Abstract
Argentina is a middle-income country with a population of 40 million people. The structure of morbidity and mortality approaches that of more developed nations, with congenital and genetic disorders contributing significantly to ill health. The health delivery system is mixed, with public, social security, and private sectors which together spend close to 10 % of the GNP. Health subsectors are decentralized at provincial and municipality levels, where health planning and financing occurs, leading to fragmentation, inefficiency, and inequities. There are about 41 clinical genetic units in major medical centers in large cities, staffed by about 120 clinical geneticists, although only a few units are fully comprehensive genetic centers. Duplications, deficiencies, and poor regionalization and coordination affect health care delivery in general and in genetics. Funding for genetic services is limited due to poor understanding and lack of political will on the part of health authorities. Recently, however, there have been some interesting initiatives by national and provincial ministries of health to improve genetic services delivery by increasing coordination and regionalization. At the same time, training in genetics of health professionals is occurring, particularly in primary health care, and registries of congenital defects are being put in place. These developments are occurring in conjunction with a new awareness by health authorities of the importance of genetics in health care and research, a heightened activism of patient organizations demanding services for neglected conditions, as well as of women movements for the right to safe abortion.
Keywords: Genetic services, Genetic testing, Argentina, Developing countries, Ethical and social issues, Genetic research
Introduction
Argentina is a middle-income country, with a per capita gross national income of 9,126 USD in 2008 (or 7,190 international dollars/purchasing power parity). It is situated in the southern tip of South America, with a population of 40 million, 90 % of whom live in urban areas. When the Spanish conquistadors arrived to what is now Argentina at the beginning of the sixteenth century, the territory was inhabited by millions of Amerindians of at least 30 different ethnicities. Spaniard colonization took place in the next two centuries and, while extensive admixture occurred, a sizable native population remained in the region. In the late nineteenth century, most remaining Amerindians were decimated by military extermination campaigns, and currently number less than 400,000 persons concentrated in the northwest, northeast, and the south of the country. West Africans brought as slaves had their numbers drastically reduced in the second half of the nineteenth century through admixture and migration to neighboring countries, and there are virtually no African descendants in modern Argentina. In the second half of the nineteenth century and first half of the twentieth century, Argentina received a huge influx of immigration from virtually all countries of Europe, as well as large contingents of European Jews and to a lesser extent, Middle Eastern peoples. In recent times, immigration is coming primarily from neighboring countries (Paraguay and Bolivia) with strong Amerindian ancestry, and small numbers from Asia.
Demography and health indicators
According to the National Census on October 27, 2010, the population of Argentina was 40,091,359 individuals, of which 4.2 % were foreign born. Currently, about 50 % of the population trace their origin to Italian immigrants and 25–30 % to Spaniards. The relative European, Amerindian, and West African genetic contributions to the gene pool have been estimated in the population of Buenos Aires in 67.5, 25.9, and 6.5 %, respectively (Martínez-Marignac et al. 2004). Average consanguinity is less than 1 %, except in some rare isolated areas (Castilla et al. 1991; Liascovich et al. 2001). The official language of the country is Spanish. The majority of the population are nominally of Catholic faith, and historically, the Catholic church has exerted a very strong political influence in a wide range of topics, such as education, reproduction rights, and abortion. The rate of population growth between 2001 and 2010 was 10.5 %, and the predicted population size for 2015 is 42.5 million. Currently, 90 % of the population live in urban areas, and the percentage of civil registration coverage of births was 99 %.
The total fertility rate is 2.3 births per woman, and the percentage of live births from women aged 35 years or more is 8 % (INDEC 2010; Argentina 2011). Life expectancy at birth is 75.2 years (79.1 years for women; 71.6 years for men). Healthy life expectancy at birth is 65.2 years (68.1 years for females; 62.5 years for men).
Infant mortality rate, which was 33.3 per 1,000 live births in 1980, came down to 12.5 in 2009. Its neonatal component was 8.5 per 1,000 live births. The under-5 mortality rate in 2009 was 15.6 per 1,000. The adult mortality rate (probability of dying between 15 and 60 years per 1,000 population) was 7.6 (8.2 for men; 7.0 for women). The maternal mortality rate in 2008 was 44 per 100,000 live births, of which at least 25 % was due to complications of unsafe abortion (there are at least 500,000 illegal induced abortions yearly, a substantial proportion of which are unsafe). Coverage of antenatal care is good (at least four antenatal visits, 99 %) as well as percentage of births attended by skilled health personnel (99.4 %; Argentina 2011).
Health services, expenditures, and financing
The total health expenditures are estimated in 9.6 % of the GNP, amounting to USD 663 per capita, distributed in the public, social security, and private sectors into which Argentina’s health system is divided (Penchaszadeh et al. 2010). The public system is funded through general taxation, maintains public hospitals and ambulatory health centers throughout the country, and spends 22 % of the country’s total health expenditures to provide free health care on demand to approximately 48 % of the population, mostly the poor and those without insurance. The public system of health care is decentralized, with hospitals and health centers belonging to provinces or municipalities. The social security sector of health services is funded by employer and employee contributions, and spends 29 % of the country’s total health expenditures through contracts with the private sector to serve 47 % of the population, largely blue-collar workers, employees, and retired persons. The private sector is a for-profit insurance-based model that spends 49.5 % of total health expenditures and serves 7.5 % of the population (middle and upper classes).
The degree of fragmentation of the health system is highlighted by the number of different budgetary and administrative health units, largely independent of each other. The public system is divided into 24 independent health administrations (one in each province), and more than 100 units in the larger municipalities, each providing health services of widely different qualities and coverage. In turn, the social security sector is fragmented in over 350 administrative entities organized by trade or territory, while the private sector includes hundreds of institutions, either delivering or financing services or both.
The national Ministry of Health is responsible for the development of general health objectives, policies and regulations, executing national health programs (such as vaccinations, campaigns against tobacco, cancer, obesity, etc.), overseeing the general operation of health services, and negotiating the coverage and fees of health insurance plans, all in coordination with provincial health authorities. However, its leverage to influence decisions at provincial level is weak as each province has the authority and the funds to plan and deliver health care to their population. This determines wide variations in coverage and quality of care between jurisdictions
The 9.6 % of GNP spent on health is divided into 2.09 % by the public sector, 2.28 % by the social security sector, 0.70 % for the retired citizens program, and 4.53 % by the private sector, which includes private insurance premiums, co-payments, and out-of-pocket expenses for drugs, clinical consultations, and medical devices (Argentina 2011; Key Market 2010; Penchaszadeh et al. 2010). It is noted that there are significant geographical inequalities. For example, the per capita income in Buenos Aires City is double that of one of the poorest provinces (USD 10,000 versus 5,000), and the health expenditure in the former is 23 % of the budget, while it is only 10 % in the latter (Maceira 2009). While the Argentine health system has an overall good level of spending and has good human and structural resources, it suffers from significant segmentation, fragmentation, and inefficiency, financing inequalities, access barriers, and inequities in quality of care.
Congenital and genetic disorders’ burden
National surveys on genetic disorders’ prevalence, exposure to risk factors, and availability of registries
There are no national surveys nor registries of prevalence of genetic disorders nor of exposure to risk factors. A pilot study conducted by the Ministry of Health in 2007–2009 assessed the feasibility of implementing a national registry of congenital defects detectable at birth in selected hospitals (Liascovich et al. 2011). The same group is now expanding this registry to other provinces with the goal of eventually developing a national registry.
Total birth prevalence of congenital/genetic disorders per 1,000 live births
There are no national/provincial data on the prevalence of congenital/genetic conditions, except for those subject to newborn screening (see below). However, as stated above, a National Registry of Congenital Defects is being put in place (Liascovich et al. 2011). The closest estimation of prevalence at birth of congenital defects in Argentina is provided by the Latin American Collaborative Study of Congenital Malformations (ECLAMC), a voluntary registry (Castilla and Orioli 2004; Campaña et al. 2010). The most recent publication of the ECLAMC regarding frequency of congenital defects in Argentina lists the prevalence at birth of the 27 most frequent congenital anomalies (Table 1) (Campaña et al. 2010).
Table 1.
Prevalence at birth per 10,000 of 27 congenital anomalies in Argentina 1994–2007 (confidence interval 95 %; Campaña et al. 2010)
| Anomaly | Rate (CI 95 %) |
|---|---|
| Omphalocele | 2.9 (2.5–3.3) |
| Gastroschisis | 3.7 (3.3–4.1) |
| Anencephaly | 7.5 (6.9–8.1) |
| Spina bifida | 9.9 (9.2–10.6) |
| Hydrocephaly | 11.1 (10.4–11.8) |
| Cephalocele | 2.5 (2.2–2.9) |
| Microtia | 4.4 (4.0–4.9) |
| Cleft lip | 3.7 (3.3–4.1) |
| Cleft lip and palate | 10.2 (9.6–11.0) |
| Cleft palate | 4.7 (4.2–5.2) |
| Esophageal atresia | 3.8 (3.4–4.3) |
| Ano–rectal atresia | 5.8 (5.3–6.4) |
| Truncal heart defect | 5.0 (4.5–5.5) |
| ASD | 2.9 (2.6–3.3) |
| VSD | 12.0 (11.3–12.8) |
| Ambiguous genitalia | 1.6 (1.4–1.9) |
| Severe hypospadias | 3.3 (3.0–3.7) |
| Renal agenesis | 2.5 (2.2–2.9) |
| Polycystic kidneys | 3.3 (2.9–3.7) |
| Hydronephrosis | 4.9 (4.4–5.4) |
| Polydactyly, postaxial | 11.2 (10.5–11.9) |
| Polydactyly, preaxial | 3.7 (3.3–4.1) |
| Limb reduction, transverse terminal | 3.0 (2.7–3.4) |
| Limb reduction, longitudinal preaxial | 1.8 (1.3–1.9) |
| Diaphragmatic hernia | 4.1 (3.7–4.6) |
| Agenesis of pectoral | 1.0 (0.8–1.2) |
| Down syndrome | 19.6 (18.7–20.6) |
Single-gene disorders
There are no “country specific” recessive diseases in Argentina. Newborn screening detects three autosomal recessive conditions. Their birth prevalences are: PKU 1/30,000, cystic fibrosis 1/9,000, and congenital adrenal hyperplasia 1/15,000 (Chertkoff et al. 1997; Visich et al. 2002; Pesquisa Neonatal 2007). Geographical clusters of single-gene disorders, usually due to founder effects, have been described but are rare (Castilla and Sod 1990). Two of the most conspicuous are of Sandhoff disease in Cordoba province (Dodelson de Kremer et al. 1987) and oculocutaneous albinism in La Rioja province (Castilla and Adams 1996). Beta thalassemia is a common recessive disease as Italian ancestry is reported by close to 50 % of the population; however, there are no birth prevalence data, and no clusters have been described (Feliu-Torres et al. 2002).
Chromosomal anomalies
There are no data on birth prevalence of selected "common" chromosomal disorders, except for Down syndrome, based largely on clinical diagnosis. According to ECLAMC, the prevalence at birth of Down syndrome in selected Argentine hospitals is 1.96 per 1,000 live births (Campaña et al. 2010).
Neural tube defects
According to ECLAMC (Campaña et al. 2010), the birth prevalence of neural tube defects per 1,000 live births in selected Argentine hospitals is:
Anencephaly, 0.75
Spina bifida, 0.99
Cephalocele, 0.25
All neural tube defects, 1.99
Percentage of infant mortality due to congenital/genetic disorders
A total of 2,787 deaths in 2009 were due to congenital defects (0.9 % of the total number of 304,525 deaths), 2,257 of them (81 %) occurring under 1 year of age. The percentage of all neonatal deaths due to congenital defects was 41.2 %; the percentage of infant deaths under 1 year of age due to congenital/genetic disorders was 24.7 %; and among children under 5, 21. 8 % (Argentina 2009b). The percentage of pediatric hospital admissions due to congenital disorders/genetic disease is unknown. It is estimated that 55 % of neonatal mortality is reducible (34.2 % by early diagnosis and treatment during gestation, 10 % by early diagnosis at delivery, and 11.9 %by early diagnosis in the newborn). Forty-two percent of post-neonatal mortality is preventable via known care and prevention strategies (Argentina 2009b).
The exposure to known risk factors that impact the prevalence of congenital/genetic disorders at birth includes:
Advanced maternal age, 8 %
Consanguineous marriage, under 1 %, not felt to be a significant factor
While migrant populations are significant in number, migration is not felt to be a significant risk factor for congenital defects
Exposure to teratogens: unknown, albeit estimated to be a significant cause of congenital defects
Noncommunicable diseases
Noncommunicable diseases are major contributors to morbidity and mortality of the adult population. Of the total number of 304,525 deaths in 2009, 89,916 (29.6 %) were accounted for by cardiovascular diseases, 57,590 (19 %) by malignancies, 18,572 (6 %) by cerebrovascular diseases, and 7,701 (2.5 %) by diabetes. Their prevention is approached in the traditional public health model of identification of, and reduction of exposure to, known environmental risk factors. Genetic susceptibility testing is not a part of public policy for any medical condition.
While it is known that noncommunicable diseases have a genetic component, their rise in incidence and prevalence in Argentina, as well as in the rest of the world, is due to changes in lifestyles and other environmental factors, although no detailed information is available. Their impact on population health should be addressed by environmental changes that favor healthy lifestyles that avoid exposures to toxins and other deleterious factors, such as unhealthy diets, tobacco smoking, and sedentarism. On the other hand, genetic testing to detect possible genetic “susceptibility” to the effect of environmental factors is not felt to be an effective and feasible strategy to control common diseases at the population level.
Availability of genetic services
Clinical genetic and cytogenetic services developed in Argentina in the late 1960s in a few public hospitals, led by physicians trained abroad. In 1970, the Ministry of Health created a National Center of Medical Genetics to conduct epidemiological research on genetic conditions and training in medical genetics. In the mid-seventies, many medical geneticists left the country because of the military dictatorship. A national survey of the public health system in 2007 counted 41 genetic units in public hospitals in Argentina, defined as a clinical entity staffed by clinical geneticists which also provides access to laboratory diagnosis (the private sector was not surveyed, and hence, there is no information). Most genetic units are staffed by a single clinical geneticist without laboratory. About 15 units have cytogenetic laboratories, and only 5 perform DNA analysis. Only five genetic units conform to the notion of a comprehensive genetic center (Alba et al. 2007; Barreiro 2007).
These genetic services are part of the vast network of 1,319 public hospitals (with a total of 76,885 beds) and 6,290 primary health care centers throughout the country. Primary health centers are staffed variably, with many of them relying in community health workers and nurses rather than physicians. Some hospital genetic services perform outreach to health centers within their area of influence, but all too often patients affected with genetic conditions must find their own way to a tertiary hospital to find genetic services. Some of the few comprehensive genetic centers in tertiary hospitals run telemedicine programs for genetic consultations accessible to secondary and primary care hospitals in the provinces.
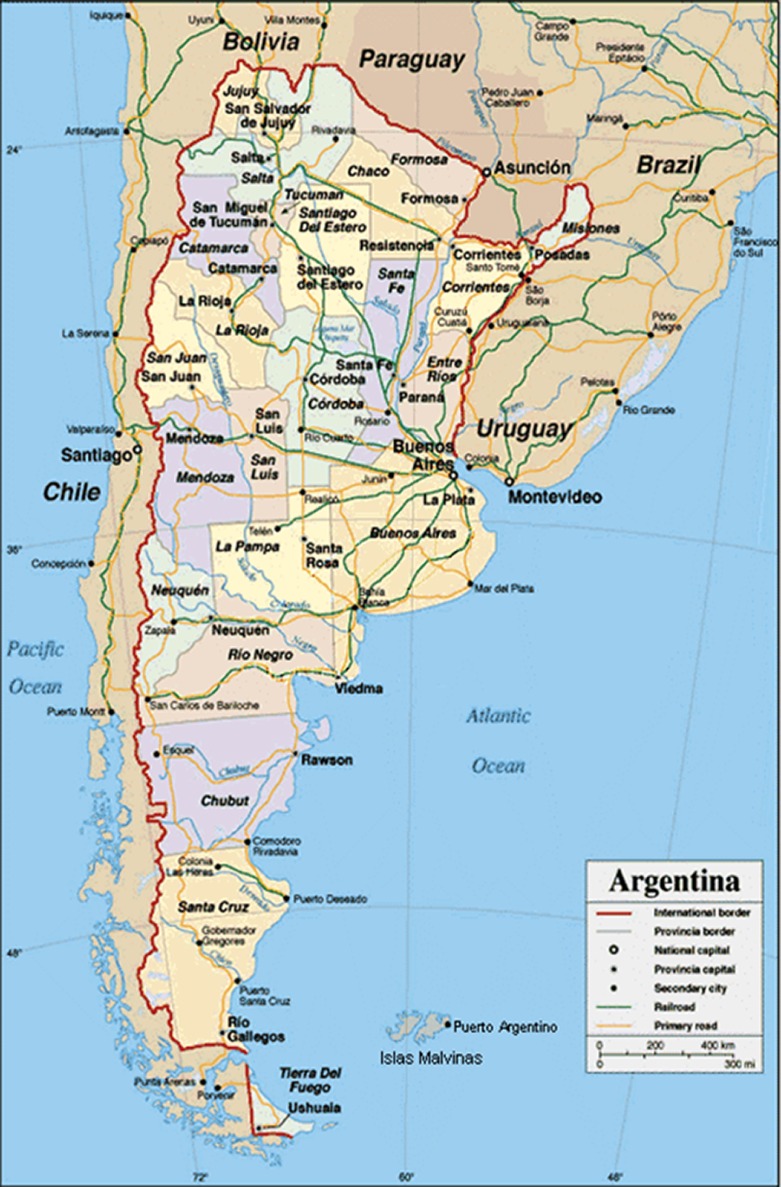
Currently, about 120 clinical geneticists certified by the Argentine Society of Genetics staff the 41 existing clinical genetics units, mostly in pediatric and maternity public hospitals of major cities and academic centers. The distribution by province of the 78 clinical geneticists who answered the survey (Alba et al. 2007) and the population of each province are shown in Table 2, while the map of the country can be seen in Fig. 1. Clinical geneticists provide genetic consultations and counseling, mostly for single-gene disorders and congenital disorders in children and newborns, while genetic services for adults are much less developed.
Table 2.
Population, number of genetic units, and number of clinical geneticists by province and the City of Buenos Aires (INDEC 2010; Alba et al. 2007)
| Province | Population | Genetic units | Clinical geneticists |
|---|---|---|---|
| Buenos Aires | 15,594,428 | 8 | 30 |
| Buenos Aires City | 2,891,082 | 9 | 22 |
| Catamarca | 367,820 | – | – |
| Chaco | 1,053,466 | – | – |
| Chubut | 506,668 | – | – |
| Cordoba | 3,304,825 | 6 | 8 |
| Corrientes | 993,338 | 1 | 2 |
| Formosa | 527,895 | – | – |
| Jujuy | 672,260 | 1 | 1 |
| La Pampa | 316,940 | – | – |
| La Rioja | 331,847 | – | – |
| Mendoza | 1,741,610 | 3 | 5 |
| Misiones | 1,097,829 | 3 | 2 |
| Neuquen | 550,344 | 1 | 1 |
| Rio Negro | 633,374 | 1 | 1 |
| Salta | 1,215,207 | 1 | 1 |
| San Juan | 680,427 | 1 | 1 |
| San Luis | 431,588 | – | – |
| Santa Cruz | 272,524 | 1 | 1 |
| Santa Fe | 3,200,736 | 3 | 2 |
| Santiago del Estero | 896,461 | – | – |
| Tierra del Fuego | 196,190 | 1 | 1 |
| Tucuman | 1,448,200 | 1 | 1 |
| Total | 40,091,359 | 41 | 78 |
Fig. 1.
Map of Argentina showing the City of Buenos Aires and the 24 provinces and their city capitals
Understaffing and long waiting lists are a problem in the genetic units surveyed. Overall, about 20 % of pediatric patients in tertiary care centers present a condition caused by a congenital defect, a single-gene disorder, or a chromosome abnormality. (Argentina 2007). These patients are rarely diagnosed in the primary or secondary levels of care. A survey on eight of the busiest genetic units in pediatric hospitals in six different jurisdictions reported 18,138 first-time visits in a 5-year period (2001–2006): 40 % with a single-gene disorder, 23 % with congenital disorders and/or mental retardation, and 13 % with a chromosome abnormality (Barreiro 2009a).
Folic acid fortification for staple foods is mandated by law. Family planning clinics and contraception are reasonably available throughout the country, notwithstanding some hurdles determined by the opposition of the Catholic church and other extremely conservative groups. On the other hand, there is very little genetic preconception care in Argentina.
Newborn screening for PKU mandated by law started in 1986, while congenital hypothyroidism (CH) was added in 1990 and cystic fibrosis (CF) in 1995. Implementation, however, began much later and has varied markedly by jurisdiction and health subsector. The tests are performed in a variety of laboratories, either in public hospitals or contracted to private labs, with little quality control. By 2007, 74 % of the provinces were testing for PKU and CH. Of those, 40 % were also screening for CF and 10 % for galactosemia (Argentina 2009a). Population coverage has correlated with resources, political will, and degree of development and organization of health services. In one third of jurisdictions providing newborn screening, coverage was less than 50 % (Argentina 2009b). The highest coverage (close to 100 %) occurs in the City of Buenos Aires (30,000 births per year), with the following prevalence per 1,000 live births among 150,000 babies tested between 2001 and 2005 (Pesquisa Neonatal 2007): PKU (0.33 per 1,000), congenital hypothyroidism (0.5 per 1,000), congenital adrenal hyperplasia (0.66 per 1,000), cystic fibrosis (0.11 per 1,000), Chagas disease (0.62 per 1,000), and syphilis (5.4 per 1,000). There are no data on follow-up and long-term management of affected infants, which presumably is very variable. In 2007, a new law was passed by Congress mandating newborn screening in all the territories of the country for PKU, CH, CF, galactosemia, congenital adrenal hyperplasia, biotinidase deficiency, retinopathy of prematurity, Chagas disease, and syphilis (Argentina 2007). The law states that the public sector and social security insurance must cover the expenses of screening and treatment for these disorders.
Special care facilities for children with disabilities due to congenital defects do exist but are scarce and poorly staffed, particularly those in the public sector. Their accessibility is restricted by economic, geographic, and bureaucratic barriers. The higher the social class of the patient and its proximity to a large city, the higher the chances of access to these scarce facilities.
Access to genetic services
There are multiple barriers to access to genetic services in Argentina as a consequence of lack of knowledge and political will by policy makers, shortage of funds, lack of perceived favorable cost/benefits ratio, and low priority assigned to genetic services. This is expressed in economic, geographic, and bureaucratic barriers, as well as underfinancing and understaffing of genetic service units.
Furthermore, social and private insurance plans rarely cover services for genetic conditions. Thus, barriers to access to genetic services within Argentina include:
Financial barriers (not being able to afford the costs of a test/service)
Geographical barriers (not enough medical genetic services in a particular area)
Untimely access (excessive waiting time, delayed diagnosis)
Unavailability of some diagnostic tests
A special barrier is constituted by the illegality of abortion for fetal indications. Voluntary abortion is a crime in Argentina, except to protect the life or health of the mother, or in cases of rape. While this restriction has not reduced the 500,000 estimated voluntary abortions that occur annually in the country (Zamberlin 2007), it has effectively prevented the development of prenatal diagnosis services within the public and social security health systems. There are no accepted fetal indications for legal terminations of pregnancy (except for anencephaly, thanks to an intervention of the Supreme Court in a recent landmark case), although they are widely practiced by middle-upper class couples in the private sector.
State of genetic services
Human resources and training
The following figures describe the Argentine state of health care workforce (Argentina 2011):
Number of physicians and density per 10,000 population (2000–2007), 121,076 (33.5 per 10,000)
Number of nursing and midwifery personnel and density per 10,000 population (2000–2007), 12,614 (3.5 per 10,000); non-certified nurses, 100,000 (28 per 10,000)
Number of other health workers and density per 10,000 population (2000–2007), 60,000; 17 per 10,000)
These figures reveal that there is no shortage of physicians, but definitely of nurses. Furthermore, physicians tend to concentrate in large cities and specialize in income-generating specialties, neglecting underserved areas and primary care focus. Genetics knowledge of physicians is poor as most medical schools do not include meaningful teaching in genetics in their curricula.
Argentina counts since the 1980s with a single accredited 4-year residence program in medical genetics for physicians, located in the City of Buenos Aires and run by the National Medical Genetics Center of the Ministry of Health, with two to three graduates per year. Other opportunities for training in medical genetics, short of a formal residence, exist in the University Hospital of Buenos Aires, the National Pediatric Hospital Garrahan, and the Centro de Educaciones Médicas e Investigaciones Clínicas, all in Buenos Aires. In addition, there are short courses in medical genetics and genetic counseling available for nongenetic health professionals, organized by academic centers and professional associations. Short courses directed at primary care health professionals and general physicians are conducted in urban and rural settings.
A special program of training primary care health professionals in several underserved provinces started in 2007 with partial funding from the Capability Project of Framework 6 of the EU, and now is continuing with government support (Barreiro 2009a, b). In addition, there are postgraduate training programs in biochemical, cytogenetic, and molecular genetics for Ph.D professionals, but highly variable in scope and unknown number of graduates.
The specialty of medical genetics is recognized by the Ministry of Health since 1991. The Argentine Society of Genetics, in conjunction with the Ministry of Health, has certified about 120 clinical geneticists who staff 41 clinical genetics units throughout the country or work in private practice, providing genetic consultations and counseling.
Non-physician genetic counselors are not a recognized or registered profession, and there is no formal postgraduate training in genetic counseling. Genetic counseling in Argentina is a physician responsibility and is provided by clinical geneticists or other physicians with genetics training. There are no genetic counselors trained abroad who work in Argentina nor are there are plans to train them locally in master’s programs or from the nursing profession.
Workload
The estimated average workload of genetic consultations (patient seen by a clinical geneticist and usually requiring physical examination) per health care professional per year in the public sector varies from 100 to 1,000 per professional per year, depending on the setting.
Genetic testing
Cytogenetics
About 15 of the 41 genetic units in the public system and academic centers perform cytogenetic analyses, including molecular cytogenetics in some units. Because of the ban on abortion for fetal indications, there is virtually no prenatal chromosome diagnosis in public hospitals. In contrast, there is a sprawling private market for prenatal screening and fetal chromosome testing with no quality control.
DNA testing
There are approximately 12 centers that perform DNA testing, concentrated in Buenos Aires and a few other major cities. DNA testing is conducted primarily for diagnostic purposes in individuals with symptoms, and only rarely for predictive purposes in healthy individuals.
The most common conditions tested are:
Fragile X,
Congenital adrenal hyperplasia
Duchenne muscular dystrophy,
Myotonic dystrophy
Beta thalassemia
Hemophilias
Achondroplasia and hypochondroplasia
Breast cancer (BRCA1 and BRCA2)
Thyroid cancer
MEN 1 and 2
Presymptomatic diagnosis of Huntington disease and other late-onset neurological diseases is generally coordinated by neurologists with the support of clinical geneticists and supported by DNA testing performed locally in very few laboratories or sent abroad. A similar situation occurs with cancer genetic counseling and testing and with cardiogenetics and other specialized clinics, which is usually under the purview of the medical specialist with occasional input of a clinical geneticist. While there are no data about direct-to-consumer genetic testing in Argentina, the presumption is that the interest and uptake are very low.
Number of tests, fees, and reimbursement
The number of genetic tests performed countrywide is very difficult to obtain. As already mentioned, there are no data on prenatal cytogenetic diagnosis, performed exclusively in the private sector. Tables 2 and 3 show the number of chromosome and DNA tests, performed annually and respectively between 1998 and 2008 and between 1999 and 2009 at the National Pediatric Hospital Garrahan of Buenos Aires, which probably performs about one half of all genetic tests in the country (Table 4). From this data, one can infer the following annual numbers countrywide:
Chromosome analyses, non-prenatal, 5,500
Chromosome analysis, prenatal, performed in the private sector, numbers unknown
DNA tests (diagnostic, non-prenatal), 2,200
Table 3.
Chromosome tests performed in 1998–2008
| Year | G bands peripheral blood | FISH | Bone marrow | Solid tumor | Chromosome instability | High resolution | Total |
|---|---|---|---|---|---|---|---|
| 1998 | 1,026 | 0 | 425 | 28 | 88 | 230 | 1,797 |
| 1999 | 976 | 122 | 431 | 38 | 56 | 233 | 1,856 |
| 2000 | 1,027 | 167 | 438 | 22 | 66 | 180 | 1,900 |
| 2001 | 1,004 | 263 | 624 | 44 | 73 | 209 | 2,217 |
| 2002 | 929 | 191 | 699 | 30 | 99 | 154 | 2,102 |
| 2003 | 1,029 | 219 | 777 | 33 | 78 | 237 | 2,373 |
| 2004 | 997 | 241 | 737 | 49 | 113 | 247 | 3,381 |
| 2005 | 988 | 351 | 729 | 63 | 126 | 232 | 2,489 |
| 2006 | 1,103 | 426 | 680 | 54 | 99 | 298 | 3,763 |
| 2007 | 1,172 | 267 | 784 | 54 | 101 | 327 | 3,877 |
| 2008 | 1,193 | 191 | 680 | 45 | 121 | 377 | 2,607 |
| 2009 | 1,198 | 192 | 590 | 27 | 168 | 444 | 2,619 |
| 12,642 | 2,630 | 7,594 | 487 | 1,188 | 3,168 | 30,981 |
National Pediatric Hospital Garrahan. Buenos Aires (no prenatal tests)
Table 4.
DNA-based tests
| Test | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fragile X | 146 | 111 | 172 | 106 | 174 | 129 | 137 | 165 | 196 | 223 | 182 |
| Cystic fibrosis DeltaF508 | 153 | 172 | 91 | 106 | 149 | 122 | 123 | 154 | 156 | 156 | 161 |
| Cystic fibrosis 29–31 mutatione | 85 | 101 | 94 | 78 | 112 | 149 | 163 | 231 | 215 | 252 | 212 |
| Cystic fibrosis linkage | 36 | 12 | 19 | 20 | 17 | 3 | 11 | 17 | 11 | 12 | 9 |
| Prader–Willi–Angelman methylation | 45 | 66 | 58 | 53 | 74 | 71 | 65 | 70 | 57 | 83 | 96 |
| DANN extraction | 80 | 101 | 190 | 100 | 111 | 169 | 165 | 129 | 115 | 106 | 160 |
| SMA (exon 7 y 8) | 36 | 47 | 47 | 35 | 47 | 46 | 54 | 63 | 61 | 70 | 64 |
| Miotónic Dystrophyde Steinert, Southern Blot | 21 | 49 | 36 | 51 | 44 | 55 | 55 | 74 | |||
| Achondroplasia | 8 | 0 | 26 | 20 | 21 | 9 | 19 | 12 | |||
| Hypocohndroplasia | 10 | 0 | 26 | 20 | 21 | 11 | 17 | 13 | |||
| Prader–Willi–Angelman linkage | 66 | 46 | 34 | 24 | 3 | 7 | 13 | ||||
| Conexin 26 | 21 | 28 | 25 | 38 | 15 | 20 | |||||
| Conexin 30 | 26 | 13 | 21 | ||||||||
| Mytochondrial mutation A1555G | 15 | 14 | 9 | ||||||||
| MTHFR (C677T y A1298C) | 17 | 10 | 87 | ||||||||
| Pharmacogenettics TPMT | 33 | 15 | 47 | ||||||||
| Friedreich’s Ataxia | 2 | 2 | |||||||||
| Total | 581 | 610 | 671 | 537 | 799 | 844 | 871 | 964 | 1,018 | 1,069 | 1,182 |
Pediatric Hospital Garrahan Buenos Aires (1999–2009)
While genetic services in the public system are provided free of charge, some labs from academic centers usually charge a nominal fee. The coverage by the social security and private insurance is highly variable. Predictive testing is rarely performed.
Prevention of congenital and genetic disorders
With the exception of folic acid fortification and rubella immunization, and occasional campaigns against alcohol intake in pregnancy, there are no specific programs for the prevention of congenital defects
Cultural and social issues pertaining to medical genetic services
The main cultural and social issues pertaining to medical genetic services in Argentina stem from the lack of genetic literacy among the population and the paucity of services available throughout the country. Furthermore, coverage for genetic services by private and social insurance is very poor, which leads to discrimination and stigmatization of people with genetic disabilities. The lack of prenatal genetic services in the public sector and the prohibition of abortion for fetal reasons increase the stress and suffering of families affected with genetic conditions. Low social class, low education level, and adherence to conservative religious precepts are associated to a high emotional burden from genetic defects.
National policies and legal frameworks
There are no national guidelines or recommendations for the provision of medical genetic services, including ethical guidelines. The national policies and legal frameworks regarding medical genetics are within the responsibility of the national Ministry of Health. In turn, the Ministry of Health of Argentina has been influenced by experts in medical genetics from the Pan American Health Organization (PAHO). Since 1982, PAHO has sporadically been convening regional consultations of experts in medical genetics, which in turn issued recommendations to member countries, including Argentina (PAHO 1984; Penchaszadeh and Beiguelman 1998; Kofman‐Alfaro and Penchaszadeh 2004; Penchaszadeh 2004; PAHO 2007a; PAHO 2007b). A special consultation took place in Argentina in 2003, in which specific recommendations were issued by the consultant, including the appointment of a blue ribbon National Commission on Genetics and Health that would have the task of surveying the status of medical genetics services in the country and pointing needs for development (Penchaszadeh 2003). This National Commission was created in 2006 and has since conducted a countrywide survey of genetic services and formulated a plan for their strengthening and coordination (Alba et al. 2007). Currently, the Ministry of Health has adopted as a national policy this Report of the National Commission and has been strengthening the network of genetic services in the public sector as well as developing a nationwide registry of congenital anomalies, which has already started in the northeastern provinces of the country (Liascovich et al. 2011). In addition, the National Pediatric Hospìtal Garrahan, which hosts the largest medical genetics department in the country, is leading a capacity building training program in clinical genetics addressed to primary health professionals in disadvantaged areas of the country, following the model implemented by the CAPABILITY project mentioned above.
Clinical laboratories are accredited by special agencies of the ministries of health. Accreditation requirements revolve around proper training of the director, physical space, equipment, handling of hazardous materials, and safety matters. Except for laboratories that perform newborn screening, there are no official agencies that control or monitor the analytical validity of tests. Quality assessment of laboratory results relies mostly on the voluntary decision of the lab directors to participate in a quality control program, usually of an international agency (Penchaszadeh and Aguiar 2009).
Chromosome and DNA studies are performed in the laboratories of public hospitals, mostly teaching hospitals, or by private laboratories. Genetic tests are usually under the responsibility of professionals with a degree equivalent to a Ph.D., who perform cytogenetic, biochemical, and molecular genetic testing, assisted by technical staff. DNA tests are performed locally only for a handful of conditions, the remainder are sent abroad on a fee-for-service basis. While these laboratories are certified by a state agency, participation in quality assessment programs is voluntary and regulation very lax, with little government oversight (Penchaszadeh and Aguiar 2009).
Research priorities in genetics/genomics
Biomedical research in Argentina has a long tradition in academic centers with three Nobel prizes in this field. The National Council for Scientific and Technological Research has existed for 50 years (www.conicet.gov.ar). The Ministry of Health funds public health research projects, including in genetics/genomics (www.msal.gov.ar/htm/Site/salud_investiga/index.html). Genetics/genomics research is conducted in several centers, such as the Department of Molecular Biology of the University of Buenos Aires (www.fcen.uba.ar), the Instituto de Investigaciones de Ingenieria Genetica y Biologia Molecular (www.conicet.gov.ar/php/datos_inst.php?n=02650), the Fundacion Leloir. (www.leloir.org.ar), the Instituto Multidisciplinario de Biología Celular (WWW.imbice.org.ar), and the Instituto de Biología Molecular y Celular of the Universidad Nacional de Rosario (www.ibr.gov.ar).
An epidemiologic study of factors associated with congenital anomalies has been in operation for 43 years in Argentina and South America: the Latin American Collaborative Study on Congenital Malformations (ECLAMC) (Castilla and Orioli 2004). This research provides baselines for the prevalence of congenital anomalies in the region and is now studying their molecular basis (Campaña et al. 2010).
Specific areas of genetics/genomics research are: basic molecular genetics, immunogenetics, molecular population genetics, forensic genetics, genome sequencing (the Trypanosoma cruzi genome was sequenced by a multinational team in which Argentine geneticists from two separate institutions played a key role), gene therapy, and stem cell research. Research in clinical genetics is concentrated in dysmorphology–cytogenetics, selected single-gene disorders such as skeletal dysplasias, muscular dystrophies, fragile X syndrome, cystic fibrosis, thalassemia, congenital deafness, and cancer (Penchaszadeh 2008).
In 2009, the Ministry of Health convened a large group of geneticists conducting research to discuss priorities in genetics research. However, the results of this exercise have not been disseminated nor acted upon. That same year, a newly created Ministry of Science and Technology began a concerted effort with the Ministry of Health and the private sector for research and development in genomic approaches in biotechnology and biomedical research, for which it has issued a number of calls for projects, with particular emphasis in public–private partnerships.
In the late 1980s and 1990s, genetic testing was utilized to identify children who had been appropriated by the military during the dictatorship (Penchaszadeh 1997). A National Genetic Data Bank was created to store DNA samples of living relatives and perform DNA testing to claimants and individuals presumed to be children of the disappeared, which led so far to 105 children and young adults recovering their true identity along 25 years of work (Penchaszadeh 1997, 2011). In 2007, the Argentine Forensic Anthropology Team was awarded a large grant by the US Department of State to perform DNA tests in about 800 unidentified remains recovered from mass and/or unnamed graves in cemeteries, presumed to be of persons disappeared by the military. DNA from the remains is matched with persons who have a relative who disappeared and provided DNA samples for the study. So far, remains from about 100 individuals have been identified (Equipo Argentino de Antropología Forense 2007).
Patient organizations and public education in genetics
In Argentina, there is a long tradition of development of patient organizations as advocates for services and research on a variety of medical conditions. Most of these organizations link with health professionals and research scientists to stimulate the development of new treatments and prevention strategies. In the recent past, the field of “rare diseases” has captured the interest of health professionals, scientists, and politicians. While most patients’ organizations deal with a particular condition, there has been recently a tendency toward union in umbrella groups. One such umbrella group is the Fundacion Geiser (Fundacion Geiser 2010). Further, the Ministry of Science and Technology funded a research project on the needs of patients and families with rare diseases, which detailed those needs and presented them to Congress in 2009 (Liljesthrom and Armando 2009). The number and strength of patient organizations in Argentina are growing, and recently, Congress passed a law to support the needs of patients with rare diseases and their families, making their coverage by insurance plans mandatory.
Conclusion
The Ministry of Health has recently shown interest in improving access to and performance of the clinical genetics services throughout the country. A National Commission on Genetics and Health, appointed in 2005, conducted countrywide studies on the situation of genetic services (Ministry of Health 2008). In 2007, the Commission submitted a proposal to the Ministry for their improvement. The proposal asked that the number of positions of clinical geneticists in public hospitals be increased and that the laboratory equipment for cytogenetics and molecular genetics in several hospitals countrywide be modernized and expanded. The Commission conducted a survey of genetic services and proposed the organization of a network of genetic services to maximize their efficiency, avoid duplication of services, and channel referrals in a regionalized manner (Alba et al. 2007).
Acting on such recommendations, in 2010 the Ministry of Health started some actions to improve the capacity of the existing genetic units in the public system. Barriers are mainly bureaucratic as each province has its own set of policies and budget, and the Ministry of Health does not have much leverage or resources to impose policies. In addition, a National Register of Congenital Defects is beginning, with pilots in selected provinces (Liascovich et al. 2011). Finally, the National Pediatric Hospital Garrahan has taken a leadership role in conducting training in clinical genetics for primary care health personnel in several underserved areas of the country.
Acknowledgments
The survey was supported by (1) the "Institute for Health and Consumer Protection" (Italy), one of the seven scientific institutes of the Joint Research Centre (JRC) of the European Commission; (2) the Department of Human Genetics, Hannover Medical School, Hannover, Germany; and (3) the Unit of Women's Health Research, Medical School, Westfaelische Wilhelms-Universitaet Muenster, Muenster, Germany. I am indebted to many colleagues for providing me with information, particularly Dr. Cristina Barreiro of the Genetic Service of the National Pediatric Hospital Garrahan and Rosa Liascovich from the National Medical Genetics Center of the Ministry of Health.
References
- Alba A, Barbero P, Barreiro C, Chertkoff L, Dain L, Ferreiro V, Francipane L, Frechtel G, Gallego M, Liascovich R, Meroni ME, Rozental S (2007) Diseño y organización de una Red Nacional de Genética Médica (Design and organization of a national network of medical genetics.) Spanish. Unpublished, available from the author
- Argentina (2007) Ministerio de Salud. Text of the newborn screening law (Spanish). Available at: http://test.e-legis-ar.msal.gov.ar/leisref/public/showAct.php?id=6601. Accessed 8 April 2012
- Argentina (2009a) Ministerio de Salud. Newborn screening program (Spanish). 2009. Accessible at: http://www.msal.gov.ar/htm/Site/promin/UCMISALUD/index.htm
- Argentina (2009b) Ministerio de Salud, Departamento de Estadística e Información de Salud. Accessible at: http://msal.gov.ar/htm/site/estadisticas.asp
- Argentina (2011) Basic Indicators. Ministry of Health and Pan American Health Organization. Accessible at: www.msal.gov.ar
- Barreiro C (2007) Collaborative Study on Clinical Genetics. Argentina. Ministerio de Salud. Comisión Salud Investiga. Spanish. 2007. Accessible at: http://www.msal.gov.ar/htm/site/salud_investiga/ecm.asp
- Barreiro C (2009a) Needs Assessment Capability Project Argentina. Report to Capability Project of European Union. Available at: www.capabilitynet.eu
- Barreiro C (2009b) Chaco outreach project. The development of a primary health care-based medical genetic service. Report to Capability Project of European Union. Available at: www.capabilitynet.eu [DOI] [PMC free article] [PubMed]
- Campaña H, Pawluk MS, López Camelo JS, ECLAMC Study Group Birth prevalence of 27 selected congenital anomalies in 7 geographic regions of Argentina. Arch Arg Pediatr. 2010;108(5):409–417. doi: 10.1590/S0325-00752010000500006. [DOI] [PubMed] [Google Scholar]
- Castilla EE, Adams J. Genealogical information and the structure of rural Latin-American populations: reality and fantasy. Hum Hered. 1996;46(5):241–255. doi: 10.1159/000154361. [DOI] [PubMed] [Google Scholar]
- Castilla EE, Orioli IM. ECLAMC: the Latin-American collaborative study of congenital malformations. Community Genet. 2004;7(2–3):76–94. doi: 10.1159/000080776. [DOI] [PubMed] [Google Scholar]
- Castilla EE, Sod R. The surveillance of birth defects in South America II. The search for geographic clusters: endemics. Adv Mutag Res. 1990;2:211–230. doi: 10.1007/978-3-642-75599-6_7. [DOI] [Google Scholar]
- Castilla EE, Gomez MA, Lopez-Camelo JS, Paz JE. Frequency of first cousin marriages from civil marriage certificates in Argentina. Hum Bio. 1991;63:203–210. [PubMed] [Google Scholar]
- Chertkoff L, Visich A, Bienvenu T, Grenoville M, Segal E, Carniglia L, Kaplan JC, Barreiro C. Spectrum of CFTR mutations in Argentine cystic fibrosis patients. Clin Genet. 1997;51(1):43–47. doi: 10.1111/j.1399-0004.1997.tb02413.x. [DOI] [PubMed] [Google Scholar]
- Equipo Argentino de Antropología Forense (2007) Spanish. Available at: http://desaparecidos.org/notas/2007/11/arg-eaaf-solicita-muestras-de.html
- Dodelson de Kremer R, Depetris de Boldini C, Paschini de Capra A, Pons de Veritier P, Goldenhersch H, Corbella L, Sembaj A, Martín S, Kremer I, Mass L, et al. Estimation of heterozygote frequency of Sandhoff disease in a high-risk Argentinian population. Predictive assignment of the genotype through statistical analysis. Medicina (Buenos Aires) 1987;47(5):455–463. [PubMed] [Google Scholar]
- Feliu-Torres A, Bonduel M, Schiuccati G, del Pozo A, et al. Beta talasemia en la Argentina. Medicina. 2002;62:124–134. [PubMed] [Google Scholar]
- Fundacion Geiser (2010) Accessible at: www.fundaciongeiser.org. Accessed 8 April 2012
- INDEC (2010) National Institute for Statistics and Census. Accessible at: www.indec.mecon.ar
- Key Market (2010) La salud en el país: cuánto se gasta y quién la paga. Health in the country: how much it is spent, and who pays. Published in: Clarin, 23 May 2010. Accessible at: http://www.ieco.clarin.com/economia/salud-pais-gasta-paga_0_133500002.html
- Kofman-Alfaro S, Penchaszadeh VB. Community genetic services in Latin America and regional network of genetic services. Community Genet. 2004;7:157–159. doi: 10.1159/000080789. [DOI] [PubMed] [Google Scholar]
- Liascovich R, Rittler M, Castilla EE. Consanguinity in South America: demographic aspects. Hum Hered. 2001;51(1–2):27–34. doi: 10.1159/000022956. [DOI] [PubMed] [Google Scholar]
- Liascovich R, Gili J, Valdez R, Somaruga L, et al. Development of a national registry of congenital anomalies in Argentine: a pilot feasibility study. Rev Argent Salud Publica. 2011;2(6):6–11. [Google Scholar]
- Liljesthrom M, Armando R (2009) Las enfermedades poco frecuentes en la Argentina: un enfoque socio-sanitario, jurídico y de investigación científica. Propuestas comunicacionales y de políticas para reducir la vulnerabilidad. (Rare diseases in Argentina: an approach from social, health, legal and research viewpoints). Report presented to the Commission of Health Polilcy of the Argentine Congress. Available at: fwww.fundacionfop.org.ar
- Maceira D (2009) Inequidad en el acceso a la salud en la Argentina (Inequity in the access to the health system in Argentina). CIPPEC, Documento de Políticas Públicas/Análisis, n° 52. Available at: http://www.cippec.org/SALUD
- Martínez-Marignac VL, Bertoni B, Parra EJ, Bianchi NO. Characterization of admixture in an urban sample from Buenos Aires, Argentina, using uniparentally and biparentally inherited genetic markers. Hum Biol. 2004;76:543–557. doi: 10.1353/hub.2004.0058. [DOI] [PubMed] [Google Scholar]
- Ministry of Health (2008) Comisión Nacional de Genética y Salud. Design and organization of a national network of medical genetics. Spanish. Unpublished, available from the author
- Pan American Health Organization (1984) Prevention and control of genetic diseases and congenital defects. Report of an Advisory Group (Castilla EE, Penchaszadeh VB, Wertelecki W, Youlton R). Scientif Publ. 460. PAHO, Washington, DC
- Pan American Health Organization (2007a) Program on genetics, public health and human rights. Unpublished document. Available from the author, in Spanish.
- Pan American Health Organization (2007b) Recommendations for the development of genetics in public health in Latin America. Report of a meeting of experts. Rio de Janeiro, June 21, 2007. Unpublished document. Available from the author, in Spanish.
- Penchaszadeh VB. Genetic identification of children of the disappeared in Argentina. JAMWA. 1997;52(1):16–27. [PubMed] [Google Scholar]
- Penchaszadeh VB (2003) Medical Genetics in Argentina: Assessment and perspectives. Report of a Consultation to the Pan American Health Organization for the Ministry of Health of Argentina. Unpublished document, available from the author
- Penchaszadeh VB (2004) Medical genetics in Latin America (editorial). Community Genet 7(2–3):65–69 [DOI] [PubMed]
- Penchaszadeh VB. Argentina: public health genomics. Public Health Genomics. 2008;12:59–65. doi: 10.1159/000153429. [DOI] [PubMed] [Google Scholar]
- Penchaszadeh VB. Genetic admixture, identity and health in South America; dialogues between anthropology and genetics. New York: Palgrave Macmillan; 2011. Forced disappearance and suppression of identity of children in Argentina: experiences in genetic identification; pp. 213–243. [Google Scholar]
- Penchaszadeh VB, Aguiar MJB. Regulatory issues in clinical and laboratory genetics in developing countries. Examples from Latin America. In: Kristoffersson U, Cassiman JJ, Schmidtke J, editors. Quality issues in clinical genetic services. Heidelberg: Springer; 2009. [Google Scholar]
- Penchaszadeh VB, Beiguelman B. Medical genetics services in Latin America: report of a meeting of experts. Pan Am J Public Health. 1998;3(6):409–420. doi: 10.1590/S1020-49891998000600013. [DOI] [PubMed] [Google Scholar]
- Penchaszadeh VB, Leone F, Rovere M. The health system in Argentina: an unequal struggle between equity and the market. Italian J Public Health. 2010;7(4):350–358. [Google Scholar]
- Pesquisa Neonatal (2007) (Newborn screening). City of Buenos Aires. (Spanish) Available at: http://buenosaires.gov.ar/areas/salud/redes/archivos/datos_estadisticas_ppn.pdf
- Visich A, Zielenski J, Castaños C, Diez G, Grenoville M, Segal E, Barreiro C, Tsui LC, Chertkoff L. Complete screening of the CFTR gene in Argentine cystic fibrosis patients. Clin Genet. 2002;61(3):207–213. doi: 10.1034/j.1399-0004.2002.610307.x. [DOI] [PubMed] [Google Scholar]
- World Bank (2009) Available at: http://devdata.wordlbank.org/externatl/. Accessed 8 April 2012
- Zamberlin N (2007) Abortion in Argentina. Buenos Aires; CEDES/FEIM/IPPF; 2007. Spanish. Available at: www.cedes.org