Abstract
Background:
Coronary artery disease (CAD) is accountable for more than 30% of deaths worldwide and is, thus, deemed the most important factor in terms of disease burden around the globe. This study aimed to evaluate CAD and its risk factors in hospitalized patients in the East Azerbaijan Province, northwest Iran, from 2006 to 2007.
Methods:
Data on 18.323 patients hospitalized due to cardiovascular diseases were collected to evaluate the diseases and their risk factors in 15 hospitals in the East Azerbaijan Province, northwest Iran. We assessed the main diagnosis of cardiovascular disease on admission in each hospital. Also, types of interventional and surgical procedures were assessed and all these variables were compared between men and women.
Results:
The study population consisted of 56.6% male and 43.4% female patients. The median and range between quartile 1 and 3 (Q1–Q3) ages of the males and females were 59 (49–70) and 62 (51–71) years, respectively. Ischemic heart diseases were diagnosed in 68.4%, electrophysiological disorders in 6.5%, and valvular heart diseases in 4.5% of the patients. The frequencies of the studied risk factors were as follows: cigarette smoking (47.5%); hypertension (66.95%); diabetes mellitus (35.9%); and history of cerebrovascular accident (16.4%) and renal disease (13.4%). Medical therapy was performed in 79.23%, surgery in 6.28%, and cardiovascular interventional therapy in 13.99% of the patients. The in-hospital mortality rate was 1.57% (1.42% in the males and 1.76% in the females; p value = 0.009).
Conclusion:
The most frequent known risk factors in the hospitalized patients were smoking, alcohol consumption, and diabetes. In the northwest of Iran, age at hospitalization due to cardiovascular diseases is slightly lower than that in the Western populations; however, sex distribution, diagnoses, and treatment modalities are not significantly different from those reported in Western countries.
Keywords: Cardiovascular diseases; Risk factors; Cardiology service, hospital; Registries
Introduction
Coronary heart disease, also named coronary artery disease (CAD), is accountable for more than 30% of deaths the world over and is, consequently, regarded as the most significant factor in disease burden in the world.1 In North America and Europe, CAD is considered as the most important cause of morbidity and mortality;2 and in the United States, it is reported to have affected over 16 million.3 In Iran, CAD is the leading cause of mortality, with the disease claiming 46% of all deaths in 18 provinces.4
The National Hospital Discharge Survey (NHDS) is one of the programs of the U.S. Department of Health and Human Services and Centers for Disease Control and Prevention. In its annual summary, the NHDS provides detailed diagnoses and procedural data on cardiovascular diseases.5, 6 In Iran, the Ministry of Health, in collaboration with the Management and Planning Organization, annually reports a limited version survey entitled “National Structural Resource Allocation System of In-hospital Health Care”. According to this report, 335.364 patients were discharged from the hospitals of the East Azerbaijan Province, northwest Iran, in 2005. In addition, the report revealed that 38.892 (11.47%) patients had cardiovascular diseases and that CAD was the culprit for 942 out of the 4.844 (19.53%) in-hospital deaths. In the reports of the Management and Planning Organization, however, there are no detailed data on the exact diagnoses based on the International Classification of Diseases (ICD) and the procedures performed in this group of patients.
The present study aimed to evaluate the frequency of cardiovascular diseases and their risk factors in hospitalized patients in the East Azerbaijan Province from 2006 to 2007.
Methods
A total of 18.323 individuals out of 38.892 hospitalized patients with cardiovascular diseases in the East Azerbaijan Province, northwest Iran, were enrolled in the present study from March 2006 to March 2007. Demographic data, cardiovascular risk factors, main clinical signs and symptoms, and laboratory data were evaluated retrospectively, and final medical diagnoses were made based on the assessment by cardiologists or internists. Additionally, co-morbidities were evaluated according to the ICD, version 10, as well as surgical and non-surgical procedures and outcomes.
The demographic data comprised gender (male/female), age (year), and current residence (rural vs. urban and the name of city or province). Due to the asymmetrical pattern of age distribution in both genders in the present study, median the range between quartile 1 and 3 (Q1–Q3) was used to demonstrate the frequency of cardiovascular diseases by the function of age.
Cardiovascular risk factors, including diabetes mellitus (DM), hypertension, cigarette smoking, and family history of cardiovascular disease, as well as history of renal or cerebrovascular diseases were collected from the patients’ medical records. DM was defined as a documented history of DM (irrespective of therapy method) or fasting blood glucose ≥ 126 mg/dl. Hypertension was defined as a documented history of hypertension (irrespective of therapy method) or a systolic blood pressure > 140 mmHg and/or diastolic blood pressure > 90 mmHg measured using a sphygmomanometer, cuff, and stethoscope. Cigarette smoking was defined as a history of smoking up to 8 weeks before admission to the hospital or current smoking habits. Dyslipidemia was defined as a history of dyslipidemia requiring diet or medical therapy or laboratory data showing high serum triglyceride, total cholesterol, low-density and very low-density, or high-density cholesterol levels according to the standard values of the local laboratory testing kits. A positive family history was defined as a history of sudden cardiac death, CAD in angiography, or acute myocardial infarction in the patients’ first-degree relatives aged ≤ 55 years in the males and ≤ 65 years in the females.
The therapeutic procedures were classified in three categories: 1) medical therapy; 2) interventional therapy; and 3) surgical therapy. Medical therapy mainly consisted of the administration of cardiovascular drugs during and after hospitalization. Cardiovascular interventions included percutaneous coronary angioplasty with or without stenting (bare metal or drug-eluting stents), percutaneous transluminal mitral valvuloplasty, different interventional procedures in children with congenital heart diseases, and various electrophysiological procedures for treating cardiac arrhythmias and conduction disorders. Cardiovascular surgical procedures were primarily comprised of coronary artery bypass grafting, valve replacement or repair, palliative or total correction of congenital heart diseases, and operations on the ascending or thoracic aorta.
Data collection sheets were completed by trained staff in each hospital included in the study. The collected data were entered into Statistical Package SPSS for Windows v. 16.0 (SPSS Inc. Chicago, IL, USA). The chi-square test, with or without continuity correction, and the Fisher exact test were used for comparing the categorical variables (such as the patients’ main diagnosis, frequency of risk factors, and types of surgical or interventional procedures) between the men and the women. Statistical significance was assumed at a p value ≤ 0.05.
Results
Twenty-three out of the 18.347 patients hospitalized with cardiovascular diseases in the hospitals across the East Azerbaijan Province (from March 2006 to March 2007) had insufficient data for a definite diagnosis or other required demographic or clinical data and were, therefore, excluded from the study. Finally, 18.324 patients (10.364 [56.6%] males and 7.960 [43.4%] females) were included. A total of 15.806 (86.2%) patients were inhabitants of the East Azerbaijan Province and 2.518 (13.8%) patients came from the neighboring provinces. In the males, the median (Q1–Q3) of age at hospitalization was 59 (49–70) years and in the females 62 (51–71) years (p value = 0.001).
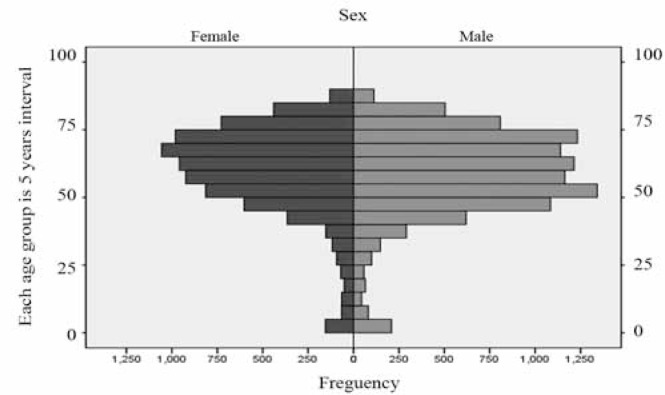
Figure 1 illustrates the age distribution in the hospitalized patients in both genders in the East Azerbaijan Province. Furthermore, hospitalization age in the males tended to be about three years earlier than that in the females, as is seen in Figure 1 (fourth decade in the males vs. fifth decade in the females). The most common age at hospitalization was 50–55 years for the males and 65–70 years for the females (Figure 1). The age distribution before 50 and after 75 years was similar in both genders.
Figure 1.
Age distribution of the hospitalized cardiovascular patients in the East Azerbaijan Province in 2006–2007. (Each age group is presented at 5-year intervals.)
Cardiovascular diseases were classified in 10 main categories (Table 1). The most common cardiovascular disease (68.4% [n = 12548]) was ischemic heart disease (7.681 [74.1%] males vs. 4.867 [61.1%] females). The second most common cause of hospitalization was electrophysiological disorders (mostly atrial fibrillation) in 1.190 (6.5%) patients, followed by valvular heart diseases in 831 (4.5%) patients. Electrophysiological disorders and valvular heart diseases were more frequent in the females than in the males (Table 1). In addition, the relative frequency in the females was higher than that in the males with respect to congenital heart disease, heart failure, hypertension, and pulmonary vascular diseases (Table 1).
Table 1.
Main diagnoses of cardiovascular diseases in both sexes hospitalized in the East Azerbaijan Province in 2006–2007*
| Gender | P value | Total n=18324 | ||
|---|---|---|---|---|
|
|
|
|||
| Female (n=7960) | Male (n=10364) | |||
|
|
|
|
|
|
| Ischemic heart diseases | 4867 (61.1) | 7681 (74.1) | < 0.001 | 12548 (68.4) |
| Valvular heart diseases | 509 (6.4) | 322 (3.1) | < 0.001 | 831 (4.5) |
| Congenital heart diseases | 279 (3.5) | 294 (2.8) | 0.011 | 573 (3.1) |
| Heart failure | 311 (3.9) | 355 (3.4) | 0.092 | 666 (3.6) |
| Hypertension | 272 (3.4) | 165 (1.6) | < 0.001 | 437 (2.4) |
| Pulmonary vascular diseases | 113 (1.4) | 121 (1.2) | 0.150 | 234 (1.3) |
| Pericardial, myocardial and endocardial diseases | 101 (1.3) | 190 (1.8) | 0.003 | 291 (1.6) |
| Electrophysiological disorders | 647 (8.2) | 543 (5.3) | < 0.001 | 1190 (6.5) |
| Vascular disorders | 60 (0.8) | 49 (0.5) | 0.019 | 109 (0.6) |
| Other | 737 (9.3) | 586 (5.7) | < 0.001 | 1323 (7.2) |
Data are presented as n (%)
In the present study, the medical records of patients with cerebrovascular diseases were not assessed.
The extracted descriptive statistics of the different demographic and clinical variables are summarized in Tables 1–4.
Table 4.
Type of interventional procedures in the patients hospitalized with cardiovascular diseases in the East Azerbaijan Province in 2006–2007*
| Sex | P value | Total (n=2564) | ||
|---|---|---|---|---|
|
| ||||
| Female (n=989) | Male (n=1575) | |||
|
|
|
|||
| Angioplasty | 452 (45.7) | 861 (54.7) | < 0.001 | 1313 (51.2) |
| Pacemaker implantation | 199 (20.1) | 215 (13.7) | < 0.001 | 414 (16.1) |
| Isolated valvuloplasty | 144 (14.6) | 130 (8.3) | < 0.001 | 274 (10.4) |
| Angioplasty and valvuloplasty | 178 (18.0) | 348 (22.1) | 0.014 | 526 (20.5) |
| Radiofrequency ablation | 7 (0.7) | 6 (0.4) | 0.396 | 13 (0.5) |
| Implantation of cardioverter defibrillator | 9 (0.9) | 14 (0.9) | 0.956 | 23 (0.9) |
| Other | 0 | 1 (0.06) | 1.000 | 1 (0.04) |
Data are presented as n (%)
The findings of the current study revealed the frequency of the risk factors in the patients as follows: cigarette smoking (47.5%); hypertension (66.95); DM (35.9); alcohol consumption (4.3%); opium abuse (7.0%); history of cerebrovascular accident (16.4%); renal disease (13.4%); and family history of cardiovascular diseases in the first-degree relatives of the patients (24.2%).
All of the hospitalized patients underwent medical therapy during their hospital stay; however, 79.23% (14519/18324) received only medical therapy, 6.28% (1151/18324) underwent different surgical procedures (Table 3), and 13.99% (2564/18324) received cardiovascular interventional therapy (Table 4). Ninety (0.49%) patients experienced both surgical and interventional therapy.
Table 3.
Type of surgical procedures in the patients hospitalized with cardiovascular diseases in the East Azerbaijan Province in 2006–2007*
| Sex | P value | Total (n=1151) | ||
|---|---|---|---|---|
|
|
|
|||
| Female (n=371) | Male (n=780) | |||
|
|
|
|
|
|
| CABG | 164 (44.2) | 596 (76.4) | < 0.001 | 760 (66.0) |
| Valve surgery | 61 (16.4) | 54 (6.9) | < 0.001 | 115 (10.0) |
| CABG + Valve surgery | 10 (2.7) | 12 (1.5) | 0.267 | 22 (1.9) |
| Congenital | 104 (28.0) | 93 (11.9) | < 0.001 | 197 (17.1) |
| Other | 32 (8.6) | 25 (3.2) | < 0.001 | 57 (4.9) |
Data are presented as n (%)
CABG, Coronary artery bypass graft surgery
In this study, the in-hospital mortality rate was 1.57% (287/18324), including 147 (1.76%) females and 140 (1.42%) males (Chi-square = 6.863, p value = 0.009). In the patients who underwent cardiac surgery, the in-hospital mortality rate was 1.91% (1.54% in the males and 2.69% in the females). The in-hospital mortality rate of cardiovascular interventional therapy in our study was 1.44% (1.42% in the males and 1.46% in the females).
Discussion
Cardiovascular diseases claim 16.7 million lives annually, contributing to 29.2% of the total global deaths according to the World Health Organization Report 2003. By 2010, cardiovascular diseases had been the most important cause of death in developing countries.7 Moreover, cardiovascular diseases accounted for 34.3% (831.272) of all 2.426.264 deaths in 2006, or one of every 2.9 deaths in the United States.8 In Iran, cardiovascular diseases were responsible for 38% of the deaths in 19989 and 39.1% in 2004–2005.10 In the East Azerbaijan Province, cardiovascular diseases and cancer accounted for 58.9% (41.3% cardiovascular diseases and 17.6% cancer) of all deaths in 2003.11
Hospitalized cardiovascular disease patients are at risk of further mortality. In the East Azerbaijan Province in 2006, diagnosis of cardiovascular diseases accounted for 11.47% of the hospitalizations and 19.53% of the in-hospital deaths that occurred in these patients. In addition, the total mortality rate in all the hospitalized patients in the East Azerbaijan Province was 1.44% (4844/335364) in 2006; while in our study, the mortality rate in the hospitalized cardiovascular disease patients was 1.57%.
The relative frequency of cardiovascular diseases in the males in our study was higher than that in the females (56.6% vs. 43.4%). Similar to our findings, in the Lloyd study8 in the United States in 2006, 50.7% of the hospitalized patients were male and 49.3% were female.
De la Hera et al.,12 in Spain in 2004, presented a report of the hospital registry of patients with myocardial infarction in which the mean age of the patients was 66.5 years (45.6% older than 70 years) and the females represented 29.1% of the patient population. In our study, the mean age was 59 and 62 years in the males and females, respectively, for all cardiovascular diseases (Two thirds of the patients suffered from ischemic heart diseases). In our study, in the subgroup of patients with ischemic heart diseases, the females represented 38.8% of the patients (Table 1). The mean age at hospitalization seems to be slightly lower in our study than in the De la Hera et al. study, while the percentage of the female population affected by ischemic heart diseases in our survey is higher than that in the De la Hera et al. study.
Our study revealed that the females, hospitalized due to cardiovascular diseases, had a higher in-hospital mortality rate (1.76%) than their male counterparts (1.42%). In the Lloyd-Jones study,8 the mortality rate among the hospitalized patients with cardiovascular diseases in the United States was 1.42% and 1.28% in the females and males, respectively, in 2006.
De la Hera et al.12 reported the frequency of risk factors in patients hospitalized with myocardial infarction as follows: 63% smoking; 43% arterial hypertension; and 22.3% DM. The frequency of cigarette smoking (47.5%) was lower in our study than that in the De la Hera et al. study, whereas the frequencies of hypertension (66.9%) and DM (33.9%) were higher in our study.
In the Azarasa study,13 carried out in northwest Iran in 2009, a total of 600 patients scheduled for cardiac surgery were evaluated in a tertiary referral educational hospital, and the frequency of the risk factors was as follows: cigarette smoking (42.1%); opium abuse (12.0%); and alcohol consumption (8.1%).
Comparison of the frequencies of the cardiovascular risk factors between the general population of the East Azerbaijan Province and the cardiovascular disease patients hospitalized in the East Azerbaijan Province hospitals revealed that the prevalence of the risk factors was two to five times higher in the latter. For instance, Sayf Farshad et al.11 reported the percentages of hypertension and smoking to be 38.8% and 14.9%, respectively, in adults aged between 15 and 64 years in the East Azerbaijan Province in 2003; while in our study, 66.9% of the patients were cigarette smokers and 47.5% suffered from hypertension. Additionally, according to the Larijani et al. and Esteghamati et al.14 studies, the frequency of DM in different provinces of Iran in the general population (adults) was about 7% to 16.3%, as opposed to 35.9% in our study.
Our study confirmed the results of some studies previously performed in Iran9–11 and other countries.15–18 Chiming in with some previous surveys, in our study the most important risk factors were smoking, alcohol consumption, and DM. Furthermore, sex distribution, pattern of diagnosis, and treatment modalities were not significantly different from those in Western populations.
Conclusion
In the northwest of Iran and in the East Azerbaijan Province, the age at hospitalization due to cardiovascular diseases is slightly lower than that in Western countries. Most of the cardiovascular risk factors as well as the pattern of diagnosis and treatment modalities were similar to those in other western countries.
Table 2.
Relative frequency of the risk factors in the hospitalized patients with cardiovascular diseases in the East Azerbaijan Province in 2006–2007*
| Female (n=7960) | Male (n=10364) | P value | Total (n=18324) | |
|---|---|---|---|---|
|
|
|
|
|
|
| Smoking | 1433 (18.0) | 6581 (63.5) | < 0.001 | 8014 (43.7) |
| Hypertension | 5938 (74.6) | 6260 (60.4) | < 0.001 | 12198 (66.6) |
| Diabetes mellitus | 3319 (41.7) | 3223 (31.1) | < 0.001 | 6542 (35.7) |
| Family history of cardiac diseases | 1934 (24.3) | 2498 (24.1) | 0.775 | 4432 (24.2) |
| Alcohol consumption | 56 (0.7) | 767 (7.4) | < 0.001 | 823 (4.5) |
| Opium abuse | 159 (2.0) | 1150 (11.1) | < 0.001 | 1309 (7.1) |
| History of cerebrovascular accident | 1425 (17.9) | 1586 (15.3) | < 0.001 | 3011 (16.4) |
| History of renal disease | 947 (11.9) | 1492 (14.4) | < 0.001 | 2439 (13.3) |
Data are presented as n (%)
Acknowledgments
Many special thanks are due to the trained staff in all the 15 surveyed hospitals in the East Azarbaijan Province that helped us with data collection from a huge number of patients. We also express our gratitude to our dear colleagues in the Cardiovascular Research Center. This study was funded by the Cardiovascular Research Center, Tabriz University of Medical Sciences. This study was approved and supported by Tabriz University of Medical Sciences.
References
- 1.McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, Luepker RV. Recent trends in acute coronary heart disease--mortality, morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. N Engl J Med. 1996;334:884–890. doi: 10.1056/NEJM199604043341403. [DOI] [PubMed] [Google Scholar]
- 2.Clarify about coronary artery disease- Clarify registry. http://www.clarify-registry.com/download/CLARIFY_About_CAD.pdf. Coronary Artery Disease – Backgrounder – - CLARIFY registry. (4 May 2010).
- 3.Heart information center Coronary artery disease. http://www.texasheartinstitute.org/HIC/Topics/Cond/CoronaryArteryDisease.cfm. (2 May 2010).
- 4.Beyranvand MR, Emami MA, Aliasgari A, Kolahi AA. One-year outcome of patients with acute myocardial infarction. J Teh Univ Heart Ctr. 2007;4:229–232. [Google Scholar]
- 5.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2007;165:1–209. [PubMed] [Google Scholar]
- 6.DeFrances CJ, Hall MJ. 2005 National Hospital Discharge Survey. Adv Data. 2007;385:1–19. [PubMed] [Google Scholar]
- 7.Cardiovascular disease: prevention and control. Geneva: World Health Organization; 2010. ( http://www.who.int/dietphysicalactivity/publications/facts/cvd/en/. (2 May 2010) [Google Scholar]
- 8.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 9.Kimiagar SM, Ghaffarpour M, Houshiar-Rad A, Hormozdyari H, Zellipour L. Food consumption pattern in the Islamic Republic of Iran and its relation to coronary heart disease. EMHJ. 1998;4:539–547. [Google Scholar]
- 10.Khosravi A, Rao C, Naghavi M, Taylor R, Jafari N, Lopez AD. Impact of misclassification on measures of cardiovascular disease mortality in the Islamic Republic of Iran: a cross-sectional study. Bull World Health Organ. 2008;86:688–696. doi: 10.2471/BLT.07.046532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Syeffarshad M, Kousha A, Pourdowlati S, Karamouz M, Farahbakhsh M, Hakimi S, Sadeghi-Bazargani H. Cardiac risk factor analysis in East Azerbaijan, Iran. The Cardiology. 2007;3:1–4. [Google Scholar]
- 12.de la Hera JM, Barriales V, Moris C, Alvarez Tamargo JA, Rubín J, Barriales-Villa R, Sanmartín JC, Rodríguez Lambert JL, Investigadores del Projecto RIMAS Myocardial infarction registry in Asturias: the RIMAS project. Med Clin (Barc) 2004;123:169–173. doi: 10.1016/s0025-7753(04)74450-4. [DOI] [PubMed] [Google Scholar]
- 13.Azarasa M, Azarfarin R, Changizi A, Alizadehasl A. Substance use among Iranian cardiac surgery patients and its effects on short-term outcome. Anesth Analg. 2009;109:1553–1559. doi: 10.1213/ANE.0b013e3181b76371. [DOI] [PubMed] [Google Scholar]
- 14.Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, Safaie A, Forouzanfar M, Gregg EW. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: national survey of risk factors for non-communicable diseases of Iran. Diabetes Care. 2008;31:96–98. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 15.Hu FB, Stampfer MJ, Manson JE, Grodstein F, Colditz GA, Speizer FE, Willett WC. Trends in the incidence of coronary heart disease and changes in diet and lifestyle in women. N Engl J Med. 2000;343:530–537. doi: 10.1056/NEJM200008243430802. [DOI] [PubMed] [Google Scholar]
- 16.Kristensen PL, Wedderkopp N, Møller NC, Andersen LB, Bai CN, Froberg K. Tracking and prevalence of cardiovascular disease risk factors across socio-economic classes: a longitudinal substudy of the European Youth Heart Study. BMC Public Health. 2006;6:1–9. doi: 10.1186/1471-2458-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ulmer H, Kelleher C, Diem G, Concin H. Long-term tracking of cardiovascular risk factors among men and women in a large population-based health system: the Vorarlberg Health Monitoring & Promotion Programme. Eur Heart J. 2003;24:1004–1013. doi: 10.1016/s0195-668x(03)00170-2. [DOI] [PubMed] [Google Scholar]
- 18.Lawlor DA, Harro M, Wedderkopp N, Andersen LB, Sardinha LB, Riddoch CJ, Page AS, Anderssen SA, Froberg K, Stansbie D, Davey Smith G. Association of socioeconomic position with insulin resistance among children from Denmark, Estonia, and Portugal: cross sectional study. BMJ. 2005;331:183. doi: 10.1136/bmj.331.7510.183. [DOI] [PMC free article] [PubMed] [Google Scholar]