are presented as mean±standard error of the mean. One-way analysis of variance (ANOVA) followed by Tukey post hoc test was used to determine statistically significant differences in the infarct and edema volumes and the cortical width index. P<0.05 was considered statistically significant. The difference between the number of BrdU+/Dcx+ cells in the studied groups was analyzed by Mann–Whitney U-test. P<0.05 was considered as statistically significant difference. Pearson’s correlation was used for regressions analysis of functional performance versus lesion volume, cortical width index and the number of BrdU+/Dcx+ cells using statistical software (GraphPad Prism 3.02).
Acknowledgments
This work was supported by the National Institutes of Health grant HL63290 (BZ), HL52246 (JHG) and ZZ Biotech L.L.C.
Footnotes
Conflict of interest
B.V.Z. is the scientific founder of ZZ Biotech, a biotechnology company with a focus to develop APC and its functional mutants for stroke and other neurological disorders. J.H.G. is a member of the Scientific Advisory Board of ZZ Biotech LLC.
REFERENCES
- Candelario-Jalil E, Alvarez D, González-Falcón A, García-Cabrera M, Martínez-Sánchez G, Merino N, Giuliani A, León OS. Neuroprotective efficacy of nimesulide against hippocampal neuronal damage following transient forebrain ischemia. Eur. J. Pharmacol. 2002;453:189–195. doi: 10.1016/s0014-2999(02)02422-6. [DOI] [PubMed] [Google Scholar]
- Chen J, Zhang ZG, Li Y, Wang Y, Wang L, Jiang H, Zhang C, Lu M, Katakowski M, Feldkamp CS, Chopp M. Statins induce angiogenesis, neurogenesis, and synaptogenesis after stroke. Ann. Neurol. 2003;53:743–751. doi: 10.1002/ana.10555. [DOI] [PubMed] [Google Scholar]
- Cheng T, Liu D, Griffin JH, Fernández JA, Castellino F, Rosen ED, Fukudome K, Zlokovic BV. Activated protein C blocks p53-mediated apoptosis in ischemic human brain endothelium and is neuroprotective. Nat. Med. 2003;9:338–342. doi: 10.1038/nm826. [DOI] [PubMed] [Google Scholar]
- Cheng T, Petraglia AL, Li Z, Thiyagarajan M, Zhong Z, Wu Z, Liu D, Maggirwar SB, Deane R, Fernández JA, LaRue B, Griffin JH, Chopp M, Zlokovic BV. Activated protein C inhibits tissue plasminogen activator-induced brain hemorrhage. Nat. Med. 2006;12:1278–1285. doi: 10.1038/nm1498. [DOI] [PubMed] [Google Scholar]
- Connolly AJ, Ishihara H, Kahn ML, Farese RV, Jr, Coughlin SR. Role of the thrombin receptor in development and evidence for a second receptor. Nature. 1996;381:516–519. doi: 10.1038/381516a0. [DOI] [PubMed] [Google Scholar]
- Fernández JA, Xu X, Liu D, Zlokovic BV, Griffin JH. Recombinant murine-activated protein C is neuroprotective in a murine ischemic stroke model. Blood Cells, Mol., Dis. 2003;30:271–276. doi: 10.1016/s1079-9796(03)00034-2. [DOI] [PubMed] [Google Scholar]
- Gale AJ, Tsavaler A, Griffin JH. Molecular characterization of an extended binding site for coagulation factor Va in the positive exosite of activated protein C. J. Biol. Chem. 2002;277:28836–28840. doi: 10.1074/jbc.M204363200. [DOI] [PubMed] [Google Scholar]
- Gong Y, Hua Y, Keep RF, Hoff JT, Xi G. Intracerebral hemorrhage: effects of aging on brain edema and neurological deficits. Stroke. 2004;35:2571–2575. doi: 10.1161/01.STR.0000145485.67827.d0. [DOI] [PubMed] [Google Scholar]
- Gorbacheva L, Davidova O, Sokolova E, Ishiwata S, Pinelis V, Strukova S, Reiser G. Endothelial protein C receptor is expressed in rat cortical and hippocampal neurons and is necessary for protective effect of activated protein C at glutamate excitotoxicity. J. Neurochem. 2009;111:967–975. doi: 10.1111/j.1471-4159.2009.06380.x. [DOI] [PubMed] [Google Scholar]
- Griffin JH, Zlokovic BV, Mosnier LO. Protein C anticoagulant and cytoprotective pathways. Int. J. Hematol. 2012;95:333–345. doi: 10.1007/s12185-012-1059-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Liu D, Gelbard H, Cheng T, Insalaco R, Fernández JA, Griffin JH, Zlokovic BV. Activated protein C prevents neuronal apoptosis via protease activated receptors 1 and 3. Neuron. 2004;41:563–572. doi: 10.1016/s0896-6273(04)00019-4. [DOI] [PubMed] [Google Scholar]
- Guo H, Singh I, Wang Y, Deane R, Barrett T, Fernández JA, Chow N, Griffin JH, Zlokovic BV. Neuroprotective activities of activated protein C mutant with reduced anticoagulant activity. Eur. J. Neurosci. 2009a;29:1119–1130. doi: 10.1111/j.1460-9568.2009.06664.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Guo H, Wang Y, Singh I, Liu D, Fernández JA, Griffin JH, Chow N, Zlokovic BV. Species-dependent neuroprotection by activated protein C mutants with reduced anticoagulant activity. J. Neurochem. 2009b;109:116–124. doi: 10.1111/j.1471-4159.2009.05921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath DL, Vink R. Improved motor outcome in response to magnesium therapy received up to 24 h after traumatic diffuse axonal brain injury in rats. J. Neurosurg. 1999;90:504–509. doi: 10.3171/jns.1999.90.3.0504. [DOI] [PubMed] [Google Scholar]
- Junge CE, Sugawara T, Mannaioni G, Alagarsamy S, Conn PJ, Brat DJ, Chan PH, Traynelis SF. The contribution of protease-activated receptor 1 to neuronal damage caused by transient focal cerebral ischemia. Proc. Natl. Acad. Sci. U.S.A. 2003;100:13019–13024. doi: 10.1073/pnas.2235594100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschen E, Hernandez I, Zogg M, Jia S, Hessner MJ, Fernandez JA, Griffin JH, Huettner CS, Castellino FJ, Weiler H. Activated protein C targets CD8+ dendritic cells to reduce the mortality of endotoxemia in mice. J.Clin. Invest. 2010;120:3167–3178. doi: 10.1172/JCI42629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschen EJ, Fernandez JA, Cooley BC, Yang XV, Sood R, Mosnier LO, Castellino FJ, Mackman N, Griffin JH, Weiler H. Endotoxemia and sepsis mortality reduction by non-anticoagulant activated protein C. J. Exp. Med. 2007;204:2439–2448. doi: 10.1084/jem.20070404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Cheng T, Guo H, Fernández JA, Griffin JH, Song X, Zlokovic BV. Tissue plasminogen activator neurovascular toxicity is controlled by activated protein C. Nat. Med. 2004;10:1379–1383. doi: 10.1038/nm1122. [DOI] [PubMed] [Google Scholar]
- Luo Y, Kuo C-C, Shen H, Chou J, Greig NH, Hoffer BJ, Wang Y. Delayed treatment with a p53 inhibitor enhances recovery in stroke brain. Ann. Neurol. 2009;65:520–530. doi: 10.1002/ana.21592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosnier LO, Gale AJ, Yegneswaran S, Griffin JH. Activated protein C variants with normal cytoprotective but reduced anticoagulant activity. Blood. 2004;104:1740–1744. doi: 10.1182/blood-2004-01-0110. [DOI] [PubMed] [Google Scholar]
- Mosnier LO, Zlokovic BV, Griffin JH. The cytoprotective protein C pathway. Blood. 2007;109:3161–3172. doi: 10.1182/blood-2006-09-003004. [DOI] [PubMed] [Google Scholar]
- Petraglia AL, Marky AH, Walker C, Thiyagarajan M, Zlokovic BV. Activated protein C is neuroprotective and mediates new blood vessel formation and neurogenesis after controlled cortical impact. Neurosurgery. 2010;66:165–171. doi: 10.1227/01.NEU.0000363148.49779.68. discussion 171–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schallert T, Whishaw IQ. Bilateral cutaneous stimulation of the somatosensory system in hemidecorticate rats. Behav. Neurosci. 1984;98:518–540. doi: 10.1037//0735-7044.98.3.518. [DOI] [PubMed] [Google Scholar]
- Shors TJ, Miesegaes G, Beylin A, Zhao M, Rydel T, Gould E. Neurogenesis in the adult is involved in the formation of trace memories. Nature. 2001;410:372–376. doi: 10.1038/35066584. [DOI] [PubMed] [Google Scholar]
- Soleman S, Yip PK, Duricki DA, Moon LDF. Delayed treatment with chondroitinase ABC promotes sensorimotor recovery and plasticity after stroke in aged rats. Brain. 2012;135:1210–1223. doi: 10.1093/brain/aws027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Jin K, Xie L, Childs J, Mao XO, Logvinova A, Greenberg DA. VEGF-induced neuroprotection, neurogenesis, and angiogenesis after focal cerebral ischemia. J. Clin. Invest. 2003;111:1843–1851. doi: 10.1172/JCI17977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taguchi A, Soma T, Tanaka H, Kanda T, Nishimura H, Yoshikawa H, Tsukamoto Y, Iso H, Fujimori Y, Stern DM, Naritomi H, Matsuyama T. Administration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse model. J. Clin. Invest. 2004;114:330–338. doi: 10.1172/JCI20622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiyagarajan M, Fernández JA, Lane SM, Griffin JH, Zlokovic BV. Activated protein C promotes neovascularization and neurogenesis in postischemic brain via protease-activated receptor 1. J. Neurosci. 2008;28:12788–12797. doi: 10.1523/JNEUROSCI.3485-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Praag H, Christie BR, Sejnowski TJ, Gage FH. Running enhances neurogenesis, learning, and long-term potentiation in mice. Proc. Natl. Acad. Sci. U.S.A. 1999a;96:13427–13431. doi: 10.1073/pnas.96.23.13427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Praag H, Kempermann G, Gage FH. Running increases cell proliferation and neurogenesis in the adult mouse dentate gyrus. Nat. Neurosci. 1999b;2:266–270. doi: 10.1038/6368. [DOI] [PubMed] [Google Scholar]
- Walker CT, Marky AH, Petraglia AL, Ali T, Chow N, Zlokovic BV. Activated protein C analog with reduced anticoagulant activity improves functional recovery and reduces bleeding risk following controlled cortical impact. Brain Res. 2010;1347:125–131. doi: 10.1016/j.brainres.2010.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Zhang Z, Wang Y, Zhang R, Chopp M. Treatment of stroke with erythropoietin enhances neurogenesis and angiogenesis and improves neurological function in rats. Stroke. 2004;35:1732–1737. doi: 10.1161/01.STR.0000132196.49028.a4. [DOI] [PubMed] [Google Scholar]
- Wang Y, Kilic E, Kilic U, Weber B, Bassetti CL, Marti HH, Hermann DM. VEGF overexpression induces postischaemic neuroprotection, but facilitates haemodynamic steal phenomena. Brain. 2005;128:52–63. doi: 10.1093/brain/awh325. [DOI] [PubMed] [Google Scholar]
- Wang Y, Thiyagarajan M, Chow N, Singh I, Guo H, Davis TP, Zlokovic BV. Differential neuroprotection and risk for bleeding from activated protein C with varying degrees of anticoagulant activity. Stroke. 2009;40:1864–1869. doi: 10.1161/STROKEAHA.108.536680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhang Z, Chow N, Davis TP, Griffin JH, Chopp M, Zlokovic BV. An activated protein C analog with reduced anticoagulant activity extends the therapeutic window of tissue plasminogen activator for ischemic stroke in rodents. Stroke. 2012;43:2444–2449. doi: 10.1161/STROKEAHA.112.658997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z, Wang P. Recombinant human erythropoietin increases cerebral cortical width index and neurogenesis following ischemic stroke. Neural Regeneration Res. 2012:7. doi: 10.3969/j.issn.1673-5374.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PD, Zlokovic BV, Griffin JH, Pryor KE, Davis TP. Preclinical safety and pharmacokinetic profile of 3K3A-APC, a novel, modified activated protein C for ischemic stroke. Curr. Pharm. Des. 2012;18:4215–4222. doi: 10.2174/138161212802430413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Zhang Z, Zhang RL, Cui Y, LaPointe MC, Silver B, Chopp M. Tadalafil, a long-acting type 5 phosphodiesterase isoenzyme inhibitor, improves neurological functional recovery in a rat model of embolic stroke. Brain Res. 2006;1118:192–198. doi: 10.1016/j.brainres.2006.08.028. [DOI] [PubMed] [Google Scholar]
- Zhang R, Wang Y, Zhang L, Zhang Z, Tsang W, Lu M, Zhang L, Chopp M. Sildenafil (Viagra) induces neurogenesis and promotes functional recovery after stroke in rats. Stroke. 2002;33:2675–2680. doi: 10.1161/01.str.0000034399.95249.59. [DOI] [PubMed] [Google Scholar]
- Zhao B-Q, Wang S, Kim H-Y, Storrie H, Rosen BR, Mooney DJ, Wang X, Lo EH. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat. Med. 2006;12:441–445. doi: 10.1038/nm1387. [DOI] [PubMed] [Google Scholar]
- Zhong Z, Ilieva H, Hallagan L, Bell R, Singh I, Paquette N, Thiyagarajan M, Deane R, Fernandez JA, Lane S, Zlokovic AB, Liu T, Griffin JH, Chow N, Castellino FJ, Stojanovic K, Cleveland DW, Zlokovic BV. Activated protein C therapy slows ALS-like disease in mice by transcriptionally inhibiting SOD1 in motor neurons and microglia cells. J. Clin. Invest. 2009;119:3437–3449. doi: 10.1172/JCI38476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlokovic BV. Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat. Rev. Neurosci. 2011;12:723–738. doi: 10.1038/nrn3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlokovic BV, Griffin JH. Cytoprotective protein C pathways and implications for stroke and neurological disorders. Trends Neurosci. 2011;34:198–209. doi: 10.1016/j.tins.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlokovic BV, Zhang C, Liu D, Fernandez J, Griffin JH, Chopp M. Functional recovery after embolic stroke in rodents by activated protein C. Ann. Neurol. 2005;58:474–477. doi: 10.1002/ana.20602. [DOI] [PubMed] [Google Scholar]