Abstract
Objectives
Hearing aids provide the basis for improving audibility and minimizing developmental delays in children with mild to severe hearing loss. Multiple guidelines exist to recommend methods for optimizing amplification in children, but few previous studies have reported hearing aid fitting outcomes for a large group of children. The current study sought to evaluate the proximity of the fitting to prescriptive targets and aided audibility of speech, as well as survey data from pediatric audiologists who provided hearing aids for the children in the current study. Deviations from prescriptive target were predicted to have a negative impact on aided audibility. Additionally, children who were fitted using verification with probe microphone measurements were expected to have smaller deviations from prescriptive targets and improved audibility than cohorts fitted without these measures.
Design
Hearing aid fitting data from 195 children with mild to severe hearing losses were analyzed as part of a multicenter study evaluating outcomes in children with hearing loss. Proximity of fitting to prescriptive targets was quantified by calculating the average RMS error of the fitting compared to Desired Sensation Level prescriptive targets for 500, 1000, 2000 and 4000 Hz. Aided audibility was quantified using the speech intelligibility index (SII). Survey data from the pediatric audiologists who fit amplification for children in the current study were collected to evaluate trends in fitting practices and relate those patterns to proximity of the fitting to prescriptive targets and aided audibility.
Results
More than half (55%) of the children in the study had at least one ear that deviated from prescriptive targets by more than 5 dB RMS on average. Deviation from prescriptive target was not predicted by pure tone average (PTA), assessment method or reliability of assessment. Study location was a significant predictor of proximity to prescriptive target with locations who recruited subjects who were fit at multiple clinical locations (University of Iowa and Boys Town National Research Hospital) having larger deviations from target than the location where the subjects were recruited primarily from a single, large pediatric audiology clinic (University of North Carolina). Fittings based on average real-ear to coupler differences (RECD) resulted in larger deviations from prescriptive targets than fittings based on individually-measured RECD. Approximately 26% of the children in the study had aided audibility less than .65. Aided audibility was significantly predicted by the proximity to prescriptive targets and PTA, but not age in months.
Conclusions
Children in the study had a wide range of fitting outcomes in terms of proximity to prescriptive targets (RMS error) and aided speech audibility (SII). Even when recommended hearing aid verification strategies were reported, fittings often exceeded the criteria for both proximity to the prescriptive target and aided audibility. The implications for optimizing amplification for children are discussed.
INTRODUCTION
For children with mild to severe hearing loss, hearing aids provide audibility of the acoustic cues necessary to support the acquisition of speech and language skills. Guidelines and protocols have been developed to assist clinicians in providing adequate amplification to support speech and language acquisition for children (Seewald et al. 2005; Bagatto et al. 2010; King 2010) and documenting communicative outcomes in children with hearing loss (Bagatto et al. 2011). Despite the widespread use of hearing aids and acceptance of the need for effective amplification, few studies have examined the characteristics and adequacy of hearing-aid fittings in young children to determine if these important objectives are being achieved. As a result, many of the specific factors that influence the aided audibility of speech in this population have not been verified. As part of a multi-center effort to examine outcomes in children with hearing loss (Moeller et al. 2011), the current study sought to examine the characteristics of hearing aid fittings in a large cohort of infants and young children with permanent hearing loss and the factors that contribute to variability in aided audibility in pediatric hearing-aid fittings.
Quantifying the adequacy of hearing-aid fitting for infants and young children is challenging because measures frequently used in adult amplification, such as speech recognition (e.g., Hornsby et al. 2011) and listener ratings of satisfaction or quality of life (e.g., Hnath-Chisolm et al. 2007), are not as readily obtainable in young children. Recent fitting guidelines recommend that pediatric audiologists use probe microphone measurements of hearing aid gain and output to estimate the audibility of speech (King, 2010; Bagatto et al. 2010). Prescriptive formulae offer target values for selecting gain based on the long-term average speech spectrum (LTASS) and maximum output based on a sweep of multiple pure tones at a high intensity level near the maximum output of the hearing aid. Methods that have specific prescriptive formulae for children include the Desired Sensation Level v. 5.0a (DSL; Scollie et al. 2005) and National Acoustics Laboratories NAL-NL2 (Keidser et al. 2011). Prescriptive approaches for children were developed to provide a consistent and systematic fitting that maximizes the audibility of speech across a wide range of listening environments, without exceeding levels of loudness discomfort. One metric of the adequacy of hearing aid fitting in children is the proximity of the fitting to the practitioner’s intended prescriptive approach. Justification for assessing fitting quality using proximity of fit-to-target assumes that prescriptive approaches represent an appropriate and uniform method of pediatric hearing aid fitting.
Recent data reveal that school-age children with hearing aid fittings that approximate either NAL-NL1 or DSL prescriptive approaches achieved high levels of aided speech understanding, audibility, and loudness comfort over a wide range of input levels. For example, Scollie and colleagues (2010) compared DSL and NAL-NL1 prescriptive approaches for a group of 48 children between 6 and 19 years of age who were experienced and consistent users of amplification. On average, both prescriptions resulted in consonant recognition scores of 85% in quiet and comparable speech recognition thresholds in noise for sentences with considerable individual variability in speech recognition across subjects. More recently, Bagatto et al. (2011) reported auditory developmental outcomes data for 68 infants and young children who were fit to DSL v.5. Results suggested that children with hearing loss who were fit with amplification using DSL were successful in achieving age-appropriate auditory development milestones. However, degree of hearing loss was a significant predictor of outcomes with greater degrees of hearing loss associated with greater developmental delays. In another investigation, over 200 children with hearing loss were randomly assigned to either DSL 4.1 or NAL-NL1 prescriptions (Ching et al. 2012). Results indicated no significant differences between prescriptions on average across language, speech production, and functional auditory skills at age 3. These studies suggest that auditory development outcomes in infants and younger children, as well as speech recognition outcomes in older children and young adults are generally positive when prescriptive approaches are used to specify amplification.
Although evidence that consistently fitting hearing aids to prescriptive targets can positively influence outcomes in controlled studies, limited data suggest that pediatric hearing aid fittings in clinical populations are significantly more variable. The proximity of pediatric hearing aid fittings to prescriptive targets was evaluated by Strauss and van Dijk (2006) for twenty 3–6 year-old children with moderate to profound sensorineural hearing loss. Only 25% of the hearing aids in that study were within +/− 5 dB of DSL targets at three or more frequencies and the majority of the participants had hearing aid outputs significantly below prescribed targets at 4000 Hz and 6000 Hz. Degree of hearing loss was not a significant predictor of the deviations from target, suggesting that difficulty matching targets was not simply related to the presence of significant hearing loss. Because probe microphone measures were only used for half of the fittings, the authors concluded that the significant deviations from prescriptive targets could have been related to a lack of systematic verification. However, direct comparisons between the accuracy of the fittings that were verified using probe microphone measures and the fittings without verification were not reported, so the contribution of verification method to the deviations from prescriptive target remains unresolved. Additionally, the proximity of the fitting to the prescriptive target alone does not directly reflect how much of an average speech signal is audible to a child through their hearing aid.
The aided audibility of speech is also an important outcome of hearing aid fitting for children. The audibility of amplified speech is typically quantified using the aided audibility index (AAI; Stelmachowicz, Lewis, Kalberer, & Creutz, 1994) or more recently as the aided speech intelligibility index (SII; ANSI S3.5–1997). The SII is a numerical estimate of audibility across the frequency range of speech and is calculated by estimating the audibility of an average speech signal compared to the listener’s hearing thresholds or level of background noise, whichever is greater. The calculation is completed for a discrete number of frequency bands, which are each assigned an importance weight based on the contribution of that frequency band to the average speech recognition score for a group of adult listeners with normal hearing. The audibility of each band is multiplied by the importance weight for that band. The weighted audibility of all bands is summed to create a number between 0 and 1 that describes the weighted audibility of the LTASS, where a value of 0 indicates that none of the LTASS is audible and 1 represents complete audibility. The SII can be used to compute audibility for aided or unaided speech spectra.
The SII has been used to quantify the relationship between audibility and speech recognition for children with normal hearing (Scollie, 2008; Gustafson & Pittman, 2009; McCreery & Stelmachowicz, 2011) and children with hearing loss (Stelmachowicz et al. 2000; Scollie, 2008). For adults, the SII can be applied to transfer functions to predict speech recognition with relative accuracy (see Amlani, Punch & Ching, 2002 for a review). Transfer functions for speech recognition based on the SII for children with normal hearing vary as a function of age, even when the linguistic context of the stimulus is significantly constrained (Scollie, 2008; McCreery & Stelmachowicz, 2011). In general, children need greater audibility as measured by the SII in order to achieve maximum levels of speech recognition (Stelmachowicz et al. 2001; Scollie, 2008). Despite the limitations of the SII for estimating aided audibility for children, speech recognition results from children have generally followed the same pattern as adults with increasing speech recognition as audibility increases, but with a shallower transfer function slope than what has been reported for adults.
Aided audibility has been shown to predict communicative outcomes in children with hearing loss, including language development and speech understanding. Stiles, Bentler and McGregor (2012) reported that children with mild to moderately-severe hearing loss with an aided SII less than 0.65 demonstrated greater delays in vocabulary development than children with hearing loss with better aided audibility. Davidson and Skinner (2006) used the aided SII to quantify the audibility of hearing aid fitting and predict speech recognition outcomes in a group of 26 children and young adults with severe-to-profound hearing loss between the ages of 6 and 16 years. Speech recognition scores were measured using the Lexical Neighborhood Test (LNT; Kirk et al. 1999). Although audibility was limited due to the subjects’ significant hearing losses, individual differences in aided audibility were significant predictors of aided speech recognition ability for both soft and average speech input levels. More recently, Sininger and colleagues (2010) reported aided SII data for a cohort of 44 children with mild to profound hearing loss. In all, the investigators found that the SII decreased systematically as degree of hearing loss increased using a 70 dB speech signal. The relationship between aided audibility and outcomes was not examined by Sininger and colleagues because aided audibility values were highly correlated with degree of hearing loss in that study. Although these findings confirm the relationship between audibility and hearing loss for hearing aids fit closely to prescriptive targets using a consistent and systematic approach, data from Strauss and van Dijk (2006) illustrate the significant variability in audibility that can occur in young children when fittings deviate significantly from prescriptive target in clinical populations. Thus, an evaluation of the characteristics of hearing aid fittings in children should include metrics of proximity to prescriptive targets and aided audibility, as well as an analysis of the impact that deviations from prescriptive approaches have on aided audibility.
In addition to specifying the characteristics of hearing aid fittings in children, the current study sought to identify factors that contributed to deviations from prescriptive targets and limited audibility. Identifying such provides specific guidance for improving the adequacy of hearing-aid fitting and maximizing communication and auditory development. The verification method used to fit the hearing aid is one potential factor that could influence the accuracy of hearing aid fittings in children. In order to account for the rapid ear canal growth and related acoustic changes that occur during early childhood, the ear-canal acoustics of the child must be integrated into the hearing-aid fitting and part of the on-going process of hearing-aid verification (Bagatto et al. 2005). Individual ear canal acoustics can be accounted for directly by measuring the output of the hearing aid in the child’s ear using a probe microphone measurement system. However, real-ear verification requires multiple measurements be taken to ensure that speech is audible over a range of input levels and that the maximum output does not exceed estimated discomfort levels. Because of the time and cooperation required, real-ear measurements may not be practical in infants and young children (Bagatto et al. 2005). An alternative method involves measuring the real-ear-to-coupler-difference (RECD; Feigin et al. 1989; Sinclair et al. 1996), which requires a single probe microphone measurement of the child’s ear canal with the earmold in place. The ear canal response is compared to the same sound measured in a 2 cc coupler, and the difference is used to estimate the response of the hearing aid in the child’s ear for verification completed in the 2 cc coupler. Age-related average RECD values are available in cases where the response cannot be reliably measured on an individual child (Bagatto et al. 2002). Despite the common goal of these methods to integrate individual ear canal acoustics into the hearing aid verification process, variability related to the specific verification approach could influence the consistency of hearing aid fitting in children. In general, individually-measured RECD would be predicted to be more accurate than an age-related average RECD for an individual child, resulting in closer approximation to the intended prescriptive targets.
The clinical setting and expertise of the hearing aid service provider where the child receives their hearing aid could also influence the quality of hearing aid fitting outcome. Clinics that specialize in pediatric assessment and amplification may be more likely to have the equipment and expertise needed to implement pediatric assessment and verification protocols, although the effect of the audiologist’s pediatric experience and training on fitting outcomes in children has not been evaluated previously. While some children with hearing loss receive amplification at large centers that specialize in pediatrics, many live in areas where pediatric audiologists are not easily accessible. The previously cited findings from Strauss and van Dijk (2008) suggest that nearly 50% of children in their study received hearing aids without verification, although the pediatric training and experience of the audiologists who fit the children in that study were not reported. The availability and extent of hearing aid funding and other resources may vary across states and localities, which may impact the quality of hearing aids available for children. Therefore, the current study sought to evaluate how characteristics of pediatric hearing aid fittings varied across different clinical settings and study sites.
Hearing aid fitting outcomes, including proximity to prescriptive target and aided audibility, have the potential to moderate the development of children with hearing loss. The primary goal of the current study was to evaluate the characteristics of hearing aid fittings for a large group of children with mild to severe sensorineural hearing loss. The aided audibility of the long-term average speech spectrum as measured by the aided SII and the proximity of the fitting to the intended prescriptive target were measured as part of an on-going longitudinal study, known as the Outcomes for Children with Hearing Loss. Factors which may have influenced the proximity to prescriptive target and aided audibility of hearing aid fittings in infants and young children, including age, audiometric configuration, verification method and clinical setting of the fitting were analyzed. In addition to electroacoustic hearing-aid measurements obtained by audiologists at the time of study visits, survey data from the pediatric audiologists who fit the children in the study were used to evaluate the training, expertise and verification methods. Three research questions were investigated in this group of infants and young children with mild to severe hearing loss:
What is the proximity of hearing aid fitting to the intended prescription?
How do deviations from prescriptive targets affect aided SII?
What patient or provider factors influence the adequacy of hearing aid fittings in this population?
METHOD
Participants
Participants included 195 children with hearing loss recruited as part of the Outcomes for Children with Hearing Loss longitudinal study. Children were recruited from three study sites and surrounding areas including 15 U.S. states: University of Iowa, Iowa City, Iowa (UI; n = 68); University of North Carolina, Chapel Hill, NC (UNC; n=43); Boys Town National Research Hospital, Omaha, Nebraska (BTNRH; n= 84). Children with pure tone averages between 25 and 75 dB HL and confirmed sensorineural, mixed or permanent conductive hearing loss were part of the OCHL cohort. Children with developmental disabilities in addition to hearing loss were not included. To be included in the current analyses, children wore an air conduction hearing aid in at least one ear. Seventy additional children who wore hearing aids with frequency lowering signal processing were excluded from the current analysis due to current limitations in calculating aided audibility for frequency-lowered signals using a standard method, such as the SII. Children ranged in age from 5 to 85 months (Mean = 41.29 months; SD = 20.5). The sample included 98 female and 97 male participants.
Pure tone audiometry
Pediatric audiologists at each test site performed audiometric testing on all children. Air and bone conduction thresholds were obtained for each ear at 500, 1000, 2000, and 4000 Hz using visual reinforcement audiometry, conditioned play audiometry, or conventional audiometry depending on the child’s age and developmental factors. Insert earphones (ER-3A) were used for air conduction thresholds and Radioear BC-71 transducer with a standard or pediatric headband was used for bone conduction thresholds. If testing could not be completed, the child’s audiologist provided a copy of the most recent reliable audiogram. The three-frequency pure tone averages were 48.49 dB (SD=16 dB) for the left ear and 48.02 dB (SD =15 dB) for the right ear.
Hearing aid verification measures
One pediatric audiologist at each of the three test sites completed electroacoustic hearing aid measurements as part of the study protocol in a clinical test room at each study visit. Hearing aid quality control measurements included measures of total harmonic distortion, frequency range, and output sound pressure level at 90 dB (OSPL90) obtained in a 2 cc coupler following ANSI S3.22 (2003). Following electroacoustic assessment, the audiologist conducted probe microphone measures to quantify the real-ear-to-coupler-difference (RECD) for verification of speech audibility and maximum output (Bagatto et al. 2005). When the RECD could not be measured due to limited cooperation or subject noise, an age-related average RECD estimated the acoustic characteristics of the child’s occluded ear. Hearing-aid verification was then completed in the 2 cc coupler. Audioscan Verifit™ software calculated aided and unaided SII for the participants, using the standard male speech signal (carrot passage) presented at 65dB SPL (average speech) and 50 dB SPL(soft speech), following ANSI S3.5 (1997). A swept pure tone at 90 dB SPL measured maximum output. The obtained fitting data were then compared to the prescriptive targets of the DSL 5.0a for each input level and the deviation from DSL target was calculated by taking the root-mean-square (RMS) of the deviations from target across four frequencies (500, 1000, 2000, and 4000 Hz) into a single RMS error value. The RMS or quadratic mean is calculated by taking the square root of the mean of the squared errors across frequency.
Hearing aid fitting targets were generated based on the audiogram obtained at the study visit. To evaluate the characteristics of the hearing aid fittings, an RMS error of fit-to-target less than 5 dB was considered to be adequate proximity to DSL prescriptive targets, based on previous studies of hearing aid fittings with adults (Byrne & Cotton, 1988; Cox & Alexander, 1990; Baumfield & Dillon, 2001; Moore, Alcantara & Marriage, 2001). For the aided SII, values less than .65 were considered to be less than optimal based on data from Stiles et al. (2012) and normative SII data from Bagatto et al. (2011). For the range of hearing losses in the current study, aided SII of .65 or higher was attainable for most fittings within 5 dB RMS error of DSL v.5 prescriptive targets.
Audiology service provider survey data
Each child’s local audiology service provider was asked to complete a survey that was designed to establish information about the education, experience and clinical setting where the child’s audiology and hearing aid services were provided. Providers who followed multiple children enrolled in the study completed a questionnaire for each child, so that data were available individually for each child in the study. Specific questions were asked regarding the hearing aid fitting and verification methods used for the specific child enrolled in the study as well as the audiologists’ comfort level with pediatric assessment and amplification procedures. Service providers were offered a gift card for their time completing the provider survey. A copy of the survey is included in Appendix A. Surveys were returned for 64% of the children. The survey data were analyzed by linking each audiologist’s response to the specific child that the audiologist fit from the study. This linkage allowed direct comparison between the fitting outcomes measured at the study visit and the prescriptive approach, verification method, training and experience, and availability of hearing-aid verification equipment in their clinical setting.
RESULTS
Descriptive hearing aid verification data
Verification and ANSI standard hearing aid measurements were obtained for 195 right hearing aids and 188 left hearing aids. All of the hearing aids were behind-the-ear (BTE) hearing aids. FM systems were used in conjunction with hearing aids by 25% of participants (63% reported no FM use; 12% did not report). Children who used FM were significantly older (mean = 51.96 months, SD = 16.3 months) than children who were reported not to use FM (mean = 36.6 months, SD = 20.2 months) [F(1,180) = 22.83, p < 0.001, ηp2=0.357. At the study visit, real-ear-to-coupler-difference (RECD) measurements were completed on 103 right ears and 98 left ears and age-related average RECDs were used for 78 right ears and 76 left ears. The ANSI S3.22 (2003) measures of hearing aid quality are included in Table 1. Data from the audiology service provider survey revealed that the prescriptive approach used to fit the hearing aid was reported to be DSL in all cases except two (four ears), where NAL-NL1 was reported as the prescriptive approach. Those four ears were excluded from analyses where the proximity of the fitting was compared to DSL v.5.
Table 1.
Results of ANSI S3.22 (2003) measures
| Left | Right | |||
|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | |
| Average gain | 24.69 dB (9.315) | 7 – 53 dB | 24.39 dB (8.967) | 7 – 47 dB |
| Average OSPL | 97.42 dB (6.758) | 68–118 dB | 97.47 dB (6.421) | 80–119 dB |
| Maximum OSPL | 104.81 dB (6.5 dB) | 86 – 124 dB | 104.80 dB (6.71 dB) | 92 – 125 dB |
| Frequency range | 212.99 – 6692.48 Hz | 200 – 8000 Hz | 217.13 – 6596.32 Hz | 200 – 8000 Hz |
| Total Distortion | ||||
| 500 Hz | 0.72 % | 0 – 7 % | 0.72 % | 0 – 7 % |
| 800 Hz | 0.48 % | 0 – 5 % | 0.48 % | 0 – 5 % |
| 1600 Hz | 0.58 % | 0 – 23 % | 0.58 % | 0 – 23 % |
OSPL = Output Sound Pressure Level at 90 dB
Proximity to prescriptive target
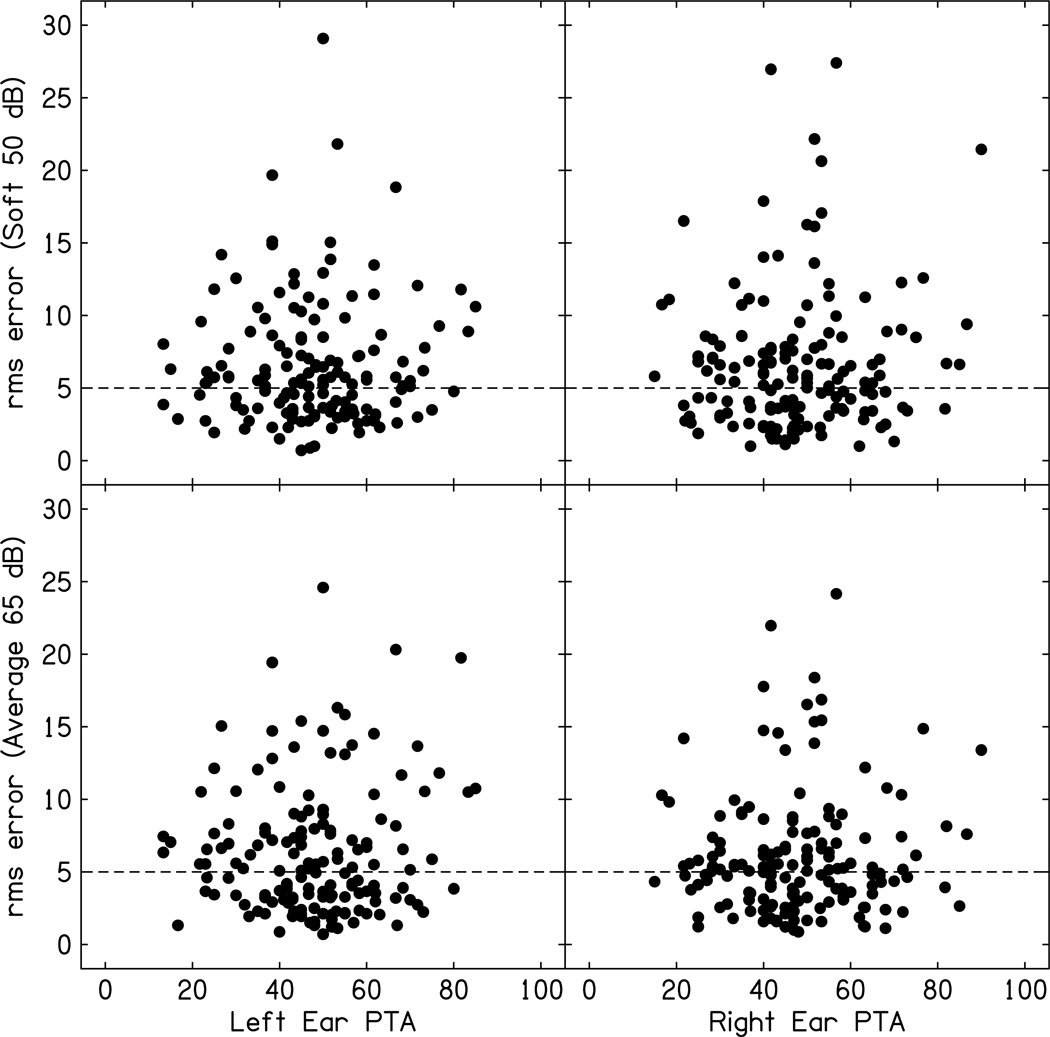
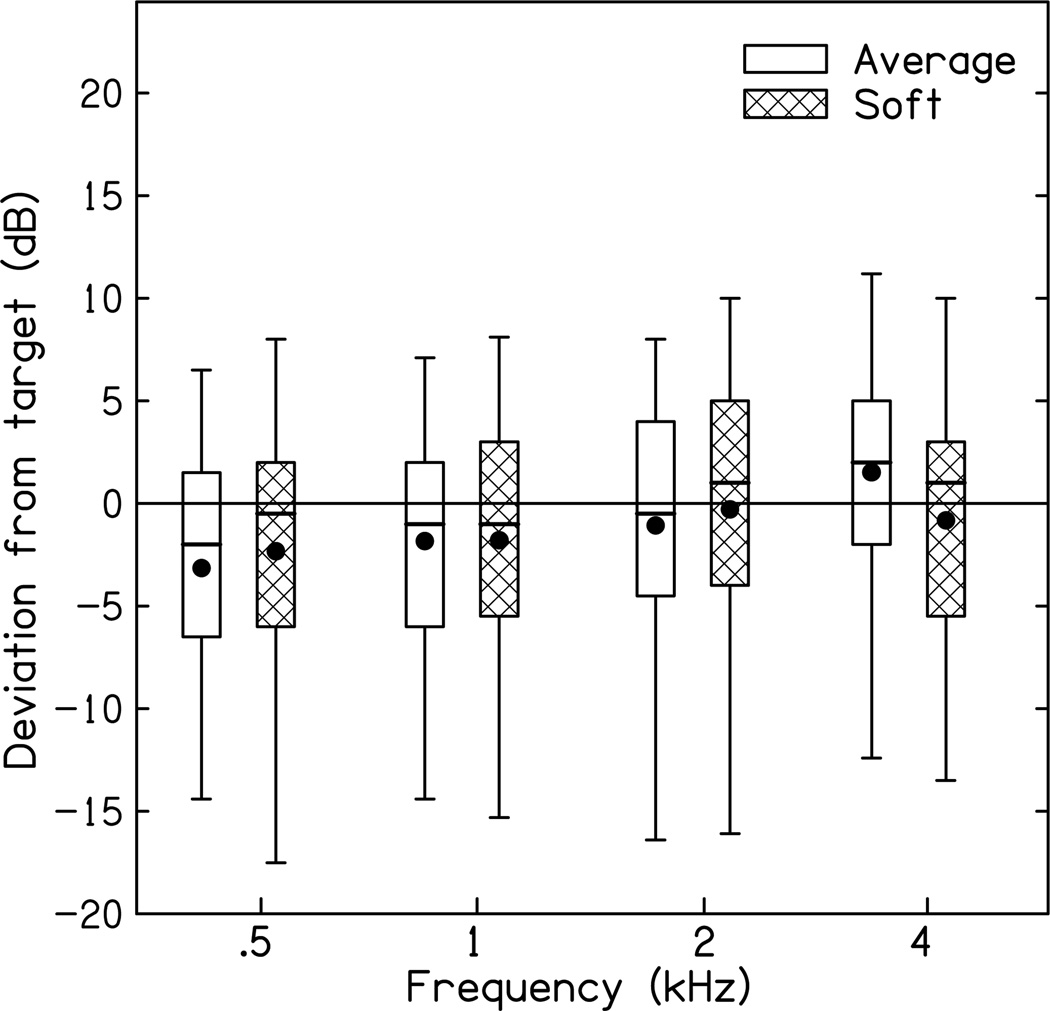
Figure 1 displays the RMS error of the fit to DSL prescriptive target obtained for soft and average speech as a function of pure tone average. Based on the criterion that an RMS error less than 5 dB was considered to be an optimal fit to DSL prescriptive targets, 54.2% (n=97) of the fittings exceeded 5 dB RMS error for fit-to-target for the right ear and 55.6% (n=95) had RMS errors that exceeded 5 dB for the left ear. To evaluate the impact of degree of hearing loss on the proximity of the fitting to prescriptive target, the relationship between pure tone average (PTA) and RMS error was evaluated. The correlations between RMS error and PTA were not significant for either ear or input level (right ear average, r = 0.047, p = .559; Left ear average, r = 0.078, p = .782; right ear soft, r = 0.079, p = 0.334; left ear soft, r = 0.039; p =.636), suggesting that degree of hearing loss did not predict RMS error. Figure 2 includes the absolute differences between the real ear aided response for average and soft input levels as a function of frequency for each of the frequencies used to compute RMS error. To determine if there were significant differences in deviations from target across frequency, a repeated-measures ANOVA was completed with level (50 dB and 65 dB) and frequency (500, 1000, 2000 and 4000 Hz) as factors. The main effect of frequency was significant [F(3,528) =23.194, p < 0.001, ηp2=0.116], suggesting that deviations from prescriptive target were different across frequencies. A post-hoc test using Bonferroni adjustment for multiple comparisons suggested that 500 Hz was significantly lower than 4000 Hz (difference = 4.16 dB). None of the other differences were significant after controlling for multiple comparisons. The effect of level and the two-way interaction between frequency and level were not significant, reflecting that the differences between soft and average input levels were not significant and that the relationship between soft and average input levels did not differ significantly as a function of frequency.
Figure 1.
Proximity of the hearing aid fitting to prescriptive target in RMS error (dB) plotted by pure tone average (PTA). The dashed line across each panel represents the 5 dB RMS error criterion used in the current study. Top panels include data for soft speech inputs (50 dB SPL) and bottom panels include data for average speech inputs (65 dB SPL). The left panels are plotted by the left ear PTA and the right panels are plotted by right ear PTA.
Figure 2.
Average of both ears for deviations from prescriptive target as a function of frequency. Box plots represent median (solid middle line) and interquartile range (25th and 75th percentile). Error bars represent the 5th and 95th percentile for each site. Open boxes are for average speech level inputs (65 dB SPL) and hatched boxes are for soft speech level inputs (50 db SPL). Filled circles represent mean data for each condition.
Because the hearing aid fittings were compared to the study audiogram, which was not always the same audiogram used to fit the hearing aid, audiometric assessment method and reliability of the study audiogram were analyzed as potential contributors to deviations from prescriptive targets. An analysis of variance (ANOVA) was conducted with test method (visual reinforcement audiometry, conditioned play audiometry, or conventional audiometry) and test reliability (good or fair-poor) as between-subjects factors. The main effects of test method [F(2,175) = 0.599, p =0.559, ηp2=0.007] and reliability [F(1,175) = 0.236, p =0.628, ηp2=0.001] and corresponding two-way interaction between test method and reliability [F(2,175) = 0.260, p =0.771, ηp2=0.003] were not significant. The lack of significant contribution for assessment factors indicates that the deviation from prescriptive target was not influenced by either the assessment method or reliability.
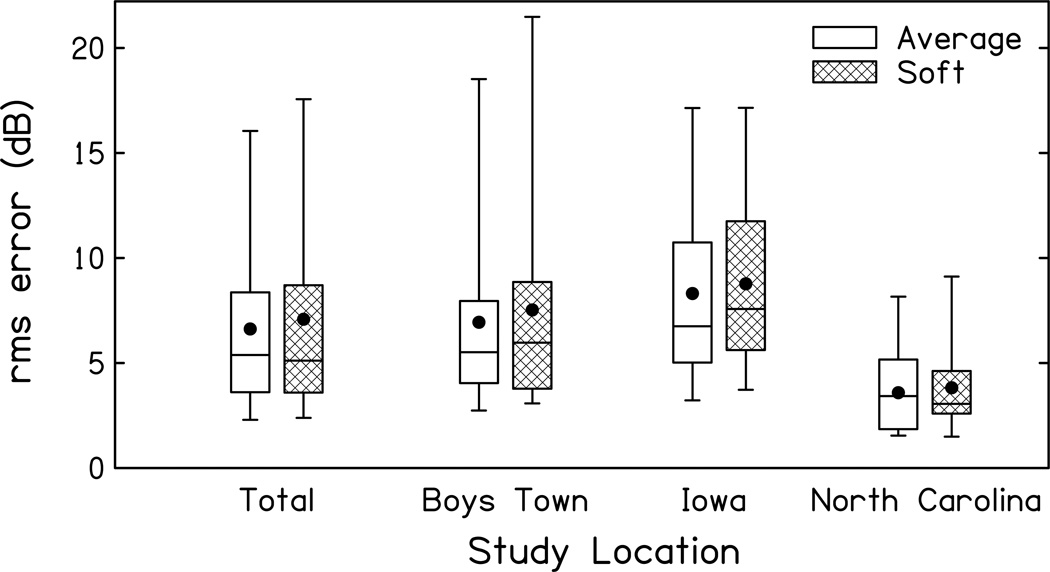
Figure 3 displays the total RMS error for average and soft speech input levels, as well as the RMS errors for each study location. A multivariate analysis of variance (MANOVA) was completed to determine if the RMS error for fit-to-target for right and left ears or soft and average speech input levels were significantly different across study sites.
Figure 3.
Average of both ears for proximity of the hearing aid fitting to prescriptive target in RMS error (dB) including overall total and data for each study location. Box plots represent median (solid middle line) and interquartile range (25th and 75th percentile). Error bars represent the 5th and 95th percentile for each site. Open boxes are for average speech level inputs (65 dB SPL) and hatched boxes are for soft speech level inputs (50 db SPL). Filled circles represent mean data for each condition.
The combined multivariate effect of site on RMS error was significant [Wilks λ = 0.830; F(8,326) = 3.974, p < 0.001, ηp2=0.089]. The corresponding univariate tests of RMS error differed significantly as a function of study location [Right ear average input, F(2,166) = 14.46, p <0.001, ηp2=0.148; Left ear average input, F(2,166) = 13.03, p <0.001, ηp2=0.136; Right ear soft input, F(2,166) = 13.121, p <0.001, ηp2=0.137; Left ear soft input, F(2,166) = 11.827, p <0.001, ηp2=0.125]. To examine the patterns of significant differences in RMS error across study location while controlling for Type I error, Fisher’s LSD was used to calculate a minimum mean significant difference in RMS error of 2.86 dB. For comparisons of both ears and both input levels, UNC had significantly lower RMS errors on average than the UI and BTNRH across all comparisons. The difference between average RMS errors for UI and BTNRH were not significant after controlling for multiple comparisons.
Given the significantly variability across subjects in the time between their last clinical audiology visit and the study visit where the fitting was evaluated (Range = 0 – 408 days), the relationship between the RMS error and days since the last clinical audiology visit was calculated for a subgroup of 72 subjects from all three study sites where this information was available. The range and distribution of RMS error for the subgroup (RMS error range = 0.87–22.5) was representative of the entire sample (RMS error range = 0.87 – 24.5; Kolmogorov-Smirnov test comparing distribution of RMS error of subgroup to remaining sample, p = .135). The correlation between days since the last clinical audiological assessment and the study visit and the RMS error was not significant (r = −.121, p = .363), suggesting that the magnitude of the deviation from prescriptive target was not related to the length of time since the last audiological assessment.
To examine the influence of verification method on the RMS error relative to prescriptive targets, the difference in RMS error in dB deviation from target was compared for fittings reported in the audiology service provider survey to have been verified with age-related average RECD and fittings reported to have been verified with RECD measured individually for each child. A one-way analysis of variance was completed with verification method (average vs. measured) as the between-subjects factor. Results indicated that the difference in RMS error (1.76 dB) between verification methods was significant [F(2,179) = 3.798, p = .024, ηp2=0.041] and larger for fittings using an average RECD (7.44 dB; SD = 5.3 dB) than for fittings using an individually-measured RECD (5.72 dB; SD = 3.71 dB). To quantify the differences in RMS error that could have been related to differences in the verification method between the clinical hearing aid visit and study visit the RMS error for fittings where the same verification method was reported for both the clinical and study visits was compared to the RMS error for fittings where a different verification method was reported in the audiology survey than was used at the study visit. The mean difference in RMS error between subjects where the same verification method was used for both visits (5.63 dB, SD= 3.24) and where a different verification method was used between the study visit and clinical visit reported in the audiology service provider survey (5.89 dB, SD = 4.1) was not significant (F(1,118) = 1.23, p = .545, ηp2=0.005).
Aided speech audibility
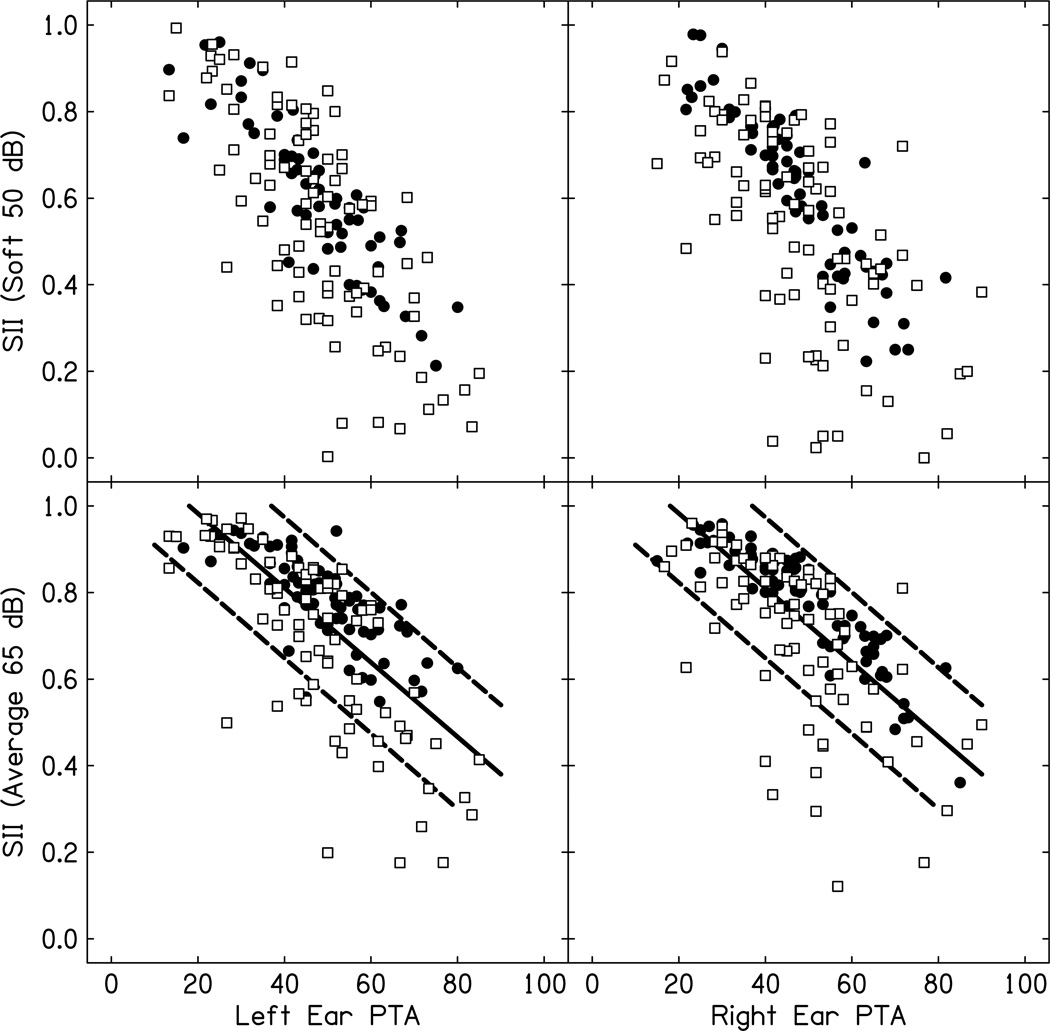
Figure 4 displays the aided audibility of speech as a function of PTA for average and soft speech input levels and left and right ears.
Figure 4.
Speech intelligibility index (SII) values for soft speech input levels (50 dB SPL; top panels) and average speech input levels (65 dB SPL; bottom panels) as a function of left ear (left panels) and right ear (right panels) pure tone average. The closed circles are fittings with < 5 dB RMS error and the open squares are fittings with >5 dB RMS error. For the average speech input levels, the normative SII range from Bagatto et al. 2011 is plotted as solid (mean) and dashed (confidence intervals) lines.
Only 26% of the right ear (n=47) and left ear (n=45) fittings had aided audibility below an SII of 0.65, the criterion set for adequate aided audibility. Linear regression assessed the relationship between audibility, RMS error relative to prescriptive target, and PTA while controlling for age. For the right ear, the linear regression model that included age (in months), three-frequency PTA, and RMS error was significant, accounting for 78.1% of the variance in aided audibility [Adjusted R2= 0.781, F(3,150) = 178.727, p < 0.001]. Age was not a significant predictor of audibility (p = 0.612), but both PTA (p < 0.001) and RMS error (p < 0.001) were significant. For PTA, there was a significant decrease in audibility as thresholds increased (β = −.663). Observed RMS errors also had a significant negative impact on aided audibility (β = −.563). The same model for the left ear data accounted for 76% of the variance in aided audibility [Adjusted R2= 0.761, F(3,143) = 156.003, p < 0.001] with the same statistical patterns of contribution for age (p = .544), PTA (p < .001; β= −681) and RMS error (p < 0.001, β= −.681).
Pediatric audiology provider survey data
One hundred twenty-six survey responses were received from 69 audiologists describing pediatric hearing-aid fitting experience and practices for the professionals who fit the hearing aids for children in the current study. Some audiologists who responded to the survey fit multiple participants in the study. This represents a response rate for 64% of participants and 55% of audiologists. By study location, 42 responses were received for the UI participants (representing 22 clinical locations), 41 for the BTNRH participants (representing 14 clinical locations) and 43 for the UNC participants (representing 2 clinical locations). All of the providers who responded had graduate degrees in audiology (Education: Au.D. = 44.6%, n=88; Master’s degree = 18.5%, n=36; other degree = 1%, n=2). The practice settings were primarily hospital (51.8%; n=101), followed by private practice (5.6%, n=11), school system (4.6%, n=9), university (2.1%, n =4) and one subject did not report his/her work setting. Most of the service providers reported using either real ear measures (12.8%, n =16) or simulated real-ear measurements based on RECD (age-related average RECD, 14.4%, n= 18; individually-measured RECD, 59.2%, n = 74) as the method for verifying audibility. The verification method reported for the fitting was the same as the verification method used for the study in 72% of cases. Some respondents indicated that they used aided sound field behavioral thresholds as the verification method for 17 subjects (9.1%). Although the limited number of respondents who reported using aided sound field thresholds prevents the comparison of RMS errors across fitting methods statistically, the RMS error of fit-to-target was larger on average for subjects whose fittings were verified using aided sound field (7.92 dB; SD = 4.67 dB) than for subjects who received probe microphone measures as verification (5.67 dB; SD = 3.95 dB). All of the providers who reported using aided sound field testing as their verification method reported having probe microphone equipment in their clinics. There was no significant relationship between providers’ reported years of professional experience and RMS fitting error (r = 0.044; p = .653).
DISCUSSION
The purpose of this study was to evaluate the characteristics of hearing aid fittings in infants and young children with mild to severe hearing loss. Whereas previous studies revealed that adherence to prescriptive targets supports positive auditory, speech, and language outcomes (Bagatto et al., 2011) and that aided speech audibility predicts vocabulary development (Stiles et al., 2012) and speech recognition (Davidson & Skinner, 2006), few studies have examined the audibility and proximity to prescriptive targets in children. Previous data from a small clinical population of children revealed that only 25% of preschool children were fit to the specified target at three or more frequencies and that only half of the children received verification with probe microphone measures (Strauss & van Dijk, 2008). However, the link between the fitting practices of the audiologists in that study and the fitting outcome were not directly reported. The present study evaluated hearing aid fittings of 195 children with mild to severe hearing loss using the RMS error in dB relative to the prescriptive target and an estimate of aided audibility for each participant. Multiple variables contributed to larger RMS errors and limited audibility. Additionally, survey data from audiology service providers supplied supporting information about the expertise and hearing-aid verification methods used for 126 children in the study whose audiologists completed the survey.
Hearing aid fitting characteristics
Overall, most children in the study were fit with hearing aids with characteristics that met consensus guideline recommendations (AAA, 2003; Bagatto et al. 2010). Specifically, children were fit binaurally (92.3%, 180/195) with behind-the-ear hearing aids (100%). Children were primarily fit with digital hearing aids (97.4%, 190/195) with low distortion. Approximately 25% of participants reported using FM systems in conjunction with hearing aids, which is reasonable for a cohort of infants and young children. Children who used FM in conjunction with hearing aids were significantly older (mean = 51.96 months; SD=16.3 months) than children who did not use FM (mean = 36.6 months; SD = 20.2 months), reflecting more frequent use of FM as children enter the age range for preschool.
The proximity of pediatric hearing-aid fittings to prescriptive targets was 6.6 dB on average across all fittings. This value exceeded the 5 dB criterion set forth in previous adult studies of proximity related to prescriptive target (Byrne & Cotton, 1988; Cox & Alexander, 1990; Baumfield & Dillon, 2001; Polonenko et al. 2010). The current cohort of hearing-aid fittings also deviated from prescriptive target to a greater degree than published reports evaluating the relationship between prescriptive approaches and developmental outcomes in children (Ching et al. 2012). For children with mild to severe hearing loss, fitting the hearing aid within 5 dB of prescriptive targets represents a reasonable and achievable standard if appropriate verification methods are used. Approximately 60% of the children in the study had at least one hearing aid that exceeded 5 dB RMS error and 55% exceeded 5 dB RMS error in both ears. Age and degree of hearing loss were not significant predictors of deviation from target, which ran counter to the hypotheses of the current study. Age was anticipated to be a significant predictor of fitting error due to normal age-related variability observed in behavioral thresholds, as well as the changes in ear canal acoustics that occur during early childhood related to growth (Bagatto et al., 2005). The lack of contribution from degree of hearing loss is likely related to the fact that most of the children in the study had mild to moderate hearing loss, which would not be expected to limit the ability to match targets for the frequency range of targets evaluated in this study (500 – 4000 Hz). Contrary to previous results suggesting limited audibility at 4000 Hz, the current study found the largest deviations from prescriptive target at 500 Hz. Children with greater degrees of loss may experience limited aided audibility or significant deviations from prescriptive targets related to gain or bandwidth limitations of the hearing aid. Such limitations may have contributed to deviations from prescriptive targets reported in previous studies that included children with moderate to profound hearing losses (Strauss & van Dijk 2008).
A potential limitation of the design of the current study was related to the audiogram used to evaluate each child’s hearing aid fitting. Fittings in the current study were compared to prescriptive targets based on the audiogram collected on the day of the study visit. The thresholds obtained at that visit may have differed from the audiogram on which the child’s local audiologist based the most recent hearing aid fitting. Differences in thresholds obtained between the two tests could have been due to actual changes in thresholds (temporary or permanent), or test reliability due to either child or tester variables. However, there was no relationship between the length of time since the child’s last audiological evaluation with their service provider and the size of the deviation from prescriptive target, despite the fact that some participants had not been evaluated by their audiologist in over a year. Additionally, there was no difference in the proximity to prescriptive target between children whose audiologists reported using a different verification method at the fitting than was used to evaluate the fitting at the study visit.
The verification method reported by the child’s audiologist was found to predict variability in both the fit to prescriptive target and aided audibility. The verification method used to fit the hearing aid was the same used to evaluate the fit for the study in 72% of cases. While the incorporation of RECD into the hearing aid fitting is expected to minimize variability in fitting related to growth, approximately 35% of children required the application of an age-related average RECD at the time of their study visit, which is less likely than a measured RECD to account for the variability on an individual basis. The child’s degree of hearing loss was predicted to contribute to RMS error in fit-to-prescriptive targets, particularly for listeners with the greatest degrees of hearing loss, where limitations of amplification or loudness discomfort may limit the ability to match targets. This was not observed, likely due to the range of hearing losses included in the study, which were primarily mild-to-moderate. Therefore, the ability to provide audibility and accurately match prescriptive targets was not as likely to be limited by the listener’s dynamic range or the hearing aid characteristics, as in previous studies with children who have greater degrees of hearing loss (Davidson & Skinner, 2006).
Site and verification method reported in the audiology service provider survey, however, were both significant predictors of the RMS error. Subjects recruited at UNC had significantly smaller fitting errors than subjects recruited from the UI or BTNRH. This finding is likely related to the fact that the majority of the children recruited at UNC received their hearing aids through the UNC clinic, whereas the children recruited at Iowa and BTNRH received their hearing aids from a larger number of audiology practices throughout the catchment areas. Another potential contributor to differences across site could be related to differences in the availability of hearing aid funding and other resources. Although all three states where most of the participants reside have relatively strong funding opportunities for hearing aids, differences in the ability to replace hearing aids in the case of progressive losses may have influenced the differences in fittings across study sites. Smaller errors at UNC may also reflect a more consistent approach between the methods used by the clinical audiologists and those used to assess fitting quality in the study. The verification method reported by the fitting audiologist also resulted in a small, but significant difference (1.7 dB) in RMS error. The use of an age-related average RECD resulted in larger deviations from prescriptive target than fittings where the RECD was measured individually. Although this finding is congruent with previous reports that measured RECD is more accurate on an individual basis than an age-related average RECD (Bagatto et al. 2010), whether the average or measured RECD is used clinically is often dependent on the child’s age and cooperation. The reduction in RMS error for the measured RECD supports published recommendations, which suggest that RECD should be measured whenever possible and an age-related average can be used when measurement of RECD is not feasible due to the child’s cooperation or other factors (Bagatto et al. 2010; King, 2010).
The other primary outcome of the current study aside from proximity to prescriptive targets was the audibility of speech for average and soft input levels. Most of the children in the study had aided audibility that exceeded the .65 aided SII criterion that was set for adequate audibility. This criterion was based on research by Stiles and colleagues (2012) on the impact of aided audibility on vocabulary development and the normative SII by degree of hearing loss data from Bagatto et al. (2011). Approximately 26% of study participants had aided audibility of less than .65 in at least one ear. In the current study, children with the greatest degrees of hearing loss or largest deviations from prescriptive targets had the poorest audibility. Data reported by Sininger and colleagues (2010) highlight the relationship between audibility and degree of hearing loss for fittings matched closely to DSL targets using a consistent fitting methodology. However, the variability in aided audibility in the current sample is much greater than what was reported by Sininger et al., even for children with mild and moderate degrees of hearing loss. This discrepancy is likely related to the fact that the participants in Sininger et al. received hearing-aid verification at the same location by audiologists affiliated with the study. This would make the cohort from Sininger et al. more similar to the cohort of children from UNC in the current study, who showed significantly less variability in fitting than children enrolled at Iowa and BTNRH. The deviation of the fitting from prescriptive target was also a significant predictor of aided audibility, even when controlling for the influence of degree of hearing loss. Specifically, large deviations were related to significant decreases in audibility when controlling for degree of hearing loss. While many participants with fitting errors greater than 5 dB achieved aided audibility similar to their peers with the same degree of hearing loss and smaller fitting errors, the contribution of deviations from prescriptive targets was nearly as large as the contribution of degree of hearing loss. Additionally, fitting errors had a much more substantial impact on audibility for children with greater degrees of hearing loss, who are prescribed less audibility than their peers with lesser degrees of hearing loss.
Pediatric audiologist survey data
The current study also sought to explore the relationships between the experience, verification methods and practice setting of service providers and fitting outcomes in children. While a wide range of factors could potentially influence the variability of hearing-aid fitting outcomes in children, factors specific to professional practices are important contributors that could be improved through training and education. Each audiologist’s responses from the survey were linked to the specific child fitting outcomes in the study to allow for a direct comparison of reported fitting practices and outcomes. All but a limited number of practitioners who responded to the provider survey reported following current guidelines for pediatric amplification (AAA, 2003; Bagatto et al., 2010; King 2010). The vast majority of service providers reported using the DSL prescriptive method (98%; 123/125), while the remaining two service providers reported using NAL-NL1. Recent studies suggested that although there are differences between DSL v. 4 and NAL-NL1 in both gain and output, speech recognition and audibility outcomes are similar between the two prescriptions(Scollie et al., 2010; Ching et al., 2010; Ching et al. 2012). Comparisons are further complicated by the fact that updated versions of each algorithm (DSL v.5 and NAL-NL2) have been developed and are used clinically by pediatric audiologists. Despites these developments, Crukley & Scollie (2012) reported similar speech recognition outcomes for DSL v.5 as were reported for DSL 4.1 in quiet. This trend reflects the fact that changes to pediatric prescriptive formulae are based on evidence and would not be likely to result in significant changes in audibility or speech understanding.
Approximately 86% of the audiologists who responded to the survey reported that they used either real-ear or simulated real-ear measurements based on RECD as their primary method of verification, consistent with current recommendations (Bagatto et al. 2010; King 2010). The remaining 9% reported using aided sound field behavioral thresholds as the primary method of verification for pediatric hearing aid fitting. All of the audiologists who reported using aided behavioral thresholds as a verification method reported having access to probe microphone equipment in their clinic, suggesting that access to verification equipment was not a factor in their decision not to use probe microphone measures. The relatively small number of respondents who used aided sound field thresholds as verification prevents statistical comparisons of RMS error to subjects who were fit using probe microphone methods. However, the average error in fit-to-target was larger for children who were verified behaviorally (7.9 dB; Range= 4 – 21.5 dB) than for children who reportedly received objective probe microphone verification (5.6 dB; Range= 0.87 – 12 dB). There was no significant relationship between years of professional experience and the size of the deviation from prescriptive target, suggesting that professional experience was not a factor in the deviations from prescriptive target observed in the current study.
Despite the widespread reported use of DSL and probe microphone measures by audiologists who fit hearing aids for the children in the current study, a wide range of variability in the proximity of the fitting to the prescriptive target was observed, particularly for subjects recruited at the UI and BTNRH sites. The variability in fit-to-target despite the reported application of recommended pediatric procedures highlights challenges in the consistent implementation of clinical protocols. Specifically, audiologists in the current study reported using recommended verification methods, but did not always achieve optimal fittings related to their stated prescriptive goal. However, the survey did not ask service providers what circumstances might have prevented fitting closer to prescriptive target. Further research of clinical practices of pediatric audiologists would be needed to determine why the fitting errors were so large despite the reported use of published pediatric protocols. Survey respondents may have reported what they knew to be recommended practices and protocols, rather than the methods that they actually used clinically. Furthermore, pediatric audiologists may have had to adjust the hearing-aid fitting away from prescriptive targets to minimize the occurrence of feedback or because of the audiometric configuration. Practitioners must use the information obtained during hearing-aid verification to optimize the fitting as part of an on-going assessment process in order to achieve a consistent hearing-aid fitting outcome.
Limitations and directions for future research
While the current study was one of the first to evaluate the audibility of hearing aid fittings in a large population of children with mild to severe hearing loss, there are several important limitations that must be considered when evaluating the results of this study and the implications for clinical practice. The average time interval between the child’s clinical hearing aid evaluation and study visit was less than 6 months, but varied significantly across participants. There was no significant relationship between the length of time between the clinical and study visits and the deviation from prescriptive target for a subset of the children in the study. Nonetheless, the potential for changes in audiometric thresholds between the hearing aid fitting and study visit leaves the potential for errors that were related to progression or fluctuation of hearing loss in some cases.
The 5 dB RMS error criterion for proximity to prescriptive targets has been used in previous studies and is an attainable standard for most children with mild to severe hearing loss. However, validation studies have revealed similar speech recognition outcomes (Scollie et al. 2010) between the NAL-NL1 and DSL 4.1 fitting prescriptions, despite the fact that NAL-NL1 prescribes less gain than DSL on average. A comparison of NAL and DSL fitting outcomes was not within the scope of the current study, as all but two children were fit to DSL. Deviations from prescriptive target were associated with reductions in audibility, even when controlling for degree of hearing loss. Further longitudinal investigation of the children in this cohort will allow estimation of the impact of deviations from prescriptive target on aided audibility and developmental outcomes.
It should be noted that the group of children in this study is likely to be different than the general population of children with mild to severe hearing loss in the United States. Many children with hearing loss are not served by centers that specialize in pediatric amplification, as was the case for nearly one-third of the subjects; as a result, the current study may overestimate audibility and underestimate the deviations from prescriptive targets of hearing aid fittings among children with hearing loss in the general population. Although most of the verification measures used to document the hearing aid fitting quality incorporated individually-measured RECDs, a large proportion of children received verification based on age-related average RECD measures. The proximity of fittings to prescriptive targets may have been different if a larger proportion of the verification in the current study were based on measured RECDs.
Conclusion
The current study evaluated the hearing aid fittings of 195 children with hearing loss. Fitting proximity as measured by RMS error in fit-to-target was not related to the child’s age, assessment method, assessment reliability or PTA. The study location and verification method were both significant predictors of RMS error in fit-to-target with larger errors being associated with study locations where participants were recruited from a wide range of clinical locations outside of the study (Iowa and BTNRH). The aided audibility for 74% of the subjects was found to be greater than .65 aided SII, but PTA and RMS error in fit-to-target were both found to be significant predictors of audibility, with limited audibility associated with higher PTA and larger RMS errors. Hearing aid fittings that were reported in survey data to have been verified using the child’s measured RECD or in-situ probe microphone measures had smaller deviations from prescriptive target than fittings reported as verified using an average RECD or functional gain. Although 86% of the pediatrics audiologists who fit children in the study reported using methods recommended by published pediatric verification guidelines, significant deviations from prescriptive target were still persistent in some cases. Further emphasis and training on expected audibility outcomes for children who wear hearing aids will help clinicians to identify the impact of deviations from prescriptive target on speech audibility.
Acknowledgements
This work was supported by a NIH/NIDCD RO1 DC009560 (Bruce Tomblin/ Mary Pat Moeller Principle Investigators). The authors would like to thank Elizabeth Walker, Meredith Spratford and two anonymous reviewers for helpful comments on an earlier version of the manuscript. The authors also wish to thank Shana Jacobs for her efforts in data collection and the audiologists who completed the survey for the current study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: No conflicts of interest.
Contributor Information
Ryan W. McCreery, Boys Town National Research Hospital.
Ruth A. Bentler, University of Iowa
Patricia A. Roush, University of North Carolina- Chapel Hill
References
- Amlani AM, Punch JL, Ching TYC. Methods and Applications of the Audibility Index in Hearing Aid Selection and Fitting. Trends in Amplification. 2002;6(3):81–129. doi: 10.1177/108471380200600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANSI. Methods for calculation of the speech intelligibility index. ANSI S3.5-1997. New York: American National Standards Institute; 1997. [Google Scholar]
- ANSI. Specification of hearing aid characteristics. ANSI S3.22-2003. New York: American National Standards Institute; 2003. [Google Scholar]
- Bagatto M, Scollie SD, Seewald RC, Moodie KS, Hoover BM. Real-Ear-to-Coupler Difference Predictions as a Function of Age for Two Coupling Procedures. Journal of the American Academy of Audiology. 2002;13(8):407–415. [PubMed] [Google Scholar]
- Bagatto M, Moodie S, Scollie S, Seewald R, Moodie S, Pumford J, Liu KPR. Clinical protocols for hearing instrument fitting in the Desired Sensation Level method. Trends in amplification. 2005;9(4):199–226. doi: 10.1177/108471380500900404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagatto M, Scollie SD, Hyde M, Seewald R. Protocol for the provision of amplification within the Ontario infant hearing program. International journal of audiology. 2010;49(Suppl 1):S70–S79. doi: 10.3109/14992020903080751. [DOI] [PubMed] [Google Scholar]
- Bagatto MP, Moodie ST, Malandrino AC, Richert FM, Clench Da, Scollie SD. The University of Western Ontario Pediatric Audiological Monitoring Protocol (UWO PedAMP) Trends in amplification. 2011;15(1):57–76. doi: 10.1177/1084713811420304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumfield A, Dillon H. Factors affecting the use and perceived benefit of ITE and BTE hearing aids. Br J Audiol. 2001;35:247–258. doi: 10.1080/00305364.2001.11745243. [DOI] [PubMed] [Google Scholar]
- Byrne D, Cotton S. Evaluation of the National Acoustic Laboratories’ new hearing aid selection procedure. J Speech Hear Res. 1988;31:178–186. doi: 10.1044/jshr.3102.178. [DOI] [PubMed] [Google Scholar]
- Ching TY, Dillon H, Hou S, Zhang V, Day J, Crowe K, Marnane V, et al. A randomized controlled comparison of NAL and DSL prescriptions for young children: Hearing-aid characteristics and performance outcomes at three years of age. International journal of audiology. 2012:1–12. doi: 10.3109/14992027.2012.705903. ePub ahed of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TYC, Scollie SD, Dillon H, Seewald R, Britton L, Steinberg J. Prescribed real-ear and achieved real-life differences in children’s hearing aids adjusted according to the NAL-NL1 and the DSL v.4.1 prescriptions. International Journal of Audiology. 2010;49:S16–S25. doi: 10.3109/14992020903082096. [DOI] [PubMed] [Google Scholar]
- Chisolm TH, Johnson CE, Danhauer JL, Portz LJP, Abrams HB, Lesner S, McCarthy Pa, et al. A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults. Journal of the American Academy of Audiology. 2007;18(2):151–83. doi: 10.3766/jaaa.18.2.7. [DOI] [PubMed] [Google Scholar]
- Crukley J, Scollie SD. Children’s Speech Recognition and Loudness Perception with the Desired Sensation Level v5 Quiet and Noise Prescriptions. American journal of audiology. 2012 doi: 10.1044/1059-0889(2012/12-0002). ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- Cox R, Alexander Evaluation of an in-situ probe microphone method for hearing aid fitting verification. Ear Hear. 1990;11:31–39. doi: 10.1097/00003446-199002000-00008. [DOI] [PubMed] [Google Scholar]
- Davidson LS, Skinner MW. Audibility and speech perception of children using wide dynamic range compression hearing aids. American journal of audiology. 2006;15(2):141–53. doi: 10.1044/1059-0889(2006/018). [DOI] [PubMed] [Google Scholar]
- Feigin JA, Kopun JG, Stelmachowicz PG, Gorga MP. Probe-tube microphone measures of ear-canal sound pressure levels in infants and children. Ear and hearing. 1989;10(4):254–8. doi: 10.1097/00003446-198908000-00008. [DOI] [PubMed] [Google Scholar]
- Gustafson SJ, Pittman AL. Sentence perception in listening conditions having similar speech intelligibility indices. International journal of audiology. 2011;50(1):34–40. doi: 10.3109/14992027.2010.521198. [DOI] [PubMed] [Google Scholar]
- Hornsby BWY, Johnson EE, Picou E. Effects of Degree and Configuration of Hearing Loss on the Contribution of High- and Low-Frequency Speech Information to Bilateral Speech Understanding. Ear and Hearing. 2011;32(5):543–555. doi: 10.1097/AUD.0b013e31820e5028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keidser G, Dillon HR, Flax M, Ching T, Brewer S. The NAL-NL2 prescription procedure. Audiology Research. 2011;1(1S):e24. doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AM. The national protocol for paediatric amplification in Australia. International journal of audiology. 2010;49(Suppl 1):S64–S69. doi: 10.3109/14992020903329422. [DOI] [PubMed] [Google Scholar]
- Kirk KI, Eisenberg LS, Martinez AS, Hay- McCutcheon M. Lexical neighborhood test: Test-retest reliability and interlist equivalency. Journal of the American Academy of Audiology. 1999;10:113–123. [Google Scholar]
- McCreery RW, Stelmachowicz PG. Audibility-based predictions of speech recognition for children and adults with normal hearing. The Journal of the Acoustical Society of America. 2011;130(6):4070. doi: 10.1121/1.3658476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller MP, Bass-Ringdahl S, Ambrose SE, VanDam M, Tomblin JB. Understanding communication outcomes: New tools and insights. In: Seewald RC, Bamford JM, editors. A Sound Foundation Through Early Amplification: Proceedings of the 2010 International Conference; Phonak AG; Chicago, IL. 2011. pp. 245–260. [Google Scholar]
- Moodie ST, Bagatto MP, Miller LT, Kothari A, Seewald R, Scollie SD. An Integrated Knowledge Translation Experience: Use of the Network of Pediatric Audiologists of Canada to Facilitate the Development of the University of Western Ontario Pediatric Audiological Monitoring Protocol (UWO PedAMP v1.0) Trends in amplification. 2011;15(1):34–56. doi: 10.1177/1084713811417634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BCJ. Cochlear hearing loss. 2nd Edition. West Sussex, England: Wiley; 2007. [Google Scholar]
- Moore BC, Alcantara J, Marriage J. Comparison of three procedures for initial fitting of compression hearing aids I. Experienced users fitted bilaterally. Br J Audiol. 2001;35:339–353. doi: 10.1080/00305364.2001.11745252. [DOI] [PubMed] [Google Scholar]
- Polonenko MJ, Scollie SD, Moodie S, Seewald RC, Laurnagaray D, Shantz J, Richards A. Fit to targets, preferred listening levels, and self-reported outcomes for the DSL v5.0 a hearing aid prescription for adults. International journal of audiology. 2010;49(8):550–60. doi: 10.3109/14992021003713122. [DOI] [PubMed] [Google Scholar]
- Scollie SD. Children’s speech recognition scores: the Speech Intelligibility Index and proficiency factors for age and hearing level. Ear and hearing. 2008;29(4):543–556. doi: 10.1097/AUD.0b013e3181734a02. [DOI] [PubMed] [Google Scholar]
- Scollie S, Seewald R, Cornelisse L, Moodie S, Bagatto M, Laurnagaray D, Beaulac S, et al. The Desired Sensation Level multistage input/output algorithm. Trends in amplification. 2005;9(4):159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scollie SD, Ching TYC, Seewald RC, Dillon H, Britton L, Steinberg J, King K. Children’s speech perception and loudness ratings when fitted with hearing aids using the DSL v.4.1 and the NAL-NL1 prescriptions. International journal of audiology. 2010;49(Suppl 1):S26–S34. doi: 10.3109/14992020903121159. [DOI] [PubMed] [Google Scholar]
- Seewald R, Moodie S, Scollie S, Bagatto M. The DSL method for pediatric hearing instrument fitting: historical perspective and current issues. Trends in amplification. 2005;9(4):145–157. doi: 10.1177/108471380500900402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair ST, Beauchaine KL, Moodie KS, Feigin JA, Seewald RC, Stelmachowicz PG. Measurement as a Function of Age. American Journal of Audiology. 1989;5:52–56. [Google Scholar]
- Sininger YS, Grimes A, Christensen E. Auditory Development in Early Amplified Children?: Factors Influencing Auditory-Based Communication Outcomes in Children with Hearing Loss. Ear & Hearing. 2010:166–185. doi: 10.1097/AUD.0b013e3181c8e7b6. (1999) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stelmachowicz PG, Hoover BM, Lewis DE, Kortekaas RW, Pittman AL. “ The relation between stimulus context, speech audibility, and perception for normal-hearing and hearing-impaired children ”. J. Speech Hear. Res. 2000;43:902–914. doi: 10.1044/jslhr.4304.902. [DOI] [PubMed] [Google Scholar]
- Stelmachowicz PG, Lewis D, Kalberer A, Creutz T. Situational hearing aid response profile (SHARP v 2.0) Omaha, NE: Boys Town National Research Hospital; 1994. [Google Scholar]
- Stiles DJ, Bentler RA, Mcgregor KK. The Speech Intelligibility Index and the Pure-Tone Average as Predictors of Lexical Ability in Children Fit with Hearing Aids. Journal of Speech, Language, and Hearing Research. 2012 doi: 10.1044/1092-4388(2011/10-0264). first published online on January 5, 2012 as doi:10.1044/1092-4388(2011/10-0264) [DOI] [PubMed] [Google Scholar]
- Strauss S, van Dijk C. Hearing instrument fittings of pre-school children: do we meet the prescription goals? International journal of audiology. 2008;47(Suppl 1):S62–S71. doi: 10.1080/14992020802300904. [DOI] [PubMed] [Google Scholar]
- Tharpe AM, Ashmead DH. A longitudinal investigation of infant auditory sensitivity. American journal of audiology. 2001;10(2):104–12. doi: 10.1044/1059-0889(2001/011). [DOI] [PubMed] [Google Scholar]