Abstract
Objective
Clinical guidelines exist to promote antibiotic stewardship, particularly in ambulatory care settings such as the emergency department (ED). However, there is limited evidence on prescribing practice for persons with spinal cord injury and disorder (SCI/D). The goal of this study was to assess trends in antibiotic prescribing in the ED setting for persons with SCI/D.
Design
A retrospective dynamic cohort study design.
Setting
ED visits that did not result in same day hospitalization over 6 years (fiscal year (FY) 2002-FY2007) in Department of Veterans Affairs (VA) facilities
Participants
Veterans with SCI/D.
Outcome measures
VA clinical and administrative databases were used to identify the cohort and to obtain demographics, diagnoses, and medications. The rate of antibiotic prescribing for ED visits was defined as the number of antibiotics/total ED visits.
Results
Veterans with SCI/D had 21 934 ED visits and 5887 antibiotics prescribed over the study period (rate of 268.4 prescriptions/1000 visits). The antibiotic prescribing rate increased from 238.8/1000 visits in FY2002 to 310.8/1000 visits in FY2007 (P < 0.0001). This increase in the rate of prescribing was seen across all patient demographics and factors assessed.
Conclusion
Although clinical guidelines for judicious use of antibiotics in persons with SCI/D have been disseminated to providers, antibiotic prescribing in an ED setting is high and continuing to rise in this population.
Keywords: Physician's practice patterns, Spinal cord injuries, Antibiotic prescribing patterns, Antibiotic resistance, Veterans, Clinical guidelines
Introduction
Antibiotic resistance is an increasing problem worldwide and antibiotic use, whether appropriate or inappropriate, is a driving force in the emergence of resistance. The emergency department (ED) has the highest rates of antibiotic prescribing in adults across ambulatory care visits ranging from 26 to 62%.1–5 From 1992 through 2000, antibiotic use in the ED in the general adult population was stable.1 However, recent data suggest increases in prescribing in the ED, particularly in those adults 65 years of age and older.2,6 Other literature has focused specifically on acute respiratory infections (ARIs), and particularly on ARIs where antibiotic treatment is rarely indicated (acute bronchitis, cough, upper respiratory infection, and laryngitis), and found decreased rates of antibiotic prescribing in the ED for these conditions.3–5,7,8
Antibiotic prescribing has been described in a number of healthcare settings in the general adult population as well as in nursing home populations. However, prescribing data are limited in populations with disabilities, such as in persons with spinal cord injury and disorder (SCI/D).9,10 Understanding prescribing patterns in the ED for this population is important because it is likely that ED physicians are treating these patients in the ED and writing prescriptions for their illnesses. Research in this population may be even more relevant because persons with SCI/D have greater need for antibiotic treatment as a result of frequent infections including urinary tract infections (UTIs), pneumonia, and pressure ulcers with associated osteomyelitis.11 In addition, as a result of these frequent infections, opportunities for inappropriate antibiotic use may be more likely than in the general patient population.
Trends in antibiotic prescribing and factors associated with prescribing have not been assessed over an extended period of time in persons with SCI/D, thus it is not clear how the trends seen in the general population compared to those with SCI/D. The goal of this study was to assess antibiotic prescribing trends in the ED for Veterans with SCI/D and identify factors associated with prescribing.
Methods
Study design and setting
A retrospective analysis of a dynamic cohort of Veterans with SCI/D receiving care at ED s in Department of Veterans Affairs (VA) facilities was conducted from 1 October 2001 through 30 September 2007 (Fiscal year (FY) 2002-FY2007). There are over 900 VA ambulatory care facilities and community-based outpatient clinics in which Veterans can receive services. This study was approved by the Hines VA Institutional Review Board and Research and Development Committees.
Data sources and covariates
Veterans were identified using an ongoing registry of Veterans with SCI/D maintained by the VA Allocation Resource Center, which is used to allocate resources to VA medical centers. Data for this cohort were obtained from the VA National Patient Care Databases Medical SAS data sets, which are administrative databases that include demographic and utilization data for all VA facilities and are updated nightly with patient medical record information from the local VA facility.12,13 The focus of this study was on outpatient management of infections, thus only ED visits (identified by ED clinic stop codes) that did not result in hospitalization on the same day were included in this analysis. In addition, factors that may be associated with antimicrobial prescribing were also collected from this database including demographic characteristics (e.g. age, gender, and race), infectious disease diagnoses defined using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9-CM) (ARIs, pneumonia, UTI, osteomyelitis, septicemia/blood stream infections), comorbid health conditions within 90 days of the visit (e.g. heart and cerebrovascular disease, dementia, chronic obstructive pulmonary disease, liver disease, diabetes, cancer, and decubitus/pressure ulcers), and VA facility geographic region.
Age was categorized into three groups (18–49 years, 50–64 years, and 65+ years) while race was classified as non-Hispanic white, non-Hispanic black, and Hispanic/other (white Hispanic, black Hispanic, Asian, and American-Indian). Hispanic and ‘other’ ethnic groups were combined due to small sample sizes. The total number of comorbidities as well as the presence of comorbid conditions (dichotomous yes or no variable) was determined. At the time of this study, there were 23 SCI centers in the VA SCI system of care. We grouped care by whether it occurred at a facility with an SCI center or a non-SCI center.
The VA Spinal Cord Dysfunction Registry (SCD-R), a national database, was used to obtain neurologic classification (tetraplegia vs. paraplegia) and characteristics of SCD (age at onset, duration of injury) for the sample.
National data extracts from the VHA Decision Support System were used to identify outpatient antibiotic prescriptions (date of prescription and type of antibiotic) within 3 days of the ED visit. These data extracts from clinical data bases contain information on medications used in the outpatient setting in the VA beginning with FY2002. Antibiotics were divided into broad- or narrow-spectrum drugs. Broad-spectrum antibiotics included the following categories: amoxicillin/clavulanate, second-generation, third-generation, and fourth-generation cephalosporins, azithromycin, clarithromycin, and fluoroquinolones.9,10,14,15
Statistical analysis
Antimicrobial prescribing was calculated as a visit-based rate defined as the number of antibiotics prescribed during an ED visit per total ED visits multiplied by 1000. The population-based rate was defined as the number of antibiotics prescribed during an ED visit per total patients with ED visits multiplied by 1000. Multivariable random-effect Poisson regression modelling was used to assess prescribing trends by year and other covariates associated with prescribing; incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were calculated. A logistic regression model with a random effect was used to assess change in the percentage of ED visits with antibiotics. The proportion of broad-spectrum antibiotics prescribed was defined as the number of ED visits with broad-spectrum antibiotics per total ED visits with antibiotics. Similar proportions were computed for different antibiotic classes. Multivariable random-effect logistic regression modelling was used to assess broad-spectrum prescribing trends by year and other covariates associated with broad-spectrum prescribing. Odds ratios (ORs) and 95% CIs were calculated. All statistical analyses were performed using STATA (STATA 11.0, 2009, College Station, TX, USA).
Results
A total of 485 826 outpatient visits occurred over the 6-year study period, of which 21 934 (4.5%) were ED visits. Table 1 describes the demographics of patients being treated during these ED visits; the majority was white men over age of 50 years with paraplegia. For those with an available date of injury (n = 8857 (40.4%)), the average age at injury was 40.1 years (median: 37.0) and the average duration of injury was 17.2 years (median: 14.9). Nearly 60% were seen at a non-SCI center and 60% were seen at a facility that was in the southern region of the U.S. The most common infection was UTI. Most had one of the comorbid conditions listed previously and about 20% had at least one infection. Ten percent of the ED visits had primary diagnoses associated with diseases of the genitourinary system. The next most common diagnoses were associated with the musculoskeletal/connective system, followed by injuries and poisonings (Table 2).
Table 1.
Demographic characteristics of 21 934 emergency department visits
| Characteristic | Number of visits (%) |
|---|---|
| Gender | |
| Male | 21 253 (96.9%) |
| Female | 681 (3.1%) |
| Age group in years | |
| <50 | 4873 (22.2%) |
| 50–65 | 10 380 (47.3%) |
| 65 + | 6681 (30.5%) |
| Race/ethnicity | |
| White, not hispanic | 13 869 (63.2%) |
| Black, not hispanic | 6042 (27.6%) |
| Hispanic/other | 2023 (9.2%) |
| Duration of injury in years | |
| <10 | 5138 (23.4%) |
| 10–20 | 2714 (12.4%) |
| 20 + | 5225 (23.8%) |
| Duration of injury unknown | 8857 (40.4%) |
| Level of injury | |
| Tetraplegia | 8260 (37.7%) |
| Paraplegia | 11 979 (54.6%) |
| Level of injury unknown | 1695 (7.7%) |
| Type of facility | |
| VA SCI Specialty Center | 8842 (40.3%) |
| VA Non-SCI Center | 13 092 (59.7%) |
| Comorbidity within 90 days of visit | |
| Yes | 13 187 (60.1 %) |
| No | 8747 (39.9%) |
| Number of sites of infection | |
| 0 | 17 511 (79.8%) |
| 1 | 4320 (19.7%) |
| 2 + | 103 (0.5%) |
| Types of infections | |
| Lower respiratory infection | 282 (1.3%) |
| Pneumonia | 275 (1.3%) |
| Septicemia | 17 (0.1%) |
| Upper respiratory infection | 485 (2.2%) |
| Urinary tract infection | 3379 (15.4%) |
| Cellulitis | 411 (1.9%) |
| Geographic region | |
| Northeast | 2192 (10.0%) |
| Midwest | 3127 (14.3%) |
| South | 12 710 (57.9%) |
| West | 3905 (17.8%) |
Table 2.
Primary ICD-9 diagnosis code for emergency department visits
| N (%) | |
|---|---|
| Infectious & Parasitic Diseases (001–139) | 255 (1.2%) |
| Malignant Neoplasms (140–209) | 130 (0.6%) |
| Other Neoplasms (210–239) | 33 (0.2%) |
| Diseases of Endocrine/Nutritional/Metabolic Systems (240–279) | 591 (2.7%) |
| Diseases of Blood and Blood Forming Organs (280–289) | 81 (0.4%) |
| Mental Disorders (290–319) | 830 (3.8%) |
| Diseases of Nervous System/Sense Organs (320–389) | 938 (4.3%) |
| Diseases of Circulatory System (390–459) | 1135 (5.2%) |
| Disease of Respiratory System (460–519) | 1636 (7.5%) |
| Disease of Digestive System (520–579) | 1196 (5.5%) |
| Diseases of Genitourinary System (580–629) | 3706 (16.9%) |
| Complications of Pregnancy, Childbirth and the Puerperium (630–679) | 8 (0.04%) |
| Diseases of Skin (680–709) | 1330 (6.1%) |
| Diseases of Musculoskeletal System/Connective System (710–739) | 2391 (10.9%) |
| Congenital Abnormalities (740–759) | 26 (0.1%) |
| Certain Conditions Originating in the Perinatal Period (760–779) | 3 (0.01%) |
| Symptoms, Signs & Ill Defined Conditions (780–799) | 3496 (15.9%) |
| Injury/Poisonings (800–999) | 2455 (11.2%) |
| Factors Influencing Health Status and Contact with Health Services (V01-V89) | 1694 (7.7%) |
5003 ED visits (22.8%) had an antibiotic prescription associated with it, which increased over the study period, from 20.1% in FY2002 to 25.9% in FY2007 (P ≤ 0.0001) (Table 3). A number of patients (17%) received more than one antibiotic for the associated visit. There were 5887 antibiotics prescribed at a rate of 268.4 prescriptions per 1000 visits. The antibiotic prescribing rate increased from 238.8 per 1000 visits in FY2002 to 310.8 per 1000 visits in FY2007 (random effect Poisson regression model IRR 1.05, 95% CI 1.04–1.07, P < 0.0001). This increase in rate of prescribing was seen across all patient demographics and factors assessed. In the regression model, factors associated with higher rates of prescribing included Veterans with an injury of 10 or more years, having a pressure ulcer, not residing in the Northeast, and total number of infections (Table 4). For specific infections, the highest rates of prescribing were seen in those with UTI (IRR 3.2, 95% CI 3.0–3.4) or lower respiratory infection (LRI) (IRR 3.2, 95% CI 2.7–3.7) (data not shown). Lower prescribing rates were seen for Black patients and at VA SCI centers.
Table 3.
Antibiotic prescribing for emergency department visits by year
| Fiscal year | Number of antibiotics | Number of ED visits | Rate of antibiotic use per 1000 visits | Number of visits with antibiotics | Percent of visits with antibiotics | Number of visits with broad-spectrum antibiotics | Percent of antibiotic visits with broad-spectrum antibiotics | Number of broad-spectrum antibiotics | Percentage of antibiotics that were broad-spectrum |
|---|---|---|---|---|---|---|---|---|---|
| 2002 | 843 | 3530 | 238.8 | 710 | 20.1 | 454 | 63.9 | 506 | 60.0 |
| 2003 | 810 | 3275 | 247.3 | 699 | 21.3 | 444 | 63.5 | 474 | 58.5 |
| 2004 | 927 | 3577 | 259.2 | 793 | 22.2 | 452 | 57.0 | 497 | 53.6 |
| 2005 | 1086 | 3919 | 277.1 | 930 | 23.7 | 563 | 60.5 | 618 | 56.9 |
| 2006 | 1006 | 3724 | 270.1 | 859 | 23.1 | 488 | 56.8 | 532 | 52.8 |
| 2007 | 1215 | 3909 | 310.8 | 1012 | 25.9 | 567 | 56.0 | 633 | 52.1 |
| Total | 5887 | 21 934 | 268.4 | 5003 | 22.8 | 2968 | 59.3 | 3260 | 55.3 |
Table 4.
Factors associated with prescribing in multivariable random-effect Poisson regression model
| Characteristic | IRR | 95% CI |
|---|---|---|
| Year | 1.04 | 1.02–1.05* |
| Black (vs. White race) | 0.86 | 0.80–0.92* |
| Hispanic/other | 1.00 | 0.89–1.13 |
| Duration of injury 10+ years (vs. <10 years) | 1.15 | 1.06–1.24* |
| Duration of injury unknown | 0.95 | 0.87–1.04 |
| Paraplegia (vs. tetraplegia) | 0.97 | 0.91–1.03 |
| Level of injury unknown | 0.70 | 0.60–0.82* |
| SCI center (vs. non-SCI center) | 0.89 | 0.83–0.95* |
| Pressure ulcer (vs. no pressure ulcer) | 1.14 | 1.06–1.23* |
| Number of infections | 3.00 | 2.85–3.16* |
| Midwest region (vs. Northeast) | 1.26 | 1.11–1.43* |
| West region | 1.22 | 1.08–1.37* |
| South region | 1.13 | 1.02–1.26* |
*Variables statistically significant at the <0.05 level.
In over half (59.3%) of the ED visits with antibiotics, broad-spectrum antibiotics were prescribed (3260 broad-spectrum prescriptions) (Table 3). The rate of broad-spectrum prescriptions decreased from 63.9% in FY2002 to 56.0% in FY2007 (random effect logistic regression model OR 0.93, 95% CI 0.90–0.97, P < 0.0001); decreasing by approximately 1% per year. The decrease in broad-spectrum use was largely driven by fluoroquinolones, which comprised 42.7% of antibiotics (Fig. 1A). The rate of prescribing for other antibiotics also decreased over time (Fig. 1B), except for trimethoprim/sulfamethoxazole, which increased from 8.5% in FY2002 to 13.2% in 2007 (P = 0.001) and contributed to the overall increase in antibiotic prescribing.
Figure 1.
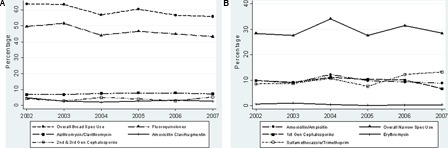
(A) Percentage of broad-spectrum antibiotics prescribed among emergency department visits in which antibiotics were prescribed. (B) Percentage of narrow-spectrum antibiotics prescribed among emergency department visits in which antibiotics were prescribed.
Discussion
The ED is a common location of care where antibiotics are prescribed and often overused.2,6 In this study, approximately one in five patients with SCI who visited an ED department in the 6-year study timeframe were prescribed antibiotics (22.8%). Although clinical guidelines for judicious use of antibiotics have been disseminated,16,17 the rate of antibiotic prescribing in the ED setting continues to rise.
The rate of prescribing was lower for Blacks than Whites, which has been shown in other studies.7,18 Although this may indicate better care for non-white populations, this could also be an artifact of disparate use of medical services. Therefore, it may still be important to develop interventions that narrow gaps in quality, in addition to narrowing gaps in utilization of services. Veterans seen at a VA SCI center had a somewhat lower prescribing rate (IRR = 0.89) than those seen at non-SCI centers, suggesting that specialty care at these centers may promote better quality of care and possibly more judicious use of antibiotics due to familiarity with the population. For example, ED staff at SCI centers may have greater awareness of asymptomatic bacteriuria and associated urinalysis findings and be less likely to inappropriately diagnose a UTI in a patient with SCI/D. Geographic region was also significantly associated with prescribing rates. Vanderweil et al.7 also found that prescribing for URIs was higher in the southern region of the United States.
Approximately 17% of ED visits resulted in prescribing of more than one antibiotic. Since we used a 3-day timeframe for prescription, this may in part reflect a change in prescriptions when culture results become available, e.g. narrowing the antibiotic spectrum based on urine culture and sensitivity.
We found that the number and type of infections were significantly predictive of an antibiotic prescription (IRR = 3.0) and patients diagnosed with a UTI or LRI had the highest rates of antibiotic prescribing. In the SCI population UTIs are fairly common as are complications from such infections,9,19 so antibiotic prescriptions to treat these bacterial infections is typically appropriate. Lower respiratory tract infections as well as other acute respiratory infections are common as well in SCI.20 In accordance with guidelines, most of the common upper and lower respiratory tract infections, excluding pneumonia, should not be treated with antibiotics because they are primarily viral, antibiotics provide little to no benefit.17,21 There have been few studies to assess prescribing for these infections in the SCI/D population. This is of particular importance in persons with SCI/D, because of increased risk for pneumonia and mortality due to pneumonia.20 A previous study found that 55.9% of non-pneumonic LRI visits (95% of which were for acute bronchitis) led to prescriptions for antibiotics, suggesting room for improvement in reducing use.9 A subsequent study assessed the impact of antibiotic prescribing for acute respiratory infection (ARI) on subsequent healthcare utilization in veterans with SCI/D and found that for a subset of patients, there was no impact on healthcare utilization if the patient received or did not receive an antibiotic.10 However, in patients with certain chronic respiratory conditions (cough, shortness of breath, bronchitis not specified as acute or chronic, and allergic rhinitis), antibiotic prescriptions were associated with lower risk of return for an outpatient visit, suggesting that in the absence of chronic respiratory conditions, antibiotic use for ARI can be curbed for those at high risk for respiratory complications, such as this population.10
Our findings demonstrate that though there have been increase in overall antibiotic use, the proportion of broad-spectrum antibiotics prescribed has decreased over time in the ED. This result is contrary to previous work that showed overall broad-spectrum antibiotic prescribing (including both ED and non-ED care) increasing for ARIs in this patient population.9 Overall, 50% of antibiotics prescribed in this study were broad spectrum and antimicrobial stewardship strategies are still relevant to reduce use of these antibiotics as they may contribute to development and spread of antimicrobial resistant organisms. Education efforts may be needed for SCI providers and even ED providers (who may be treating patients with SCI in the ED) regarding appropriate antimicrobial use.22 Ranji et al.23 found that active clinician education in combination with other strategies may be one of the more effective strategies in reducing inappropriate antibiotic prescribing, but these programs need to be specifically tailored to clinicians' training and specialty. A recent survey of SCI/D clinicians found that the vast majority who responded to the survey endorsed the need to improve knowledge of appropriate antibiotic prescribing to reduce antibiotic resistance.24
There are several limitations to this study. Healthcare and prescriptions outside of the VA were not captured. However, the VA system of care and available data provide a national snapshot of antibiotic prescribing in a large population of persons with SCI/D. Data were also missing for some injury characteristics which limits the ability to assess the association between these characteristics and antibiotic prescribing. Most importantly, we were unable to determine whether the antibiotic prescribing was appropriate or inappropriate. The finding that prescription rates were higher in the ED setting compared with other outpatient settings could indicate inappropriate prescribing (e.g. prescribed for asymptomatic bacteriuria in a patient seen for non-UTI complaints) or that ED visits are more likely than other outpatient visits to be due to infectious disease conditions.
Conclusion
Although clinical guidelines for judicious use of antibiotics have been disseminated, the rate of antibiotic prescribing in the ED setting is high and is continuing to rise in this population. In this study, prescriptions from the ED setting accounted for about one sixth of all outpatient antibiotic exposures in this population. Broad-spectrum antibiotic prescribing is decreasing, but there is still room for improvement in reducing use of these antibiotics. Over-prescribing of antimicrobials is likely to contribute to the emergence of antibiotic resistant organisms as well as affect the incidence, severity, and management of infections. This issue is of particular importance to patients with SCI/D because of their increased susceptibility to UTI and decubitus wound infection and their frequent use of antimicrobial agents. Education efforts focused on appropriate antimicrobial use may be needed for not only SCI/D providers but also ED providers, who may treat SCI patients in the ED.
References
- 1.McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis 2003;9(5):609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCaig L, Friedman CR. Trends in antimicrobial prescribing in ambulatory care settings in the United States, 1993–2004. Poster abstract. 2006 Annual Conference on Antimicrobial Resistance, June 26–28, 2006, Bethesda, Maryland, USA [Google Scholar]
- 3.Stone S, Gonzales R, Maselli J, Lowenstein SR. Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: a national study of hospital-based emergency departments. Ann Emerg Med 2000;36(4):320–7 [DOI] [PubMed] [Google Scholar]
- 4.Roumie CL, Halasa NB, Grijalva CG, Edwards KM, Zhu Y, Dittus RS, et al. Trends in antibiotics prescribing for adults in the United States – 1995 to 2002. J Gen Intern Med 2005;20(8):697–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thorpe JM, Smith SR, Trygstad TK. Trends in emergency department antibiotic prescribing for acute respiratory tract infections. Ann Pharmacother 2004;38(6):928–35 [DOI] [PubMed] [Google Scholar]
- 6.Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA 2009;302(7):758–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vanderweil SG, Pelletier AJ, Hamedani AG, Gonzales R, Metlay JP, Camargo CA., Jr. Declining antibiotic prescriptions for upper respiratory infections, 1993–2004. Acad Emerg Med 2007;14(4):366–9 [DOI] [PubMed] [Google Scholar]
- 8.Gonzales R, Camargo CA, Jr, MacKenzie T, Kersey AS, Maselli J, Levin SK, et al. Antibiotic treatment of acute respiratory infections in acute care settings. Acad Emerg Med 2006;13(3):288–94 [DOI] [PubMed] [Google Scholar]
- 9.Evans CT, Smith B, Parada JP, Kurichi JE, Weaver FM. Trends in antibiotic prescribing for acute respiratory infection in veterans with spinal cord injury and disorder. J Antimicrob Chemother 2005;55(6):1045–49 [DOI] [PubMed] [Google Scholar]
- 10.Evans CT, Li K, Burns SP, Smith B, Lee TA, Weaver FM. Antibiotic prescribing for acute respiratory infection and subsequent outpatient and hospital utilization in veterans with spinal cord injury and disorder. PM R 2010;2(2):101–9 [DOI] [PubMed] [Google Scholar]
- 11.Montgomerie JZ. Infections in patients with spinal cord injuries. Clin Infect Dis 1997;25(6):1285–90 [DOI] [PubMed] [Google Scholar]
- 12.VA Information Resource Center (VIREC) HSR&D National Patient Care Database (NPCD) The FY99 SAStm Datasets for the Patient Treatment File (PTF). Hines, IL: VA Information Resource Center; 2000 [Google Scholar]
- 13.VA Information Resource Center (VIREC) HSR&D National Patient Care Database (NPCD) The FY99 SAStm Datasets for the Outpatient Care File (OPC). Hines, IL: VA Information Resource Center; 2000 [Google Scholar]
- 14.Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med 2003;138(7):525–33 [DOI] [PubMed] [Google Scholar]
- 15.Mainous AG, III, Hueston WJ, Davis MP, Pearson WS. Trends in antimicrobial prescribing for bronchitis and upper respiratory infections among adults and children. Am J Public Health. 2003;93(11):1910–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shlaes DM, Gerding DN, John JF, Duncan RA, Eckman MR, Farrer WE, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis 1997;25(3):584–99 [DOI] [PubMed] [Google Scholar]
- 17.Gonzales R, Bartlett JG, Besser RE, Cooper RJ, Hickner JM, Hoffman JR, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med 2001;134(6):479–86 [DOI] [PubMed] [Google Scholar]
- 18.Vanderweil SG, Tsai CL, Pelletier AJ, Espinola JA, Sullivan AF, Blumenthal D, et al. Inappropriate use of antibiotics for acute asthma in United States emergency departments. Acad Emerg Med 2008;15(8):736–43 [DOI] [PubMed] [Google Scholar]
- 19.Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med 2002;113Suppl. 1A:67S–79S [DOI] [PubMed] [Google Scholar]
- 20.Burns SP. Acute respiratory infections in persons with spinal cord injury. Phys Med Rehabil Clin N Am 2007;18:203–16, v–vi [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomised controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ 1998;316(7135):906–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evans CT, Rogers TJ, Weaver FM, Burns SP. Providers' beliefs and behaviors regarding antibiotic prescribing in persons with spinal cord injury or disorder. J Spinal Cord Med 2011;34(1):16–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ranji SR, Steinman MA, Shojania KG, Sundaram V, Lewis R, Arnold S, et al. Closing the quality gap: a critical analysis of quality improvement strategies (Vol. 4: Antibiotic Prescribing Behavior). Rockville, MD: Agency for Healthcare Research and Quality (US); 2006. (Technical Reviews, No. 9.4.) Available from: http://www.ncbi.nlm.nih.gov/books/NBK43956/ [PubMed] [Google Scholar]
- 24.Evans CT, Rogers TJ, Burns SP, Lopansri B, Weaver FM. Knowledge and use of antimicrobial stewardship resources by spinal cord injury providers. PM R. 2011;3(7):619. [DOI] [PubMed] [Google Scholar]


