Abstract
Increasingly, emphasis is being placed on measurement-based care to improve the quality of treatment. Although much of the focus has been on depression, measurement-based care may be particularly applicable to social anxiety disorder (SAD) given its high prevalence, high comorbidity with other disorders, and association with significant functional impairment. Many self-report scales for SAD currently exist, but these scales possess limitations related to length and/or accessibility that may serve as barriers to their use in monitoring outcome in routine clinical practice. Therefore, the aim of the current study was to develop and validate the Clinically Useful Social Anxiety Disorder Outcome Scale (CUSADOS), a self-report measure of SAD. The CUSADOS was designed to be reliable, valid, sensitive to change, brief, easy to score, and easily accessible, to facilitate its use in routine clinical settings. The psychometric properties of the CUSADOS were examined in 2,415 psychiatric outpatients who were presenting for treatment and had completed a semi-structured diagnostic interview. The CUSADOS demonstrated excellent internal consistency, and high item-total correlations and test-retest reliability. Within a sub-sample of 381 patients, the CUSADOS possessed good discriminant and convergent validity as it was more highly correlated with other measures of SAD than with other psychiatric disorders. Furthermore, scores were higher in outpatients with a current diagnosis of SAD compared to those without a SAD diagnosis. Preliminary support also was obtained for the sensitivity to change of the CUSADOS in a sample of 15 outpatients receiving treatment for comorbid SAD and depression. Results from this validation study in a large psychiatric sample show that the CUSADOS possesses good psychometric properties. Its brevity and ease of scoring also suggest that it is feasible to incorporate into routine clinical practice.
Surveys of psychiatrists in clinical practice in the United Kingdom and United States have found that the majority do not use symptom rating scales of depression or anxiety to monitor progress throughout treatment [1, 2]. When outcomes are assessed, they typically are based on unstructured interactions rather than quantifiable assessments [3,4]. Although routine outcome assessment currently is not widely practiced, there is movement towards payor mandates to increase this behavior. For example, a law signed in 2006 (the Centers for Medicare and Medicaid Services’ Physician Quality Reporting Initiative; [5]) provides financial incentives to physicians to document outcomes reflecting best practices, in an effort to improve the quality of care. In addition, DSM-5 work groups are recommending the use of dimensional severity scales for various disorders [e.g., for social anxiety disorder; 6].
Conducting reliable, valid, and informative outcome assessments on a routine basis can help to optimize delivery of care [3]. This is especially important for individuals with social anxiety disorder (SAD), as it is a chronic and significantly disabling disorder [7,8]. SAD often is under-recognized in clinical settings, especially when other disorders such as depression are present [9,10]. Therefore, it often is under-treated [11–13] and tends to have the lowest proportion of met need for treatment compared to other psychiatric disorders [14]. Under-treated SAD may affect the treatment outcome of other conditions such as depression, both in pharmacologic and cognitive-behavioral treatments [15–18]. Therefore, routine monitoring of SAD symptoms over the course of treatment can aid in ensuring adequate and efficient treatment that perhaps could impact the treatment of comorbid disorders.
One of the long-term aims of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project has been to develop a series of reliable, valid, and brief instruments for use in routine practice settings. In addition to being available to clinicians for personal use without cost, each measure is designed to have the same rating instructions to facilitate comparison across symptom domains. Most recently, measures of depression (the Clinically Useful Depression Outcome Scale, or CUDOS; [19]) and the general construct of anxiety (the Clinically Useful Anxiety Outcome Scale, or CUXOS; [3]) were validated. These measures are brief (so as to reduce respondent burden and allow for easy scoring), and they provide useful clinical information to monitor progress throughout treatment.
The goal of the current report from the MIDAS Project is to validate a similar self-report measure specific to SAD, called the Clinically Useful Social Anxiety Disorder Outcome Scale (CUSADOS). As with its predecessors, the CUSADOS was designed to be clinically useful, reliable, valid, brief, quickly scored, and sensitive to change. It is acknowledged that many measures of SAD currently exist. However, some of these measures are lengthy and thus burdensome to complete (e.g., the Social Phobia and Anxiety Inventory (SPAI), administered in 20 to 30 minutes; [20]). Some measure only certain aspects of SAD, such as fear and avoidance in specific situations as in the Liebowitz Social Anxiety Scale (LSAS; [21]), or cognitions, as in the Social Interaction Self-Statement Test [22]. Others are in a true/false format rather than a Likert scale (e.g., Fear of Negative Evaluation Scale; [23]), and this is less useful as an outcome measure. Some are not readily available to clinicians and need to be purchased (e.g., the Social Phobia and Anxiety Inventory [20]), and some have reverse scoring that lengthen the amount of time required for scoring (e.g., the Fear of Negative Evaluation Scale [23]). Two other brief measures of SAD exist, with the intended purpose of screening for a SAD diagnosis: the Brief Social Phobia Scale (BSPS; [24]), and the Mini-Social Phobia Inventory (MINI-SPIN; [25]). However, the BSPS is an observer-rated measure consisting of three subscales, that the authors recommend using after completing a semi-structured diagnostic interview. It assesses fear and avoidance of a limited number of situations as well as a small number of physiological symptoms, but it does not assess cognitions commonly associated with SAD. Although it is brief, the fact that it is an observer-rated measure suggests that it may increase clinician burden relative to self-report scales. The MINI-SPIN is a self-report measure modeled after the BSPS, but it contains only three items. Therefore, the MINI-SPIN may not provide a large enough range of scores that would be sensitive to change, thus limiting its use as a symptom severity measure. In addition to their limited use as outcome measures, the brevity of these measures also may limit their utility as case-finding instruments.
In contrast to the above measures, the CUSADOS is brief, yet has enough items to provide a broad range of scores. It also has straightforward scoring (sum of all items), and includes Likert scale ratings rather than true/false statements. In addition, it assesses a combination of different aspects of SAD, including affective (e.g., “I was extremely afraid of social situations”), cognitive (e.g., “I was worried that I would make a mistake in front of others and look foolish”), situational (“I was afraid of eating, drinking, or writing in front of other people”), and behavioral (e.g., “I avoided social situations where people might pay attention to me”). The aim of the present study was to examine the psychometric properties of the CUSADOS in a sample of psychiatric outpatients, as well as its operating characteristics to examine its potential use as a screening or case-finding instrument in addition to a symptom severity measure.
Methods
Participants
The sample included 2,415 psychiatric outpatients presenting for treatment at the Outpatient Psychiatry Practice of Rhode Island Hospital. The practice treats individuals with medical insurance on a fee-for-service basis (including Medicare but not Medicaid), and is different from the hospital’s residency training outpatient clinic that treats uninsured and medical assistance individuals. Referral sources were coded for a subset of the sample (the last 1,600). The three most common referral sources were primary care physicians (n = 379; 31.6%), family members or friends (n = 210; 17.5%), and therapists in the community (n = 190; 15.8%).
Procedure
Individuals seeking treatment at the outpatient practice were asked to participate in a comprehensive diagnostic evaluation prior to meeting with their treating clinician, and to complete the CUSADOS as part of their initial paperwork. All procedures were approved by the Institutional Review Board at Rhode Island Hospital. A modified version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; [26]) was used for the diagnostic evaluation. All patients were interviewed with the full SCID, and informed consent was obtained prior to administering the SCID. The diagnosticians were kept blind to the patients’ responses on the CUSADOS to test the validity of the measure by examining its relationship with psychiatric diagnoses. Doctoral-level clinical psychologists and research assistants with bachelor’s degrees in social or biological sciences served as diagnosticians. They received extensive training, and monitoring occurred throughout the study to minimize rater drift. Psychologists first observed five interviews, then were observed while administering 15–20 interviews, and finally were required to demonstrate exact or near exact agreement with a senior diagnostician on five consecutive interviews. Research assistants were required to observe 20 interviews before administering over 20 interviews while being observed, and then demonstrated agreement with a senior diagnostician on five consecutive interviews. During the course of training, every interview was reviewed on an item-by-item basis with the senior diagnostician who observed the interview.
Ongoing supervision of diagnosticians included a weekly diagnostic case conference with all members of the team and a review of item ratings for every case by M.Z. Inter-rater reliability was assessed for 65 cases, using the joint interview method. Results indicated good inter-rater agreement, particularly for major depressive disorder (MDD) and the anxiety disorders (MDD κ = 0.90; panic disorder κ = 0.95; SAD κ = 0.84; obsessive-compulsive disorder κ = 1.0; specific phobia κ = 0.93; generalized anxiety disorder κ = 0.85; posttraumatic stress disorder κ = 0.87).
Measures
The initial version of the CUSADOS included 18 items assessing symptoms of social anxiety in the past week related to affect (“I was extremely afraid of social situations”), cognitions (“I was worried that I would make a mistake in front of others and look foolish”), situations (“I was afraid of eating, drinking, or writing in front of other people”) and behavior (“I avoided social situations where people might pay attention to me”). Content for the CUSADOS was derived from the Psychiatric Diagnostic Screening Questionnaire [27]) and diagnostic interviews such as the SCID [26]. The initial pool of items was created, and reviewed by clinicians experienced in the treatment of anxiety and mood disorders; the pool of items then was revised accordingly. Respondents were instructed to rate each item on a 5-point Likert scale indicating “how well the item describes you during the past week, including today” (0 = not at all true; 1 = rarely true; 2 = sometimes true; 3 = often true; 4 = almost always true). A one-week time frame was used, to allow for use of the scale for weekly assessments. Items are summed to derive a total score.
Global Assessment of Functioning (GAF) ratings were made by the diagnosticians during the SCID; prior reports from the MIDAS Project have indicated good inter-rater agreement on GAF ratings [28]. Participants were asked to complete a booklet of the following questionnaires at home in order to examine the convergent and discriminant validity of the CUSADOS: Eating Disorder Inventory – anorexia, bulimia, and body dissatisfaction subscales [29]; Beck Depression Inventory [30]; Brief Fear of Negative Evaluation Scale [31]; Fear Questionnaire-Social Phobia and Agoraphobia subscales [32]; Social Phobia and Anxiety Inventory-Agoraphobia subscale [20]; Posttraumatic Stress Disorder Scale [33]; Obsessive-Compulsive Inventory [34]; Penn State Worry Questionnaire [35]; Beck Anxiety Inventory [36]; Anxiety Control Questionnaire [37]; Michigan Alcohol Screening Test [38]; Drug Abuse Screening Test [39]; Whitely Index [40]; Self-Report Manic Inventory [41]; Symptom Rating Test – paranoia and psychosis subscales [42]; and Somatic Symptom Index [43,44]. All of these scales are widely used, and have demonstrated good psychometric properties.
To examine test-retest reliability, 204 patients who completed the CUSADOS at the first appointment were given a second copy of the measure at the conclusion of the intake evaluation with a pre-addressed, postage-paid envelope in which to return the measure. Patients were instructed that the purpose of this second administration was to test the performance of the scale and not to question the truthfulness or accuracy of their responses. The second administration was completed an average of 4.1 days (SD = 5.7) after the initial evaluation. Preliminary analyses on sensitivity to change were conducted by examining the performance of the CUSADOS in 15 outpatients who received 16 sessions of acceptance-based behavior therapy adjunctive to medication for comorbid depression and SAD, as part of an ongoing trial.
Statistical Analyses
To reduce item redundancy, an inter-correlation matrix was generated to identify highly correlated items that could be eliminated from the scale. Next, internal consistency was calculated using Cronbach’s alpha, and item-total correlations were computed. Test-retest reliability was examined using Pearson correlations, and Pearson correlations also were calculated to examine convergent and discriminant validity between the CUSADOS and the other measures listed above. An independent samples t test was used to determine whether patients with current SAD scored significantly higher on the CUSADOS compared to patients without a current SAD diagnosis. The operating characteristics of the CUSADOS were further examined by calculating sensitivity (the ability to correctly identify individuals with the disorder), specificity (the ability to identify individuals without the disorder), positive predictive value (PPV; the percentage of individuals identified as having the disorder by the measure and who truly have the disorder based on a “gold standard,” in this case the SCID), and negative predictive value (NPV; the percentage of individuals classified as not having the disorder by the measure who truly do not have the disorder based on a “gold standard”). Diagnostic performance was examined across a range of cutoff scores using receiver operating curve (ROC) analyses [45]. The ROC curve is a plot of the measure’s sensitivity versus one minus specificity at each cutoff score. The area under the curve (AUC) is the evaluative measure that is obtained, which ranges from 0.5 (random performance) to 1.0 (perfect performance). Finally, a paired samples t test was conducted to examine preliminary sensitivity to change of the CUSADOS in outpatients with comorbid depression and SAD who were treated with 16 sessions of acceptance-based behavior therapy adjunctive to medication.
Results
Demographic Characteristics
Participants ranged in age from 18 to 85 years old (M = 39.0, SD = 13.4), and the majority were female, Caucasian, and either married or never married (see Table 1). Over half of the patients had a high school degree or equivalency, and nearly one third received a 2- or 4-year college degree (Table 1). As shown in Table 2, more than one quarter (26.5%; n = 640) of the 2,415 patients completing the CUSADOS met current criteria for SAD. Other than SAD, the most frequent current Axis I diagnoses were MDD, generalized anxiety disorder, panic disorder with or without agoraphobia, posttraumatic stress disorder, and specific phobia.
Table 1.
Demographic Characteristics of 2,415 Psychiatric Outpatients
| Demographic Characteristic | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Female | 1430 | 59.2 |
| Male | 985 | 40.8 |
| Marital Status | ||
| Married | 1001 | 41.4 |
| Living as if married | 147 | 6.1 |
| Widowed | 45 | 1.9 |
| Separated | 117 | 4.8 |
| Divorced | 341 | 14.1 |
| Never Married | 764 | 31.6 |
| Education | ||
| Less than high school | 176 | 7.3 |
| Graduated from high school | 1490 | 61.7 |
| College degree | 749 | 31.0 |
| Race | ||
| Caucasian | 2197 | 91.0 |
| Black | 105 | 4.3 |
| Hispanic | 64 | 2.7 |
| Asian | 24 | 1.0 |
| Other | 25 | 1.0 |
Table 2.
Current DSM-IV Axis I Diagnoses of 2,415 Psychiatric Outpatients
| DSM-IV Diagnosis | Frequency | Percentage |
|---|---|---|
| Major depressive disorder | 1005 | 41.6 |
| Bipolar disorders | 122 | 5.1 |
| Dysthymic disorder | 198 | 8.2 |
| Generalized anxiety disorder | 489 | 20.2 |
| Panic disorder | 401 | 16.6 |
| Social anxiety disorder | 640 | 26.5 |
| Specific phobia | 259 | 10.7 |
| Obsessive-compulsive disorder | 159 | 6.6 |
| Posttraumatic stress disorder | 267 | 11.1 |
| Adjustment disorder | 163 | 6.7 |
| Schizophrenia | 7 | 0.3 |
| Eating disorder | 159 | 6.6 |
| Alcohol abuse/dependence | 205 | 8.5 |
| Drug abuse/dependence | 127 | 5.3 |
| Somatoform disorder | 181 | 7.5 |
| Attention deficit disorder | 195 | 8.1 |
| Impulse control disorder | 143 | 5.9 |
Note. Individuals could be given more than one diagnosis.
Item Redundancy
An inter-item correlation matrix first was generated using the original 18 items of the scale. When two items similar in content were correlated at greater than 0.75, only one item in that pair was retained to reduce redundancy of items. The determination of which item to retain in the pair was based on the item-total correlations and test-retest reliability for each item. Using this method, the following 6 items were eliminated: “I was very afraid of embarrassing myself in front of others” (correlated 0.81 with the retained item “I was worried that I would make a mistake in front of others and look foolish”); “I was terrified that others may think badly of me” (correlated 0.83 with the retained item “I was very afraid of being judged by others”); “I avoided social situations that made me very nervous” (correlated 0.84 with the retained item “I avoided social situations where people might pay attention to me”); “I felt nervous in situations where people paid attention to me” (correlated 0.84 with the retained item “I avoided social situations where people might pay attention to me”); “I felt very anxious or nervous when entering social gatherings” (correlated 0.79 with the retained item “I was afraid to walk into a crowded room because everyone would look at me”); and “I was worried about being rejected by other people” (correlated 0.89 with the retained item “I was worried that other people may not like me”). This resulted in a 12-item measure, the items of which are presented in Table 3. The remaining psychometric analyses are based on this 12-item version.
Table 3.
Item-Total Correlations and Test-Retest Reliability of Individual CUSADOS Items
| CUSADOS Item | Item-Total Correlations |
Test-Retest Reliability |
|---|---|---|
| I was very afraid of being judged by others | 0.74 | 0.77 |
| I was extremely afraid of social situations | 0.80 | 0.79 |
| I was worried that I would make a mistake in front of others and look foolish | 0.84 | 0.82 |
| I avoided social situations where people might pay attention to me | 0.80 | 0.75 |
| I was afraid to walk into a crowded room because everyone would look at me | 0.80 | 0.75 |
| I was afraid of eating, drinking, or writing in front of other people | 0.69 | 0.73 |
| I was very concerned that people would notice that I was anxious | 0.75 | 0.73 |
| I avoided eating, drinking, or writing in front of people | 0.67 | 0.76 |
| I worried that I would say something stupid in front of other people | 0.84 | 0.79 |
| I was worried about being criticized by other people | 0.84 | 0.79 |
| I was worried that other people may not like me | 0.80 | 0.80 |
| After I was criticized, I thought about it for a long time | 0.73 | 0.77 |
Note. All correlations are significant at p < 0.001. CUSADOS = Clinically Useful Social Anxiety Disorder Outcome Scale.
Reliability
The mean total score on the CUSADOS across all participants was 13.4 (SD=13.1). Internal consistency was excellent (Cronbach’s α = 0.96), and all item-scale correlations were statistically significant (ranging from 0.67–0.84, median r = 0.80; all ps < 0.001). Test-retest reliability of the overall measure (r = 0.89) and each item also were statistically significant (ranging from 0.73–0.82, median r = 0.77; all ps < 0.001; see Table 3).
Validity
A total of 381 patients completed a packet of questionnaires at home an average of 1.2 days (SD = 16.9) following the initial intake evaluation. As shown in Table 4, the CUSADOS was significantly correlated with all of the other measures, with the highest correlations being with other measures of social anxiety (median r = 0.67) compared to measures of other symptom domains (median r = 0.39). As would be expected given the common comorbidity between SAD and mood and other anxiety disorders, the CUSADOS also was moderately and significantly correlated with the measures assessing depression and anxiety. Furthermore, the CUSADOS was negatively correlated with GAF scores (r = −0.35, p < 0.001), such that higher CUSADOS scores were associated with poorer functioning.
Table 4.
Discriminant and Convergent Validity of the Clinically Useful Social Anxiety Disorder Outcome Scale (CUSADOS)
| Scale | Correlation with CUSADOS (r) |
|---|---|
| Fear Questionnaire – social phobia subscale | 0.68 |
| Brief Fear of Negative Evaluation Scale | 0.65 |
| Symptom Rating Test – paranoia subscale | 0.61 |
| Social Phobia and Anxiety Inventory – agoraphobia subscale | 0.59 |
| Anxiety Control Questionnaire | 0.57 |
| Beck Depression Inventory | 0.56 |
| Obsessive Compulsive Inventory | 0.53 |
| Anxiety Sensitivity Index | 0.51 |
| Fear Questionnaire – agoraphobia subscale | 0.48 |
| Beck Anxiety Inventory | 0.47 |
| Penn State Worry Questionnaire | 0.46 |
| Somatic Symptom Index | 0.41 |
| State-Trait Anger Expression Inventory – Trait subscale | 0.39 |
| Self-Report Manic Inventory | 0.38 |
| Posttraumatic Stress Disorder Scale | 0.37 |
| State-Trait Anger Expression Inventory – State subscale | 0.36 |
| Eating Disorder Inventory – bulimia subscale | 0.34 |
| Whitely Index | 0.29 |
| Eating Disorder Inventory – anorexia subscale | 0.28 |
| Eating Disorder Inventory – body dissatisfaction subscale | 0.24 |
| Symptom Rating Test – psychosis subscale | 0.21 |
| Michigan Alcohol Screening Test | 0.17 |
| Drug Abuse Screening Test | 0.17 |
Note. All correlations are significant at p < 0.001. Due to missing data, sample sizes range from 270 to 381.
Association with SAD Diagnosis
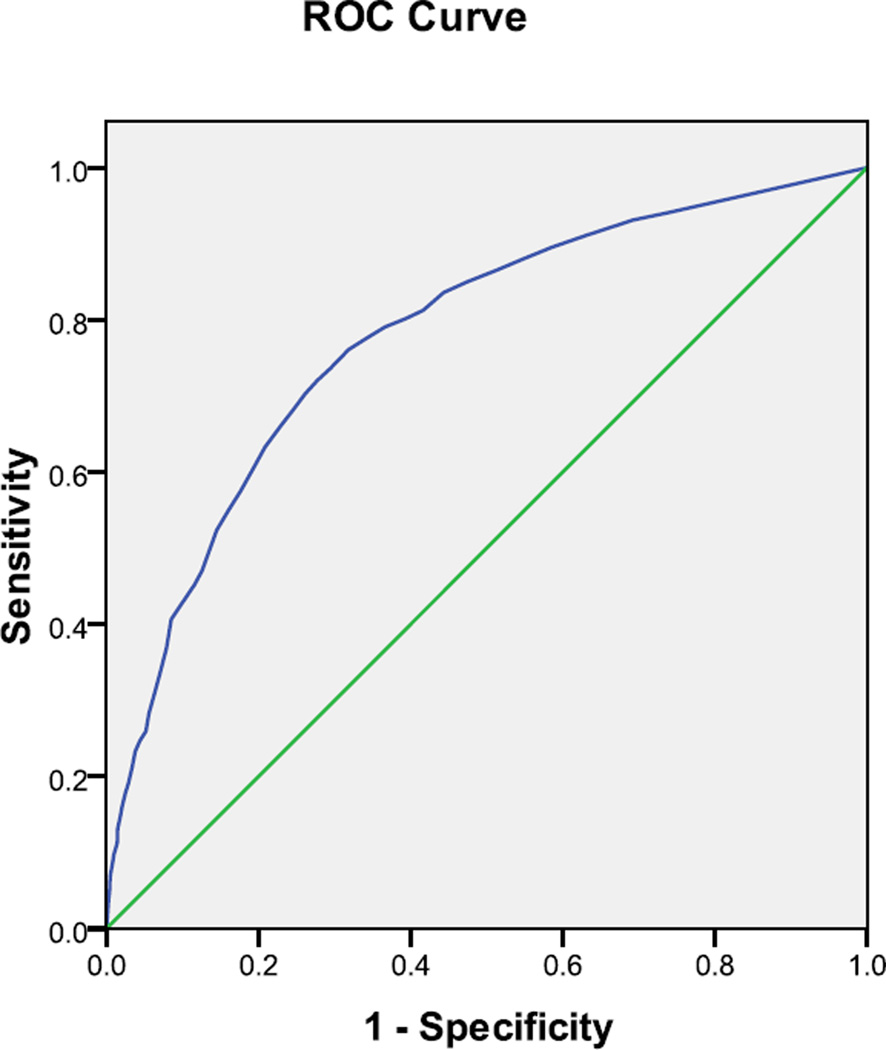
From the sample of 2,415 outpatients with available CUSADOS data, 640 (26.5%) met current criteria for SAD. Patients with SAD scored significantly higher than the patients without SAD (23.27 ± 13.67 versus 9.81 ± 10.94, respectively; t = −22.5, p < 0.001). Although the primary purpose of the CUSADOS is to serve as a symptom severity measure, analyses were conducted on the operating characteristics to suggest cut-offs for its use as a screening measure or as a potential case-finding measure, depending on the intended purpose by the user. Figure 1 shows the ROC curve comparing the diagnostic performance of the CUSADOS to the results from the SCID interview across cutoff scores. The AUC (0.78) was significant (p < 0.001). Results from this analysis indicated that cutoff scores ranging from 13–16 provided the maximum sum of sensitivity and specificity (Table 5). A cutoff score of 16 performed best in terms of operating characteristics, with a diagnostic efficiency of 73%. When examining the performance of the CUSADOS as a screening instrument, it is most important to have high sensitivity at the expense of lower specificity [46]. This may result in a greater likelihood of false positives, but from a screening perspective it is best to have higher sensitivity to alert one to the possible presence of the disorder which then would prompt additional assessment. For such a purpose, a cut-off of 4 produces a sensitivity of 89.5% with a specificity of 41.5%.
Figure 1.
Receiver Operating Curve for the CUSADOS in Detecting Social Anxiety Disorder in 2,415 Psychiatric Outpatients
Table 5.
Operating Characteristics of Various Cut-offs on the Clinically Useful Social Anxiety Disorder Outcome Scale (CUSADOS)
| Cut-off Value | Sensitivity | Specificity | PPV | NPV | Efficiency |
|---|---|---|---|---|---|
| 13 | 0.76 | 0.68 | 0.46 | 0.89 | 0.70 |
| 14 | 0.74 | 0.71 | 0.47 | 0.88 | 0.71 |
| 15 | 0.72 | 0.72 | 0.48 | 0.88 | 0.72 |
| 16 | 0.70 | 0.74 | 0.49 | 0.87 | 0.73 |
Note. PPV = positive predictive value; NPV = negative predictive value; Efficiency = diagnostic efficiency.
Sensitivity to Change
Preliminary sensitivity to change was examined by comparing pre- and post-treatment scores on the CUSADOS in 15 outpatients receiving acceptance-based behavior therapy adjunctive to medication for comorbid depression and SAD. Results from the paired samples t test showed that scores on the CUSADOS significantly decreased from pre- to post-treatment (20.43 ± 8.88 versus 11.36 ± 8.95, respectively; paired t = 3.46; p = 0.004).
Discussion
Results from this validation study of the CUSADOS show that it is a reliable and valid measure of SAD symptoms. The CUSADOS demonstrated excellent internal consistency, and test-retest reliability was high. The measure was most highly correlated with other measures of social anxiety, suggesting that it validly measures this construct. As would be expected it also correlated moderately with measures of depression and other anxiety disorders, and demonstrated low correlations with measures of other disorders such as eating and somatoform disorders. This suggests that the CUSADOS also possesses good discriminant validity. Furthermore, scores significantly differed between individuals with and without SAD, its operating characteristics were adequate, and it showed preliminary sensitivity to change following a course of acceptance-based behavior therapy.
Although many scales for SAD currently exist, they possess certain limitations. These limitations include assessment of only specific aspects of SAD and/or use of ratings with limited range (e.g., true/false rather than Likert scale ratings). Furthermore, several existing scales are lengthy which may pose a burden on those completing as well as scoring the scale, and some are costly to obtain or not widely available. These limitations in particular may be important factors that serve as barriers to routine assessment of SAD in real-world clinical practice. From the perspective of those receiving care, a study of outpatients being treated for depression indicated a preference for briefer measures to monitor their progress [47]. However, no known prior research has been conducted on patient preferences in the assessment of SAD, and this represents an area of future study. Nonetheless, the CUSADOS shows promise for its use in clinical settings, given its brevity (12 items) and easy scoring (sum of all items) in addition to its good psychometric properties.
Recent years have seen an increase in the emphasis on measurement-based care, or the use of standardized scales to assess progress in treatment [48]. Thus far the majority of the focus has been placed on the treatment of depression [49,50], and this movement has not been without its challenges. Harding et al. [50] have posited that facilitating the adoption of measurement-based care in clinical practice requires addressing challenges such as “a lack of standard and available measures and outcomes,” and “limited provider training in the use and helpfulness of measures and continuous quality improvement” (p. 1138). In addition, Bremer et al. [51] noted that a lack of well-accepted measures for disorders other than depression has represented a significant barrier to implementing strategies such as measurement-based care, compared to other fields in medicine.
The implementation of measurement-based care can be of particular importance to SAD. For instance, SAD is the fourth most common mental health disorder in the United States [52], and is the most common comorbid anxiety disorder in depressed outpatients [53]. Yet, it often is under-recognized particularly in depressed outpatients [9] and therefore is under-treated [11,14]. Many individuals with SAD may be hesitant to discuss their symptoms with their doctor, due to a fear of being embarrassed [54]. However, once SAD is identified, 75% of these individuals desire treatment for SAD once directly asked [55]. Therefore, assessment of SAD via a brief self-report questionnaire may help to identify some of these symptoms that may not be asked by practitioners or discussed by patients, which could then prompt further assessment.
It is of great importance to adequately treat SAD, given that it results in significant functional impairment and healthcare utilization [8,10,56], and remains chronic and unremitting without treatment [7]. There also is growing evidence to indicate that the presence of SAD may be detrimental to the treatment of other disorders, such as depression. For example, a multicenter study by Souery et al. [18] found that the presence of comorbid SAD and panic disorder were associated with treatment-resistant depression. Furthermore, comorbid SAD has been found to be significantly associated with an overall risk of depressive recurrence (94% with versus 68% without comorbid SAD), recurrence over twice as fast compared to those without comorbid SAD (after controlling for other Axis I and II conditions), and a greater number of depressive recurrences relative to other comorbid conditions [16]. Most of these findings have been in the context of pharmacotherapy studies; however, one study comparing cognitive behavior therapy (CBT) to medications for depression found that patients in the CBT condition fared significantly worse if they had comorbid SAD [15]. Therefore, previous research suggests that it is important to identify the presence of SAD and continue monitoring it throughout treatment in order to adjust treatment planning and optimize outcomes. The development of the CUSADOS perhaps represents one such way to facilitate that process.
Limitations of the study include use of a sample that was mostly Caucasian and insured, therefore results may not generalize to other populations with different demographic characteristics. In addition, the sample size for the analyses on sensitivity to change was small, thus making those results preliminary. Future research should replicate the sensitivity to change of the measure in larger samples. The sensitivity to change analyses also utilized a sample receiving treatment for depression in addition to SAD; therefore, future research should examine the treatment sensitivity of the CUSADOS in samples receiving treatment only for SAD.
Although the instruction of rating symptoms over the past week facilitates the use of the CUSADOS as an outcome measure, it may limit its use as a case-finding measure. Results suggested that the operating characteristics of the CUSADOS were adequate; nonetheless, caution should be exercised when using the CUSADOS as a case-finding measure due to the above potential limitation. Finally, the research was conducted within a hospital-based outpatient psychiatry practice, and the validation of the CUSADOS should be replicated in other settings (e.g., primary care practice settings). It is possible that within primary care settings, there would be a higher rate of false positives of SAD based on the CUSADOS. If that were to be the case, perhaps the CUSADOS would be best used as a screening tool rather than case-finding measure within primary care samples. Thus future research should examine the performance of the CUSADOS in primary care practices, to determine its most appropriate use in such settings.
In conclusion, the CUSADOS is a reliable and valid self-report measure of social anxiety symptoms. Given its brevity and ease of scoring, it is believed that it easily can be incorporated into routine clinical practice, without being burdensome on clinicians, patients, or support staff. Future research efforts will be undertaken to investigate the electronic administration of the CUSADOS, with the hope of further facilitating its use in real-world practice settings.
Acknowledgments
This study was supported by grant number R44MH057603 from the National Institute of Mental Health (awarded to Dr. Young), and in part by grant number K23MH085730 from the National Institute of Mental Health (awarded to Dr. Dalrymple).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gilbody SM, House AO, Sheldon TA. Psychiatrists in the UK do not use outcomes measures: national survey. Br J Psychiatry. 2002;180:101–103. doi: 10.1192/bjp.180.2.101. [DOI] [PubMed] [Google Scholar]
- 2.Zimmerman M, McGlinchey JB. Why don’t psychiatrists use scales to measure outcome when treating depressed patients? J Clin Psychiatry. 2008;69:1916–1919. doi: 10.4088/jcp.v69n1209. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman M, Chelminski I, Young D, Dalrymple K. A clinically useful anxiety outcome scale. J Clin Psychiatry. 2010;71:534–542. doi: 10.4088/JCP.09m05264blu. [DOI] [PubMed] [Google Scholar]
- 4.Zimmerman M, Chelminski I, Young D, Dalrymple K. Using outcome measures to promote better outcomes. Clin Neuropsychiatry J Treat Eval. 2011;8:28–36. [Google Scholar]
- 5.U.S. Department of Health and Human Services. Physician quality reporting initiative. Center for Medicare and Medicaid Services. 2008:110–275. [Google Scholar]
- 6.Bögels SM, Alden L, Beidel DC, Clark LA, Pine DS, Stein MB, et al. Social anxiety disorder: Questions and answers for the DSM-V. Depress Anxiety. 2010;27:168–189. doi: 10.1002/da.20670. [DOI] [PubMed] [Google Scholar]
- 7.Judd LL. Social phobia A clinical overview. J Clin Psychiatry. 1994;55:5–9. [PubMed] [Google Scholar]
- 8.Katzelnick DJ, Kobak KA, DeLeire T, Henk HJ, Greist JH, Davidson JR, et al. Impact of generalized social anxiety disorder in managed care. Am J Psychiatry. 2001;158:1999–2007. doi: 10.1176/appi.ajp.158.12.1999. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman M, Chelminski I. Clinician recognition of anxiety disorders in depressed outpatients. J Psychiatr Res. 2003;37:325–333. doi: 10.1016/s0022-3956(03)00020-7. [DOI] [PubMed] [Google Scholar]
- 10.Weiller E, Bisserbe JC, Boyer P, Lepine JP, Lecrubier Y. Social phobia in general health care: An unrecognized undertreated disabling disorder. Br J Psychiatry. 1996;168:169–174. doi: 10.1192/bjp.168.2.169. [DOI] [PubMed] [Google Scholar]
- 11.Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, et al. The epidemiology of social anxiety disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- 12.Robins LN, Regier DA. Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York, NY: Free Press; 1991. [Google Scholar]
- 13.Wagner R, Silove D, Marnane C, Rouen D. Delays in referral of patients with social phobia, panic disorder, and generalized anxiety disorder attending a specialist anxiety clinic. J Anxiety Disord. 2006;20:363–371. doi: 10.1016/j.janxdis.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Messias E, Eaton W, Nestadt G, Bienvenu OJ, Samuels J. Psychiatrists’ ascertained treatment needs for mental disorders in a population-based sample. Psychiatr Serv. 2007;58:373–377. doi: 10.1176/ps.2007.58.3.373. [DOI] [PubMed] [Google Scholar]
- 15.DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- 16.Holma KM, Holma IA, Melartin TK, Rytsala HJ, Isometsa ET. Long-term outcome of major depressive disorder in psychiatric patients is variable. J Clin Psychiatry. 2008;69:196–205. doi: 10.4088/jcp.v69n0205. [DOI] [PubMed] [Google Scholar]
- 17.Mulder RT, Joyce PR, Frampton CMA, Luty SE, Sullivan PF. Six months of treatment for depression: Outcome and predictors of the course of illness. Am J Psychiatry. 2006;163:195–100. doi: 10.1176/appi.ajp.163.1.95. [DOI] [PubMed] [Google Scholar]
- 18.Souery D, Oswald P, Massat I, Bailer U, Bollen J, Demyttenaere K, et al. Clinical factors associated with treatment resistance in major depressive disorder: results from a European multicenter study. J Clin Psychiatry. 2007;68:1062–1070. doi: 10.4088/jcp.v68n0713. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerman M, Chelminski I, McGlinchey JB, Posternak MA. A clinically useful depression outcome scale. Compr Psychiat. 2008;49:131–140. doi: 10.1016/j.comppsych.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Turner SM, Beidel DC, Dancu CV, Stanley MA. An empirically derived inventory to measure social fears and anxiety: The Social Phobia and Anxiety Inventory. Psychol Assess. 1989;1:35–40. [Google Scholar]
- 21.Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- 22.Glass CR, Merluzzi TV, Biever JL, Larsen KH. Cognitive assessment of social anxiety: Development and validation of a self-statement questionnaire. Cognit Ther Res. 1982;6:37–55. [Google Scholar]
- 23.Watson D, Friend R. Measurement of social-evaluative anxiety. J Consult Clin Psychol. 1969;33:448–457. doi: 10.1037/h0027806. [DOI] [PubMed] [Google Scholar]
- 24.Davidson JRT, Potts NLS, Richichi EA, Ford SM, Krishnan RR, Smith RD, et al. The Brief Social Phobia Scale. J Clin Psychiatry. 1991;52:48–51. doi: 10.1037/t07672-000. [DOI] [PubMed] [Google Scholar]
- 25.Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JRT. MINI-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137–140. doi: 10.1002/da.1055. [DOI] [PubMed] [Google Scholar]
- 26.First MB, Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-IV (SCID) Washington, D.C.: American Psychiatric Association; 1997. [Google Scholar]
- 27.Zimmerman M, Mattia JI. A self-report scale to help make psychiatric diagnoses: The Psychiatric Diagnostic Screening Questionnaire. Arch Gen Psychiatry. 2001;58:787–794. doi: 10.1001/archpsyc.58.8.787. [DOI] [PubMed] [Google Scholar]
- 28.Dalrymple KL, Zimmerman M. Age of onset of social anxiety disorder in depressed outpatients. J Anxiety Disord. 2011;25:131–137. doi: 10.1016/j.janxdis.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2:15–34. [Google Scholar]
- 30.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: The Guilford Press; 1979. [Google Scholar]
- 31.Leary MR. A brief version of the Fear of Negative Evaluation Scale. Pers Soc Psychol Bull. 1983;9:371–375. [Google Scholar]
- 32.Marks IM, Matthews AM. Brief standard self-rating for phobic patients. Behav Res Ther. 1979;17:263–267. doi: 10.1016/0005-7967(79)90041-x. [DOI] [PubMed] [Google Scholar]
- 33.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 34.Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive compulsive disorder scale: The Obsessive-Compulsive Inventory. Psychol Assess. 1998;10:206–214. [Google Scholar]
- 35.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 36.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 37.Rapee RM, Craske MG, Brown TA, Barlow DH. Measurement of perceived control over anxiety-related events. Behav Ther. 1996;27:279–293. [Google Scholar]
- 38.Selzer ML. The Michigan alcoholism screening test: The quest for a new diagnostic instrument. Am J Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- 39.Skinner HA. The drug abuse screening test. Addict Behav. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 40.Pilowsky I. Dimensions of hypochondriasis. Br J Psychiatry. 1967;113:89–93. doi: 10.1192/bjp.113.494.89. [DOI] [PubMed] [Google Scholar]
- 41.Shugar G, Schertzer S, Toner BB, Di Gasbarro I. Development, use, and factor analysis of a self-report inventory for mania. Compr Psychiatr. 1992;33:325–331. doi: 10.1016/0010-440x(92)90040-w. [DOI] [PubMed] [Google Scholar]
- 42.Kellner R. The Symptom-Rating Test. In: Sartorius N, Ban TA, editors. Assessment of Depression. New York, NY: Springer-Verlag; 1985. pp. 213–220. [Google Scholar]
- 43.Othmer E, DeSouza C. A screening test for somatization disorder (hysteria) Am J Psychiatry. 1985;142:1146–1149. doi: 10.1176/ajp.142.10.1146. [DOI] [PubMed] [Google Scholar]
- 44.Swartz M, Hughes D, George L, Blazer D, Landerman R, Bucholz K. Developing a screening index for community studies of somatization disorder. J Psychiatr Res. 1986;20:335–343. doi: 10.1016/0022-3956(86)90036-1. [DOI] [PubMed] [Google Scholar]
- 45.Hsiao JK, Bartko JJ, Potter WZ. Diagnosing diagnoses: Receiver operating characteristic methods and psychiatry. Arch Gen Psychiatry. 1989;46:664–667. doi: 10.1001/archpsyc.1989.01810070090014. [DOI] [PubMed] [Google Scholar]
- 46.Zimmerman M, Posternak MA, Chelminski I, Solomon DA. Using questionnaires to screen for psychiatric disorders: A comment on a study of screening for bipolar disorder in the community. J Clin Psychiatry. 2004;65:605–610. doi: 10.4088/jcp.v65n0503. [DOI] [PubMed] [Google Scholar]
- 47.Zimmerman M, McGlinchey JB. Depressed patients’ acceptability of the use of self-administered scales to measure outcome in clinical practice. Ann Clin Psychiatry. 2008;20:125–129. doi: 10.1080/10401230802177680. [DOI] [PubMed] [Google Scholar]
- 48.Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: Implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 49.Chang TE, Jing Y, Yeung AS, Brenneman SK, Kalsekar I, Hebden T, et al. Effect of communicating depression severity on physician prescribing patterns: Findings from the Clinical Outcomes in Measurement-Based Treatment (COMET) trial. Gen Hosp Psychiatry. 2012;34:105–112. doi: 10.1016/j.genhosppsych.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Harding KJK, Rush AJ, Arbuckle M, Trivedi MH, Pincus HA. Measurement-based care in psychiatric practice: A policy framework for implementation. J Clin Psychiatry. 2011;72:1136–1143. doi: 10.4088/JCP.10r06282whi. [DOI] [PubMed] [Google Scholar]
- 51.Bremer RW, Scholle SH, Keyser D, Houtsinger JVK, Pincus HA. Pay for performance in behavioral health. Psychiatr Serv. 2008;59:1419–1429. doi: 10.1176/ps.2008.59.12.1419. [DOI] [PubMed] [Google Scholar]
- 52.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 53.Dalrymple KL, Zimmerman M. Does comorbid social anxiety disorder impact the clinical presentation of principal major depressive disorder? J Affect Disord. 2007;100:241–247. doi: 10.1016/j.jad.2006.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Olfson M, Guardino M, Struening E, Schneier FR, Hellman F, Klein DF. Barriers to the treatment of social anxiety. Am J Psychiatry. 2000;157:521–527. doi: 10.1176/appi.ajp.157.4.521. [DOI] [PubMed] [Google Scholar]
- 55.Dalrymple KL, Zimmerman M. Differences in clinical presentation between depressed outpatients wanting versus not wanting treatment for comorbid social anxiety disorder. J Nerv Ment Dis. 2008;196:639–642. doi: 10.1097/NMD.0b013e318181353b. [DOI] [PubMed] [Google Scholar]
- 56.Lecrubier Y. Comorbidity in social anxiety disorder: Impact on disease burden and management. J Clin Psychiatry. 1998;59(Suppl 17):33–38. [PubMed] [Google Scholar]