Abstract
Isolated bilateral internal iliac artery (IIA) aneurysm is a rare and potentially lethal disease. Endovascular repair of this disorder is a matter of debate. A symptomatic 68-year-old male presented with severe pelvic pains. Computed tomography revealed a leaking 46-mm aneurysm in the right IIA, a 27-mm aneurysm in the left IIA, and ectatic changes at a diameter of 31 mm in the right common iliac artery (CIA). Due to lower rates of morbidity and mortality, an endovascular approach was chosen instead of open surgical repair. However, due to anatomical constraints, an endograft had to be implanted in a healthy aorta in order to support an iliac branch endograft in the left CIA. Subsequently, following coil embolization of the left IIA, an iliac stent graft was extended to the right external iliac artery (EIA). Two-year follow-up CT imaging showed complete exclusion of all the aneurysms and patency of the pelvic visceral arteries. The patient is currently asymptomatic.
Endovascular repair of bilateral isolated IIAs can be a feasible treatment option. However, due to limited availability of sizes in iliac branch devices currently on the market, a main body device is sometimes required to be deployed in a healthy aorta for additional endograft support.
Keywords: Iliac aneurysm, Iliac artery, Treatment outcome
Introduction
The incidence of isolated iliac aneurysms is approximately 2%.1 A small number of case reports have described bilateral isolated internal iliac artery (IIA) aneurysms. Isolated IIA aneurysms account for approximately 0.3–0.4% of all intra-abdominal aneurysms.2 Isolated IIA aneurysms are typically asymptomatic, and 29–73% of isolated IIA aneurysms are asymptomatic at diagnosis. Mortality following isolated IIA aneurysm rupture ranges from 50–100%,3–5 and it is often due to delayed diagnosis and difficulties associated with intraoperative management.3, 4
Treatments can be categorized into open surgical and endovascular. The former includes techniques such as ligation, excision, and endoaneurysmorrhaphy, while the latter includes treatments such as coil embolization and endoluminal stenting. In this case report, we will present the case of endovascular repair of bilateral isolated IIA aneurysm with an iliac branched stent-graft.
Case Report
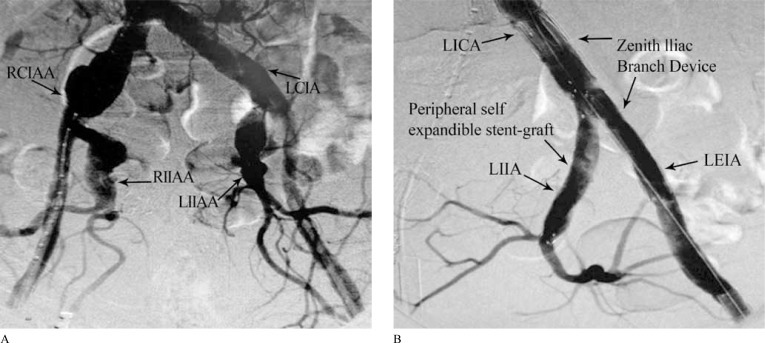
A 68-year-old male presented with severe pelvic pains. The patient had stable coronary artery disease (with a history of coronary artery bypass), severe left ventricular dysfunction (ejection fraction = 20%), hypertension, and hyperlipidemia. A computed tomography scan revealed a right IIA with a 46-mm aneurysm, a left IIA with a 27-mm aneurysm, and an ectatic right common iliac artery (CIA) (31 mm in diameter). The abdominal aorta (24 mm in diameter) and external iliac arteries (8.5 mm in diameter) were all healthy (Figure 1A).
Figure 1.
A) Preoperative angiogram, demonstrating large isolated internal iliac artery aneurysms bilaterally; B) Postoperative angiogram, demonstrating exclusion of the left internal iliac artery aneurysm following deployment of a branched endograft and extension to the level of left obturator artery
RCIAA, Right common iliac artery aneurysm; LCIA, Left common iliac artery; RIIAA, Right internal iliac artery aneurysm; LIIAA, Left internal iliac artery aneurysm; LEIA, Left external iliac artery; LIIA, Left internal iliac artery; LEIA, Left external iliac artery
The patient was considered high risk for open surgical repair, and an endovascular solution was developed.
The following was implemented via the femoral access. The right IIA aneurysm was embolized using three Cook Tornado embolization coils with a 10-mm tapering diameter (Cook Medical Inc., Bloomington, Indiana). A Zenith Iliac Branch endograft (ZBIS-12-45-41; Cook Medical Inc.) was deployed at the level of the left iliac bifurcation, and a Fluency Plus (Bard Peripheral Vascular, Inc., Tempe, Arizona) peripheral covered stent (9 × 80mm) was deployed in the left IIA (Figure 1B). Finally, a Zenith Flex main body endograft (TFFB-26-96-ZT; Cook Medical Inc.) was inserted from the right CIA; the main body graft was extended into the Zenith Iliac Branch endograft by an iliac leg extension (TFLE-16-56- ZT; Cook Medical, Inc.) and also extended into the right external iliac artery by another iliac leg extension (TFLE-12-107-ZT; Cook Medical, Inc). The procedure lasted for one hour forty-five minutes, and 300 cc of contrast dye was used. The patient was discharged 72 hours post-procedure.
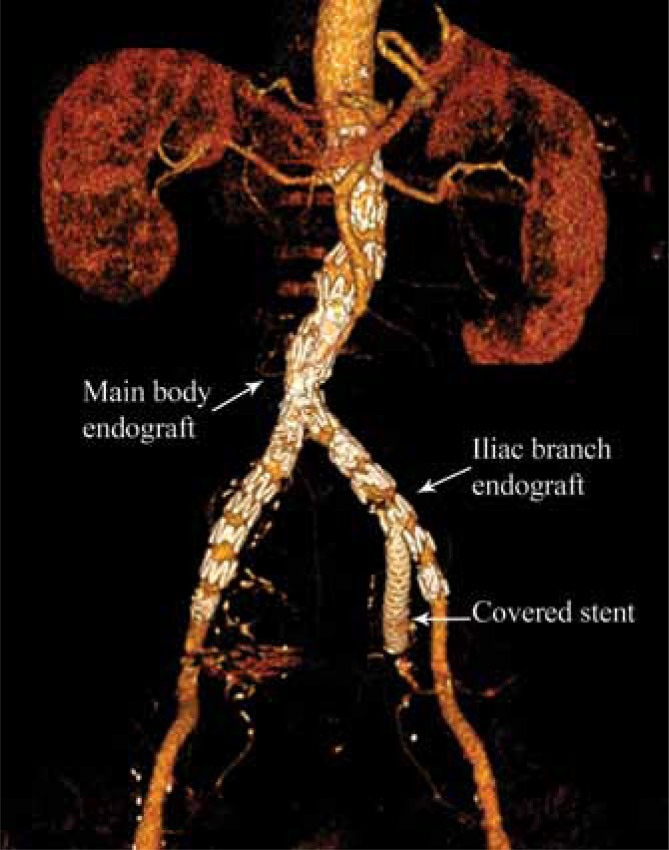
Two years after the procedure, computed tomography angiography showed complete exclusion of the bilateral isolated IIA aneurysms, patency of the pelvic arteries, and no signs of endoleaks or device migration (Figure 2).
Figure 2.
Two-year post-implant computed tomography angiography, showing right and left internal iliac artery aneurysms successfully excluded with a Cook Zenith Iliac Branch Device
Discussion
To the authors’ knowledge, this is the first report of endovascular treatment of symptomatic, bilateral isolated aneurysms using an iliac branch endograft.
For this patient, two other treatment options were considered but dismissed: 1) bilateral IIA embolization and monitoring of the right CIA aneurysm was dismissed because of potential comorbidities (e.g., buttock necrosis/claudication, ischemic colitis, impotence, and neurologic deficits); and 2) embolization of the right IIA and placement of a bifurcated main body endograft in the aortic artery to be extended to the external iliac artery on the right and thereafter to be extended to the iliac bifurcation on the left, with the left IIA monitoring, was dismissed for several reasons: a) the left IIA aneurysm would inevitably need treatment; b) subsequent intervention could not include embolization (because the right IIA would already be embolized);c) an iliac bifurcated device could not eventually be placed on the left CIA because the internal iliac covered bridging stent could not be inserted from the right CIA and up and over through the main body bifurcation (alternatively, the covered bridging stent could be inserted through the brachial access, but documented complication rates are as high as 7 – 11%);6–8 and d) the patient preferred to undergo one treatment instead of several.
While our solution, which involved placement of a main body endograft in a healthy aorta, was not ideal, we saw no other viable option. An iliac branch endograft deployed in the CIA, without the support of a main body device in the aorta, would certainly migrate due to the large proximal diameter of the CIA and the small proximal diameter of the iliac branch device.
Conclusion
In the future, the preferred treatment for isolated IIA aneurysms may be to implant a branched endograft at the level of the iliac bifurcation without the need for a main body endograft in the aorta. However, current endograft designs do not allow for this. As more physicians choose endovascular solutions, it is our hope that medical device manufacturers will compete to develop endografts with branched technology to treat isolated IIA aneurysms.
Acknowledgments
The authors would like to thank Salar Samimi for technical and research support. There are no conflicts of interest for any of the authors. There has been no financial support either for the procedure or for the preparation of this manuscript.
References
- 1.Richardson JW, Greenfield LJ. Natural history and management of iliac aneurysms. J VascSurg. 1988;8:165–171. [PubMed] [Google Scholar]
- 2.Brunkwall J, Hauksson H, Bengtsson H, Bergqvist D, Takolander R, Bergentz SE. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg. 1989;10:381–384. doi: 10.1067/mva.1989.13733. [DOI] [PubMed] [Google Scholar]
- 3.Verta MJ, Jr, Janevicius RV. Isolated hypogastric artery aneurysms. J Cardiovasc Surg (Torino) 1982;23:432–434. [PubMed] [Google Scholar]
- 4.Lozano P, Julià J, Corominas C, Gomez F. Ruptured aneurysms of the internal iliac artery. Report of two cases. J Cardiovasc Surg (Torino) 1995;36:591–594. [PubMed] [Google Scholar]
- 5.Lee WA, O›Dorisio J, Wolf YG, Hill BB, Fogarty TJ, Zarins CK. Outcome after unilateral hypogastric artery occlusion during endovascular aneurysm repair. J Vasc Surg. 2001;33:921–926. doi: 10.1067/mva.2001.114999. [DOI] [PubMed] [Google Scholar]
- 6.Grollman JH, Jr, Marcus R. Transbrachial arteriography: techniques and complications. Cardiovasc Intervent Radiol. 1988;11:32–35. doi: 10.1007/BF02577022. [DOI] [PubMed] [Google Scholar]
- 7.Watkinson AF, Hartnell GG. Complications of direct brachial artery puncture for arteriography: a comparison of techniques. Clin Radiol. 1991;44:189–191. doi: 10.1016/s0009-9260(05)80868-2. [DOI] [PubMed] [Google Scholar]
- 8.Heenan SD, Grubnic S, Buckenham TM, Belli AM. Transbrachial arteriography: indications and complications. Clin Radiol. 1996;51:205–209. doi: 10.1016/s0009-9260(96)80324-2. [DOI] [PubMed] [Google Scholar]