Abstract
In recent years scientific progress has dramatically raised the potential of genetic services, but the actual benefits of these developments are not universally shared. In countries of low and middle incomes, improvements in genetic services frequently lag behind. Since this is generally caused by lack of resources and not by the lack of political will, the question arises, how can one most easily acquire the necessary capital to improve the health care in these areas. Public–private partnerships (PPPs) offer one approach to solve this issue, aiming at the inclusion of private enterprises in the realisation of public authority services. So far PPPs have been used exclusively in other health service areas. In this paper a first attempt is being made to discuss the feasibility of transferring the concept of PPP to genetic services, and consideration is given as to where the most promising starting point might be. We start by defining a multilevel structure that needs to be considered in providing comprehensive genetic care. We continue by explaining the concept of PPPs and their current types of implementation in medical services. We then examine how the PPP model could be applied to genetic services or sections thereof. We arrive at the conclusion that a likely starting point for PPP in genetic services is at the level of the infrastructure building service.
Increasing genetic proficiency and transforming genetic services into practice
The value of a rapidly increasing bank of genetic knowledge for health care can be appreciated only when it is being transferred from the phase of product development and process innovation (Bühner 2004; Jung 2006) into practice (Bell 1998; Bennett et al. 2010; Daiger 2005; Wright et al. 2010). But how is theoretical knowledge applied in medical services in a fast and effective manner (Burke et al. 2006)? Research results cannot be directly applied in practice; usually a long evaluation procedure is necessary to demonstrate efficacy and to ensure that it does not endanger the patient. The evaluation of new medical products typically takes many years before the patient can finally profit from its development. There are not only technical and scientific but also financial challenges to be overcome, including the establishment and stabilization of effective infrastructures with adequate staff and other resources.
To maintain a service long term, not only the costs must be considered but also demand, to include an adequate awareness of the needs and conditions of the targeted population. In this context regard to equal access to health care and social services must be taken into account. Thus, a comprehensive examination of the health system is a prerequisite to the foundation upon which genetic services can be built (Kaye 2001).
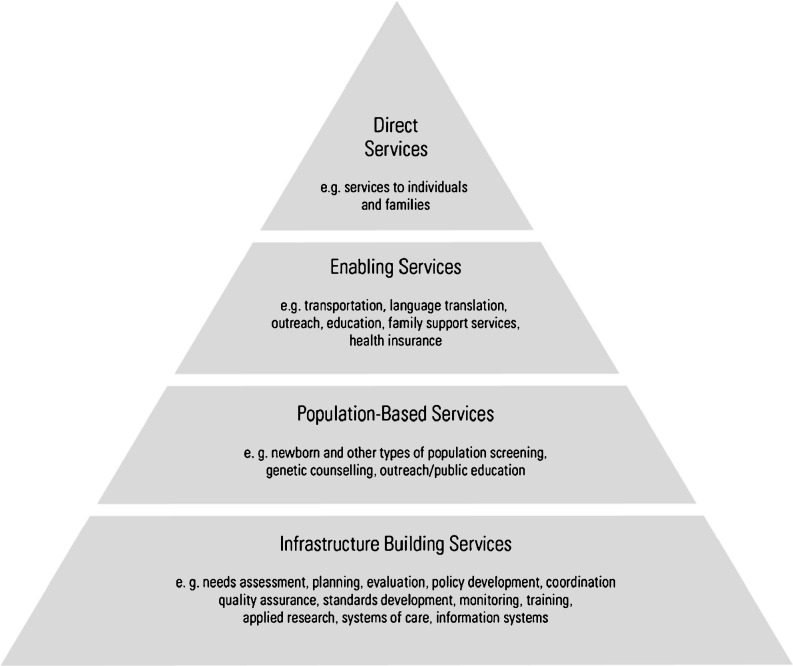
To ensure that scientific achievements are properly integrated into genetic care, changes may need to happen in the health system. For example, primary care practitioners will require training to be kept up to date with developments (Emery 2001). An efficient and effective transfer of knowledge requires multidisciplinary governance, including state oversight and professional self-regulation. We wish to illustrate this by adapting the conceptual framework of the Maternal and Child Health Bureau (2000). This document contains a concept that targets four levels of the health service with partially overlapping components.
The four levels can be characterised as follows (Fig. 1):
Fig. 1.
The pyramid of genetics in health care
Infrastructure building services
This level serves as a basis for effective installation of genetic services in health systems, as structural requirements are specified and basic decisions are made. Initially, legal framework and regulatory infrastructure must be developed. Further crucial issues are policy development, a planning system, a health needs assessment and strategy development. Organisational conditions must be created, so that genetic services in primary care can be applied. From a formal framework, standards and guidelines must be derived and practitioners must be educated and assessed. With the implementation of genetic services, it is necessary to collect data for applied research, for example evaluating consultation and referrals and quality assurance. To successfully build an infrastructure, all stakeholders, health professionals, healthcare providers, genetic services specialists, consumers and consumer groups should be actively included.
Population-based services
Building on the existing infrastructure, genetic services must be deployed by realizing specific application programs. Depending on the program, different population groups and different diseases are considered. The principle for these services is to be generally available and accessible for the whole population. Population-based services include preventive measures such as (a) preconception, (b) prenatal, (c) newborn metabolic screening, (d) newborn hearing screening, (e) paediatric developmental screening and (f) screening for adult-onset disorders. Furthermore, genetic counselling and public education are important factors for improved medical health care by genetic services.
Enabling services
Enabling services should assist in making genetic services available to the general public. Some sectors of the community may have little perspective of access to genetic services, or must first surmount specific barriers to care. These include, those on low income, geographically isolated, culturally disadvantaged or those with special and complex health needs (i.e. traditionally inadequately cared for). For many of these people, enabling services are essential—without them they are excluded from the available therapeutic services. Tangible examples of enabling services include transport, language translation, outreach, education, family support services, health insurance, care coordination, house visits and case management and they are commonly provided by agencies. In summary, enabling services are additional services so that a broader population can benefit from the existing programs.
Direct health care services
At this level, the clear applications of genetic services come into play. They are targeted at individual patients and operate when acute need or individual health requirements occur outside of the programmes, and may be provided by various professionals depending on availability and tradition, including clinical geneticists, genetic nurses, genetic counsellors, midwives, primary care practitioners, social workers and laboratory staff.
Lack of funds in emerging economies
Comprehensive medical genetic services are now widely available in the industrialized countries, while in the developing world health care policy is often forced to prioritise other sectors and only rarely includes adequate genetic services (Christianson et al. 2011).
Considering the determinate funds (Gwatkin and Guillot 1999), it is possible to redistribute the current resources by modifying the criteria for redistribution and rationing priorities within the offered services. Thereby some patients can get necessary access to additional health care, while medical provision can be reduced for another group of less needy patients. It is both essential and equitable to have a high index of transparency as it relates to the accordance of the responsible persons and/or health ministers. The prospect of this being attained depends on the political, ethical and economic will of the emerging country.
There are several possibilities to use the resources in a more efficient way. Economisation of some areas in health care would save resources that could be used for other purposes (Fozouni and Güntert 2000). For example, the public hospital sector could reduce costs through more efficient treatment and optimising organisational structures. This would reduce the essential costs of the hospital sector but keep the services offered intact. The freed financial resources could then be used for clinical genetic services.
Another solution is to increase the overall health care budget on principle. The increased budget would improve the health care authorities’ ability to meet the needs of the population. Capital would have to be raised by increasing taxes or social security contributions. Money could also be generated by redistributing other governmental financial resources, although this may come at the expense of social services. Private and publicly traded companies also present an alternative source of capital.
The most viable and non-disruptive model for a government would be to create a public–private partnership. As it is likely that the municipality cannot or is unable to perform its public duties alone, a public–private partnership (PPP) is a preferred option.
Public–private partnership
The PPP as a solution—history and increase in popularity
PPPs represent an innovation, which can narrow the gap between the rich and poor countries. It involves the close cooperation between the private and public sectors to make both financial and non-financial resources available for the desperately needed improvement of medical services in countries with low and middle incomes (Smith 2000; Yaïch 2009).
Public–private partnerships should be applied in those areas where economic incentives have failed and where the open market, insofar as it exists in the countries in question, has not been able to establish a balance between supply and demand (Ziemba 2004). In recent years the political and social will has changed towards a more dedicated pursuit of this concept. PPPs are now seen by many as a means towards improved health services (Bazzoli et al. 1997).
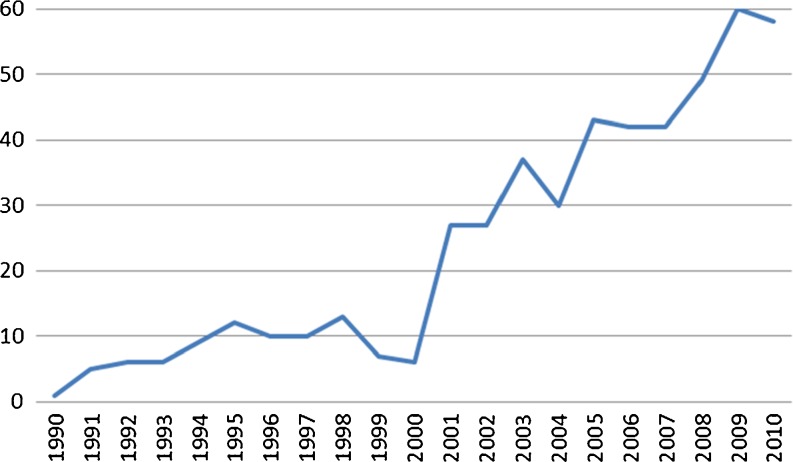
Figure 2 charts the number of published articles in the PubMed database, which include public–private partnerships either in the title or in the abstract. As shown in Fig. 2 prior to 1990, there were no mentions in publications. The first increase was recorded in 2001, with an exponential increase over the whole time axis. Reporting and discussion demonstrate a high level of interest in the subject.
Fig. 2.
Numbers of PPP publications in PubMed
The chart mirrors the historical development of PPPs. Until the late 1970s, there were hardly any cooperative ventures between the private and public sectors. Those that did exist were frequently characterised by mistrust on both sides. The partnerships were mostly limited to public sector relationships between donor agencies and recipient country governments (Buse and Walt 2000a; The World Bank Partnerships Group 1998; Mitchell-Weaver and Manning 1992).
In the early 1980s under the influence of the neoliberal ideologies on public order and attitudes, the relationship between the two sectors started to change (Lüders 2009). Influential international organisations recognised the significance of the private sector and campaigned to achieve a more important role (Ollila 2003). From then on an increasing number of PPPs were formed. The great increase in the number of publications after 2001 may not be assumed to imply a greater number of PPPs, only a more substantial publication record. The experience gathered on existing projects was more widely reported in order to publicise the function and best practice of PPP. More attention is now being given to project performance figures and their comparison with the results of other completed projects.
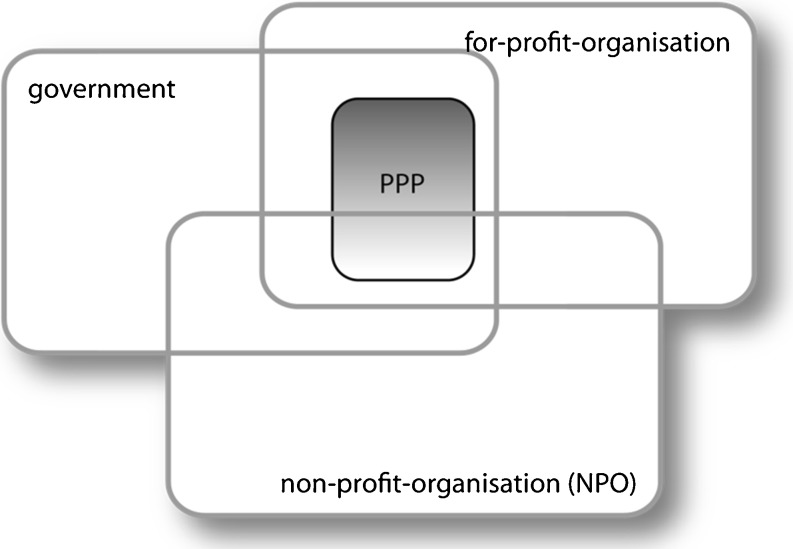
What is a PPP? Definitions of parties and cooperation
What is a PPP? The nature, variety and individuality of public–private partnerships make definition difficult (Reich 2000; Buse and Waxman 2001). The reason there are so many differing definitions is to be found in the diversity of the areas in which PPPs have been applied. PPPs are more prevalent in the areas of energy, water utilities and telecommunications than in public health (the World Bank Group’s PPI Project-Database, http://ppi.worldbank.org; Datta 2009). They are applied in industrialised countries as well as in countries with low and middle incomes. Furthermore there are notable differences in the involved establishments and institutions of both the public and private sectors. The organisations from both sectors vary in size, organisational form, sphere of activity, area of responsibility, financial and manpower resources, and culture. As a result the combination potential for PPPs between the two sectors is extremely diverse. The different cultures, living standards and health systems in the individual countries with low and middle incomes must also be considered and increase the complexity of the issue. Seen in this context, each new PPP presents a unique challenge. In order to better understand PPPs, we will proceed by considering the individual cooperating partners in more detail (Fig. 3).
Fig. 3.
Involved partners
In general the public sector consists of the intergovernmental organisations (IGO), government authorities, ministries, institutions and those programmes, for which the government is legally responsible. The public sector concentrates on the public interest, stewardship and solidarity considerations. It is best presented when involved in issues such as “policy management, regulation, ensuring equity, preventing discrimination or exploitation, ensuring continuity and stability of services, and ensuring social cohesion (through the mixing of races and classes for example, in the public schools)” (Osborne and Gaebler 1992). It is also concerned with social responsibility and environmental awareness (UN 1997).
In the private sector we differentiate between for profit and non-profit organisations (NPO). The former are those enterprises or other organisations which exist primarily in order to make a profit. In the health sector, these include the pharmaceutical companies, operators of private clinics, laboratories and other profit-oriented manufacturers or service providers. The private sector is especially noteworthy for its creativity and dynamism and its “access to finance, knowledge of technologies, managerial efficiency, and entrepreneurial spirit” (UN 1997). The sector also has other advantages, in its ability to rapidly adjust to new conditions, to discontinue unsuccessful or obsolete activities, to innovate and replicate successful experiments, and to perform complex or technical tasks, and all of these with a high degree of efficiency (Rosenau 1999; Björkmann 2008).
As NPO, we recognise those organisations operating as charities, foundations or as private enterprises, which, complementary to state and free market, provide specific support and services for their members (self-help) or third parties. They are not profit oriented and reinvest their surplus funds according to their goals; their aim is to satisfy the social, cultural or scientific endeavours of their members. They can be relief organisations for disaster control, medical services or emergency rescue services. Not-for-profit organisations (or “third sector”) can be involved in PPPs and may exhibit particular strengths in compassion, commitment and trust. The third sector carries conviction when “moral codes and individual responsibility for behavior” (Osborne and Gaebler 1992) are relevant.
The literature shows broad agreement that public authorities, the private sector and the NPOs, where they are active, are best equipped to fulfil their tasks. A combined effort could produce improved results where weaknesses of one could be compensated for by the strengths of the others (Table 1).
Table 1.
Character of participants (Radawan 2005)
| Subsector | Advantages | Liabilities |
|---|---|---|
| Public | Accessible | Low quality care |
| Client oriented | Difficult to mainstream | |
| Low cost | Low educated | |
| NGO | High quality | Small coverage |
| Target the poor | Lack of resources | |
| Low cost | Cannot be scaled up | |
| Involve the community | Ad hoc interventions | |
| For profit | High quality | Ad hoc interventions |
| Huge outreach | High cost | |
| Innovative | Clusters in cities |
In the following, various definitions are examined from which the nature of cooperation is derived: means to “bring together a set of actors for the common goal of improving the health of the population based on the mutually agreeable roles and principles” (Kickbusch 1998). “A partnership means that both parties have agreed to work together in implementing a program and that each party has a clear role and say in how that implementation happens” (Balgescu and Young 2005).
“Public–private partnership (PPP) refers to a variety of co-operative arrangements between the government and private sector. The private sector partner may be either a provider or group of providers, or an entity from the commercial production or distribution sectors. Such partnerships provide a method of involving the private sector in delivering public goods or services and/or securing the use of assets necessary to deliver public services. PPPs also provide a vehicle for coordinating with nongovernmental actors to undertake integrated, comprehensive efforts to meet community needs. The structure of the partnership varies, to take advantage of the expertise of each partner, so that resources, risks and rewards can be allocated in a way that best meets clearly defined public needs” (Axelsson et al. 2003). Most commonly used definition in the health arena is that proposed by Buse and Walt: “a collaborative relationship which transcends national boundaries and brings together at least three parties, among them a corporation (and/or industry association) and an IGO, so as to achieve a shared health-creating goal on the basis of a mutually agreed division of labour” (Buse and Walt 2000a).
The functioning of the partnership is based on the synergy arising from the linking of abilities, knowledge and resources, and the application of technologies spanning all sectors to achieve the social goals, sharing different kinds of risk (Bovis 2010) and utilising the active involvement of representatives of both private and public sectors (Nikolic and Maikisch 2006). In the words of Raman and Björkmann (2009), the core elements of a viable partnership are “beneficence (joint gains), autonomy (of each partner), jointness (shared decision making and accountability), commitment (to public health goals) and equity (fair returns in proportion to investment and effort)”.
Although Buse and Walt highlight three central areas relevant to global PPPs, a comprehensive description of PPPs would seem to be more appropriate for a general presentation. In order to differentiate PPPs from the classical collaboration between the public and private sectors, seven fundamental features of a PPP are presented as follows:
Fulfilment of a public duty: A PPP cooperation always results in the discharging of a public duty. This understanding covers those areas of public service, where the authority has a duty or responsibility to provide amenities and services to the community in compliance with constitutional or statutory legislation.
The partners in a PPP include at least one public authority and at least one private contractor: The prerequisite qualification for a public authority partner in a PPP is the meaningful activity of a public authority, i.e. a local authority or a decentralised organisation, dedicated to serving the interest of the public and responsible for providing the public with major services. Private partners are commercial companies, who have the expertise and economic appreciation to implement the common goal.
Provision of an economic service: The common aim and effort must yield an economic result. Both partners are interested in achieving an output from the project. The public partner expects an effective and efficient discharge of the public duty in question, while the private partner hopes that the PPP will provide an opportunity to expand into new areas of operation and win further business contracts. The PPP typically yields a financial remuneration for the private contribution through a service fee from the public authority and/or the user.
Mutual responsibility association: Focusing on mutual aims by both partners and the cooperative accomplishment of the tasks signifies a joint sharing of responsibility. This marks the clear difference between the classic customer–contractor relationship and the public authority–private contractor relationship.
Bundling resources: In a PPP the capital, equipment and knowledge necessary for the fulfilment of the project are supplied by the partner most capable of providing this. The potential for synergy effects and savings through efficiency is utilised.
Risk allocation: In a PPP it is typical for the risks to be distributed among the partners according to their ability to deal with them, i.e. who can best calculate and influence the risks.
Long-term and process-oriented cooperation: An elementary characteristic of a PPP is the orientation to its life cycle, i.e. the cooperation is maintained throughout the complete life cycle of the project. The focus remains on the service aimed for. The development process is not completely defined and can be revised and changed during the life of the project with the mutual agreement of the partners.
Motives of PPP
In the preceding definition, the attributes of the various partners and their cooperation were examined. In the following, the focus is on the motives of the various organisations involved in the cooperative ventures. This should clarify the driving forces that operate in the cooperation.
Until recently the private and noncommercial sectors were often perceived publicly as mistrustful antagonists. This tension has been eased through a convergence of interests and changes in the conditions for PPPs in the health services. One of the main factors for the creation of partnerships is the recognition that neither side can achieve its goals alone, i.e. a cooperation is inevitable. The motives of the public authorities to form partnerships with the private sector are (1) to guarantee and improve the health services through (2) the utilisation of additional (private) resources, (3) to gain access to commercial knowledge and management skills for (4) increased efficiency and (5) thereby to achieve more authority (Buse and Walt 2000b).
The challenges faced by the nations with low and middle incomes are enormous, especially in the fight against infectious diseases such as HIV and tuberculosis. A most persuasive argument in favour of partnerships is the prospect of more resources and programmes, which can benefit the medical care for the population. In spite of restricted resources, new care facilities can be offered in the short term. Additional services become possible without the need for prioritisation.
Nevertheless there is considerable scepticism about the motives of private companies, even when there are considerable advantages for the general health service involved through their cooperation in the PPPs. Private companies are often assumed to be using the partnerships to reach new markets with a view to generating future profits or trying to extend their influence (Björkmann 2008). These assumptions mirror the cultural divide between the private and public sectors. The interest of industry in global public health, which is also pertinent in other areas where PPPs apply, is described as follows by Buse and Walt (2000a):
Increases influence in the global arena: Affords opportunity for involvement in the articulation, interpretation and implementation of global rules governing trade, health standards and reform of the UN
Increased influence at the national level, The use of UN systems to gain access to policy makers, institutions, information, etc. (including proximity to regulatory process)
Direct financial benefits, Tax breaks, market identification, development, penetration and manipulation.
Brand and image promotion: Increased global recognition, improved image through association with United Nations
Increased authority and added legitimacy through association with UN
Enhanced corporate citizenship
Although the motives of the two sides appear diametrically opposed, they can be harmonised. There are alternative ways to attain one’s own goals, and the possibility of a win–win situation if the appropriate partner is found and mutually acceptable operating conditions are agreed (Richter 2004a). Rosenau (1999) stipulates five factors which, if followed, improve the chances of success: (1) Key decisions should be made at the outset of the project and laid down in a precise plan. (2) Responsibility should be clearly defined. (3) Feasible goals should be set, and (4) continuous incentives should apply for the partners. (5) The project progress should be monitored.
If the appropriate partners are found and the stated basic rules of the project are adhered to, then the partnership will succeed despite the opposing interests (Richter 2004b), as many success stories have demonstrated. In summary, where goals overlap, but cannot be achieved alone, then PPP offers the best possibility to harmonise opposing interests and mutually cooperate to achieve success.
Risks for PPP
A potential risk for PPP is when it leads to parallel systems presenting in a country or region. In a worst case scenario, this can develop to a point where by gradual attrition, the responsibility is transferred to the private partner and the public authority withdraws willingly or sometimes unwillingly. A long-term guarantee of medical service is not then possible, since the private partner is subject to market fluctuations and self-interest may predominate. Furthermore the lack of transparency in the development and functioning of the PPP project and the stipulation and monitoring of the aims become critical (Goel et al. 2007). Another critical point is the possibility that the local health sector staff, who are involved for example in the distribution of medication, may be so excessively burdened that they neglect to fulfil their normal tasks (Pefile 2003).
There may be no comprehensive strengthening of the regional structure, since this does not fall within the area of responsibility of the PPP or no such mandate has been defined. Even if the ministries are more involved, it is conceivable that the access to large quantities of external resources will have negative effects. Resources may be diverted to fulfil other national priorities, which may lead to corruption or internal rivalry to gain control of the funds and their distribution (Buse and Walt 2000a). Especially in emerging and developing countries, venality is an important issue. Transparency International (2010) publishes the Corruption Perception Index, a measure for corruption in a country. In countries with low indices, PPP bear the risk that a project will be manipulated in such a way that interests of a particular group will be represented. Furthermore, the effectiveness of PPP is generally still unclear and needs more evaluation (Barr 2007).
Finally, it may be said that PPP is predominantly positive and attributed with high potential. A comprehensive literature review reveals that negative aspects exist only in a minor form. Possibly, this could arise from prevalent positive belief and good experience. A final consideration will be possible when closed projects are evaluated after a long-term period.
PPP application areas
A breakdown of the PPP applications by disease patterns reveals that approx. 85 % of PPPs are concerned with specific diseases such as HIV/AIDS, malaria and tuberculosis. Relatively few have focused on the improvement of the medical system. Some 5 % focus on reproductive health issues, 5 % on blindness and cataracts, 3 % on nutrition deficiency syndromes and the remainder are involved with health policy and research, the safety of injections and chemicals, and digital divide (Barr 2007; Nishtar 2004). According to this source, there are still no PPPs in the area of genetic services. Considering the areas of activities, the first genetic services applications could be derived from them.
The majority of PPPs focus on the development and deployment of medicines. This can encompass the complete life cycle process from fundamental research through product development, trials, licensing and, if required, conforming to the conditions of low incomes and middle incomes countries, funding and launching. In contrast, other partnerships concentrate on the distribution of medicines, inoculants or other medical products such as diagnostic equipment, contraceptives or mosquito nets. A few partnerships attempt to improve the access of the poor population to a wider spectrum of health services and products (Yaïch 2009). Still others concentrate on a specific indication and offer comprehensive measures to treat it.
Various systems of classification have been presented for the categorisation and conceptualisation of PPPs based on their type of activity. The classification by Buse and Walt as shown in Table 2 comprises three areas which are presented below. These three categories are to be found again in similar classifications by Nishtar (2004) and Widdus (2001) but extended in areas that will not be addressed here.
Table 2.
Classification of PPPs
| Buse and Walt (2000b) | Nishtar (2004) | Widdus (2001) |
|---|---|---|
| Product-based partnerships | Improving access to healthcare products | Distributing a donated or subsidized product, to control a specific disease |
| Product development partnerships | Product development | Developing a product |
| Systems/issues-based partnerships | Global coordination mechanisms | Disease control through product donation and distribution |
| Strengthening health services | Strengthening health services | |
| Public advocacy and education | Educating the public | |
| Regulation and quality assurance | Improving product quality or regulation | |
| Coordinating multifaceted efforts |
Product-based partnerships are mainly drug donation programmes (Peters and Phillips 2004). Products are distributed to the public sector of countries with low incomes, e.g. condoms for women or AIDS medication. As a general rule, drug donation programmes are implemented where the efficacy of a medicine has been established but where the effective demand is restrained through a limited willingness or ability to pay. Private pharmaceutical companies normally initiate this type of partnership. They aim through the partnership to reduce costs and extend the target population, who need but cannot afford the medication (Pefile 2003). While private enterprises follow short-term objectives such as extending their range of political contacts on a global and national scale, they also use partnerships to foster the long-term goal of improving their company image. Since this goal cannot be guaranteed, critical discussions frequently occur about the drug donation programmes with reference to the creation of dependency and the lack of sustainability (Buse and Walt 2000a).
Product development partnerships differ from product donation partnerships in various aspects (Meredith and Ziemba 2008; WHO 2007). Firstly, they are not focused on particular countries; secondly, these partnerships are generally driven by the public sector. Thirdly, product development partnerships are not based on a lack of demand. The majority of these products are perceived as necessary by the public sector and are designated for support through public investment (Widdus and White 2004). They frequently do not reach the market because the industry recognises that the financial yield will not justify the necessary investment (Widdus 2005). Their discovery and development are withheld and not made available (Kettler et al. 2003). For example the research for a vaccine against AIDS is seen as an important public service; the industry however is uncertain as to whether the investment for the research and development of a new effective vaccine can be amortised, since they must carry the risk of writing off the costs of failure (Brown 2008; Nwaka and Ridley 2003; Ziemba 2005). Furthermore, even if an effective vaccine should be discovered, the private sector cannot be sure that a sufficient number of financially strong markets exist to buy the product, thereby justifying their development and marketing investments. Additional costs, for unforeseen events in unknown markets which must be included in the calculation, are another unpredictable grey zone (Kettler et al. 2003). For these reasons the PPPs for product development demand that a range of risks faced in the invention, development and/or marketing be carried by the public sector, thereby reducing the opportunity costs and improving the prospects of the involved industry partners (Wheeler and Berkley 2001).
The systems/issues-based partnerships are an eclectic group. A number have been formed to surmount market failures, such as the Malaria Vaccine Initiative. Other system relevant PPPs were formed to augment the attempts of governments in specific areas, e.g. the partnership of Secure the Future and to retain further private nonmedical resources for the fight against disease (Buse and Walt 2000b).
The costs of PPPs
Regardless of which type of PPP is considered, the question of the costs involved will invariably be raised—a question that can only be answered after additional investigation. If it is also necessary to establish whether PPPs are cost-effective, i.e. if the relationships between outlay and outcome are to be analysed, then the range of parameters needing to be examined is greater and the analysis more complex. Some PPPs have had external audits and can answer the question about the relationship of the costs to the standard form of supply for their project.
A generalisation or a systematic comparison of the various studies made is not yet possible since no standardised and generally acknowledged performance indicators exist. Also no standard form of survey has been agreed, so that benchmarks have not been established for this area. This may be due to the divergent types of partners and cultural backgrounds. Nevertheless the basic demand for evaluation (Widdus 2003; Barr 2007) and for specific performance indicators and management models has been growing. The first designs to address this have been formulated, for example, how a system of Performance Management could appear (Gwen 2008).
A systematic search of the literature in the PubMed data base was made in order to arrive at a rough estimate of the costs for a PPP and its cost effectiveness. This took account of the first analyses of the health services in low and middle incomes countries. Various PPP synonyms were used, combined with various expressions of cost and cost effectiveness, as search terms. The result was a list of 40 available articles, each of which was examined for its contents and results (Table 3).
Table 3.
Result of systematic literature search
| Assessment | N = 40 | % |
|---|---|---|
| No cost study | 26 | 65 |
| No PPP | 5 | 12.5 |
| In USA/Europe | 5 | 12.5 |
| Not in area of health service | 1 | 2.5 |
| Valid | 3 | 7.5 |
Twenty-six studies mentioned costs, not in connection with a cost analysis of a PPP project, but either with reference to costs of a small part of the project or to a secondary source that had nothing to do with the project. Further groups included in this category were evaluations restricted to the outcome without reference to the costs (Peters and Phillips 2004). Five publications were not PPPs, but mentioned this form of partnership in their conclusions as a feasible alternative to the actual structure. Five studies were of projects in the USA or Europe; one was not in the health service area. Of the three remaining studies, two were identical, having been published with differing text in two different publications (Sinanovic and Kumaranayake 2006a/Sinanovic and Kumaranayake 2006b) (Table 4).
Table 4.
Results of studies of PPP costs
| Author | Karki et al. (2007) | Sinanovic and Kumaranayake (2006a) |
| Country | Nepal | South Africa |
| Diseases | TB | TB |
| PPP | A semi-governmental hospital (Patan Hospital), three NGOs [Yala Urban Health Programme (YUHP), Nepal Anti-TB Association (NATA) and Care & Fair] and one private nursing home were invited to become treatment centres | • Public–private workplace: represents a partnership between provincial TB programmes and mining companies |
| • Public–private non-government (PNP): a partnership between provincial TB programmes and non-governmental organisations (NGOs) providing community-based DOT | ||
| Results | • Overall costs for treating a TB patient under the PPP scheme averaged US$89.60 | • Cost per case cured |
| • PNP US$354–446 | ||
| • PWP US$788–979 | ||
| • Public sites US$700–1,000 | ||
| Conclusion | • Treating TB patients in the PPP scheme had a low additional cost | • PPP models could significantly reduce costs to the patient |
| • Doubling the case notification rate and maintaining a high success rate | • Scaling up of effective services could occur at much lower cost than solely relying on public sector models |
It may be noted that these two studies relate to projects which cannot be assigned wholly to any of the categories of PPP described above, but rather are pieced together from various elements. Product development, for example, is not to be found in these studies. In contrast, the following categories “disease control through product donation and distribution”, “educating the public” and “strengthening health services” are all mentioned. In reality PPPs are significantly more complex than as expressed in their definitions. The categories and definitions used are not clear demarcations but only orientation criteria.
The composition of the partnerships in the two countries is very different. This is an example of the broad range of possibilities for a variety of service providers in a health service to cooperate in a PPP. Although the same disease may be a target, the formation of the partnership is individual. A comparison of the costs for the two countries would not be meaningful for two reasons. Firstly, the pro capita income in South Africa is a multiple of that in Nepal. Secondly, the care service structures differ on account of the different PPP members. Only one common conclusion is possible, namely how the PPP compares to the other care services in the respective country. In both results a positive trend can be noted. While Kaki et al. (2007) reports higher auxiliary costs but also describes a higher outcome, Sinanovic and Kumaranayake (2006a) report a basic advantage in the involvement of private partners. Even though the two countries have different economic conditions, they can both claim successful experience with a PPP.
The analysis of cost and effectiveness of the care service is of particular importance. However, considering this aspect alone may not necessarily lead to the desired goal. As Karki et al. (2007) reported, the initial costs of the project are higher than for the normal provision of care service but the medical success must also be evaluated as higher. Thus a further step must be taken to determine whether the project was cost-effective, i.e. whether the better outcome was sufficient to justify the additional outlay.
Sinanovic and Kumaranayake (2006a) found out that PPP models of TB treatment provision are more cost-effective than the purely public sector provision. A closer look at the health care models reveals differences in health care provision. Possibly the funding model is not the causal factor per se which influences the effectiveness of health care provision. It is rather the structure which the funding model creates. PPP is a more flexible alternative compared with a whole health care funding system and may bring about the necessary changes.
The evaluation of partnerships, which improve or extend the medical care services in the short or middle term, should be carried out as a second step. Initially, the central argument should predominate, namely that the health care of the population is improved. The analyses will be relevant and advisable after a PPP has been operating over a longer period of time. Should the care service extend over many years, it will be essential to examine whether the money has been effectively used. With the efficient use of resources, it may be possible to provide care to a greater number and in other populations.
Finally, the studies from the different countries for the same disease show positive results, giving promise for the future. PPPs can definitely contribute to improvements. Transfer of the results is difficult, but under favourable conditions, a similar success should be possible with genetic services.
Transferability to genetic services
Most PPPs have been formed to solve specific problems. In care services they usually exist independently and are seldom integrated with other services at a local level. Currently no PPPs exist in the area of genetic services. In view of highly diverse cultural backgrounds in emerging economies, it is uncertain how the experience gained in other PPPs can be transferred to genetic services. Nevertheless an attempt will be made here to identify the potentially promising application areas.
For a transfer and recommendation, it is necessary to determine the areas where similarities or overlaps are likely to be found within the health service and for which PPP experience exists. Comparing the genetic services pyramid (Fig. 1) with the categories from Table 2, various possibilities emerge (Table 5).
Table 5.
Integration of the genetic services pyramid with the categories of PPPs
| Pyramid | Buse and Walt (2000b) | Nishtar (2004) | Widdus (2001) |
|---|---|---|---|
| Direct health services | |||
| Enabling services | • Improving access to healthcare products | • Educating the public | |
| • Public advocacy and education | |||
| Population-based services | • Product-based partnerships | • Disease control through product donation and distribution | |
| • Distributing a donated or subsidized product, to control a specific disease | |||
| Infrastructure building services | • Product development partnerships | • Product development | • Developing a product |
| • Systems/issues-based partnerships | • Global coordination mechanisms | • Strengthening health services | |
| • Strengthening health services | • Improving product quality or regulation | ||
| • Regulation and quality assurance | • Coordinating multifaceted efforts |
Most PPP categories appear applicable at the level of infrastructure building services. Product development partnerships, so far the most frequently met PPP form, also occur at this level. It is likely that this would create the entry point of the PPP concept in genetic services. Examples could include:
EQA schemes (e.g. http://www.eurogentest.org/laboratories/eqa/),
Certification and accreditation of laboratories and clinics,
Certification of personnel and
Providing training programmes and courses (e.g. http://www.eurogentest.org/unit6/info/courses/index.xhtml
At the level of the population-based services, product-based partnerships/disease control can occur through product donation and distribution. Based on the experience from existing partnerships, a detailed analysis of this concept would be required to determine both the key issues and the companies which would potentially be the most suitable partners. Practical experience gained can be merged into a business plan. Precise partnerships could be envisaged to combat specific disease conditions. Other examples are:
Providing laboratory resources for metabolic screening and
Providing personnel (e.g. genetic nurses, counsellors, laboratory staff).
The enabling services are an important factor to improve access to medical supply. Particularly travel costs are a non-negligible factor (Cohen et al. 2004). Even if patients have to travel long distances, it can cause high costs and be a considerable barrier for them (Paz-y-Mino 2004). In order to minimize patients’ travel costs, telemedicine is one appropriate alternative to improve access to genetic services. Here, PPP can be a relevant solution to develop such structures. Examples may include:
Offering special health insurance (e.g. mother and child, e.g. http://publications.paho.org/english/Bolivia_OP_213.pdf),
Supporting patient organisations (see http://www.patientsorganizations.org/),
Producing educational materials (e.g. http://www.eurogentest.org/patient/leaflet/patients.xhtml),
Telemedicine (e.g. http://www.capabilitynet.eu/Meetings/Trolleholm/Documents/02_CAPABILITY%20WS1_A._Christianson.pdf) and
Collecting and transporting laboratory samples.
Partnerships could potentially be created at the level of the Direct Health Services. A demand for this type of service is likely to escalate with increasing public health impact of rarer genetic conditions including familial cancer. The barriers here would be particularly high as there are no clear examples of PPPs operating, and practical examples are lacking. Potential areas are:
Processing of individual laboratory samples (e.g. www.capabilitynet.eu/Meetings/South_Africa/Documents/J_Schmidtke.pdf) and
Organising “syndrome clubs” with foreign experts.
Conclusion
PPP, a concept of financing complex community tasks, is becoming increasingly popular in health care. PPPs bring together skills, knowledge and resources, and can mobilize private finance, increase access, introduce efficiencies in the delivery of public health services and improve outcomes. There are already numerous successful partnerships operating in countries with low and middle incomes. Thus far, they are established in other application areas, but these can serve as models for the implementation of PPPs in genetic services. It is possible that experience from PPP projects can be projected onto the genetic service pyramid. The level of infrastructure building services offers a good starting point. In a country where no genetic services are currently offered, it would be expedient to first establish a stable foundation, on which further capacity can be structured and integrated as a sustainable feature of the care service. Depending on local circumstances, i.e. where genetic services are established in principle, other entry points could be considered.
Acknowledgments
We would like to thank Dr. Hilary Harris for the support and critically reading the manuscript. Mike Gibson’s editorial help is gratefully acknowledged. All members of the Capability and GenTEE partnerships are thanked for discussions. This project was part of the CAPABILITY Special Support Action funded by the EC 6th Framework Programme, contract number: LSSG-CT-2006-037275.
Conflict of interest
The authors declare no conflicts of interest.
Footnotes
This is a contribution to Special Issue: Capability.
References
- Axelsson H, Bustreo F, Harding H. Private sector participation in child health. Washington: The World Bank Group; 2003. [PMC free article] [PubMed] [Google Scholar]
- Barr AD. A research protocol to evaluate the effectiveness of public–private partnerships as a means to improve health and welfare systems worldwide. Am J Public Health. 2007;97:19–25. doi: 10.2105/AJPH.2005.075614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzoli GJ, Stein R, Alexander JA, Conrad DA, Sofaer S, Shortell SM. Public–private collaboration in health and human service delivery: evidence from community partnerships. Milbank Q. 1997;75:533–561. doi: 10.1111/1468-0009.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J. The new genetics in clinical practice. BMJ. 1998;316:618. doi: 10.1136/bmj.316.7131.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett C, Burke S, Burton H, Farndon P. A toolkit for incorporating genetics into mainstream medical services: learning from service development pilots in England. BMC Health Serv Res. 2010;10:125. doi: 10.1186/1472-6963-10-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Björkmann JW (2008) Public-private partnerships in health care services of less developed countries. Manuscript available from the author
- Blagescu M, Young J (2005) Partnerships and accountability: current thinking and approaches among agencies supporting Civil Society Organisations. Working Paper 255, London; Overseas Development Institute http://kms1.isn.ethz.ch/serviceengine/Files/ISN/22721/ipublicationdocument_singledocument/0D762521-9F6E-4EA2-868D-2465F6038655/en/wp255.pdf. Accessed 26 Dec 2010
- Bovis C (2010) Editorial—Public private partnerships: the challenges and opportunities for delivering public services in the 21st century. EPPPL 01/2010:1–14
- Brown D. The portfolio approach to successful product development in global health. In: Matlin S, Francisco A, Sundaram L, Faich H-S, Gehner M, editors. Health partnerships review. Geneva: Global Forum for Health Research; 2008. [Google Scholar]
- Bühner R (2004) Betriebswirtschaftliche Organisationslehre. Oldenburg, München 196–197
- Burke W, Khoury MJ, Stewart A, Zimmern RL. The path from genome-based research to population health: development of an international public health genomics network. Genet Med. 2006;8:451–458. doi: 10.1097/01.gim.0000228213.72256.8c. [DOI] [PubMed] [Google Scholar]
- Buse K, Walt G. Global public–private partnerships: part I—a new development in health? Bull World Health Organ. 2000;78:549–561. [PMC free article] [PubMed] [Google Scholar]
- Buse K, Walt G. Global public–private partnerships: part II—what are the health issues for global governance? Bull World Health Organ. 2000;78:699–709. [PMC free article] [PubMed] [Google Scholar]
- Buse K, Waxman A. Public-private health partnerships: a strategy for WHO bulletin of the WHO. Bull World Health Organ. 2001;79:748–754. [PMC free article] [PubMed] [Google Scholar]
- Maternal and Child Health Bureau (2000) Title V Block Grant program; guidance and forms for the Title V application and annual report. HRSA, MCHB, Department of Health and Human Services, OMB NO 0915–0172
- Christianson A, Zimmern R, Kristoffersson U, J. Schmidtke J, Kent A, Raouf R, Barreiro C, Nippert I (2011) Health needs assessment for medical genetic services for congenital disorders in middle- and low-income nations. J Comm Genet [DOI] [PMC free article] [PubMed]
- Cohen D, Barton G, Gray J, Brain K. Health economics and genetic service development: a familial cancer genetic example. Fam Cancer. 2004;3:61–67. doi: 10.1023/B:FAME.0000026812.87551.bf. [DOI] [PubMed] [Google Scholar]
- Daiger SP. Was the Human Genome Project worth the effort? Sci. 2005;308:362–364. doi: 10.1126/science.1111655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta A. Public–private partnerships in India: a case for reform? Econ Polit Wkly. 2009;44:73–78. [Google Scholar]
- Emery J, Hayflick S. The challenge of integrating genetic medicine into primary care. BMJ. 2001;322:1027. doi: 10.1136/bmj.322.7293.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fozouni B, Güntert B. Prioritätensetzung im deutschen Gesundheitswesen—die Triade zwischen Rationierung, Rationalisierung und rationaler Allokation. Gesundheitswesen. 2000;62:559–567. doi: 10.1055/s-2000-13043. [DOI] [PubMed] [Google Scholar]
- Goel NK, Galhotra A, Swami HM (2007) Public private partnerships in the health sector. The Internet Journal of Health. http://www.ispub.com/journal/the_internet_journal_of_health/volume_6_number_2_7/article/public_private_partnerships_in_the_health_sector.html. Accessed 26 Dec 2010
- Gwatkin D, Guillot M. The burden of disease among the global poor: current situation, future trends, and implications for strategy. Washington: World Bank; 1999. [Google Scholar]
- Gwen D (2008) PPP initiatives and the HR crisis in the health sector. Working paper. http://stpse.ro/atasamente/226_C_Working%20paper_V4.pdf. Accessed 26 Dec 2010
- Jung H. Allgemeine Betriebswirtschaftslehre. München: Oldenburg; 2006. [Google Scholar]
- Karki DK, Mirzoev TN, Green AT, Newell JN, Baral SC (2007) Costs of a successful public–private partnership for TB control in an urban setting in Nepal. BMC Public Health. doi:10.1186/1471-2458-7-84 [DOI] [PMC free article] [PubMed]
- Kaye CI, Laxova R, Livingston JE, Lloyd-Puryear MA, Mann M, McCabe E, Therrell BL. Integrating genetic services into public health—guidance for state and territorial programs from the National Newborn Screening and Genetics Resource Center (NNSGRC) Community Genet. 2001;4:175–196. doi: 10.1159/000051179. [DOI] [PubMed] [Google Scholar]
- Kettler H, White K, Jordan S. Valuing industry contributions to public–private partnerships for health product development. Geneva: Initiative on Public-Private Partnerships for Health; 2003. [Google Scholar]
- Kickbusch I, Quick J. Partnerships for health in the 21st century. World Health Stat Q. 1998;51:68–74. [PubMed] [Google Scholar]
- Lüders J. Public Private Partnership—Der Versuch einer kritischen Auseinandersetzung. Norderstedt: GRIN; 2009. [Google Scholar]
- Meredith S, Ziemba E. The new landscape of product development partnerships (PDPs) In: Matlin S, Francisco A, Sundaram L, Faich H-S, Gehner M, editors. Health partnerships review. Geneva: Global Forum for Health Research; 2008. [Google Scholar]
- Mitchell-Weaver C, Manning B. Public–private partnerships in third world development: a conceptual overview. Stud Comp Int Dev. 1992;26:45–67. doi: 10.1007/BF02743762. [DOI] [Google Scholar]
- Nikolic I, Maikisch H (2006) Public–private partnerships and collaboration in the health sector. An overview with case studies from recent European experience. Working paper. http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2006/11/01/000090341_20061101140721/Rendered/PDF/378070Public0p1artnerships01PUBLIC1.pdf. Accessed 17 Dec 2010
- Nishtar S (2004) Public–private partnerships in health—a global call to action. Health Res Pol Syst. doi:10.1186/1478-4505-2-5 [DOI] [PMC free article] [PubMed]
- Nwaka S, Ridley RG. Virtual drug discovery and development for neglected diseases through public–private partnerships. Nat Rev Drug Discov. 2003;2:919–928. doi: 10.1038/nrd1230. [DOI] [PubMed] [Google Scholar]
- Ollila E. Health-related public–private partnerships and the United Nations. In: Deacon B, Ollila E, Koivusalo M, Stubbs P, editors. Global social governance: themes and prospects. Helsinki: Ministry for Foreign Affairs of Finland; 2003. pp. 36–73. [Google Scholar]
- Osborne D, Gaebler T. Reinventing government: how the entrepreneurial spirit is transforming the public sector. New York: Addison-Wesley; 1992. [Google Scholar]
- Paz-y-Miño C. Genetic services in Ecuador. Community Genet. 2004;7:137–41. doi: 10.1159/000080784. [DOI] [PubMed] [Google Scholar]
- Pefile S. Donation programmes for HIV/AIDS-related the early experience of the Diflucan® partnership programme and Viramune® donation programme. Geneva: Initiative on Public-Private Partnerships for Health; 2003. [Google Scholar]
- Peters DH, Phillips T. Mectizan donation program: evaluation of a public–private partnership. Trop Med Int Health. 2004;9:A4–A1. doi: 10.1111/j.1365-3156.2004.01209.x. [DOI] [PubMed] [Google Scholar]
- Radwan I (2005) India - Private Health Services for the Poor. Discussion paper, 958 Washington, DC. http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627–1095698140167/RadwanIndiaPrivateHealthFinal.pdf. Accessed 14 Mai 2012
- Raman AV, Björkman JW. Public–private partnership in the provision of health care services to the poor in India. In: Dinello N, Shaoguang W, editors. China, India and beyond—development drivers and limitations. Cheltonham: Edward Elger Publishing; 2009. pp. 143–172. [Google Scholar]
- Reich M. Public–private partnerships for public health. Nat Med. 2000;6:617–620. doi: 10.1038/76176. [DOI] [PubMed] [Google Scholar]
- Richter J. Public–private partnerships for health: a trend with no alternatives? Development. 2004;47:43–48. doi: 10.1057/palgrave.development.1100043. [DOI] [Google Scholar]
- Richter J (2004b) Public-private partnerships and international health policy-making. Ministry of Foreign Affairs of Finland, Helsinki, http://formin.finland.fi/Public/Print.aspx?contentid=73317&nodeid=15458&culture=en-US&contentlan=2. Accessed 04 Jan 2011
- Rosenau P. The strengths and weaknesses of public–private policy partnerships. Am Behav Sci. 1999;43:10–34. [Google Scholar]
- Sinanovic E, Kumaranayake L (2006a) Financing and cost-effectiveness analysis of public–private partnerships: provision of tuberculosis treatment in South Africa. Cost Eff Resour Alloc. doi:10.1186/1478-7547-4-11 [DOI] [PMC free article] [PubMed]
- Sinanovic E, Kumaranayake L. Sharing the burden of TB/HIV? Costs and financing of public–private partnerships for tuberculosis treatment in South Africa. Trop Med Int Health. 2006;11:1466–1474. doi: 10.1111/j.1365-3156.2006.01686.x. [DOI] [PubMed] [Google Scholar]
- Smith R. Vaccines and medicines for the world's poorest. Public–private partnerships seem to be essential. BMJ. 2000;320:952–953. doi: 10.1136/bmj.320.7240.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank Partnerships Group (1998) Partnership for development: proposed actions for the World Bank. Discussion paper, Washington, DC. http://www.worldbank.org/html/extdr/pfd-discpaper.pdf. Accessed 24 Feb 2011
- Transparency International (2010) The Corruption Perception Index 2010. ISBN 978-3-935711-60-9
- United Nations (1997) Public–private partnerships: the enabling environment for development. http://unpan1.un.org/intradoc/groups/public/documents/un/unpan000727.pdf. Accessed 04 Jan 2011
- Wheeler C, Berkley S. Initial lessons from public–private partnerships in drug and vaccine development. WHO Bulletin. 2001;79:728–734. [PMC free article] [PubMed] [Google Scholar]
- Widdus R. Public–private partnerships for health: their main targets, their diversity, and their future directions. WHO Bulletin. 2001;79:713–720. [PMC free article] [PubMed] [Google Scholar]
- Widdus R. Public–private partnerships for health require thoughtful evaluation. Bull World Health Organ. 2003;81:235. [PMC free article] [PubMed] [Google Scholar]
- Widdus R. Public–private partnerships: an overview. Trans Roy Soc Trop Med Hyg. 2005;99:S1–8. doi: 10.1016/j.trstmh.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Widdus R, White K (2004) Combating diseases associated with poverty–financing strategies for product development and the potential role of public–private partnerships. The Initiative on Public-Private Partnerships for Health (IPPPH), Geneva. http://www.who.int/intellectualproperty/topics/ppp/en/CombatingDiseases-Abridged.pdf. Accessed 04 Jan 2011
- World Health Organisation (2007) Draft global strategy and plan of action on public health, innovation and intellectual property. http://apps.who.int/gb/phi/pdf/igwg2/PHI_IGWG2_ID3-en.pdf. Accessed 04 Jan 2011
- Wright CF, Brice P, Stewart A, Burton H. Realising the benefits of genetics for health. Lancet. 2010;376:1370–1371. doi: 10.1016/S0140-6736(10)61310-4. [DOI] [PubMed] [Google Scholar]
- Yaïch M. Investing in vaccines for developing countries: how public–private partnerships can confront neglected diseases. Landes Biosci. 2009;5:368–369. doi: 10.4161/hv.5.6.8172. [DOI] [PubMed] [Google Scholar]
- Ziemba E (2004) Public–private partnerships for neglected diseases: opportunities to address pharmaceutical gaps for neglected diseases. Background paper. http://archives.who.int/prioritymeds/report/background/pubpriv.doc, Accessed 27 Apr 2012
- Ziemba E (2005) Public–private partnerships for product development: financial, scientific and managerial issues as challenges to future success. Research report. http://www.who.int/intellectualproperty/studies/Ziemba.pdf, Accesses 26 Dec 2010