Abstract
We examined major trends and patterns regarding sodium and potassium intake and the ratio of sodium and potassium in the diets of South Koreans. We analyzed detailed 24-hour dietary recall data collected from 10,267; 8,819; and 9,264 subjects ages two years and older in the 1998, 2005, and 2009 Korean National Health and Nutrition Examination Surveys, respectively. Mean sodium intake did not change significantly between 1998 and 2009 (4.6 g/d vs 4.7 g/d), while potassium intake increased significantly [2.6 g/d vs. 2.9 g/d (p < 0.001)]. The major dietary sodium sources were kimchi, salt, soy sauce, and soybean paste, and most potassium came from unprocessed foods (white rice, vegetables, kimchi, and fruits). About 50 percent of the participants consumed 4 or more grams of sodium per capita per day. The proportion of respondents consuming 4 to 6 grams of potassium per capita per day increased from 10.3 percent in 1998 to 14.3 percent in 2009 (p < 0.001), and the sodium-potassium ratio decreased from 1.88 to 1.71 (p < 0.001). One major implication is that efforts to reduce sodium in processed foods will be ineffective and future efforts must focus on both education to reduce use of sodium in food preparation and sodium replacement in salt, possibly with potassium.
Keywords: diet, sodium, potassium, trend, pattern, the ratio of sodium to potassium
INTRODUCTION
Hypertension is a major risk factor for morbidity and mortality, particularly in East Asia (1). Globally, cardiovascular disease (CVD) is the number one cause of mortality, and in 2008 a major component was stroke and other forms of cerebrovascular disease (2), with some estimates of roughly 25 percent of all CVD deaths linked to hypertension. Gastric cancer is the most common cancer worldwide, with age-standardized 2007 incidence rates of 40.4 and15.9 cases per 100,000 person-years for men and women, respectively (3).
South Korea is known to have a very high incidence of both hypertensive disease and stomach cancer, with the former responsible for 9.6 percent of total mortality in 2010 (4, 5). Stomach cancer is equally significant, and the South Korean diet is implicated in this problem (6, 7). High sodium intake is seen as a major cause of both stomach cancer and hypertension. Potassium has been found to be protective in both epidemiological and clinical studies, showing that a high-potassium diet lowers blood pressure in individuals with raised average blood pressure (8).
The traditional South Korean diet is generally high in sodium. According to a 2009 government report on the country’s nutritional status, South Koreans consumed 4.6 grams of sodium per capita per day and 2.5 grams of potassium per capita per day (9). This is far greater than the World Health Organization (WHO) recommendation of 2 grams of sodium per capita per day, though potassium intake is within the limits established by the WHO of 70–80 mmol (2.7–3.1 g) per capita per day (10). No previous studies have examined sodium and potassium intake patterns and sodium-potassium ratio in South Korea. Using nationally representative data from the Korean National Health and Nutrition Examination Survey (KNHANES), this study examines sodium and potassium intake from individual dietary surveys for the period 1998– 2009.
METHODS
Study Population
KNHANES is a cross-sectional health and nutrition study of nationally representative samples of noninstitutionalized South Korean civilians ages 1 year and older. KNHANES is based on a multistage, stratified area probability sample of noninstitutionalized South Korean households in different geographic areas and in different age and sex groups. Baseline data were collected in 1998 with follow-up exams in 2001, 2005, and 2007–9. Weights indicating the probability of being sampled were assigned to each respondent, enabling the results to represent the entire South Korean population. The 1998 and 2001 KNHANES were conducted by the Korea Institute for Health and Social Affairs (KIHASA) and the Korea Health Industry Development Institute (KHIDI); the 2005 KNHANES was conducted by the KIHASA, the KHIDI, and the Korea Centers for Disease Control and Prevention (KCDC). The 2007–9 KNHANES was conducted solely by the KCDC (11).
For the purposes of this study, we used data from individuals ages 2 years and older from KNHANES 1998, 2005, and 2009. Final sample sizes were n=10,267, n=8,819, and n=9,264; respectively.
Dietary Data
A single twenty-four-hour dietary recall was collected from each respondent through in-person interviews. Recipes for all food items consumed were also collected. To enhance recall, particularly for away-from-home food consumption, actual food shapes and two-dimensional models of plates and bowls were used to assist the respondent’s report of the volumes of the food items consumed (12) . Based on the recipes collected from each household during the interview, the weight of each ingredient was estimated from the volume of food ingested. Sodium and potassium intake was then calculated using information from the Korean Food Composition Tables (13) and the recipe database for the KNHANES (14). We present measures of grams per capita per day (g/capita/d) that take into account nonconsumers and the percent consuming each of the food groups examined.
Selected Food Items
Food groups for this study were created using the system developed at the University of North Carolina at Chapel Hill (UNC). The UNC food-grouping system categorizes and groups individual US Department of Agriculture (USDA) food items from multiple studies over time to ensure comparable food and nutrient compositions. It is important to note that USDA food groups were broken into more detailed, nutrient-based food categories using a systematic method described in detail elsewhere (15). Additional food groups were added to represent unique Korean foods.
From the UNC food groups, sodium-rich seasonings and specific food items were separated based on their proportionate contribution to total daily sodium and potassium levels. Specifically, foods were listed in descending order of proportionate contribution to sodium (or potassium) intake. Foods representing 0.2 percent or more of total daily intake of sodium (or potassium) were selected for inclusion.
The final food groups for sodium included seasonings (salt, seasoning powder [MSG], soy sauce, soybean paste, fermented red pepper paste, and other seasonings), kimchi (traditional fermented cabbage), ramen (Korean noodles), processed meat (ham, sausage, bacon, and others), other noodles and pasta, other sauces, and milk and milk/soy drinks. For potassium the final good groups included vegetables, kimchi, fruits, white rice, starches, seaweeds, milk and milk/soy drinks, plain fish, coffee and tea, pork, soybean paste, plain poultry and poultry dishes, beef, ramen, and other foods.
Statistical Analysis
All statistical analyses were conducted using SAS (release 9.2; Cary, NC, USA). The χ2-test was used to compare the percentage of demographically variable groups by year. The student t-test was also used to assess differences in consumption (per capita and per consumer) across mean intakes of sodium and potassium. All statistical tests compare 1998 and 2009 only with ρ < 0.05 set for statistical significance.
RESULTS
The distributions of respondents’ demographic factors are presented in table 1. Mean age of the sample increased slightly between 1998 and 2009. Levels of education and income changed significantly between 1998 and 2009. Specifically, there were increases in those with more than a high school education and at the highest level of income. Residence in rural areas decreased.
Table 1.
Distribution of demographic factors in KNHANES1, 1998, 2005 and 2009
| Demographic group | 1998 | 2005 | 2009 | P value for percent4 |
|||
|---|---|---|---|---|---|---|---|
|
| |||||||
| No. of subjects |
Percent | No. of subjects |
Percent | No. of subjects |
Percent | ||
| Sample size (n) | |||||||
| Number of Individuals | 10,400 | 100 | 8,930 | 100 | 9,391 | 100 | |
| Mean of Age2 | 33.1±0.4 | 35.3±0.3 | 37.3±0.4 | <0.001 | |||
| Age groups (%) | |||||||
| 2-6 y | 875 | 7.9 | 631 | 5.8 | 663 | 4.9 | 0.0723 |
| 7-12 y | 911 | 9.1 | 915 | 9.1 | 889 | 7.2 | |
| 13-18 y | 980 | 10 | 747 | 8.1 | 738 | 8.9 | |
| 19-39 y | 3,416 | 35.4 | 2,511 | 34.8 | 2,248 | 32.5 | |
| 40-59 y | 2,565 | 24.5 | 2,574 | 28 | 2,517 | 30.5 | |
| 60 y+ | 1,520 | 11.6 | 1,441 | 13.2 | 2,209 | 15.1 | |
| Gender (%) | |||||||
| Male | 4,984 | 48.7 | 4167 | 50.2 | 4,182 | 50.2 | <0.01 |
| Adults (≥19 y) education (%) | |||||||
| <High school diploma | 3,236 | 36.7 | 2,338 | 30.7 | 3,091 | 35.3 | <0.001 |
| ≥High school diploma | 4,276 | 63.3 | 4,201 | 69.3 | 3,909 | 64.7 | |
| Income as percentage of poverty (%)3 | |||||||
| Low (<120%) | 3,671 | 32.7 | 1,878 | 19.9 | 2,526 | 23.5 | 0.1884 |
| Middle (120-250%) | 4,340 | 45.9 | 3,495 | 40.1 | 3,292 | 37 | |
| High (≥250%) | 1,961 | 21.5 | 3,403 | 39.9 | 3,443 | 39.5 | |
| Region (%) | |||||||
| Large City | 4,130 | 47.9 | 4,102 | 47.1 | 4,069 | 46.4 | <0.05 |
| Small City | 2,658 | 32 | 3,089 | 35.2 | 3,320 | 37.2 | |
| Rural | 3,612 | 20.1 | 1,739 | 17.7 | 2,002 | 16.4 | |
Weighted to be nationally representative.
Mean±Standard Error.
Calculated values based on poverty threshold of each year.
χ2- test comparing the percent of each demographic group between 1998 and 2009.
Sodium: Trends and Sources
Mean sodium intake was 4.6 g/capita/d, 4.5 g/capita/d, and 4.7 g/capita/d in 1998, 2005, and 2009, respectively (table 2) and did not change significantly during this time period. But the mean sodium intake of females decreased from 4.1 g/capita/d in 1998 to 3.9 g/capita/d in 2009 (p < 0.01), whereas male intake significantly increased from 5.1 g/capita/d in 1998 to 5.5 g/capita/d in 2009 (p< 0.001). Mean sodium intake for most age groups decreased except in the middle-aged group (ages 40–59 years), whose consumption increased from 5.1 g/capita/d in 1998 to 5.3 g/capita/d in 2009 (p < 0.05). We also measured total salt intake (table 2). The results show that in 2009 for rural, small city and large cities the intake was 11.8 g/capita/d, 11.5 g/capita/d and 12 g/capita/d, respectively. Average national salt intake levels in 2009 was 11.8 g/capita/d.
Table 2.
Sodium (Salt) and Potassium Intake (grams/day) in South Korea, 1998, 2005 and 2009
| Demographic group |
Sodium (Salt) intake, g/d/capita | Potassium intake, g/d/capita | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1998 | 2005 | 2009 | P value1 |
1998 | 2005 | 2009 | P value2 |
|
| Age groups | ||||||||
| 2-6 y | 2.3 ( 5.8) | 2.3 (5.8) | 2.0 (5.0) | <0.01 | 1.6 | 1.7 | 1.7 | 0.2769 |
| 7-12 y | 3.6 ( 9.0) | 3.6 (9.0) | 3.3 (8.3) | 0.1323 | 2.3 | 2.3 | 2.3 | 0.4215 |
| 13-18 y | 4.2 (10.5) | 4.2 (10.5) | 4.1 (10.3) | 0.3492 | 2.4 | 2.4 | 2.5 | 0.184 |
| 19-39 y | 5.2 (13.0) | 4.8 (12.0) | 5.2 (13.0) | 0.6875 | 2.9 | 2.6 | 3.1 | <0.01 |
| 40-59 y | 5.1 (12.8) | 5.0 (12.5) | 5.3 (13.3) | <0.05 | 2.8 | 2.8 | 3.2 | <0.001 |
| 60 y+ | 4.2 (10.5) | 4.5 (11.3) | 4.1 (10.3) | 0.3132 | 2.3 | 2.5 | 2.6 | <0.01 |
| Gender | ||||||||
| Male | 5.1 (12.8) | 4.9 (12.3) | 5.5 (13.8) | <0.001 | 2.8 | 2.7 | 3.2 | <0.001 |
| Female | 4.1 (10.3) | 4.1 (10.3) | 3.9 (9.8) | <0.01 | 2.4 | 2.4 | 2.5 | <0.01 |
| Adults (≥19 y) education | ||||||||
| <High school diploma |
4.6 (11.5) | 4.6 (11.5) | 4.6 (11.5) | 0.5776 | 2.4 | 2.5 | 2.7 | <0.001 |
| ≥High school diploma |
5.1 (12.8) | 4.9 (12.3) | 5.3 (13.3) | 0.1356 | 2.9 | 2.7 | 3.2 | <0.001 |
| Income as percentage of poverty (%)3 | ||||||||
| Low (<120%) | 4.4 (11.0) | 4.4 (11.0) | 4.2 (10.5) | <0.05 | 2.4 | 2.5 | 2.5 | <0.05 |
| Middle (120- 250%) |
4.5 (11.3) | 4.5 (11.3) | 4.8 (12.0) | <0.05 | 2.6 | 2.6 | 2.9 | <0.001 |
| High (≥250%) | 4.7 (11.8) | 4.8 (12.0) | 4.9 (12.3) | 0.0878 | 2.9 | 2.9 | 3.1 | <0.01 |
| Region | ||||||||
| Large City | 4.5 (11.3) | 4.5 (11.3) | 4.7 (11.8) | <0.05 | 2.6 | 2.6 | 3.1 | <0.001 |
| Small City | 4.6 (11.5) | 4.7 (11.8) | 4.6 (11.5) | 0.6698 | 2.6 | 2.5 | 3 | <0.001 |
| Rural | 4.5 (11.3) | 4.5 (11.3) | 4.8 (12.0) | 0.062 | 2.5 | 2.6 | 2.8 | <0.001 |
|
| ||||||||
| Total | 4.6 (11.5) | 4.5 (11.3) | 4.7 (11.8) | 0.0887 | 2.6 | 2.6 | 2.9 | <0.001 |
Student t-test comparing mean per capita sodium intake between 1998 and 2009.
Student t-test comparing mean per capita potassium intake between 1998 and 2009.
Calculated values based on poverty threshold of each year.
Most individuals consumed more daily sodium than is recommended. Over 50 percent of participants consumed 4 g/capita/d or more of sodium at all three time points examined, with only 11.0 percent, 11.7 percent, and 15.9 percent consuming less than 2 g/capita/d in 1998, 2005, and 2009, respectively (table 3).
Table 3.
Distribution of Dietary Sodium and Potassium Intake (%) in South Korea, 1998, 2005 and 2009
| Group | Sodium | Potassium | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1998 | 2005 | 2009 | P value 1 | 1998 | 2005 | 2009 | P value1 | |
| < 2g/d | 11.0 | 11.7 | 15.9 | 0.2404 | 39.0 | 34.7 | 31.2 | <0.001 |
| 2-4 g/d | 35.0 | 37.8 | 34.0 | 48.1 | 54.9 | 50.6 | ||
| 4-6 g/d | 25.6 | 28.5 | 25.0 | 10.3 | 9.2 | 14.3 | ||
| ≥ 6g/d | 23.5 | 22.0 | 25.2 | 2.6 | 1.2 | 3.9 | ||
χ2- test comparing the percent of each group between 1998 and 2009.
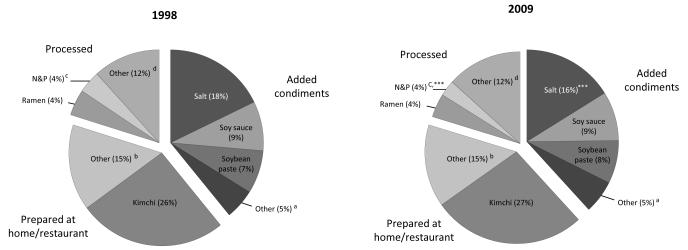
The major sources of dietary sodium were kimchi and salt, followed by soy sauce, soybean paste, and ramen. This order did not change between 1998 and 2009. Sodium intake from kimchi increased from 1.19 g/capita/d in 1998 to 1.31 g/capita/d in 2009 (p < 0.05). The absolute intake (p < 0.05) and percentage (p < 0.001) of sodium from salt decreased significantly between 1998 (0.87 g/capita/d; 17.8 percent) and 2009 (0.80 g/capita/d; 16.1 percent). MSG consumption also decreased during this time period (p < 0.001), while fermented red pepper paste and other seasonings (including such as fermented soybean paste and curry powder) increased (figure 1). Shifts in sodium intake per capita (grams), per consumer (grams), and in percentages consuming are found in Supplementary Table 1 and 2 are available at the JHH website. Per capita and per consumer changes in consumption of sodium from added condiments and some packaged, processed foods. Consumers obtained large amounts of sodium from ramen (1.46 g/consumer/d in 2009) and noodles/pasta 1.09 g/consumer/d in 2009 (see Supplementary Table 1) despite the relatively small proportions of consumers (0.14 % and 0.17% in 2009, respectively, Supplementary Table 2).
Figure 1.
Top 5 sources of dietary sodium in South Korea, 1998 and 2009
aOther added condiments
bOther unprocessed foods
cNoodles and pasta
dOther processed foods
***Percentage contribution to sodium or potassium intake between 1998 and 2009 is statistically significant, students t-test p < 0.001.
Potassium: Trends and Sources
Mean potassium intake significantly increased between 1998 and 2009, 2.6 g/capita/d versus 2.9 g/capita/d (p < 0.001). Specifically, potassium consumption among adults ages 19–39, 40–59, and 60 and older increased during this time period: 2.9 g/capita/d versus 3.1 g/capita/d (p < 0.01); 2.8 g/capita/d versus 3.2 g/capita/d (p < 0.001); and 2.3 g/capita/d versus 2.6 g/capita/d (p < 0.01), respectively. Potassium intake also increased across all levels of income and education and all regions (table 2).
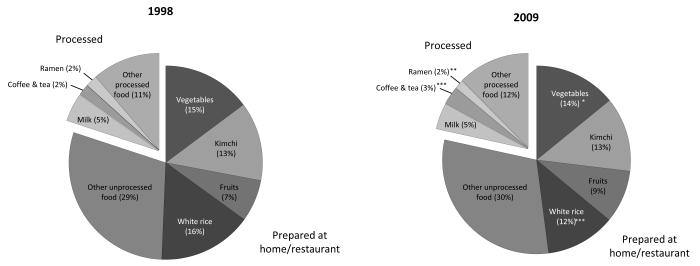
The proportion of individuals consuming 2 g/capita/d or more of potassium in 1998, 2005, and 2009 was 39.0%, 34.7%, and 31.2% respectively. At the same time persons consuming 4 to 6 g/capita/d of potassium increased significantly (p < 0.001) (table 3). Most of the potassium consumed came from unprocessed foods. In 1998 white rice was the major source of potassium, followed by vegetables, kimchi, and fruits. The major sources of potassium were not changed in 2009. There were, however, small but significant increases in potassium intake from fruits, 0.21 g/capita/d in 1998 compared to 0.31 g/capita/d in 2009 (p < 0.001), and decreases in potassium from white rice, 0.35 g/capita/d in 1998 compared to 0.29 g/capita/d in 2009 (p < 0.001) (figure 2). Shifts in potassium intake per capita (grams), per consumer (grams), and in percentage consuming are in Supplemental Tables 3 and 4. The major sources of potassium intake per consumer were fruit, followed by starch, vegetables and milk & milk/soy drinks (0.61, 0.49, 0.43 and 0.41 g/consumer/d, respectively, Supplemental Table 3). Differences between per capita and per consumer estimates were largely based on differences in the percent consuming each of these food groups (Supplemental Table 4) On the other hand, per capita and consumer mean potassium intake levels were similar for white rice and vegetables (Supplemental Table 3), for example, because large proportions of the population reported consuming each (97.0% and 97.3% in 2009, respectively, Supplemental Table 4).
Figure 2.
Top 5 sources of dietary potassium in South Korea, 1998 and 2009
*Percentage contribution to sodium or potassium intake between 1998 and 2009 is statistically significant, students t-test p < 0.05.
**Percentage contribution to sodium or potassium intake between 1998 and 2009 is statistically significant, students t-test p < 0.01.
***Percentage contribution to sodium or potassium intake between 1998 and 2009 is statistically significant, students t-test p < 0.001.
Sodium-Potassium Ratio
Table 4 shows the mean per capita sodium-potassium ratio. Between 1998 and 2009 the mean sodium-potassium ratio decreased from 1:88 to 1:71 (p < 0.001). The sodium-potassium ratio decreased in all population subgroups. And the population percentage of sodium-potassium ratio greater than 2 significantly decreased over time from 35.1% to 27%, whereas the percentage of persons with a sodium-potassium ratio 0.5, 0.5 to ≤ 1.0, and 1.0 to ≤ 2.0 increased significantly (p < 0.001) (table 5).
Table 4.
Sodium-Potassium Ratio in South Korea, 1998, 2005 and 2009
| Demographic group | 1998 | 2005 | 2009 | P value1 |
|---|---|---|---|---|
| Age groups | ||||
| 2-6 y | 1.50 | 1.46 | 1.27 | <0.001 |
| 7-12 y | 1.65 | 1.65 | 1.49 | <0.05 |
| 13-18 y | 1.88 | 1.88 | 1.73 | <0.05 |
| 19-39 y | 1.94 | 1.90 | 1.81 | <0.001 |
| 40-59 y | 1.96 | 1.86 | 1.74 | <0.001 |
| 60 y+ | 2.00 | 1.93 | 1.68 | <0.001 |
| Gender | ||||
| Male | 1.91 | 1.87 | 1.80 | <0.001 |
| Female | 1.86 | 1.81 | 1.62 | <0.001 |
| Adults (≥19 y) education | ||||
| <High school diploma | 2.04 | 1.92 | 1.78 | <0.001 |
| ≥High school diploma | 1.94 | 1.88 | 1.74 | <0.001 |
| Income as percentage of poverty (%)2 | ||||
| Low (<120%) | 1.96 | 1.84 | 1.75 | <0.001 |
| Middle (120-250%) | 1.85 | 1.78 | 1.73 | <0.01 |
| High (≥250%) | 1.78 | 1.76 | 1.67 | <0.05 |
| Region | ||||
| Large City | 1.87 | 1.74 | 1.63 | <0.001 |
| Small City | 1.85 | 1.87 | 1.63 | <0.001 |
| Rural | 1.96 | 1.84 | 1.72 | <0.001 |
|
| ||||
| Total | 1.88 | 1.84 | 1.71 | <0.001 |
Student t-test comparing mean per capita sodium-potassium ratio between 1998 and 2009
Calculated values based on poverty threshold of each year.
Table 5.
Distribution of Sodium-Potassium Ratio in South Korea, 1998, 2005 and 2009
| Group | 1998 | 2005 | 2009 | P value1 |
|---|---|---|---|---|
| Ratio ≤ 0.5 | 1.7 | 1.1 | 2.2 | <0.001 |
| 0.5 < Ratio ≤ 1.0 | 11.8 | 9.0 | 14.2 | |
| 1.0 < Ratio ≤ 2.0 | 51.4 | 56.6 | 55.7 | |
| 2.0 < Ratio | 35.1 | 33.3 | 27.9 |
χ2-test comparing the percent of each group between 1998 and 2009.
DISCUSSION
Sodium intake in South Korea is a major health risk. Most individuals consume more daily sodium than is recommended. Over 50 percent of our participants consumed 4 g/capita/d or more of sodium at all three time points examined, with fewer than 16 percent of the sample consuming the recommended < 2 g/capita/d in 2009. Per capita total salt intake was 11.8 g/capita/d in 2009. While potassium intake increased slightly, linked with a decrease in sodium-potassium ratios in all population subgroups, over 80 percent of South Koreans consumed a sodium-potassium ratio above 1.0, the highest ratio suggested in the literature.
Overall, sodium intake in South Korea is considerably higher, and potassium intake considerably lower than recommended levels (10). These trends represent an important risk factor for the health of South Korean adults, as high sodium intake has been associated with increased risk of many chronic diseases (16) and higher sodium-potassium ratios are associated with significantly increased risk of several chronic diseases (17), including cardiovascular diseases (18) and all-cause mortality (16).
We estimated the mean sodium intake was 4.5 to 4.7 g/capita/d between 1998 and 2009 in Korea. In South Korea more than half of our participants consumed twice the reference intake of 2 grams per day (g/d) between 1998 and 2009. Similar results have been found in many other countries, particularly in East Asia, with mean sodium intake exceeding recommended levels. In 1997–98 adults ages 40–59 in China consumed between 3.0 and 6.7 g/d, and those in Japan consumed between 4.3 and 4.8 g/d (19). Although sodium intake in Western countries is slightly lower than that observed in Asian countries, it is still higher than the WHO recommended levels. In 2007-2008, the average sodium intake of the U.S. population aged two years and older was 3.3 g/d (20), while that in the United Kingdom’s was 8.1 g salt (sodium 3.2 g) for adult in 2011 (21).
Although potassium intake in South Korea was lower than recommended levels, it was similar to select other research in the US, China, and other countries. For instance, usual potassium intake among American men and women, 3.3 g/capita/d and 2.4 g/capita/d, respectively in NHANES III (16), and elderly hospital patients among men and women, 3.1 g/capita/d and 2.9 g/capita/d, respectively, in Guangdong Province, China in 2007-2008 (22). Potassium intake (range; 3.2g/capita/d-4.8 g/capita/d) in the European countries participating in the European Food Consumption Validation Project (EFCOVAL) is slightly higher than that observed in South Korea, Japan, and the United States (23), but almost all countries fall short of meeting the recommended potassium intake. A more recent summary of work has shown that the average potassium intake was from 1.7 g/d in China to 3.7 g/d in Finland, the Netherlands, and Poland (24). Potassium intake in the USA was 2.8-3.3 g/d for men and 2.2-2.4 g/d for women (25).
The 2002 joint WHO–Food and Agriculture Organization of the United Nations (FAO) Expert Consultation recommended that the general population consume a sufficient amount of potassium to maintain the molar ratio of sodium to potassium of 1:1 or approximately 70–80 millimoles (mmol) of potassium per day (10). But this is controversial and some scholars recommended around 0.5 (26, 27). In the present study, the mean sodium-potassium ratio was very high, 1.71 in 2009, especially among males and those 19–39 years old (1.80 and 1.81 respectively). This level is higher than the sodium-potassium ratio observed among American men and women (1.31 and 1.23, respectively) in NHANES III (16). Although many studies reported that high sodium or low potassium intake are associated with increased risk for CVD, it is difficult to find the dietary sodium-potassium ratio linked with these same health outcomes.
Individuals did not meet the recommended intake for sodium or potassium in 1998 or 2009, and there were only minor shifts in the levels and major dietary sources of these nutrients over time. In most developed countries about 77 percent of total sodium intake comes from processed foods and only 12 percent from sodium naturally occurring in foods (28). Our study shows a very different situation in South Korea, with kimchi processed either at home (the main source) or in commercial settings contributing 26 to 27 percent of total sodium intake between 1998 and 2009. Salt and soy sauce were also significant sources of sodium intake, 16.1 percent and 8.7 percent, respectively, in 2009. What is most important to note is that these foods are processed mainly at home or are condiments added during food preparation, not packaged processed foods, as is observed regarding sodium consumption in most developed countries. Major contributors to potassium consumption have also changed very little over time and are not packaged processed foods.
The WHO’s global goal is to reduce salt intake to less than 5 grams (2,000 milligrams of sodium) per person per day by 2025 (29), and some countries are aiming for even lower levels in the longer term (30). Many countries have introduced salt reduction initiatives, often led by governments and sometimes by nongovernmental organizations but rarely by industries (31). The salt reduction strategy of the UK consisted of two principal areas of work: a consumer awareness campaign and the creation of an enabling environment by working closely with the food industry to provide clear nutrition labeling and to reformulate processed foods. China also has health promotion and educational approaches to encourage people to use less salt while cooking and they have introduced the use of a calibrated salt spoon to aid in this. In America, the National Salt Reduction is to address industry comment that sodium reduction targets should be uniform and not vary by state or local regions (32). The South Korean government has also pledged to develop national salt reduction strategies by establishing networks among government, industries and academies, and the Korea Food and Drug Administration (KFDA). The 10 action plans for improving the health of children include lowering the amount of sugars, sodium, and trans-fatty acids in children’s favorite foods (33). Our results indicate that sodium substitutes in salt, soy sauce, and soybean paste represent a critical component of any such effort.
Clearly there are important limitations in utilizing 24-hour recall data to measure sodium and potassium intake. Twenty-four hour urine collection is the gold standard; however this is impractical to use it in field surveys or clinical settings. Previous studies indicate a correlation between sodium excretion measured by 24-hour urine and sodium intake. Kim et al. (34) reported that urinary sodium excretion was 180 ±73.9 mmol/day (4.1 g/day), which was about 90.5% for Korean adults. In other studies, Park et al. (35) reported that 24-h sodium and potassium excretion values for Korean hypertensive adults were 150±40 mEq/day (3.5 g/day) and 49±10 mEq (1.9 g/day), respectively. These results were similar to the result of this study which reported 4.6–4.7 g/day of sodium intake and 2.6–2.8 g/day of potassium intake considering a urinary excretion rate between 1998 and 2009 in Korea. No South Korean studies have measured potassium intake with twenty-four hour urinary excretion methods. However studies to estimate the relationship between sodium and potassium intake and urinary excretion in this population are necessary.
The South Korean food supply is changing rapidly, and hypertension and CVDs are still major health burdens among adults. This study points out that individual use of sodium at the home preparation level is the critical issue. Nevertheless, it is unlikely that such high levels of sodium can be removed from the South Korean diet. In addition, education to encourage reduced use of sodium in preparation of kimchi, reduced added salt during other food preparation, and reduced consumption of soy sauce and soybean paste is necessary. Finally, a focus on sodium reduction in processed foods, possibly through potassium as a sodium replacement, should be considered.
Supplementary Material
ACKNOWLEDGMENTS
We thank Frances Dancy, BS, UNC Carolina Population Center, for her helpful administrative assistance; Donna R. Miles, PhD, for programming and technical support; and Tom Swasey for graphic support.
Footnotes
CONFLICT OF INTEREST None of the authors report any conflict of interest. Online supporting material is associated with this manuscript.
Supplementary information is available at JHH’s website
REFRENCES
- 1.Eastern Stroke and Coronary Heart Disease Collaborative Research Group Blood pressure, cholesterol, and stroke in eastern Asia. Lancet. 1998;352(9143):1801–7. [PubMed] [Google Scholar]
- 2.World Health Organization [cited 2012 March 1];Fact sheet, the top ten causes of death (updated June 2011) 2008 Available from: http://www.who.int/mediacentre/factsheets/fs310/en/index.html.
- 3.Jung K-W, Park S, Kong H-J, Won Y-J, Boo Y-K, Shin H-R, et al. Cancer Statistics in Korea: Incidence, Mortality and Survival in 2006-2007. J Korean Med Sci. 2010;25:1113–1121. doi: 10.3346/jkms.2010.25.8.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korea S. Causes of death 2010 in Korea. 2011.
- 5.WCRF/AICR . Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. World Cancer Research Fund/American Institute for Cancer Research; Washington, DC: 2007. [Google Scholar]
- 6.Nan HM, Park JW, Song YJ, Yun HY, Park JS, Hyun T, et al. Kimchi and soybean pastes are risk factors of gastric cancer. World J Gastroenterology. 2005;11:3175–3181. doi: 10.3748/wjg.v11.i21.3175. Epub 2005/06/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee J-K, Park B-J, Yoo K-Y, Ahn Y-O. Dietary factors and stomach cancer: A case-control study in Korea. Int J Epidemiol. 1995;24:33–41. doi: 10.1093/ije/24.1.33. [DOI] [PubMed] [Google Scholar]
- 8.He FJ, MacGregor GA. Beneficial effects of potassium. Br Med J. 2001;323:497–501. doi: 10.1136/bmj.323.7311.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korea Centers for Disease Control and Prevention Korea Health Statistics 2009: Korea National Health and Nutrition Examination Survey (KNHANESIV-3) 2010.
- 10.World Health Organization . Review and updating of current WHO recommendations on salt/sodium and potassium consumption. World Health Organization; Geneva, Switzerland: 2011. [Google Scholar]
- 11.Ministry of Health and Welfare. Korea Institute for Health and Social Affairs Korea National health and nutrition survey 1998, 2001, 2005, 2007-2009 (in Korean) 1999.
- 12.Ministry of Health and Welfare. the Korean Centers for Disease Control and Prevention. the Korea Health Industry Development Institute Guideline for Nutrition Survey of the Korea National Health and Nutrition Examination Survey 1998-2009.
- 13.National Rural Living Science Institute the Food composition Table in Kroea in 1996, 2001, 2006: National Rural Living Science Institute 1996, 2001, 2006.
- 14.Ministry of Health and Welfare. Korea Health Industry Development Institute Development of Recipe Database for Korea Health and Nutrition Examination (in Korean) 1998.
- 15.Piernas C, Popkin BM. Snacking increased among U.S. adults between 1977 and 2006. J Nutr. 2010;140:325–332. doi: 10.3945/jn.109.112763. Epub 2009/12/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, et al. Sodium and potassium intake and mortality among US adults: Prospective Data From the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011;171:1183–1191. doi: 10.1001/archinternmed.2011.257. [DOI] [PubMed] [Google Scholar]
- 17.Teramoto T, Kawamori R, Miyazaki S, Teramukai S, Omega Study Group et al. Sodium intake in men and potassium intake in women determine the prevalence of metabolic syndrome in Japanese hypertensive patients: OMEGA Study. Hypertens Res. 2011;34:957–962. doi: 10.1038/hr.2011.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geleijnse JM, Witteman JC, Stijnen T, Kloos MW, Hofman Aa, Grobbee DE. Sodium and potassium intake and risk of cardiovascular events and all-cause mortality: the Rotterdam Study. Eur J Epidemiol. 2007;22:763–770. doi: 10.1007/s10654-007-9186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stamler J, Elliott P, Dennis B, Dyer AR, Kesteloot H, Liu K, et al. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary) J Hum Hypertens. 2003;17:591–608. doi: 10.1038/sj.jhh.1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Food Survey Research Group . Sodium Intake of the U.S. Population. What We Eat In America, NHANES 2007-2008. Food Surveys Research Group; 2011. [Google Scholar]
- 21.Department of Health Assessment of dietary sodium in adults (aged 19 to 64 years) in England, 2011. 2011.
- 22.Liang W, Lee AH, Binns CW. Dietary intake of minerals and the risk of ischemic stroke in guangdong province, china, 2007-2008. Prev Chronic Dis. 2011;8:A38. [PMC free article] [PubMed] [Google Scholar]
- 23.Crispim SP, de Vries JH, Geelen A, Souverein OW, Hulshof PJ, Lafay L, et al. Two non-consecutive 24 h recalls using EPIC-Soft software are sufficiently valid for comparing protein and potassium intake between five European centres--results from the European Food Consumption Validation (EFCOVAL) study. CORD Conference Proceedings; 2011. pp. 447–458. [DOI] [PubMed] [Google Scholar]
- 24.van Mierlo LA, Greyling A, Zock PL, Kok FJ, Geleijnse JM. Suboptimal potassium intake and potential impact on population blood pressure. Arch Intern Med. 2010;170:1501–1502. doi: 10.1001/archinternmed.2010.284. Epub 2010/09/15. [DOI] [PubMed] [Google Scholar]
- 25.Institute of Medicine . In: Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Medicine Io, editor. The National Academies Press; Washington DC: 2005. [Google Scholar]
- 26.WHO/FAO . Diet, nutrition, and the prevention of chronic diseases.Report of a Joint WHO/FAO Expert Consultation. WHO; Geneva, Switzerland: 2003. (WHO Technical Report Series 916). [Google Scholar]
- 27.Appel LJ, Anderson CA. Compelling evidence for public health action to reduce salt intake. N Engl J Med. 2010;362:650–652. doi: 10.1056/NEJMe0910352. Epub 2010/01/22. [DOI] [PubMed] [Google Scholar]
- 28.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10:383–393. doi: 10.1080/07315724.1991.10718167. Epub 1991/08/01. [DOI] [PubMed] [Google Scholar]
- 29.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 30.Cappuccio FP, Capewell S, Lincoln P, McPherson K. Policy options to reduce population salt intake. Br Med J. 2011;343:d4995. doi: 10.1136/bmj.d4995. Epub 2011/08/11. [DOI] [PubMed] [Google Scholar]
- 31.Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29:1043–1050. doi: 10.1097/HJH.0b013e328345ed83. [DOI] [PubMed] [Google Scholar]
- 32.WHO . Creating an enabling environment for population-based salt reduction strategies. WHO; 2010. [Google Scholar]
- 33.Park HK. Nutrition policy in South Korea. Asia Pac J Clin Nutr. 2008;17:343–345. [PubMed] [Google Scholar]
- 34.Kim HJ, Paik HY, Lee SY, Shim JE, Kim YS. Salt usage behaviors are related to urinary sodium excretion in normotensive Korean adults. Asia Pac J Clin Nutr. 2007;16:122–128. [PubMed] [Google Scholar]
- 35.Park S, Park JB, Lakatta EG. Association of central hemodynamics with estimated 24-h urinary sodium in patients with hypertension. CORD Conference Proceedings; 2011. pp. 1502–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.