Abstract
The Greater Sekhukhune-CAPABILITY Outreach Project was undertaken in a rural district in Limpopo, South Africa, as part of the European Union-funded CAPABILITY programme to investigate approaches for capacity building for the translation of genetic knowledge into care and prevention of congenital disorders. Based on previous experience of a clinical genetic outreach programme in Limpopo, it aimed to initiate a district clinical genetic service in Greater Sekhukhune to gain knowledge and experience to assist in the implementation and development of medical genetic services in South Africa. Implementing the service in Greater Sekhukhune was impeded by a developing staff shortage in the province and pressure on the health service from the existing HIV/AIDS and TB epidemics. This situation underscores the need for health needs assessment for developing services for the care and prevention of congenital disorders in middle- and low-income countries. However, these impediments stimulated the pioneering of innovate ways to offer medical genetic services in these circumstances, including tele-teaching of nurses and doctors, using cellular phones to enhance clinical care and adapting and assessing the clinical utility of a laboratory test, QF-PCR, for use in the local circumstances.
Keywords: Medical genetic services, Congenital disorders, South Africa
Introduction
Serious congenital disorders1 contribute significantly to the burden of infant and childhood death and disability in middle- and low-income nations, including South Africa (Christianson et al. 2006; World Health Organisation (WHO) 1999; WHO 2010a). In the mid-1990s, before the effects of the current HIV/AIDS epidemic were felt, and at a time when South Africa was still experiencing positive epidemiological transition, the National Department of Health recognised a growing need to develop medical genetics services for the care and prevention of congenital disorders.
A national task team, sponsored by the WHO, drew up the National Department of Health’s ‘National policy guidelines for the management and prevention of genetic disorders, birth defects and disability’ (National Department of Health 2001). In 2006, the Limpopo Provincial Department of Health and Social Development, having previously hosted a successful clinical genetic outreach programme in the province in the 1990s, formed a task team to plan and implement provincial medical genetic services in accordance with the National Department of Health’s national policy guidelines (Christianson et al. 2000).
The Greater Sekhukhune-CAPABILITY Outreach Project (GraSCOP) was initiated in 2007 from that task team, with funding from CAPABILITY, to pilot a primary and secondary health care service for the care and prevention of congenital disorders in the Greater Sekhukhune district of Limpopo Province (Fig. 1). The objectives of GraSCOP were as follows:
To assess and further develop the principles and practices of primary health care-based medical genetic services as outlined in the South African National Department of Health’s ‘National guidelines for the management and prevention of genetic disorders, birth defects and disabilities’.
To further assess and develop the Medical Genetic Education Programme (MGEP), a distance learning education programme developed for, and currently used by, the National Department of Health for post-graduate nurse training.
To re-evaluate the epidemiology of common congenital disorders in this setting.
To test the clinical utility of DNA-based medical genetic tests and technologies for this setting. CAPABILITY is a programme developed in support of EuroGentest. The criteria developed for clinical utility by EuroGentest were used for this objective to evaluate if they could be applied in a developing country.
To use the knowledge and experience acquired from the project to assist in the implementation and development of medical genetic services throughout Limpopo and other provinces in South Africa.
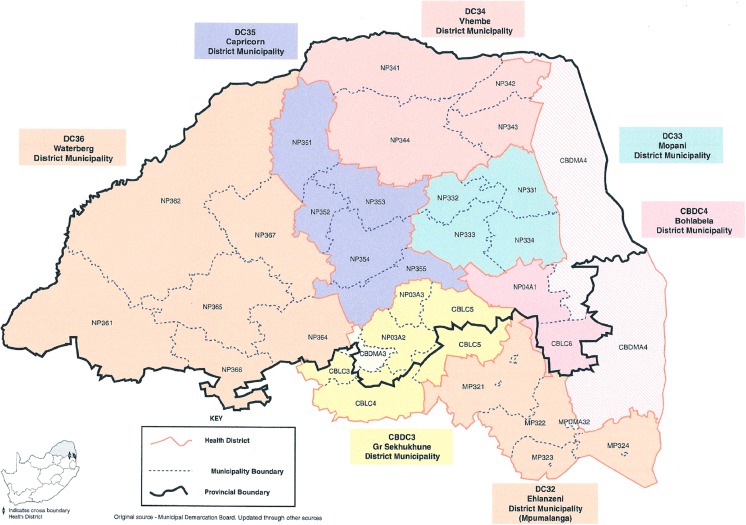
Fig. 1.
Map of the Greater Sekhukhune district of Limpopo Province
Greater Sekhukhune is one of six health districts in Limpopo, South Africa’s northern-most province. The district has one secondary care (regional) hospital, St. Rita’s Hospital, which serves six primary care (district) hospitals and these are networked to 75 clinics. There are also six community health centres and mobile clinics (HST 2006). The health district’s southern border lies almost equidistant by road from Polokwane, the capital of Limpopo province, and Johannesburg, the site of the Division of Human Genetics, National Health Laboratory Service (NHLS) and Faculty of Health Sciences, University of the Witwatersrand. It was thus conveniently situated for a collaborative clinical genetic outreach programme involving the Limpopo Department of Health and Social Development and the Division of Human Genetics, NHLS and University of the Witwatersrand.
Limpopo province demography and health services
In 2006, when GraSCOP was being planned, Limpopo Province had a population of 5.671 million people, approximately 12 % of the country’s population, living in an area of 123,910 km2 (10.2 % of the country’s landmass). The population is sparsely distributed, approximately 45.5 people per square kilometre, and most people (86.7 %) live in rural areas. The vast majority (94 % or 5.323 million people) of this population depended on the public health care system (HST 2006). This comprised 37 hospitals, 30 district (primary care) hospitals, 5 regional (secondary care) hospitals and 2 tertiary (academic) hospitals, one in Polokwane and the other at Mankweng, 30 km east of Polokwane. These hospitals were supported by a network of 433 clinics, 26 community health centres and 130 mobile clinics (Dr. J. McCutcheon, Limpopo Department of National Health and Social Development, personal communication). The healthcare budget for Limpopo Province of period April 2006 to March 2007 was ZAR 5,228 million (approximately ZAR 7 to US$1), 10.5 % of national healthcare budget (HST 2006).
The healthcare facilities were staffed by 883 medical doctors, including community service doctors, 75 medical specialists and 5,827 professional nurses. There were 14.8 doctors/100,000 people and 110.3 professional nurses/100,000 people. However, 26.8 % of medical posts and 15 % of professional nursing posts were vacant (HST 2006).
The number of births in Limpopo Province was approximately 140,290 annually. Of the women who deliver, an estimated 93.4 % receive antenatal care, and 87.7 % of births were assisted by hospital staff and are therefore hospital or clinic based. The infant mortality rate in 2006 was 37/1,000 live births (HST 2006).
Primary health care practitioner training with the medical genetic education programme
To initiate GraSCOP, 38 nurses and 6 primary health care doctors from St. Rita’s Hospital and its 6 referring primary care hospitals were offered training with the MGEP. The MGEP is a distance learning medical genetic education programme developed by South African medical geneticists and medical genetic counsellors in collaboration with the Genetic Services Sub-Directorate of the National Department of Health. It is now the primary vehicle for post-graduate medical genetic training of nursing staff in the country.
When offered in Greater Sekhukhune for the GraSCOP, a feature of the two MGEP courses was the inclusion of the six primary health care doctors on the courses, one from each of the primary care hospitals. The two courses were undertaken by 44 participants and the examination results, for those that completed the course, were similar to those from previous courses held elsewhere in the country. The difference was that eight (18 %) candidates did not attend all the contact teaching days (four) and complete the course and therefore could not write the examination. This was exceptional for these two MGEP courses. In the past, never more than 5 % of candidates did not complete a course. At the time the training was being done, the dropout rate was noted, but no valid reason was obvious.
During the GraSCOP, a third MGEP course was undertaken, in collaboration with the Limpopo Department of Health and Social Development, in which a trial of the MGEP contact day teaching was done by tele-teaching to hospital-based tele-conferencing facilities. Prior to undertaking the tele-teaching, previously genetic-trained nursing staff were trained to act as facilitators to assist the teaching at each of the teaching sites. This was the first attempt at undertaking the MGEP contact day teaching in this manner and was very successful: 86 % of the candidates passed the examination. Further piloting of tele-teaching of the MGEP programme contact days will now be undertaken, hopefully with similar results. Doing the contact day teaching for MGEP in this manner ensures the course can be taught to more nurses and doctors at significantly less cost, with less travel and inconvenience to both students and lecturers.
Clinical genetic outreach clinics to St. Rita’s Hospital
The training of the doctors and nursing staff with MGEP was to enable them to recognise infants and children in their hospitals with congenital disorders, initiate relevant investigations, possibly clinically diagnose the more common congenital disorders and undertake treatment and counselling appropriate to their situation. They were then intended to refer these patients, with their parents, to the regular outreach clinics held at St. Rita’s Hospital by medical geneticists and medical genetic counsellors of the Division of Human Genetics. It was also proposed that the nursing staff or doctor attend these clinics with their patients.
The purpose of nursing staff and doctors attending the outreach clinics with their patients was so that they could receive further ‘on the job’ teaching, training and support from the outreach clinical genetic staff. To accommodate the expected number of patients that would attend the outreach clinics, these were initially held monthly. From the outset, the outreach clinics were poorly attended by patients and staff from the referring primary care hospitals. Despite efforts to improve this situation, it was never resolved. Patients seen at the outreach clinics were mostly those diagnosed and being treated at St. Rita’s Hospital, the secondary care hospital.
Reasons were sought for this failure to network the primary care hospitals to St. Rita’s for the outreach clinics. Two cogent and interconnected reasons were determined. When the protocol for GraSCOP was developed in 2006, there were 26.8 % vacancies in medical practitioner posts and 15 % for nursing posts in the Limpopo Province (HST 2006). The 2008 figures record a significant increase in vacancies, to 35.4 % for medical practitioners and 43.7 % for nursing staff. In 2008, 42.1 % of all health professional posts in the public health sector in Limpopo Province were vacant. This, with the burden of HIV/AIDS and TB in the Province, was placing huge stress on the health services, including on available health professionals, in the Province (HST 2006).
The care and prevention of congenital disorders must rate a lower priority in these circumstances. Hospital managers considered they could not release doctors and nurses from their post to attend the outreach clinics. Obviously, in these circumstances, undertaking epidemiological studies was also not possible. This is also an explanation why so many candidates did not complete the MGEP course.
During the GraSCOP project, 68 patients with congenital disorders were assessed at St. Rita’s Hospital. They had a wide range of different diagnoses including myotonia congenita, an undescribed AD pigmentary abnormality, Noonan syndrome, osteogenesis imperfecta, Down syndrome, trisomies 13 and 18, undiagnosed patients with dysmorphic features and developmental delay, microcephaly, macrocephaly, hyrocephalus, limb defects and ambiguous genitalia. Most of the referrals were considered appropriate, the patients requiring diagnosis, advice on particular clinical problems and counselling. The patients were seen with St. Rita’s Hospital staff, thus affording them the opportunity to receive teaching, training and advice during the clinics.
It was noted during the GraSCOP that between outreach clinics communication between St. Rita’s Hospital and the Division of Human Genetics staff was at times difficult. Towards the end of the project, to try and overcome the problem, cell phones capable of taking photographs were given to the paediatrician and the neonatal ward at St. Rita’s Hospital. With the cell phones, photographs of 16 infants and children with congenital disorders with dysmorphic features were taken and transmitted to the Division of Human Genetics. Reviewing the photographs and other clinical details obtained by fax or through cell phone conversation, a clinical geneticist in the Division of Human Genetics offered a tentative diagnosis and suggested relevant investigations and treatment to the attending staff at St. Rita’s Hospital. The patient and their parents were then followed up at the next genetic outreach clinic. To date, this has mostly been used to assist in the diagnosis and treatment of neonates with congenital disorders. Although in its early stages, this appears to be an acceptable way to offer clinical support to clinicians in rural areas like Greater Sekhukhune. Further formal evaluation, in a specifically designed research project, of the use and role of cellular phones with cameras to assist primary health care practitioner with the care of children with congenital disorders is recommended.
The experience of GraSCOP clearly indicates the need for countries in sub-Saharan Africa, who will have similar or poorer health services than those present in South Africa, to undertake in-depth health needs assessment when initiating and developing services for the care and prevention of congenital disorders. What was of concern in this situation is how quickly the staffing situation in Limpopo Province deteriorated and the effect this had on the possibility of providing basic primary health care for infants and children with congenital disorders.
Clinical utility of QF-PCR for the postnatal diagnosis of Down syndrome
During GraSCOP, the clinical utility of quantitative fluorescence polymerase chain reaction (QF-PCR) for the postnatal diagnosis of Down syndrome, using the EuroGentest criteria, was evaluated in the circumstances pertaining to South Africa (CAPABILITY 2010).
Down syndrome is a common congenital disorder in South Africa (Christianson 1996). A birth prevalence of 2.1 per 1,000 live births was previously recorded in a rural hospital in Limpopo Province (Venter et al. 1995). A retrospective audit of chromosomal analyses done in the Division of Human Genetics cytogenetic laboratory from January 2007 to May 2008 documented that 653 specimens were received with a clinical diagnosis of Down syndrome. In 12 % of these specimens, a test result could not be obtained because of failed lymphocyte culture growth due to problems occurring before the specimens arrived at the laboratory. The most common problem was prolonged specimen transit time. Normal chromosome results were found in 33 % of specimens analysed and 1 % had a diagnosis different from Down syndrome. A diagnosis of Down syndrome was confirmed in only 54 % of the specimens received.
These findings confirm previous reports that doctors and nurses have difficulty making a clinical diagnosis of Down syndrome in black infants in South Africa. This research documented that in Down syndrome infants and children, only 16 % of the Down syndrome infants were diagnosed in the early neonatal period and less than 50 % before 6 months of age (Christianson 1996). It also raised the logistical problem of transporting specimens within the time frame, and in the conditions, required to maintain lymphocyte viability for their successful culturing.
Analysis of specimens with a diagnosis of Down syndrome forms a significant proportion of the work undertaken in the Division of Human Genetics cytogenetic laboratory. The laboratory’s workload has been increasing year on year while the number of cytogeneticists to do the work had decreased. There are very few cytogeneticists in South Africa and replacing staff that leave is difficult. The consideration was therefore developed to use QF-PCR for the postnatal diagnosis of Down syndrome, to relieve the excessive workload on staff in the cytogenetic laboratory. In addition, this solved the specimen transport problem. DNA, the transport of which is easier and not constrained by time and exacting conditions, would be used for testing as opposed to requiring live lymphocytes. Initially, it was planned to use only specimens from Greater Sekhukhune for the clinical utility evaluation of QF-PCR for the postnatal diagnosis of Down syndrome.
Due to the cytogenetic laboratory losing 50 % of its staff in early 2008 (still not replaced), after consultation with senior academic paediatricians in Limpopo Province and at the Universities of Pretoria and the Witwatersrand, Gauteng Province, this was extended, as a necessity, to include all specimens with a clinical diagnosis of Down syndrome received in the laboratory. Lectures were given to paediatricians in the referral area of the Division of Human Genetics on QF-PCR and its use, including counselling information for patients with positive results. A fact sheet on this was sent to doctors referring patients to the Division of Human Genetics and accompanied test results for patients confirmed by QF-PCR as having Down syndrome. Information from a medical geneticist or genetic counsellor is also available on a designated phone line in the Division of Human Genetics.
By May 2010, 1,288 specimens with a clinical diagnosis of Down syndrome were analysed by QF-PCR. A diagnosis of Down syndrome was confirmed in 818 specimens (63.5 %) and not confirmed in 470 specimens (36.5 %), results similar to the audit in the cytogenetic laboratory, considering that the problem of failed lymphocyte culture was eliminated by doing QF-PCR. QF-PCR cannot differentiate translocation Down syndrome and misses 30 % of mosaic Down syndrome in those patients with low mosaicism in the blood. These drawbacks were considered acceptable in the circumstances pertaining in the division’s cytogenetic laboratory, given that QF-PCR is also approximately 30 % less expensive than routine cytogenetic analysis and results are available in 48–72 h. Using QF-PCR testing in this way reduced the cytogenetic laboratory’s workload by 34 %. Since QF-PCR was implemented for the postnatal diagnosis of Down syndrome, there have been no objections or known refusals to use the test from any doctors. Many have utilised the open contact line in the Division of Human Genetics to obtain information. The parents of only one patient demanded routine cytogenetic analysis instead of QF-PCR for their child.
For a test to have clinical utility, EuroGentest considers it should meet the criteria listed below:
-
The natural history of the disease, if known, should be considered so that testing and intervention can be properly timed.
The natural history of Down syndrome is well known. The timing of postnatal diagnostic testing for Down syndrome should be when the diagnosis is first suspected. Given the limitations of doctors and nurses in South Africa to clinically diagnose Down syndrome in infants, the need for a diagnostic test is essential to confirm or deny the diagnosis.
-
Interventions that might follow a positive test should be effective and available.
The World Health Organisation has stated that ‘developing’ countries should provide the ‘best possible care available’ for people with genetic and congenital disorders (WHO 1985, 1999). Effective care for people with congenital disorders, diagnosis, treatment and counselling is available throughout South Africa. It varies significantly in quality between rural settings, where primary health care facilities prevail, and urban areas, where primary health care has easier access to secondary and tertiary care. However, infants and children in underserved areas can be diagnosed, basic treatment given (e.g. for cardiac failure), counselled by genetic trained nursing staff if available and referred to secondary and tertiary care hospitals should this be necessary. In addition, community-based rehabilitation is available from primary and secondary care hospitals.
-
Qualified pre-test and post-test measures, including appropriate consent processes and genetic counselling, should be in place when needed.
Genetic counselling for the parents of infants and children with Down syndrome is obviously not universally available in South Africa. However, counselling from other health care practitioners, nurses, primary care medical practitioners, paediatricians and obstetricians is available in the different health care settings. The training of nurses and primary health care medical practitioners in the basics of medical genetics, including imbuing counselling skills, is recognised in the National Department of Health’s ‘National guidelines for the management and prevention of genetic disorders, birth defects and disabilities’ (National Department of Health 2001). Support is also available to health care practitioners from the four academic departments of human genetics in the country. Pre-test consent for testing is practiced throughout the country—a practice that all practitioners have become particularly aware of, and competent at, because of the HIV/AIDS epidemic. To an extent, limited by prevailing circumstances, this criterion is met.
-
Health risks associated with testing and interventions following positive and negative test results as well as with not testing should be considered.
There are no health risks associated with postnatal testing of Down syndrome with QF-PCR. Treatment for infants and children with Down syndrome is essential. Infants and children with Down syndrome not afforded treatment have a high mortality rate and poor long-term developmental outcome. A mortality rate of 65 % for infants and children with Down syndrome by age 2 years has previously been documented in Limpopo Province (Christianson et al. 2002).
-
The financial costs and benefits should be evaluated.
Using QF-PCR for the postnatal diagnosis of Down syndrome is significantly cheaper than routine cytogenetic analysis, in part because the test is less labour intensive and also because of the need for repeat tests due to negated culture failure.
QF-PCR is also faster, a result being available 48 h after the specimen reaches the laboratory as opposed to 10 to 14 days for routine cytogenetic analysis. This latter figure would be in a well-staffed laboratory, but is not possible in the Division of Human Genetics cytogenetic laboratory due to staff shortages.
Finally, and of particular import, was that using QF-PCR for the postnatal diagnosis of Down syndrome reduced the workload of the cytogenetic laboratory by a third. Had this not been achieved, the consideration was that routine cytogenetic analysis for patients clinically diagnosed with Down syndrome would have had to be withdrawn, and no diagnostic test would have been available.
-
Testing services should provide educational materials, access to genetic counselling and maintain surveillance over their activities.
Written educational material on the use of QF-PCR was, and continues to be, distributed to medical practitioners requesting the test. Lectures on the topic were also given, and these will be repeated as necessary.
The main drawback to using QF-PCR for the postnatal diagnosis of Down syndrome is that it does not distinguish between trisomy 21, translocation Down syndrome and chromosome 21 mosaicism. In the audit of the cytogenetic laboratory, of the specimens confirmed with Down syndrome, 95 % were trisomy 21, 3.6 % had Robertsonian translocations and 1.4 % were mosaic.
Of the 3.6 % of Down syndrome infants diagnosed who would have a translocation involving chromosome 21, half would be familial and the other half appear de novo. The parents of the infant with familial translocation Down syndrome would be at high risk in subsequent pregnancies of having another child with Down syndrome. The educational material that accompanies positive results for Down syndrome explains this. It also advises that this is explained to all parents, and that mothers are urged to seek counselling about prenatal diagnosis early in future pregnancies. Medical practitioners are also asked to specifically request cytogenetic analysis in all Down syndrome patients with a family history of Down syndrome.
It also has to be accepted that a small number of infants with mosaic Down syndrome will not have their diagnosis confirmed with QF-PCR. In the event a medical practitioner is concerned about a negative result with QF-PCR, they are advised to refer the child to a paediatric or medical genetic clinic for evaluation.
In the manner described above, it is hoped to minimise these problems of using QF-PCR for the postnatal diagnosis of Down syndrome. However, in the circumstances pertaining in South Africa, these problems were considered minimal by comparison to the alternatives—not offering any genetic diagnostic test for infants or children with Down syndrome or losing more cytogeneticists because of work stress and having to close the laboratory.
We consider the EuroGentest approach to evaluating clinical utility of medical genetic tests confirms the current clinical utility of QF-PCR for the postnatal diagnosis of Down syndrome in South Africa. In addition, using QF-PCR should be considered by other middle- and low-income countries initiating and developing services for the care and prevention of congenital disorders.
Conclusion
The knowledge and experience gained from the GraSCOP have serious implications for medical genetic services regarding the care and prevention of congenital disorders in Limpopo Province and, by extension, throughout South Africa. Other provinces are similarly, and in some cases, worse affected by staff shortages and the HIV/AIDS and TB epidemics. Developing medical genetic services in these circumstances will be difficult and it is proposed that Health Needs Assessment is the objective way to clarify matters and plan future medical services for the care and prevention of congenital disorders (CAPABILITY 2010).
Despite barriers to implementing services for the care and prevention of congenital disorders, as encountered in GraSCOP, South Africa and other middle- and low-income nations must persevere with their development. The WHO has recently prioritised such services for middle- and low-income countries, noting that they are necessary to help them achieve their Millennium Development Goals (WHO 2010a, b). Numerous interventions are available for middle- and low-income nations that are both effective and cost-efficient (WHO 2000, 2010a; Christianson et al. 2006). Their implementation can be assisted by innovations like those pioneered in GraSCOP tele-teaching for education and training, using cellular phones to improve clinical care of infants and children with congenital disorders in rural areas and the use of QF-PCR for the postnatal diagnosis of Down syndrome and other autosomal trisomies to assist laboratory service provision.
Acknowledgments
The authors would like to acknowledge Mrs. B. Kruger for assistance with the QF-PCR project and Mrs. S. Walters with teaching the MGEP programme. The work was undertaken as a part of the CAPABILITY project funded by a grant from the European Commission’s 6th Framework Programme (contract number LSSG-CT-2006-067275).
Footnotes
A congenital disorder is defined as any structural or functional abnormality that is present from birth. Serious congenital disorders can cause death or disability. The term congenital disorder is synonymous with birth defect, the term often preferred in America (Christianson et al. 2006; WHO 2007).
This article will be part of the special issue: Capability/GenTEE.
References
- CAPABILITY (2010) The CAPABILITY report. Model approaches for capacity building for the translation of genetic knowledge into practice and prevention. www.capabilitynet.eu/Documents/Reports2.%20Recommendations.pdf. Accessed 12 May 2011
- Christianson AL. Down syndrome in sub-Saharan Africa. J Med Genet. 1996;33:89–92. doi: 10.1136/jmg.33.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christianson AL, Venter PA, Modiba JH, Nelson MM. The development of a primary health care clinical genetic service in rural South Africa—the Northern Province experience 1990–1996. Community Genet. 2000;3:77–84. doi: 10.1159/000051108. [DOI] [Google Scholar]
- Christianson AL, Zwane ME, Manga P, Rosen E, Venter A, Downs D, Kromberg JGR. Children with intellectual disability in rural South Africa: prevalence and associated disability. J Intellec Disabil Res. 2002;46(2):179–186. doi: 10.1046/j.1365-2788.2002.00390.x. [DOI] [PubMed] [Google Scholar]
- Christianson AL, Howson CP, Modell B (2006) March of Dimes global report on birth defects: the hidden toll of dying and disabled children. March of Dimes Birth Defects Foundation, White Plains, USA. Available at: www.marchofdimes.com/globalprograms. Accessed 1 May 2011
- Health Systems Trust (HST) (2006) South African health review. Available at http://www.hst.org.za. Accessed 13 Dec 2012
- National Department of Health (2001) Policy guidelines for the management and prevention of genetic disorders, birth defects and disabilities. Department of Health, Pretoria, South Africa. http://www.doh.gov.za/docs/policy/humangenetics.pdf. Accessed 18 Jun 2013
- Venter PS, Christianson AL, Hutamo CM, Makhura MP, Gericke GS. Congenital anomalies in rural black South African neonates—a silent epidemic? S Afr Med J. 1995;85(1):15–20. [PubMed] [Google Scholar]
- WHO (1985) Community approaches to the control of hereditary diseases. Report of an advisory group. Geneva, Switzerland: World Health Organization
- WHO (2000) Primary health care approaches for prevention and control of congenital and genetic disorders. Geneva, Switzerland: World Health Organization
- WHO (2010a) Birth defects. Report by the Secretariat for the 125th session of the Executive Board. Geneva, Switzerland: World Health Organization. Available at http://apps.who.int/gb/ebwha/pdf_files/EB126/B126_10-en.pdf. Accessed 13 Dec 2012
- WHO (2010b) Sixty-third World Health Assembly adopts resolutions on MDGs, infant feeding, pneumonia, and birth defects. Available at http://www.who.int/child_adolescent_health/news/archive/2010/17_5_10/en/. Accessed 13 Dec 2012
- WHO/March of Dimes (2007) Management of birth defects and haemoglobin disorders. Geneva, Switzerland: World Health Organization
- World Health Organisation/World Alliance for the Prevention of Birth Defects (1999) Services for the prevention and management of genetic disorders and birth defects in developing countries. Geneva, Switzerland: World Health Organization