Abstract
Study design
A single-center institutional review board-approved prospective cross-sectional observational study.
Context
Urodynamic studies are essential to accurately direct bladder management following spinal cord injury (SCI). There is no consensus on how often testing should be performed.
Objective
To determine the impact of annual urodynamic studies on guiding bladder management following SCI.
Methods
Individuals with traumatic SCI undergoing annual urological evaluations were enrolled in this study. They had to be injured for at least 2 years so that urodynamic changes could be compared with their previous annual urodynamic evaluation. Changes in the urodynamic parameters and autonomic dysreflexia were determined by comparing this study with the previous year's study. All studies were done with the same physician and nursing staff. Demographic data, bladder management, urodynamic parameters, and the need and type of interventions based on the urodynamic study were obtained. The main outcome measure was whether or not there was a need for an intervention based on the urodynamics. Interventions were classified as urological intervention, non-urological intervention, or a combination of urological and non-urological intervention. The impact of the type of bladder management, length of injury, and level of injury was also evaluated.
Results
Ninety-six consecutive individuals with SCI undergoing annual urodynamic evaluations were enrolled over a 5-month period. Overall, 47.9% of individuals required at least one type of intervention based on urodynamic studies: 82.6% were urological interventions (medication changes were most common, comprising 54.3% of urological interventions); 13.0% were non-urological interventions; and 4.3% were a combination of non-urological and urological interventions. The need for interventions did not appear to be influenced by the type of bladder management, the length of time post-injury or level of injury.
Conclusion
Annual urodynamic evaluation plays an important role in guiding bladder management following SCI.
Keywords: Spinal cord injuries, Morbidity, Tetraplegia, Paraplegia, Urology, Neurogenic bladder, Urodynamics, Bladder management, Detrusor sphincter dyssynergia, Autonomic dysreflexia
Introduction
Since World War I, there has been a significant decline in urological causes of death after spinal cord injury (SCI). Mortality related to renal complications after SCI has decreased from 80% in World War I to 40% in World War II to 25% during the Korean War to minimal numbers during the Vietnam War to the present.1 Important reasons for this decline include a better understanding of the significance of changes in bladder and sphincter physiology following SCI, and improved bladder management based on urodynamic monitoring and upper tract evaluation.
There is a strong consensus that urodynamic evaluation is essential to urological evaluations because clinical evaluation alone is not sufficient2–5 However, there is less agreement regarding the ideal frequency of testing. For example, for the person with no urological complaints, some healthcare professionals recommend a yearly evaluation for the first 5 years followed by an evaluation every 2 years until the 10th year and then yearly; some recommend yearly evaluation for the first 5–10 years and then every other year.6 Some patients are not scheduled for urodynamic evaluation unless they are having urinary symptoms.
For the past 20 years, our urology department has evaluated individuals with SCI on an annual basis regardless of the presence or absence of symptoms, type of management, or length of injury. This prospective study was undertaken to determine the usefulness of annual urodynamics on bladder management in individuals with SCI. We are not aware of any studies that have specifically investigated the impact of an annual urodynamic evaluation on bladder management.
Methods
A 5-month prospective institutional review board-approved cross-sectional observational study of consecutive individuals with SCI coming in for annual urological evaluations was undertaken. Individuals had to have been injured for at least 2 years and had to have had a urodynamic evaluation the previous year so that any changes in bladder/sphincter function from prior years could be evaluated.
Demographic data included gender, age of the individual at the time of evaluation, length of injury, level of injury, and completeness of injury using the American Spinal Injury Association impairment score (AIS).7 For purposes of this study, the levels of injury were grouped with regard to bladder function and the potential for autonomic dysreflexia (AD). Group 1: C1–T6 was those most likely to develop AD with bladder filling, Group 2: T7–T11 was those most likely to have an overactive detrusor, and Group 3: T12–S2 was more likely to have an underactive detrusor.
All individuals underwent our standard urodynamic protocol. Following a pretest urine sample, they were placed on a culture-specific antibiotic. Our policy was to not only treat for prevention of possible post-urodynamics urinary tract infection or sepsis, but to assure that there was no inflammation of the bladder wall prior to the urodynamic study. Individuals with no bacteriuria were given a single dose of antibiotic 1 hour prior to testing. Those with bacteriuria and pyuria were treated for 3–5 days prior to testing depending on the amount of pyuria and presence or absence of symptoms.
On the day of testing, individuals underwent a urological history and physical examination, and a review of the previous urodynamics by the urologist (T.A.L.). The individuals were set-up in a lithotomy position and underwent a multichannel urodynamic evaluation. Urodynamic parameters included the vesical pressure (Pves), urethral pressure (Pura), detrusor pressure (Pdet), abdominal pressure (Pabd), and flow rate. Careful blood pressure monitoring was performed in individuals with injuries at thoracic (T)6 or above. The fill rate was 60 ml per minute. Blood pressures were taken at the beginning and throughout the study. If there was a change in either the urodynamic parameters or blood pressures (AD) from the previous year, the study was repeated a second time to confirm the changes. All of the studies were done under direct supervision of the urologist. This protocol and urologist have not changed in the past 20 years.
Based on the annual urodynamic evaluation, the criteria used by the authors to recommend that an intervention be undertaken are shown in Table 1. The main outcome of this study was whether or not a person needed an intervention based on these criteria. The urodynamic evaluation led to at least one of the following management strategies: urological intervention, non-urological intervention, or a combination of urological and non-urological interventions. There were no standardized interventions. Individuals were informed of the risks, benefits, and alternatives of treatment and an intervention was decided upon. Follow-up by the SCI medical service was recommended if there was an increase in AD compared with previous years, but no significant change in bladder and sphincter function. In these cases AD was most likely to be due to non-urological issues such as chronic constipation. While not part of this study, all patients also had a renal scan just prior to or shortly after their annual urodynamics study.
Table 1.
Criteria used to recommend an intervention
| • New onset or increased force of involuntary contractions (>40 cm H20) |
| • New onset of autonomic dysreflexia (BP > 140 mm/Hg systolic) due to a urological cause (increased detrusor overactivity, increased detrusor sphincter dyssynergia or post-void residual) |
| • New onset of autonomic dysreflexia not felt to be due to a urological cause (no change from previous urodynamic parameters) |
| • New onset of decreased bladder wall compliance (causing increased intravesical pressure) |
| • Resumption of previous urodynamic bladder/sphincter dysfunction due to discontinuation of previously prescribed medications |
| • Need to change current bladder management due to patient dissatisfaction/new problems |
Results
A total of 96 consecutive individuals with traumatic SCI were evaluated in this prospective study. The gender, age of patient at time of urodynamic evaluation, length of injury, level of injury, and AIS is shown on Table 2. The male-to-female ratio was 5 to 1. It is not possible to determine an exact ratio of tetraplegia to paraplegia because of the groupings. However, using the C2–T6 (70 individuals)/T7–S2 (25 individuals) groupings, the ratio is 3.6/1. With the exception of one individual who complained of skin breakdown from his external condom catheter, none of the individuals in this study complained of new urological problems since their previous urodynamic evaluation. The types of interventions based on the urodynamic findings/complaints are shown on Table 3.
Table 2.
Demographics
| Gender | Male: 80; female: 16 |
| Age at evaluation (years): | Average: 44.6, range: 18–80 |
| Length of injury | 2–5 years (32), 6–10 years (13), 11–16 years (21), >16 years (30) |
| Level of injury | C1–T6: (73), T7–T11: (13), T12–S2: (10) |
| American Spinal Injury Association impairment score (AIS) | A: (73) B: (18) C: (1) D: (4) |
Overall, 47.9% (46 of 96) of individuals required some type of intervention (urological or non-urological or combination of both) based on their annual urodynamic study using the criteria listed on Table 1. 39.6% (38 of 96) of the individuals required urological interventions. Urological changes in management were most common, comprising 82.6% (38 of 46) of all interventions. The individual with penile skin breakdown had no changes in bladder function; however, urodynamics helped to determine other bladder management options. Only non-urological interventions were needed in 10.9% (5 of 46). (These individuals had a new onset of AD during monitoring despite no other changes in urodynamic parameters from previous evaluations. They were referred to the SCI clinic for further evaluation.) An additional 6.5% (3 of 46) needed a combination of urological medication and non-urological intervention.
The single most common intervention was a medication change. Overall, 69% (32 of 46) of individuals requiring interventions needed urological medication interventions (with or without other types of interventions). Of these, 6 individuals resumed taking a medication, 19 began a new medication, 7 increased dosage of a medication, and 1 decreased dosage of a medication.
Because of very similar rates of intervention with regard to the various bladder managements, the various lengths of injury and various levels of injury, which would therefore require a very large sample size, it was not possible to determine whether there were statistically significant differences between these groups. However, the frequency of interventions based on the criteria outlined in Table 1 was determined. Of the 7 individuals who voided with control as their bladder management method, 57.1% (4 of 7) required urodynamic-directed interventions. Of the 36 individuals who used intermittent catheterization (IC) as their method of management, 52.8% (19 of 36) required interventions. Of the 11 individuals who had reflex voiding bladder management program and 54.5% (6 of 11) required interventions. Of the 23 individuals who had an indwelling urethral catheter, 39.1% (9 of 23) required some type of intervention. Of the 19 individuals who had an indwelling suprapubic indwelling catheter, 42.1% (8 of 19) required intervention. The percentage of individuals who did and did not require intervention based on bladder management is shown on Fig. 1.
Figure 1.
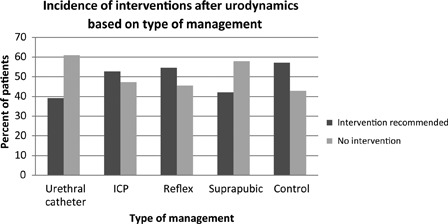
Impact of the type of bladder management on management interventions based on urodynamic findings.
The duration of injury did not seem to affect the frequency of interventions. Of individuals who had been injured for 5 years or less at the time of urodynamic evaluation, 46.9% (15 of 32) required interventions. Of those had been injured 6–10 years, 38.5% (5 of 13) required interventions. Of those injured 11–16 years, 52.4% (11 of 21) required interventions. Of those injured more than 16 years, 50% (15 of 30) required interventions. The percentage of individuals who did and did not require interventions based on length of injury is shown on Fig. 2.
Figure 2.
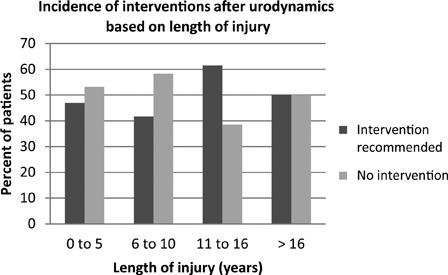
Impact of the length of injury on management interventions based on urodynamic findings.
The level of injury also did not seem to affect the frequency of interventions, as shown on Fig. 3. It should be noted that while there were no obvious differences in frequency of interventions based on the level of injury in any of the groupings, the C2 to T6 group was the largest (70 individuals) and is therefore expected to be the most representative. In this group, 51% required interventions, compared with 49% who did not require interventions.
Figure 3.
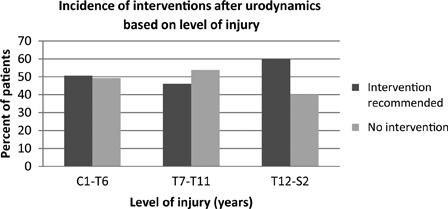
Impact of the level of injury on management interventions based on urodynamic findings.
The majority of individuals had undergone yearly renal scans. None of them had stasis or hydronephrosis of the upper tracts. The impact of the AIS on management interventions was not evaluated because of the predominance of individuals with AIS A.
Discussion
Urodynamic studies remain an essential component of initial urologic evaluation after SCI. It has been shown that while the physical examination can predict general bladder and sphincter function, it cannot predict specific urodynamic parameters that may affect the upper tracts.8 For example, information regarding degree of detrusor sphincter dyssynergia (which may cause high voiding pressures), prolonged duration of bladder contractions and post-void residuals, would not be able to be determined by a person's history.9–12
Urodynamic studies are important to assess bladder and sphincter function regardless of the type of bladder management. This is to assure that intravesical pressures are kept at a minimum. High intravesical pressures impair urine flow from the upper tracts by obstructing flow through the ureterovesical junction and ureteral orifice prior to entering into the bladder. One role of urodynamic studies is to evaluate the effectiveness of anticholinergic medication for those on IC. A common misconception is that urodynamic studies are not needed for those with indwelling catheters because the urine flows freely through the catheter out of the bladder. However, there is potentially more risk of upper tract stasis and hydronephrosis in those with indwelling catheters, because the catheter itself may trigger involuntary contractions resulting in high intravesical pressures. The potential problem in those with an indwelling catheter is obstructed urine flow at the ureterovesical junction into the bladder, not obstructed drainage through the catheter out of the bladder. Thus, it is even more imperative that intravesical pressures are monitored and effectively managed in those with indwelling catheters.12
Urodynamic studies are also an important way to determine the degree of detrusor sphincter dyssynergia in those who reflexly void, whether they are on an alpha-blocker, or had a sphincterotomy or other type of management of their sphincter.
Some healthcare providers may consider only performing urodynamics when an individual with SCI develops urological symptoms rather than has an annual evaluation. However, symptoms have been found to have a poor correlation with urodynamics and management decisions. One study compared results of urodynamic testing to clinical symptoms reported by patients and the results of ultrasound examinations evaluating treatment failures. The authors found clinical symptoms and/or results of ultrasound examinations were not sufficient to direct treatment. They found that if they had relied solely on clinical symptoms, 68.75% of the treatment failure would not have been detected.12 We had similar results in our study. All of the patients were coming in for their routine annual examination. Five of our 96 (5.2%) patients reported a new onset of problems in their bladder management since their last evaluation. We have significant concerns about waiting until a person has symptoms to perform urodynamic testing. Symptoms may not occur until a person has an irreversible or severe problem. For example, a person on IC or indwelling catheter may begin to have a gradual decrease in bladder capacity, increase in bladder wall trabeculation (fibrosis) and a decrease in bladder wall compliance. Eventually these anatomic problems become severe enough that the person develops lower tract symptoms such as incontinence or AD. They may have also developed upper tract hydronephrosis due to a gradual increase in intravesical pressure. At this point, management becomes very difficult due to irreversible anatomic changes of the bladder wall.
We also have concerns about only performing urodynamic studies in individuals with an abnormal upper tract study, such as renal scan or renal ultrasound. Upper tract studies do not give any specific information about bladder and sphincter function. As seen in this study, our urological interventions were based on urodynamic findings, despite a normal renal scan to prevent upper tract deterioration. However, upper tract studies are important because an abnormal upper tract study does help to direct the urgency and aggressiveness and follow-up of the interventions.
Table 3.
Urodynamic findings/complaints requiring interventions
| Type of bladder management | Changed urodynamic findings/complaints (each line indicates a separate patient) | Type of intervention |
|---|---|---|
| Intermittent catheterization (n = 19) | ↑ Involuntary contractions | Urological |
| ↓ Sphincter overactivity (incontinence) | Urological | |
| ↑ Involuntary contractions | Urological | |
| Difficulty passing catheter (sphincter)/AD (new) | Urological/non-urological | |
| Low leak point pressure/incontinence | Urological | |
| Involuntary contractions (new)/poor hand function | Urological | |
| ↑ Involuntary contractions | Urological | |
| ↓ Bladder wall compliance (new) | Urological | |
| ↑ Involuntary contractions | Urological | |
| ↑ Involuntary contractions/AD (new) | Urological | |
| Involuntary contractions (new) | Urological | |
| ↑ Involuntary contractions despite anticholinergic medication | Urological | |
| ↑ Involuntary contractions/decreased capacity | Urological | |
| ↑ AD | Urological | |
| ↑ Involuntary contractions | Urological | |
| ↑ Involuntary contraction/pain with caths | Urological | |
| ↓ Bladder wall compliance | Urological | |
| Involuntary contractions (new) | Urological | |
| ↑ Involuntary contractions on anticholinergic | Urological | |
| Suprapubic (n = 8) | ↓ Bladder wall compliance | Urological |
| Involuntary contraction (new)/AD (new) | Urological | |
| Involuntary contractions (new)/dry mouth | Urological | |
| ↑ Involuntary contractions | Urological | |
| ↓ Bladder wall compliance | Urological | |
| Low BP (new)/↓ bladder wall compliance | Urological/non-urological | |
| AD (new) | Non-urological | |
| ↑ Involuntary contractions | Urological | |
| Indwelling urethral catheter (n = 9) | ↑ AD | Non-urological |
| ↓ Bladder capacity/AD (new) | Urological/non-urological | |
| ↑ Involuntary contractions/AD (new) | Urological | |
| Involuntary contractions (new) | Urological | |
| ↑ Involuntary contractions/↓ bladder capacity | Urological | |
| ↑ Involuntary contractions | Urological | |
| ↑ AD (new) | Non-urological | |
| ↓ Bladder capacity/involuntary contractions (new) | Urological | |
| ↑ AD | Non-urological | |
| Voids with control (n = 4) | ↑ Leak point pressures (valsalva voiding) | Urological |
| ↑ Leak point pressures (valsalva voiding) | Urological | |
| ↑ Leak point pressure/↑ post void residual (PVR) | Urological | |
| ↓ Bladder wall compliance | Urological | |
| Reflex voiding(n = 6) | ↑ PVR | Urological |
| ↑ PVR and urinary tract infections | Urological | |
| ↑ voiding pressure | Urological | |
| Normal voiding pressures/penile skin breakdowns | Urological | |
| Involuntary contraction (new)/AD (new) | Urological | |
| ↑ AD | Non-urological |
While there is agreement on the importance of urodynamic evaluations, data are limited on long-term outcomes from annual evaluations. One retrospective study evaluated the usefulness of 5 years of annual urodynamic evaluations in 80 individuals with SCI. The investigators found that the treatment strategies based on urodynamic studies had to be modified in all but three individuals in order to preserve the upper tracts. At initial presentation, 51 patients performed IC, 7 had indwelling catheters, 10 utilized reflex voiding, 2 patients presented with a Brindley stimulator, and 10 patients used abdominal straining. At the end of the 5-year review, no patients had signs of upper tract damage. To achieve this goal, 8 patients underwent sphincterotomy, 3 received a Brindley stimulator, 3 underwent bladder augmentation, 1 had a Kock pouch, 12 received intravesical botulinum A toxin, and 22 received intravesical anticholinergic therapy.12
Our study was not designed to determine the optimal schedule for bladder testing in individuals with SCI. Further studies are needed to answer this question. Although this study does not prove that an annual evaluation is preferable to other frequencies of testing, it does show the usefulness of an annual urodynamic evaluation. Overall, 47.9% (46 of 96) of those undergoing their annual evaluation needed some type of intervention based on their urodynamic study. It was interesting to note that there was no obvious difference in the number of individuals needing interventions based on their urodynamic values based on the various types of bladder management. One would expect that patients with indwelling catheters would require more interventions than those using other types of management. One reason that this may not have been the case is that the individuals in this study had had multiple urodynamics and interventions for many years. It is possible that acutely, one type of management may have required more treatment than another, but once the conditions stabilized, the need for interventions became similar. In addition to helping to direct interventions, another advantage of a yearly annual urodynamic studies is that it serves as a baseline study for the following year.
The annual urodynamic evaluation was helpful in reinforcing the importance of taking a medication that had previously been prescribed. Urodynamic studies identified 15 individuals who required a change in their alpha-blocker or anticholinergic dosage or method of administration. Five of those (33%) had stopped taking their alpha-blockers or anticholinergic medication. The major reason for stopping was lack of any perceived benefits from the medications. Therefore, the annual urodynamic checkup was important because we were able to reemphasize and readjust their medications. Urodynamic studies also provided a visual means of reinforcing the need to continue required medications, and educating patients who needed their medication dosage increased. A man who was a reflex voider had started having problems with skin breakdowns from his external condom catheter. In this case, urodynamic studies helped determine which alternative bladder management program would work best for him.
This study also emphasized another important role of urodynamic testing. In addition to bladder and sphincter function, the urodynamic test was very helpful at evaluating AD in those with injuries at T6 and above. Blood pressure monitoring during urodynamics is especially helpful, since it has been reported that more than 40% of SCI individuals have ‘silent AD’ and do not give a history or have awareness that they develop dysreflexia.13
Not only do urodynamic studies help identify AD, but by comparing current findings with prior urodynamic studies it is possible to determine whether the severity of AD has gotten better or worse. In this study, AD usually occurred with one of three situations: a new onset of involuntary contractions from the previous year, an increase in force or duration of involuntary contractions from a previous year, or from increased problems with constipation from a previous year. Urodynamic studies can also be helpful in excluding the bladder/sphincter as a cause of a new onset of AD. If the person develops AD, yet all of the urodynamic parameters are the same as the previous year, it is likely that the cause of the AD is a non-urological issue such chronic constipation, a pressure ulcer (sometimes inadvertently lying on it during a urodynamic evaluation), or other noxious stimuli.
Conclusions
Following SCI, there are a large number of individuals who require interventions based on an annual urodynamic evaluation. In our experience, the annual urodynamic evaluation identified individuals who required interventions in management, or further urological or non-urological evaluations.
Acknowledgements
We thank the urology nurses, Barbara Harrison, Jody Crecco, and Ciel Jacalan, who helped with the urodynamic studies.
References
- 1.Donnelly J, Hackler RH, Bunts RC. Present urological status of the World WAR II paraplegic: 25-year follow up. Comparison with status of the 20-year Korean War Paraplegic and 5 year Vietnam Paraplegic. J Urol 1972;108(4):558–62 [DOI] [PubMed] [Google Scholar]
- 2.Schurch B, Schmid DM, Kaegi K. Value of sensory exam in predicting bladder function in patients with T12-L1 fractures and spinal cord injuries. Arch Phys Med Rehabil 2003;84(1):83–8 [DOI] [PubMed] [Google Scholar]
- 3.Schurch B, Schmid DM, Karsenty G, Reitz A. Can neurologic examination predict type of detrusor sphincter-dyssynergia in patients with spinal cord injury? Urology 2005;65(2):243–6 [DOI] [PubMed] [Google Scholar]
- 4.Shenot PJ, Rivas DA, Watanabe T, Chancellor MB. Early predictors of bladder recovery and urodynamics after spinal cord injury. Neurourol Urodyn 1998;17(1):25–9 [DOI] [PubMed] [Google Scholar]
- 5.Wyndaele JJ. A critical review of urodynamic investigations in spinal cord injured patients. Paraplegia 1984;22:138–44 [DOI] [PubMed] [Google Scholar]
- 6.Linsenmeyer TA, Culkin D. APS recommendations for the urological evaluation of patients with spinal cord injury. J Spinal Cord Med 1999;22(2):139–42 [DOI] [PubMed] [Google Scholar]
- 7.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011;34(6):535–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wyndaele JJ. Correlation between neurological data and urodynamic function in spinal cord injured patients. Spinal Cord 1997;35(4):213–6 [DOI] [PubMed] [Google Scholar]
- 9.Wyndaele JJ. Urology in spinal cord injured patients. Paraplegia 1987;25:267–9 [DOI] [PubMed] [Google Scholar]
- 10.Killorian W, Gray M, Bennet JK, Green BG. The value of urodynamics and bladder management in predicting upper urinary tract complications in male spinal cord injury patients. Paraplegia 1992;30:437–41 [DOI] [PubMed] [Google Scholar]
- 11.Gerridzen RG, Thijssen AM, Dehoux E. Risk factors for upper tract deterioration in chronic spinal cord injury patients. J Urol 1992;147:416–8 [DOI] [PubMed] [Google Scholar]
- 12.Nosseir M, Hinkel A, Pannek J. Clinical usefulness of urodynamic assessment for maintenance of bladder function in patients with spinal cord injury. Neurourol Urodyn 2007;26:228–23 [DOI] [PubMed] [Google Scholar]
- 13.Linsenmeyer TA, Campangnolo DI, Chou IH. Silent autonomic dysreflexia during voiding in men with spinal cord injuries. J Urol 1996;155(2):519–22 [PubMed] [Google Scholar]


