Abstract
Introduction
There is a critical need for public health interventions to support the independence of older adults as the world’s population ages. Health smart homes (HSH) and home-based consumer health (HCH) technologies may play a role in these interventions.
Methods
We conducted a systematic review of HSH and HCH literature from indexed repositories for health care and technology disciplines (e.g., MEDLINE, CINAHL, and IEEE Xplore) and classified included studies according to an evidence-based public health (EBPH) typology.
Results
One thousand, six hundred and thirty nine candidate articles were identified. Thirty-one studies from the years 1998–2011 were included. Twenty-one included studies were classified as emerging, 10 as promising and 3 as effective (first tier).
Conclusion
The majority of included studies were published in the period beginning in the year 2005. All 3 effective (first tier) studies and 9 of 10 of promising studies were published during this period. Almost all studies included an activity sensing component and most of these used passive infrared motion sensors. The three effective (first tier) studies all used a multicomponent technology approach that included activity sensing, reminders and other technologies tailored to individual preferences. Future research should explore the use of technology for self-management of health by older adults, social support and self-reported health measures incorporated into personal health records, electronic medical records, and community health registries.
Keywords: Health Smart Homes, Evidence-Based Public Health, Aging in Place, Independent Aging, STARE-HI
1. Introduction
As the worldwide population of older adults grows, the economic need for population-based interventions to support their needs has been widely recognized[1]. The Institute of Medicine has declared chronic disease a public health crisis[2] and older adults bear a disproportionate burden of chronic illness among the larger population. To enable older adults to maintain their own wellness as a resource for independent living, there is a need to develop comprehensive health monitoring and management systems to help maintain function and independence[2] and to identify methods that can predict and prevent declines in community health status[3]. Health smart homes (HSH) and home-based consumer health (HCH) technologies are potential solutions to support older adults to age in place – the ability to live in a residence of their choice without moving as their needs for health care services change[4]. In this review, HSH are defined as residential settings that have technology components, such as activity sensors[5], embedded in the environment to enable passive monitoring. HCH are defined as other health technologies, such as a telehealth medication management device[6], that are not necessarily embedded in the environment but designed for use in the home by older adults and their families.
Modern public health practice relies on population-based, evidence-based and prevention-oriented interventions at individual, community and system levels[7] whereas gerontological nursing practice aims to maximize independence and minimize disability of older adults across the continuum of care[8]. HSH/HCH may form part of a public health strategy to maximize independence and minimize disability in older adults. Data collected through prevention and self-management efforts on the part of older adults and their families through HSH/HCH technologies have the potential to integrate with clinical and public health information systems to provide support across the continuum of care. However, the needs of older adults frequently blur the lines between disease prevention and health promotion as defined by previous eras of public health practice[3,9,10], with some conditions being risk factors for others[10]. In addition, older adults[5], family caregivers[11], clinicians[12], designers[12], public health practitioners[13] and policy makers[13] have different needs when it comes to technology and information. For instance, where an older adult might perceive a need for reminders to remember events [5], a family caregiver might perceive a need for information about a relative’s condition[11] and policy makers might perceive a need for cost and effectiveness information about technology[13]. In the context of health informatics and public health projects, assessment and understanding of all stakeholder needs is an important and accepted practice[14].
HSH/HCH research has been conducted in both health services and technology disciplines and scientific findings have been published in different literature repositories that do not always overlap in their indexing. For example, the ACM Digital Library and MEDLINE repositories index published works from two largely distinct disciplines, specifically, those of technology and health sciences research. As a result, HSH/HCH research has not been characterized in a way that can easily inform population-based interventions that aim to maximize independence and minimize disability in older adults. This fragmentation of reported evidence represents a knowledge gap concerning what research has been done and communication barriers for knowledge translation to relevant stakeholders.
To understand how HSH/HCH can inform population-based interventions to maximize independence and minimize disability in older adults, existing research must be framed as evidence in a way that can be understood by public health practitioners, policy makers, designers, evaluators and other stakeholders[15]. The aim of this study is to characterize the state of HSH/HCH research to inform population-based interventions that support aging in place through systematic review and classification of the scientific literature using health informatics evaluation guidelines[16–18], informatics study types[19] and an evidence-based public health (EBPH) typology[20,21]. In addition, we identify the stakeholders involved in each included study.
2. Methods
2.1. Search Strategy
The search methodology was developed and refined by three researchers (BR, GD, HT) who conduct HSH/HCH and health informatics research. The search methodology included searches of MEDLINE, CINAHL, SciVerse ScienceDirect, the ACM Digital Library and IEEE Xplore databases to provide comprehensive coverage of indexed literature from many disciplines. As the term “smart home” is not well-defined, our search terms also include “e-health”, “health monitoring”, “telemedicine”, “telehealth”, “home-based health technology”, “gerontechnology” and “gerotechnology” in combination with “older adult”, “aging”, “ageing”, “elderly”, “community-dwelling” and “senior”. Searches were conducted for the date range January 1980 to October 2011.
Inclusion/exclusion criteria were developed by two researchers (BR, GD). We did not exclude any studies based on study design or methodology because we wanted to capture the range of all studies that would show possible evidence in the topic area[22]. Since “aging in place” is not uniformly operationalized in the literature, our review focused on support of independence and prevention of health events that threaten the independence of older adults whether these concepts were operationalized as independent variables or not. Inclusion criteria included English language studies of technologies to support older adults in residential settings; involved any participants that were 60 years of age or older; focused on support of independence (for example: medication reminder systems) or prevention of health events that threaten independence (for example: systems to monitor activity levels); enabled collection of data for health monitoring or communication.
Exclusion criteria included those studies focused on specific diseases or conditions because older adults often cope with multiple morbidities; about technology strictly for delivery of clinical care services (for example: telemedicine case management of patients with diabetes); focused on acute care or short-term acute care follow-up (for example: remote monitoring of homebound patients with congestive heart failure); about everyday assistive technologies (for example: canes, walkers, and shower benches); about surveillance technologies strictly for home security (for example: camera systems solely used to detect intruders); concerned with “environmentally-friendly” smart homes with features designed for power-efficiency and convenience (for example: sensing systems solely used to monitor energy consumption); about development tools and environments for programmers and engineers, proposed models, architectures, frameworks, computational approaches, algorithms, communication protocols, ontologies, data standards, methods for data storage, gateway technologies, middleware, wearable sensors because our focus was on technologies in the environment not on a person, evaluation methods, interface design because it is a method not a technology, sensor design refinements, and/or issues in technical design.
2.2. Data Abstraction
The Statement on Reporting of Evaluation studies in Health Informatics (STARE-HI) provides guidelines for reporting studies of informatics applications[16–18]. The STARE-HI guidelines were implemented in a web-based tool for data management during article review and analysis. We assessed each included study to identify reported STARE-HI items to set a baseline of completeness of reporting for current and future research in this topic area. In particular, we were interested in comparing items related to ethical concerns to findings from prior STARE-HI research[16,17].
The evidence-based public health (EBPH) typology describes etiologic evidence (or type 1), intervention evidence (or type 2), contextual (or type 3) evidence. Etiologic evidence relates to problem identification; in the case of this review, the problem is the need to support aging in place for older adults. Intervention evidence is classified according to emerging, promising, effective (first tier) and effective (second tier) categories[20,21]. Contextual evidence explains how specific interventions can be implemented in different settings[20,21] for transferability[23]. Friedman and Wyatt define a hierarchy of study types along a flexible continuum of technology development that are identified as needs assessment, design validation, structure validation, usability test, laboratory function, laboratory user effect, field function, field user effect and problem impact[19].
Classification criteria based on the EBPH categories and informatics study types (See Table I) were developed using an approach informed by one used to develop criteria in review of public health strategies for prevention of childhood obesity[24]. Emerging technologies are those that have undergone validity testing with at least one older adult participant; promising technologies are those that have undergone further feasibility testing with 10 or more study participants; effective (first tier) technologies are those ready for evaluation with larger populations in different settings; effective (second tier) technologies are those that are ready for large-scale dissemination and implementation (see Table I). In addition, we determined the presence or absence of health-related smart home technology types[25] for each study to determine areas for future research.
Table I.
Classification criteria for HSH/HCH evidence
| Required Criteria and Details |
|---|
EMERGING
|
PROMISING
|
EFFECTIVE (FIRST TIER)
|
EFFECTIVE (SECOND TIER)
|
3. Results
Thirty-one publications from the years 1998–2011 were included in the review. Interestingly, no publications from the years 2003 and 2004 met the criteria for inclusion. The included studies are not a comprehensive list of all smart homes and home-based consumer health technologies (HSH/HCH) worldwide but a list of those studies from the scientific literature that met the inclusion criteria of this review. For summaries of the included studies, see Table II (sample size and study design), Table III (EBPH types, HSH/HCH technology types and IRB/consent reporting) and Table IV (descriptions and results for effective and promising studies).
Table II.
Sample size and study design for included studies
| AUTHOR | SAMPLE SIZE | STUDY DESIGN |
|---|---|---|
| Kawarada et al. (1998)[35] | n=2 (1 older adult) ECG in bathtub n=2 (1 older adult) weight in lavatory n=5 (4 older adults) ECG in bed |
Technology Trial |
| Dario et al. (1999)[36] | n=13 (older adults) microwave task n=35 (not older adults) entire system n=16 (not older adults) interface |
Technology Trial, Descriptive Study |
| Glascock & Kutzik (2000)[37] | n=1 (older adult) | Technology Trial |
| Kawarada et al. (2000)[38] | n=2 (1 older adult) ECG in bathtub n=2 (1 older adult) weight in lavatory n=5 (4 older adults) ECG in bed n=6 (older adults) continuous monitoring |
Technology Trial |
| Sixsmith (2000)[39] | n=22 (older adults) + n=20 (family members) | One-Group Pretest-Posttest |
| Ogawa et al. (2002)[40] | n=2 (older adults) | Technology Trial |
| Ohta et al. (2002)[41] | n=8 (older adults) | Technology Trial, Descriptive Study |
| Chan et al. (2005)[42] | n=4 (older adults) | Technology Trial |
| Kelly (2005)[43] | n=1700 (older adults) | Historical Controlled Trial |
| Alwan et al. (2006)[44] | n=25 (older adults) + n=26 (family members) | One-Group Pretest-Posttest |
| Fujimura et al. (2007)[45] | n=8 (older adults) + n=7 (family members) | Descriptive Study |
| Glascock & Kutzik 2007)[46] | n=2 (older adults) case studies (out of three facilities with n=29, n=6, n=20) | Descriptive Study |
| Tamura et al. (2007)[47] | n=18 (11 older adults) | Technology Trial |
| Tomita et al. (2007)[48] | n=78 (older adults) (intervention=34, control=44) | Randomized Controlled Trial |
| Brownsell et al. (2008)[49] | n=52 (older adults) (intervention=24, control=28) | Non-Equivalent Control Group Pretest-Posttest |
| Demiris et al. (2008)[50] | n=9 (older adults) | One-Group Posttest Repeated Measures |
| Diermaier et al. (2008)[51] | n=2 (older adults) | Technology Trial |
| Rahal et al. (2008)[52] | n=14 (6 older adults) | Technology Trial |
| Rantz et al. (2008)[53] | n=2 (older adults) case studies (out of total n=34) | Descriptive Study |
| Mahoney et al. (2009)[54] | n=13 (older adults) + n=4 (family members) + 9 (staff) focus groups n=10 (older adults) + n=10 (family members) + 9 (staff) pilot |
Technology Trial, Descriptive Study, One-Group Pretest-Posttest |
| Noury et al. (2009)[55] | n=12 (older adults) | Technology Trial, Descriptive Study |
| Otjacques et al. (2009)[56] | n=40 (older adults) interviews n=19 (older adults) technology trial |
Descriptive Study, Technology Trial |
| Rantz et al. (2009)[57] | n=2 (older adults) case studies (out of total n=39) | Descriptive Study |
| Skubic et al. (2009)[58] | n=34 (older adults) | Descriptive Study |
| Junnila et al. (2010)[59] | n=2 (older adults) | Technology Trial |
| Kim et al. (2010)[60] | n=110 (older adults) surveys out of 365 issued n=31 (older adults) interviews |
Descriptive Study |
| Riche et al. (2010)[61] | n=14 (older adults) interviews n=2 (older adults) technology trial |
Descriptive Study, Technology Trial |
| Etchemendy et al. (2011)[62] | n=17 (15 older adults) | One-Group Pretest-Posttest Repeated Measures |
| Kaye et al. (2011)[63] | n=233 (older adults) | Longitudinal Community Cohort Study |
| Lee et al. (2011)[64] | n=2 (older adults) | Descriptive Study |
| van Hoof et al. (2011)[65] | n=18 (older adults) baseline n=12 (older adults) exit |
One-Group Pretest-Posttest |
Table III.
EBPH category and HSH/HCH technology type for included studies
| AUTHOR | EBPH CATEGORY | TECHNOLOGY TYPE* | IRB/CONSENT |
|---|---|---|---|
| Kawarada (1998)[35] | Emerging | Phys, Fx | - |
| Dario (1999)[36] | Emerging | Cog/Sen | - |
| Glascock (2000)[37] | Emerging | Fx | ✓ |
| Kawarada (2000)[38] | Emerging | Phys, Fx | - |
| Sixsmith (2000)[39] | Promising | Fx | - |
| Ogawa (2002)[40] | Emerging | Phys, Fx, Saf | - |
| Ohta (2002)[41] | Emerging | Fx | - |
| Chan (2005)[42] | Emerging | Fx | ✓ |
| Kelly (2005)[43] | Effective (1st) | Fx, Saf, Sec, Cog/Sen | - |
| Alwan (2006)[44] | Promising | Phys, Fx, Saf | ✓ |
| Fujimura (2007)[45] | Emerging | Fx, Soc | - |
| Glascock (2007)[46] | Promising | Fx | - |
| Tamura (2007)[47] | Emerging | Phys, Fx | ✓ |
| Tomita (2007)[48] | Effective (1st) | Fx, Sec, Cog/Sen | ✓ |
| Brownsell (2008)[49] | Effective (1st) | Fx, Saf, Sec, Cog/Sen | ✓ |
| Demiris (2008)[50] | Emerging | Phys, Fx, Saf | ✓ |
| Diermaier (2008)[51] | Emerging | Fx | - |
| Rahal (2008)[52] | Emerging | Fx | - |
| Rantz (2008)[53] | Promising | Phys, Fx, Saf | ✓ |
| Mahoney (2009)[54] | Promising | Fx, Saf | ✓ |
| Noury (2009)[55] | Emerging | Fx | ✓ |
| Otjacques (2009)[56] | Emerging | Cog/Sen | - |
| Rantz (2009)[57] | Promising | Phys, Fx, Saf | ✓ |
| Skubic (2009)[58] | Promising | Phys, Fx, Saf | ✓ |
| Junnila (2010)[59] | Emerging | Phys, Fx, Soc | ✓ |
| Kim (2010)[60] | Promising | Fx, Sec | - |
| Riche (2010)[61] | Emerging | FX, Soc | - |
| Etchemendy (2011)[62] | Emerging | Soc | ✓ |
| Kaye (2011)[63] | Promising | Fx | ✓ |
| Lee (2011)[64] | Emerging | Fx, Soc | - |
| van Hoof (2011)[65] | Promising | Fx, Saf, Soc, Cog/Sen | ✓ |
Technology types and their functions[25]: 1) Physiological monitoring (Phys) - collection and analysis of physiological measurement data such as vital signs; 2) Functional monitoring/Emergency detection and response (Fx) - collection and analysis of functional measurements data such as general activity level or falls; 3) Safety monitoring and assistance (Saf) - collection and analysis of environmental hazard data such as flooding and notification of floods; 4) Security monitoring and assistance (Sec) - detection of intruders and notification of identified threats; 5) Social interaction monitoring and assistance (Soc) - collection and analysis of data pertaining to social interactions and technologies that facilitate social interactions; 6) Cognitive and sensory assistance (Cog/Sen) - compensate for sensory deficits, give reminders or task instructions.
Table IV.
Descriptions and result summaries for effective (first tier) and promising studies
| EVIDENCE TYPE | STUDY DESCRIPTION | RESULTS |
|---|---|---|
|
Effective (1st) Kelly (2005)[43] |
6 year community-level implementation of an integrated activity/environment monitoring system with medication reminders (historical controlled trial) | “Mainstreamed” a successful smart home system to anyone over 60 as a preventive measure. Increased quality of life for OAs*, reduced hospital admissions, reduced length of stay in hospitals and reduced length of stay in nursing homes due to preventive measures. (1.4 per 1000 West Lothian OAs in hospital beds vs 2.74 per 1000 in Scotland overall, 30 days mean duration stay vs. 112 days in Scotland overall) |
|
Effective (1st) Tomita et al. (2007)[48] |
2 year randomized controlled trial to evaluate the effectiveness of commercial smart home technology with sensing and automation capabilities to support independent aging in older adults | Intervention group had a significant higher cognitive level after controlling for age and initial cognitive level. 80.4% of the intervention group lived at home versus 65.7% of control group at study end. 82.4% reported the computer “very important”/14.7% “somewhat important” at study end. All intervention group participants accepted a computer, sensor software, a lighting system, chimes for security and medication reminders; Types of problem were related to person, computer, ×10 products and the home. |
|
Effective (1st) Brownsell et al. (2008)[49] |
12 month non-randomized controlled trial to evaluate the effectiveness of a sensing system for activity and environmental monitoring | Intervention group participants maintained times outside the home at 5 per week and increased time outside from 3.6 to 4 hours while control reduced times outside from 5 to 4.4 and decreased from 2.6 to 2.4 hours per week. Intervention group experienced a 1% increase in feeling safe during the day and a 5% increase at night while the control group experienced a 1% decrease during the day and 3% decrease at night. Intervention experienced 10% decrease in fear of crime while the control experienced a 6% decrease. |
|
Promising Sixsmith (2000)[39] |
3 month field study of a sensing system for activity monitoring | OAs indicated a high level of satisfaction with the system, 1/3 felt more independent and nearly 1/2 said it helped them stay living at home. All but one FM** was satisfied with the system. There were a high number of false alerts and some OAs misunderstood the capabilities of the technology. |
|
Promising Alwan et al. (2006)[44] |
4 month pilot study to evaluate the pyschosocial impact of an activity monitoring system adapted to an independent retirement community | Technology did not decrease participant QOL (OAs, FMs) or increase informal caregiver strain. Mean number of hours of care rose from 5.16 to 8.10, suggesting that wellness reports prompted greater involvement by FMs in OAs lives. 2 case studies indicate that lowered activity levels and increased restlessness could have prompted preventive measures prior to hospitalization. |
|
Promising Rantz et al. (2008)[53] |
Using retrospective data analysis, demonstrated the ability to detect health status decline using a sensing system from an ongoing longitudinal study of 2+ years. | Changes in heart rate and restlessness in one case were indicators of decline in health status. Increase and decrease in restlessness during and following cardiac rehabilitation could have indicated increased/decreased pain in another case. |
|
Promising Glascock et al. (2007)[46] |
Longitudinal study of a sensing system for activity monitoring at 8 installations (1 site for 6 months) | 3 cases regarding detected falls, decreases in eating and increases in lavatory use prompted participant contact and preventive measures resulting in positive results. |
|
Promising Mahoney et al. (2009)[54] |
Pilot study implemented over 18 months (average 4 months/participant) to test a sensing system adapted to an independent retirement community setting and evaluate stakeholder perceptions | OAs and FMs felt the system addressed their needs and was not intrusive. Unexpectedly, for OAs there was a categorical drop from “strong agree” to “somewhat agree regarding feelings of security”. FMs reported slight increase in concern but decrease in time need to check on relatives. FMs suggested the ability to see the reason for “no activity” alerts. 5 of 10 FMs were willing to pay 60 USD/month. Water sensor alerts endorsed by staff. |
|
Promising Rantz et al. (2009)[57] |
Using retrospective data analysis, demonstrated the ability to detect health status decline using a sensing system from an ongoing longitudinal study of 3+ years. | In one case, an increase in bed restlessness prior to a fall could have been used to prompt assessment for an OA resident who was not feeling well. In another case, decreased activity and increased restlessness in a resident who experienced cognitive decline could have been used to raise levels of watchfulness. |
|
Promising Skubic et al. (2009)[58] |
Reported lessons learned from a 3+ year ongoing longitudinal study of a sensing system in a “living laboratory”. | Typical patterns of activity for an individual were monitored for changes. Detection of increased pulse pressure was consistent with cerebral cardiovascular incident in one case. Decreases in activity were consistent with depression in another. Changes in restlessness and bed tachypnea (breathing rate > 30bpm) were detected prior to a heart attack in another case. Changes in restlessness/tachnypea were detected before a surgery and returned to normal afterwards. |
|
Promising Kim et al. (2010)[60] |
Evaluated participant perceptions of sensor technology installed for 10 years in 4 different apartment buildings for older adults. | Participants felt comforted by sensor technology but did not think it changed the patterns of their lives. Residents often overestimated the capabilities of the technology. |
|
Promising Kaye et al. (2011)[63] |
Demonstrated feasibility of a large scale, longitudinal activity sensing project for older adults in their homes with average enrollment time of 33 months | Times/day walked past in-home sensor: 22, Mean walking speed: 61.0 cm/s, Fast walking: 96.0 cm/s, Slow walking: 36.2 cm/s, Average times out of home: 2/day for a mean of 208 minutes, Average computer use time when used: 76 minutes/day, Average days computer/use: 43% of days. 83% reported physical health problems using the online form. Over half reported at least one fall and 35% at least one trip to the hospital/ER. Oldest old were more likely to report a fall or cardiac issue versus young old. |
|
Promising van Hoof et al. (2011)[65] |
Investigated the use of ambient technologies by older adults enrolled for 8–23 months and the ability of technology to support aging in place | Participants had a greater sense of security after technology installation. One participant developed a fear of the equipment and had it removed after a year. Two participants were dissatisfied with false alerts but kept the technology for the increased feeling of safety. Some participants felt the technology was too loud. |
OA = Older adult
FM = Family Member
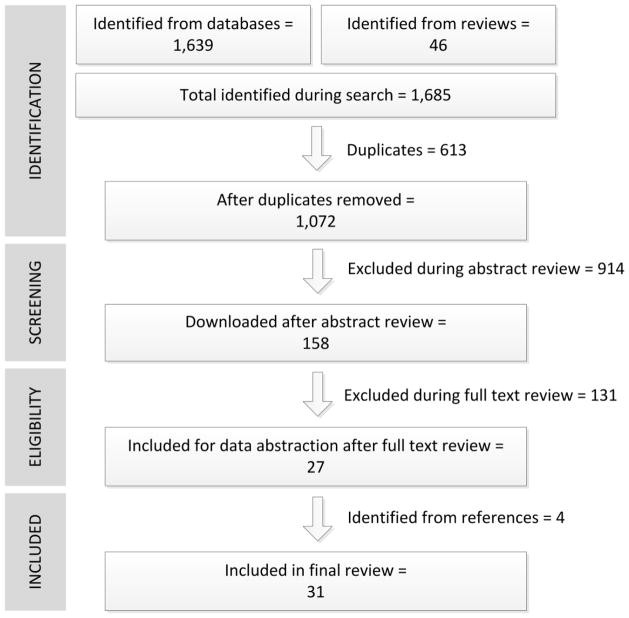
One thousand, six hundred and thirty-nine citations and abstracts were identified as potentially relevant after searching the identified databases. Forty-six additional candidate publications were identified through manual search of the reference lists of 8 literature reviews returned in the search[26–33], increasing the total to 1,685. All citations and abstracts were downloaded into a commercial reference database. After duplicate entries were removed, a total of 1,072 candidate publications remained. One researcher (BR) reviewed all abstracts, applying the inclusion/exclusion criteria. Two other researchers (SC, EM) participated in application of inclusion/exclusion criteria during full text review and data abstraction. 914 candidate publications were excluded during abstract review, thus decreasing the total to 158. Full text documents were retrieved for these 158 publications. During full text article review, 131 candidate publications were excluded, leaving a total of 27 articles for data abstraction. During data abstraction, the reference lists of included publications were reviewed for additional publications that could be included. 4 additional publications were identified for inclusion, for a final total of 31 publications. Figure 1 shows a flow chart of the search process, formatted according to PRISMA statement guidelines[34].
Figure 1.
Process flow for literature review
During full text article review and data abstraction, 2 researchers (BR, SC) independently reviewed 5 randomly selected articles from the downloaded full text results to develop a codebook for application of the STARE-HI guidelines. As a test of inter-rater reliability during data abstraction, 2 researchers (BR, EM) independently applied the STARE-HI codebook in a review of 8 randomly selected articles. Both researchers met to reconcile differences through discussion until agreement was reached about application of STARE-HI codes. Initial agreement before reconciliation was high (overall average agreement of 85% and an overall average kappa score of .069). One researcher (BR) conducted data abstraction for the remaining articles. During study classification, 2 researchers (BR, AL) independently classified all included studies according to the classification criteria (see Table I). Both researchers met to compare and reconcile differences in classifications through discussion until agreement was reached.
Included publications were closely divided between journals (n=17) and conference papers (n=14). Articles originated from 12 different countries: Austria (n=1), Canada (n=1), Finland (n=1), Italy (n=1), Luxembourg (n=1), Spain (n=1), Netherlands (n=1), Korea (n=1), United Kingdom (n=3), France (n=3), Japan (n=6), United States (n=11). The majority of included studies were strictly technology trials (n=12) or descriptive studies (n=8). Multiple publications included in this review report on the progress of the same projects over time. These projects were: TigerPlace[50,53,57,58 ], QuietCare[37,46] and Welfare Techno House[35,38,47].
3.1. Descriptive Analysis
We provide a descriptive analysis of included publications due to disparate study designs and results. Therefore, a meta-analysis of study results was not possible. We describe completeness of reporting for ethics and research items from the STARE-HI guidelines, evidence-based public health types (EBPH), types of measurements used and types of health smart home-related technology components described in each study. In addition, we summarize the outcomes, costs, theories and stakeholders reported in effective and promising studies.
3.1.1. Ethics and Research Reporting
Data abstraction using the STARE-HI guidelines enabled description of completeness of reporting regarding ethical approval, competing interests, research questions and hypotheses. Two conference[60,64] and 5 journal[37,48,54,61,65] publications explicitly reported research questions (7/31, 23%). Six of these articles were published between 2007–2011[48,54,60,61,64,65]. One conference[56] and 1 journal publication[37] explicitly reported study hypotheses (2/31, 6%). Only 1 publication contained a description of both research questions and hypothesis[37] (1/31, 3%). Eleven journal[37,42,47–50,54,58,62,63,65 ] and 5 conference articles[44,53,55,57,59] reported ethics board review and/or obtaining informed consent from study participants (16/31, 52%) (See Table III). Only 1 publication reported competing interests[65] (1/31, 3%). Interestingly, there were 2 publications about the same health monitoring technology[37,46] explicitly developed for commercial purposes but neither article reported competing interests (2/31, 6%).
3.1.2. Evidence Types
Fifty-eight percent (18/31) of included studies were classified as emerging, 32% (10/31) as promising and 10% (3/31) as effective (first tier) evidence. None of the studies were classified as effective (second tier). Prior to 2005, there were six emerging studies[35–38,40,41] and one promising study[39] (7/31, 23%). From 2005 and beyond, there were 12 emerging studies[42,45,47,50–52,55,56,59,61,62,64], 9 promising studies[44,46,53,54,57,58,60,63,65] and 3 effective (first tier) studies[43,48,49] (24/31, 77%). See Table III for the EBPH types and HSH/HCH technology types for each included study.
3.1.3. Novel Indicators
As expected at the outset of the review, “aging in place” was not measured using standardized, comparable indicators in the included studies. However, novel health indicators enabled by technology were demonstrated in individual studies. Only 4 studies, 2 effective (first tier) (Tomita et al.[48], Brownsell et al.[49]) and 2 promising (Alwan et al.[44], Kaye et al.[63]), reported the use of validated instruments of measure (for example: Mini-Mental State Examination (MMSE)[66], Falls Efficacy Scale (FES)[67] or Satisfaction With Life Scale (SWLS)[68]).
Novel health indicators from the effective (first tier) and promising studies were related to monitoring activity patterns and changes in activity patterns to detect cognitive and physical health status changes. Effective (first tier) studies described monitored activities that included fall detection[43,49], bed occupancy[43,49], motion detection[43,49], seizure detection[43] and medication reminders[43,48]. In addition, Kelly et al.[43] described system-level indicators that included decreases in delayed discharges from hospitals, reduced length of stay in nursing homes, decreases in the number of adults over 65 occupying hospital beds and lower length of stay in hospitals.
From promising studies, changes in activity levels, bed restlessness, heart rate and pulse rate were indicators for different events on a case-by-case basis[44,53,57,58]. Different cases showed: increased bed restlessness prior to a fall[57]; decreased activity levels and increased bed restlessness prior to a cognitive decline[57]; decreased bed restlessness and increased bradycardia (slow pulse rate < 30 bpm) before a cardiac event[53]; increased bed restlessness after surgery possibly caused by pain, new medication or other factors[53]; increased bed restlessness and increased bed tachypnea (breathing rate > 30 bpm) after a cardiac event heart and bypass surgery and then a return to normal after cardiac rehabilitation[58]; increased activity levels in the living room and increased bed tachypnea following knee surgery and then return to normal after recovery[58]; decreased activity levels, increased bed restlessness and increased time spent in bed prior to hospitalization for gastro-intestinal bleeding[44]; increased bed restlessness, decreased time spent in bed and increased number of bathroom visits leading up to three different admissions to a hospital emergency room[44]. Glascock and Kutzik described three cases that separately involved detection of a fall, decreases in eating and increases in lavatory use for different individuals that resulted in study participant contact and preventive care[46].
3.1.4. Technologies
Eight-seven percent (27/31) of studies had an activity sensing (Fx) component and 29% (9/31) had a physiological sensing (Phys) component (See Table III). All studies with a Phys component included an Fx component. A safety monitoring (Saf) component was included in 42% (13/31) of included studies while 13% (4/31) had security features for intruder detection (Sec). Social interactions (Soc) were supported by 23% (7/31) and 13% (4/31) implemented cognitive or sensory support (Cog/Sen) such as reminders. All promising and effective (first tier) studies included an activity sensing (Fx) component. For emerging studies not primarily concerned with activity sensing, 3% (1/31) were concerned with robotic assistance[36]; 3% (1/31) were concerned with self-assessment, recreation and integrating multiple forms of digital communication[62]; 3% (1/31) were concerned with audio/video communications[45]; 3% (1/31) were concerned with developing new ways for older adults to interact via “communication appliances”[61]; and 3% (1/31) were concerned with medication management tasks[64].
Seventy-four percent (20/27) of all studies with an activity sensing (Fx) component implemented commercially available passive infrared (PIR) sensors, including all 3 effective (first tier) studies and 9 of 10 promising studies. Minor issues with false alarms were often reported with PIR sensors, including false positives from a household fan in one case[60]. Eight publications (26%) explicitly specified single occupants as participants in studies[40–42,44,46,48,54 ], 7 (23%) described the inclusion of both single participants and couples[39,53,57–59,63,65] and the remainder did not specify whether or not couples were included. In contrast, only 3 studies raised the issue of identifying multiple occupants using PIR sensors[47,58,63]. Tamura et al.[47] and Kaye et al.[63] recognized the challenge of individual identification in 2007 and 2011, respectively. Skubic et al. reported the early development of a video sensor network that works in conjunction with PIR sensors to extract silhouettes that preserve privacy yet can distinguish between individuals[58].
3.1.5. Study Summaries
Of the three studies classified as effective (first tier), one was a randomized controlled trial (Tomita et al.[48]), one was a non-randomized controlled trial (Brownsell et al.[49]) and one was a historical controlled trial (Kelly et al.[43]). Outcome summaries for each of these studies is provided below. In addition, we describe the theories, costs and stakeholders included in the effective (first tier) and promising studies. See Table IV for a study description and results summary of each effective (first tier) and promising study.
3.1.6. Outcomes
The outcomes of the three effective (first tier) studies are summarized below. Based on their study designs, sample size and other factors described by the classification criteria in Table 1, these three studies demonstrated the strongest evidence for support of independent aging. We note that each study had limitations related to participant dropout rates[48], non-randomized comparison groups[49] and use of a historical control study design[43].
Tomita et al. reported that participants in their technology intervention group maintained physical and cognitive status versus a significant decline for participants in the control group over the 2 year study period[48]. However, there was a difference of 3.6 years of age between the intervention and control groups (72.0 vs. 75.6) attributed to drop out by 4 younger participants who chose not to take part in the study after being randomly assigned to the control group. Although almost all participants viewed the system as beneficial, nearly 50% of participants chose not to learn some function of the smart home technology[48]. The primary reasons for system non-use were identified as poor usability and power failures, coupled with participant inexperience with the system[48]. Regarding system non-use, the authors recommended increased automation as a potential solution to increase adoption. In addition, they outlined the need to determine level of interest in technology, differences in the way people age and variations in way different illnesses develop.
Brownsell et al. concluded that “second generation” HSH/HCH such as video cameras; intruder alarms; flood detectors; automatic lights; and bed, chair, motion and door sensors should be more widely deployed based on detection of 22 dangerous situations during their study. In contrast, they recommendedthat “third generation” technologies, i.e. those that extend second gen eration technologies with pattern recognition and greater interaction, be subjected to greater scrutiny. Retrospective analysis in one case demonstrated a correlation between a major health event with general decline in activity and nutrition index. However, in another case where an older adult participant received 7 major medical interventions, third generation technologies did not raise any alerts[49]. As a result, even though the study used a commercially available system, they concluded that the technology should be considered developmental and could increase risk for older adults[49]. Brownsell et al. make 6 recommendations for technology improvement: 1) implement a standards-based approach to automating service provision; 2) match older adult needs to technology and services; 3) understand where technology can help and where it cannot; 4) identify appropriate circumstances for intervention; 5) provide for automated service adaptation based on changing behavior; 6) create a mechanism for delivery of feedback to older adults, family members and health care professionals[49].
Kelly et al. reported a community-level deployment in West Lothian, Scotland that involves a wireless core home safety package with a lifeline communication unit, 2 flood detectors, 2 PIR sensors, an extreme heat detector and a smoke detector provided to anyone over the age of 60 years of age[43]. Since the included study about this project is a three-page summary of a longitudinal program implementation, we provide additional information from a comprehensive government report of the project[69]. The West Lothian project was rolled out in three phases: In phase 1 (1999), a telecommunications company and a local government agency formed a partnership to pilot smart home technology pilot in 75 residences. In phase 2 (March 2003), the smart home technology was rolled out to 1200 households where older adults were receiving home-based care services. In phase 3 (December 2003), smart home technology and support were offered to all adults over the age of 60 in the local jurisdiction, including healthy older adults[69]. As of August 2006, the program had enrolled 2,150 older adults[43,69].
As a result, the jurisdiction experienced reduced hospital admissions, reduced lengths of stay in hospitals and reduced lengths of stays in nursing homes after discharge due to these preventive measures. The authors identified communication difficulty as a barrier to transferability when trying to re-engineer business processes and shift organizational culture within multiple organizations[43].
3.1.7. Theory
Two of three effective (first tier) studies were based on theories but the theories themselves were not fully described in the publications. Tomita et al. briefly stated their study was based on “[e]xtending the concept of self-effort in maintaining functional status” (p. 24)[48] but did not cite a specific theory or conceptual model. Kelly et al. based a large scale deployment strategy on the concept of “mainstreaming”[43]. The mainstreaming approach involved making technology available to all older adults in the population to avoid stigma; the rationale was that if everyone had the technology, then technology would not an indicator of decline in function[69].
One of the ten promising studies was informed by theory or a conceptual model. Mahoney et al.[54] based their study on Bandura’s theory of perceived self-efficacy[70]. Of emerging studies, Demiris et al.[50] adapteda participatory evaluation approach based on the work of Israel et al.[71] and Otjacques et al.[56] relied on elements of the Technology Acceptance Model[72], Unified Theory of Acceptance and Use of Technology[73] and findings from gerontology research to identify ten key design rules for older adults.
3.1.8. Cost
While many included studies provided a discussion of the economic effect of growth in the older adult population as background, few included costs of HSH/HCH from the consumer point of view. With regard to consumer costs for effective (first tier) studies, the smart home technology and support service in West Lothian was originally offered for a weekly charge of £4.87[43] (€~5.95/$7.82 USD) but weekly charges were discontinued and the service was offered free of charge starting in January 2006[69]. Tomita et al. demonstrated that an existing home can be converted using commercial off-the-shelf technology for less than $400 (€~304)[48]. Brownsell et al.[49], did not report the costs of the commercial system involved in their study but discussed the lack of available cost information for telecare as a barrier to adoption.
Of promising studies, van Hoof et al. estimated costs savings of €6,000–16,000 ($~7,900–21,000 USD) if people were allowed to age in place versus being institutionalized but noted the current cost of the system used in the study was €13,500 ($~17,800 USD) due to small scale technology production[65]. Only Mahoney et al. surveyed family members involved in their study about willingness to pay for the technology. Of the 9 who responded, 5 were willing to pay $60 USD (€~45) per month while 4 were willing to pay $30 (€~23) per month[54]. Mahoney et al.’s findings compare closely with Tomita et al.’s $400 USD (€304) HSH/HCH installation cost for a 2 year period[48] and Kelly et al.’s initial £4.87 (€ ~5.95/$7.82 USD) per week[43]. However, the sample size for Mahoney et al.’s survey was small (n=9).
3.1.9. Stakeholders
Stakeholders described in the 13 combined effective (first tier) and promising studies include older adults, family members, health care professionals, researchers, housing organizations and staff, home care agencies and staff, engineers and technology vendors. Family members were discussed or engaged in 11 of the 13 studies categorized as effective (first tier) or promising but only three promising studies[39,44,54] included family members as participants. Interestingly, two of the effective (first tier) studies, Brownsell et al.[49] and Tomita et al.[48] did not discuss family members. Only Mahoney et al.[54] explicitly described the need to provide information to policy makers for decision-making while only Kaye et al.[63] discussed the role that public health professionals might play with regard to technology and aging in place.
4. Discussion
The aim of this systematic review was to characterize the range of evidence concerning how health smart homes (HSH) and home-based consumer health (HCH) technologies might support aging in place. To do so, we included study designs ranging from technology trials to community-based interventions. Our motivation was to identify and characterize the best available evidence (what has been done) in absence of the best possible evidence (what might be done)[20].
Twenty-eight of the 31 studies included in this review were classified as emerging or promising evidence. By definition, these studies did not demonstrate strong evidence of support for aging in place due to their study designs, sample size and other factors (see Table 1). Three of the 31 included studies were classified as “effective (first tier)” evidence in support of aging in place but each these studies had some limitations related to participant dropout rates[48], non-randomized comparison groups[49] and use of a historical control[43]. We note that these results were not unexpected at the outset of the review.
Overall, emerging studies made conclusions about the function and improvement of technology. Promising studies typically made conclusions about the acceptability of technology and the feasibility of measuring behavior and outcomes. Effective (first tier) studies measured actual outcomes, such as changes in cognitive levels and time outside the home, in participant samples large enough to calculate statistically significant results (see Table 1 for details).
A pattern that emerged was that almost all included studies had an activity sensing component. Of these, most used passive infrared sensors. All studies that included a physiological sensing component included activity sensing. Another pattern that emerged was that the three effective (first tier) studies were composed of multiple technology components tailored to individual preferences. These components included activity sensing and other functionality such as medication reminders, bed occupancy and fall detection. This pattern suggests that activity sensing used in conjunction with other technologies in a multicomponent approach is a successful strategy to support independent aging.
Results showed that 77% (24/31) of all included studies were published in the year 2005 and beyond. In that period, 100% of effective (first tier) studies, 90% of promising studies and 67% of emerging studies were reported. This increase in the total number of studies since 2005 and a trend toward stronger study designs is encouraging if the goal of a HSH/HCH population-based intervention to support aging in place is to be reached. However, the quality of the three studies classified as effective (first tier) is limited by weaknesses with respect to participant dropout rates[48], non-randomized comparison groups[49] and use of a historical control[43]. There was no effective (second tier) evidence that HSH/HCH technologies had been implemented successfully in contexts outside their original settings.
All publications included in this review described studies with human subjects but only slightly more than half (16/31) reported institutional review or informed consent obtained from participants. Reporting of conflicts of interest was reflected at an even lower level (1/31, 3%). These findings related to ethical issues are congruent with prior STARE-HI research where some informatics researchers placed a low priority on reporting about human subjects review and obtaining formal permissions from study participants[16,17]. The low reporting of human subjects review and conflicts of interest for some studies included in this review is an ethical point of concern. It would be beneficial for all research studies in this domain of study to report institutional review board approval and informed consent processes in keeping with standards for research that involves human subjects. Similarly, all researchers who conduct technology research with human subjects should fully disclose all financial and other potential conflicts of interests to avoid the potential for coercion, particularly with potentially vulnerable populations such as older adults.
There is a need for informatics research that is based on theoretical frameworks and models to provide a rationale for hypothesized relationships and guidance to verify them[74]. However, few publications in this review described studies that were based on a theoretical framework or conceptual model. Research that lacks a theoretical basis is consistent with findings from reviews of the use of usability[74] and evaluation methods[75] in informatics. In addition, only a small number of included studies reported the use of validated instruments to measure outcomes[44,48,49,63]. To enable comparability of results between both HSH/HCH and non-HSH/HCH interventions alike, it is important that future studies use validated, reliable instruments that are also conceptually congruent with measures of interest (i.e., functioning and Instrumental Activities of Daily Living).
There is a need for targeted, meaningful indicators in home-based telemonitoring systems[76]. Nearly all promising and effective (first tier) studies included in this review implemented passive infrared (PIR) sensors to monitor activity levels. While technology typically changes at a rapid pace, PIR sensors represent a mature technology. All PIR sensors detect motion via the same mechanism – via changes in heat within range of the sensor face. An open question with regard to PIR sensor data is the ability to decipher patterns from multiple occupants in a residence. Developing ways to use data from couples or families is an important issue since, for example, only 18.5% of men and 39.5% of women over 65 in the United States live alone[77]. Most studies in this review did not enroll couples as participants. Of those, only one study reported the results of early work to identify individuals through silhouette extraction using a video sensor network in conjunction with PIR sensors[58]. The results of this review indicate a need for methods to incorporate other types of data that contextualize automatically collected sensor data for use as meaningful indicators. Given recent recommendations that patient-reported measures of psychosocial issues and health behavior should be integrated into electronic medical records[78], future research of HSH/HCH technology should explore how compatible, standardized participant-reported measures can be captured and implemented in personal health records.
The need for a development approach that supports the needs and preferences of older adults rather than the use of a technology-driven approach was recognized in the earliest promising study included in this review[39]. Evidence showing that this issue persists was suggested by a recent study that described clinician concerns that development of telemonitoring systems was driven by available technology[76]. In contrast, many of the recently published studies included in this review demonstrate a focus on the needs and preferences of older adults[44,50,53,54,57,58,63,65].
The needs of family members of older adults and other stakeholders should also be supported in the development of HSH/HCH technology. Involving and reporting the engagement of family members is important because family members who act as informal caregivers provide most care that allows older adults with cognitive and functional limitations to live in the community[77]. However, few studies in this review included family members as participants or demonstrated evidence for technology that supports social interaction. HSH/HCH technologies are a natural fit to support existing family and peer relationships for older adults. There was a marked lack of evidence for technologies that provide feedback to older adults for decision-making in their daily activities or maintenance of their own health. In addition, only 1 study in this review described the potential role of public health practitioners by enabling “real-time epidemiology”(p. i187)[63]. Future research should include these stakeholders and topic areas.
This review identified and characterized three studies as effective (first tier) evidence for support of aging in place. One reason for the small number of included studies may be a gap in communication between technology and health sciences researchers in the area of health smart homes and home-based consumer health technology research. Another reason may be that research often fails to translate into practice because study designs do not address real-world context and what researchers consider to be evidence is often limited[79]. Transferring technology into the home from organizational settings to support independent living in older adults presents contextual challenges due to the less controlled nature of the home setting[80]. Two promising studies included in this review (6%) focused on technologies validated in other settings and then adapted to independent living settings: Alwan et al.[44] adapted a monitoring system from an assisted living setting[81] and Mahoney et al.[54] adapted a remote caregiver intervention[81]. One commercial technology seems to have started in home settings[37,46] and then was transferred to assisted living facilities[82].
Glascock and Kutzik stated that “the effectiveness of behavioral monitoring and the electronic records that are now produced will largely be determined by the market rather than by a hypothetical double-blind research project. Once a concept has been moved from the laboratory to the commercial world, market forces become the primary testing agent, not funded research projects”(p. 5)[46]. However, in a follow-up study in a home health care setting, they noted problems of attrition in enrollment when 2 of 26 participants in a twelve month pilot study could not afford to pay their phone bills[82]. This finding raises the concern that market forces may dictate denial of access to technology and services that might otherwise allow older adults with lower incomes to age in place. Further, this finding supports Brownsell’s concern that existing commercial lifestyle monitoring technologies may not be ready for deployment on a wide scale[49].
Commercial vendors appear to be focusing on the market segment for organizations that provide community housing with services. In order to provide inclusive support for aging in place in all countries, there is a need to expand this focus to older adults in all living situations. For example, in 2007, of the over 34 million Medicare enrollees age 65 and over in the United States, about 2.4% lived in community housing with services, about 4.2% long term care facilities and the remaining 93.3% lived in traditional community residential settings[77]. Since nearly 32 million community-dwelling older adults in the US alone could benefit from informatics-based solutions that allow them to age in place, focusing only on community housing with services would deprive a large segment of the world’s older adult population of their choice of living arrangement as needs for health care services change.
One of the factors related to widespread implementation and individual technology access is lack of information related to technology costs and sustainable reimbursement models. Six included studies reported limited information regarding cost. In one of these, the West Lothian project, the technology was eventually given away for free[43,69] but the intervention was not translated to other settings. In addition, this intervention[43,69] was implemented in the UK, specifically in Scotland. As a result, it lacks a reimbursement model that might translate to other countries. Future research that explores factors to translate HSH/HCH technology interventions into practice should report detailed cost information and explore sustainable reimbursement models.
5. Conclusion
This study is a systematic review of the health smart homes and home-based consumer health technologies (HSH/HCH) literature with results categorized according to an evidence-based public health (EBPH) typology. Our efforts identified three effective (first tier) studies[43,48,49] that demonstrated support for independence and prevention of health events that threaten the independence of older adults. These three studies involved multiple components with an activity sensing component coupled with other functionality such as medication reminders, bed occupancy and fall detection. One of these studies was a large scale community implementation that used a technology “mainstreaming” approach that may reduce stigma and facilitate transfer of HSH/HCH interventions between community settings[43]. While the evidence for prediction of functional decline based on changes in activity patterns (“lifestyle monitoring”) is promising, methods to interpret activity data and decipher patterns generated by multiple inhabitants who live together have yet to be reported. Longitudinal studies to develop these methods and determine the effect and impact of promising technologies should be undertaken. Existing longitudinal research studies[50,53,57,58,63] can serve as models to help move promising research to the stage of effective evidence. Future research should include ways that older adults can use activity data for preventive self-management of health, informatics strategies to connect multiple stakeholders for social support of older adults and exploration of self-reported health measures as standardized indicators with the aim of incorporating these measures into personal health records for older adult and family use; clinical information systems for clinical use; and community health registries for use by public health and aging services organizations. Research in these areas will satisfy calls for technology innovation research to support new models of person-centric care[83].
Limitations
There were a large number of technology trials and descriptive studies, with small numbers of participants, thus precluding a meta-analysis of outcomes. The three studies identified as effective (first tier) evidence had weaknesses related to participant dropout rates[48], non-randomized comparison groups[49] and use of a historical control[43].
Summary Points.
Existing knowledge about health smart homes (HSH) and home-based consumer health (HCH) technology research:
HSH/HCH technologies have the potential to support older adults to age in place as the world’s population ages.
HSH/HCH technology research is conducted in health services and technology disciplines and reporting of results is fragmented along disciplinary lines.
Fragmentation in reporting of HSH/HCH technology research creates a knowledge gap concerning what research has been done and communication barriers for knowledge translation to relevant stakeholders.
HSH/HCH technology research should be framed in ways that all stakeholders, including older adults, family caregivers, designers, clinicians, public health practitioners and policy makers, can understand what evidence exists and what is needed to support aging in place at a population level.
What this study added:
Framing HSH/HCH technology research according to an evidence-based public health typology is a feasible undertaking and illustrates the state of research over time in a simplified fashion.
The strength of evidence for HSH/HCH technologies as a population-level intervention to support aging in place for older adults has improved since 2005.
HSH/HCH technology research to support aging in place must be conducted with a focus that includes all living arrangements.
The use of STARE-HI guidelines during data abstraction can be useful to compare completeness of item reporting for studies in a literature review.
Research Highlights.
Framing HSH/HCH research using an EPBH typology is a feasible undertaking
The EPBH typology illustrates HSH technology research in a simplified fashion
Strength of evidence for HSH/HCH to support aging in place has improved since 2005
HSH/HCH research to support aging in place must include all living arrangements
STARE-HI is useful to compare completeness of item reporting in a literature review
Acknowledgments
This work was supported by the National Institute of Nursing Research [Training Grant T32NR007106] and the National Library of Medicine [Training Grant 5T15LM007442].
Footnotes
Author Contributions
BR conceptualized the study and participated in all phases of the review. GD and HT assisted with study design, search methodology, definitions and criteria. BR, SC and EM reviewed articles and applied inclusion/exclusion criteria. BR, SC, EM and AL developed and updated the codebook. BR and EM performed data abstraction. BR and AL classified included studies. All authors contributed to the writing of the manuscript. All authors approved the final manuscript.
Competing Interests
The authors have no conflicting interests to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rice DP, Fineman N. Economic implications of increased longevity in the United States. Annu Rev Public Health. 2004;25:457–73. doi: 10.1146/annurev.publhealth.25.101802.123054. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Living Well with Chronic Illness: A Call for Public Health Action. The National Academies Press; 2012. [Google Scholar]
- 3.Breslow L. Health Measurement in the Third Era of Health. Am J Public Health. 2006 Jan 1;96(1):17–9. doi: 10.2105/AJPH.2004.055970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marek KD, Rantz MJ. Aging in place: a new model for long-term care. Nursing administration quarterly. 2000;24(3):1–11. doi: 10.1097/00006216-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Demiris G, Rantz MJ, Aud MA, Marek KD, Tyrer HW, Skubic M, Hussam AA. Older adults’ attitudes towards and perceptions of ‘smart home’ technologies: a pilot study. Informatics for Health and Social Care. 2004;29(2):87–94. doi: 10.1080/14639230410001684387. [DOI] [PubMed] [Google Scholar]
- 6.Reeder B, Demiris G, Marek KD. Older adults’ satisfaction with a medication dispensing device in home care. Informatics for Health and Social Care. 2013;0(0):1–12. doi: 10.3109/17538157.2012.741084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keller LO, Strohschein S, Lia-Hoagberg B, Schaffer MA. Population-Based Public Health Interventions:Practice-Based and Evidence-Supported. Part I Public Health Nursing. 2004;21(5):453–68. doi: 10.1111/j.0737-1209.2004.21509.x. [DOI] [PubMed] [Google Scholar]
- 8.Evashwick C. Creating the continuum of care. Health matrix. 1989;7(1):30–9. [PubMed] [Google Scholar]
- 9.Stults BM. Preventive health care for the elderly. Western Journal of Medicine. 1984;141(6):832. [PMC free article] [PubMed] [Google Scholar]
- 10.Kane RL, Kane RA, Arnold SB. Prevention and the elderly: risk factors. Health services research. 1985;19(6 Pt 2):945. [PMC free article] [PubMed] [Google Scholar]
- 11.Washington KT, Meadows SE, Elliott SG, Koopman RJ. Information needs of informal caregivers of older adults with chronic health conditions. Patient Education and Counseling. 2011;83(1):37–44. doi: 10.1016/j.pec.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 12.Demiris G, Skubic M, Rantz MJ, Courtney KL, Aud MA, Tyrer HW, He Z, Lee J. Facilitating interdisciplinary design specification of “smart” homes for aging in place. Stud Health Technol Inform. 2006;124:45–50. [PubMed] [Google Scholar]
- 13.Revere D, Turner AM, Madhavan A, Rambo N, Bugni PF, Kimball A, Fuller SS. Understanding the information needs of public health practitioners: a literature review to inform design of an interactive digital knowledge management system. J Biomed Inform. 2007 Aug;40(4):410–21. doi: 10.1016/j.jbi.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Pilemalm S, Timpka T. Third generation participatory design in health informatics--Making user participation applicable to large-scale information system projects. Journal of biomedical informatics. 2008;41(2):327. doi: 10.1016/j.jbi.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Rychetnik L, Hawe P, Waters E, Barratt A, Frommer M. A glossary for evidence based public health. Journal of epidemiology and community health. 2004;58(7):538–45. doi: 10.1136/jech.2003.011585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Keizer NF, Talmon J, Ammenwerth E, Brender J, Nykanen P, Rigby M. Mini Stare-HI: guidelines for reporting health informatics evaluations in conference papers. Stud Health Technol Inform. 2010;160(Pt 2):1206–10. [PubMed] [Google Scholar]
- 17.de Keizer NF, Talmon J, Ammenwerth E, Brender J, Rigby M, Nykänen P. Systematic Prioritization of the STARE-HI Reporting Items. An Application to Short Conference Papers on Health Informatics Evaluation. Methods Inf Med. 2011 Mar 4;50(3) doi: 10.3414/ME10-01-0072. [DOI] [PubMed] [Google Scholar]
- 18.Talmon J, Ammenwerth E, Brender J, de Keizer N, Nykänen P, Rigby M. STARE-HI - Statement on reporting of evaluation studies in Health Informatics. [doi: 10.1016/j.ijmedinf.2008.09002] 2009;78:1–9. doi: 10.1016/j.ijmedinf.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Friedman CP, Wyatt J. Evaluation methods in biomedical informatics. New York, New York: Springer Verlag; 2006. [Google Scholar]
- 20.Brownson RC, Fielding JE, Maylahn CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu Rev Public Health. 2009;30(1) doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- 21.Brownson RC, Baker EA, Leet TL, Gillespie KN, True WR. Evidence-based public health. New York; Oxford: Oxford University Press; 2011. [Google Scholar]
- 22.Alborz A, McNally R. Developing methods for systematic reviewing in health services delivery and organization: an example from a review of access to health care for people with learning disabilities. Part 2. Evaluation of the literature—a practical guide. Health Information & Libraries Journal. 2004;21(4):227–36. doi: 10.1111/j.1471-1842.2004.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shuhong W, Moss JR, Hiller JE. Applicability and transferability of interventions in evidence-based public health. Health Promotion International. 2006;21(1) doi: 10.1093/heapro/dai025. [DOI] [PubMed] [Google Scholar]
- 24.Brennan L, Castro S, Brownson RC, Claus J, Orleans CT. Accelerating evidence reviews and broadening evidence standards to identify effective, promising, and emerging policy and environmental strategies for prevention of childhood obesity. Annual Review of Public Health. 2011;32:199–223. doi: 10.1146/annurev-publhealth-031210-101206. [DOI] [PubMed] [Google Scholar]
- 25.Demiris G, Hensel BK. Technologies for an aging society: a systematic review of “smart home” applications. Yearbook of medical informatics. 2008;47 (Suppl 1):33–40. [PubMed] [Google Scholar]
- 26.Bal M, Weiming S, Qi H, Xue H, editors. Collaborative Smart Home technologies for senior independent living: A review. Computer Supported Cooperative Work in Design (CSCWD); 2011 15th International Conference on; 2011 8–10 June; 2011. [Google Scholar]
- 27.Cardinaux F, Bhowmik D, Abhayaratne C, Hawley MS. Video based technology for ambient assisted living: A review of the literature. J Ambient Intell Smart Environ. 2011;3(3):253–69. [Google Scholar]
- 28.Chan M, Campo E, Estève D, Fourniols JY. Smart homes - current features and future perspectives. Maturitas. 2009;64(2):90–7. doi: 10.1016/j.maturitas.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 29.Chan M, Esteve D, Escriba C, Campo E. A review of smart homes- present state and future challenges. Comput Methods Programs Biomed. 2008 Jul;91(1):55–81. doi: 10.1016/j.cmpb.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Demiris G, Hensel BK. Technologies for an aging society: a systematic review of “smart home” applications. Yearbook of Medical Informatics. 2008:33–40. [PubMed] [Google Scholar]
- 31.Koch S. Home telehealth--current state and future trends. International Journal of Medical Informatics. 2006 Aug;75(8):565–76. doi: 10.1016/j.ijmedinf.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Koch S, Hägglund M. Health informatics and the delivery of care to older people. Maturitas. 2009;63(3):195–9. doi: 10.1016/j.maturitas.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 33.Magnusson L, Hanson E, Borg M. A literature review study of information and communication technology as a support for frail older people living at home and their family carers. Technology & Disability. 2004;16(4):223–35. [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kawarada A, Takagi T, Tsukada A, Sasaki K, Ishijima M, Tamura T, Togawa T, Yamakoshi K, editors. Evaluation of automated health monitoring system at the “Welfare Techno House. Engineering in Medicine and Biology Society; Proceedings of the 20th Annual International Conference of the IEEE; 1998 29 Oct-1 Nov 1998.1998. [Google Scholar]
- 36.Paolo D, Eugenio G, Cecilia L, Giancarlo T. MOVAID: a personal robot in everyday life of disabled and elderly people. Technology and Disability. 1999;10(2):77–93. [Google Scholar]
- 37.Glascock A, Kutzik D. Behavioral Telemedicine: A New Approach to the Continuous Nonintrusive Monitoring of Activities of Daily Living. Telemedicine Journal. 2000;6(1):33–44. [Google Scholar]
- 38.Kawarada A, Nambu M, Tamura T, Ishijima M, Yamakoshi K, Togawa T, editors. Fully automated monitoring system of health status in daily life. Engineering in Medicine and Biology Society, 2000; Proceedings of the 22nd Annual International Conference of the IEEE; 2000; 2000. [Google Scholar]
- 39.Sixsmith AJ. An evaluation of an intelligent home monitoring system. Journal of telemedicine and telecare. 2000;6(2):63–72. doi: 10.1258/1357633001935059. [DOI] [PubMed] [Google Scholar]
- 40.Ogawa M, Suzuki R, Otake S, Izutsu T, Iwaya T, Togawa T. Long term remote behavioral monitoring of elderly by using sensors installed in ordinary houses; Microtechnologies in Medicine & Biology 2nd Annual International IEEE-EMB Special Topic Conference on; 2002; 2002. [Google Scholar]
- 41.Ohta S, Nakamoto H, Shinagawa Y, Tanikawa T. A health monitoring system for elderly people living alone. Journal of Telemedicine & Telecare. 2002;8(3):151–6. doi: 10.1177/1357633X0200800305. [DOI] [PubMed] [Google Scholar]
- 42.Chan M, Campo E, Esteve D. Assessment of activity of elderly people using a home monitoring system. International journal of rehabilitation research. 2005;28(1):69–76. doi: 10.1097/00004356-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 43.Kelly D. Smart support at home: the integration of telecare technology with primary and community care systems. British Journal of Healthcare Computing & Information Management. 2005;22(3):19–21. [Google Scholar]
- 44.Alwan M, Kell S, Turner B, Dalai S, Mack D, Felder R, editors. Psychosocial Impact of Passive Health Status Monitoring on Informal Caregivers and Older Adults Living in Independent Senior Housing. Information and Communication Technologies; ICTTA ‘06. 2nd; 2006. 20060–0 0. [Google Scholar]
- 45.Fujimura K, Sato H, Mochizuki T, Koichiro K, Shimokura K, Itoh Y, Murata S, Ogura K, Watanabe T, Fujino Y, Tsuboi T. Why does IT support enjoyment of elderly life?: case studies performed in Japan. Proceedings of the 12th international conference on Human-computer interaction: interaction design and usability; Beijing, China: Springer-Verlag; 2007. [Google Scholar]
- 46.Glascock AP, Kutzik DM. An Evidentiary Study of the Uses of Automated Behavioral Monitoring. Proceedings of the 21st International Conference on Advanced Information Networking and Applications Workshops - Volume 02: IEEE Computer Society; 2007. [Google Scholar]
- 47.Tamura T, Kawarada A, Nambu M, Tsukada A, Sasaki K, Yamakoshi K. E-healthcare at an experimental welfare techno house in Japan. Open Med Inform J. 2007;1:1–7. doi: 10.2174/1874431100701010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tomita MR, Mann WC, Stanton K, Tomita AD, Sundar V. Use of currently available smart home technology by frail elders: process and outcomes. Topics in Geriatric Rehabilitation 2007. 2007 Jan-Mar;23(1):24–34. [Google Scholar]
- 49.Brownsell S, Blackburn S, Hawley MS. An evaluation of second and third generation telecare services in older people’s housing. J Telemed Telecare Journal of Telemedicine and Telecare. 2008;14(1):8–12. doi: 10.1258/jtt.2007.070410. [DOI] [PubMed] [Google Scholar]
- 50.Demiris G, Oliver DP, Dickey G, Skubic M, Rantz M. Findings from a participatory evaluation of a smart home application for older adults. Technology & Health Care. 2008;16(2):111–8. [PubMed] [Google Scholar]
- 51.Diermaier J, Neyder K, Werner F, Panek P, Zagler WL. Distributed Accelerometers as a Main Component in Detecting Activities of Daily Living. Proceedings of the 11th international conference on Computers Helping People with Special Needs; linz, Austria: Springer-Verlag; 2008. [Google Scholar]
- 52.Rahal Y, Pigot H, Mabilleau P. Location estimation in a smart home: system implementation and evaluation using experimental data. Int J Telemed Appl. 2008:142803. doi: 10.1155/2008/142803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rantz M, Skubic M, Miller S, Krampe J. Using Technology to Enhance Aging in Place. Proceedings of the 6th international conference on Smart Homes and Health Telematics; Ames, IA, USA: Springer-Verlag; 2008. [Google Scholar]
- 54.Mahoney D, Mahoney E, Liss E. AT EASE: Automated technology for elder assessment, safety, and environmental monitoring. Gerontechnology. 2009;8(1):11–25. [Google Scholar]
- 55.Noury N, Quach KA, Berenguer M, Teyssier H, Bouzid MJ, Goldstein L, Giordani M, editors. Remote follow up of health through the monitoring of electrical activities on the residential power line - preliminary results of an experimentation. e-Health Networking, Applications and Services, 2009; Healthcom 2009. 11th International Conference on; 2009 16–18 Dec; 2009. [Google Scholar]
- 56.Otjacques B, Krier M, Feltz F, Ferring D, Hoffmann M. Helping older people to manage their social activities at the retirement home. Proceedings of the 23rd British HCI Group Annual Conference on People and Computers: Celebrating People and Technology; Cambridge, United Kingdom: British Computer Society; 2009. [Google Scholar]
- 57.Rantz MJ, Skubic M, Miller SJ, editors. Using sensor technology to augment traditional healthcare. Engineering in Medicine and Biology Society, 2009; EMBC 2009. Annual International Conference of the IEEE; 2009 3–6 Sept; 2009. [DOI] [PubMed] [Google Scholar]
- 58.Skubic M, Alexander G, Popescu M, Rantz M, Keller J. A smart home application to eldercare: current status and lessons learned. Technol Health Care. 2009;17(3):183–201. doi: 10.3233/THC-2009-0551. [DOI] [PubMed] [Google Scholar]
- 59.Junnila S, Kailanto H, Merilahti J, Vainio AM, Vehkaoja A, Zakrzewski M, Hyttinen J. Wireless, multipurpose in-home health monitoring platform: two case trials. IEEE Trans Inf Technol Biomed. 2010 Mar;14(2):447–55. doi: 10.1109/TITB.2009.2037615. [DOI] [PubMed] [Google Scholar]
- 60.Kim SJ, Dave B. Silver towns and smart technologies. Proceedings of the 22nd Conference of the Computer-Human Interaction Special Interest Group of Australia on Computer-Human Interaction; Brisbane, Australia: ACM; 2010. [Google Scholar]
- 61.Riche Y, Mackay W. PeerCare: Supporting Awareness of Rhythms and Routines for Better Aging in Place. Comput Supported Coop Work. 2010;19(1):73–104. [Google Scholar]
- 62.Etchemendy E, Baños RM, Botella C, Castilla D, Alcañiz M, Rasal P, Farfallini L. An e-health platform for the elderly population: The butler system. Comput Educ. 2011;56(1):275–9. [Google Scholar]
- 63.Kaye JA, Maxwell SA, Mattek N, Hayes TL, Dodge H, Pavel M, Jimison HB, Wild K, Boise L, Zitzelberger TA. Intelligent Systems For Assessing Aging Changes: home-based, unobtrusive, and continuous assessment of aging. J Gerontol B Psychol Sci Soc Sci. 2011 Jul;66(Suppl 1):i180–90. doi: 10.1093/geronb/gbq095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee ML, Dey AK. Reflecting on pills and phone use: supporting awareness of functional abilities for older adults. Proceedings of the 2011 annual conference on Human factors in computing systems; Vancouver, BC, Canada: ACM; 2011. [Google Scholar]
- 65.van Hoof J, Kort HSM, Rutten PGS, Duijnstee MSH. Ageing-in-place with the use of ambient intelligence technology: Perspectives of older users. International Journal of Medical Informatics. 2011;80(5):310–31. doi: 10.1016/j.ijmedinf.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 66.Folstein MF, Folstein SE, McHugh PR. “ Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 67.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. Journal of Gerontology. 1990;45(6):P239–P43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 68.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of personality assessment. 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 69.Bowes A, McColgan G. Smart technology and community care for older people: innovation in West Lothian, Scotland. Edinburgh: Age Concern Scotland; 2006. [Google Scholar]
- 70.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 71.Israel B, Schulz A, Parker E, Becker A. Community-based Participatory Research: Policy Recommendations for Promoting a Partnership Approach in Health Research. Education for Health: Change in Learning & Practice. 2001;14(2):182–97. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]
- 72.Davis FD, Bagozzi RP, Warshaw PR. User Acceptance of Computer Technology: A Comparison of Two Theoretical Models. Management Science. 1989;35(8):982–1003. [Google Scholar]
- 73.Venkatesh V, Morris MG, Davis GB, Davis FD. User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly. 2003;27(3) [Google Scholar]
- 74.Yen PY, Bakken S. Review of health information technology usability study methodologies. JAMIA. 2011;19(3):413–22. doi: 10.1136/amiajnl-2010-000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rahimi B, Vimarlund V. Methods to evaluate health information systems in healthcare settings: a literature review. Journal of medical systems. 2007;31(5):397–432. doi: 10.1007/s10916-007-9082-z. [DOI] [PubMed] [Google Scholar]
- 76.Peirce SC, Hardisty AR, Preece AD, Elwyn G. Designing and implementing telemonitoring for early detection of deterioration in chronic disease: Defining the requirements. Health Informatics Journal. 2011 Sep 1;17(3):173–90. doi: 10.1177/1460458211409717. [DOI] [PubMed] [Google Scholar]
- 77.United States Federal Interagency Forum on Aging-Related Statistics. . Older Americans 2010: Key Indicators of Well-Being. Government Printing Office; 2010. [Google Scholar]
- 78.Glasgow RE, Kaplan RM, Ockene JK, Fisher EB, Emmons KM. Patient-Reported Measures Of Psychosocial Issues And Health Behavior Should Be Added To Electronic Health Records. Health Affairs. 2012 Mar 1;31(3):497–504. doi: 10.1377/hlthaff.2010.1295. [DOI] [PubMed] [Google Scholar]
- 79.Glasgow RE, Emmons KM. How Can We Increase Translation of Research into Practice? Types of Evidence Needed. Annual Review of Public Health. 2007;28(1) doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 80.Gitlin LN. Conducting research on home environments: lessons learned and new directions. Gerontologist. 2003 Oct;43(5):628–37. doi: 10.1093/geront/43.5.628. [DOI] [PubMed] [Google Scholar]
- 81.Alwan M, Dalal S, Mack D, Kell S, Turner B, Leachtenauer J, Felder R. Impact of monitoring technology in assisted living: outcome pilot. Information Technology in Biomedicine, IEEE Transactions on. 2006;10(1):192–8. doi: 10.1109/titb.2005.855552. [DOI] [PubMed] [Google Scholar]
- 82.Glascock AP, Kutzik DM. The impact of behavioral monitoring technology on the provision of health care in the home. Journal of Universal Computer Science. 2006;12(1):59–79. [Google Scholar]
- 83.Rigby M, Ronchi E, Graham S. Evidence for building a smarter health and wellness future—Key messages and collected visions from a Joint OECD and NSF workshop. International Journal of Medical Informatics. 2012;(0) doi: 10.1016/j.ijmedinf.2012.10.003. [DOI] [PubMed] [Google Scholar]