Abstract
Complexity of health care has caused ethical dilemmas and moral distress to be quite unavoidable for nurses. Moral distress is a major, highly prevalent problem in the nursing profession. The study aims to investigate the effect of education based on the “4A model” on the rate of moral distress among the nurses working in Cardiac Care Units (CCU).
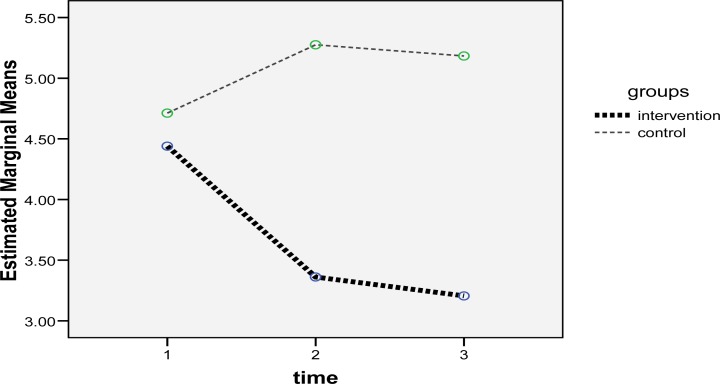
The participants consisted of 60 nurses working in Cardiac Care Units (CCU), 30 in the control and 30 in the intervention group. Those in the intervention group took part in the educational workshop about “moral distress” and “4A model”. The moral distress questionnaire was completed by both study groups 1 and 2 months after the intervention. After the intervention, the results of repeated measures analysis of variance revealed a significant difference in the moral distress mean scores between the intervention and the control groups (P<0.001) and within the two groups (P<0.001). Moreover, a significant difference was found between the two study groups regarding the mean score of moral distress 1 and 2 months after the intervention. The findings of the current study revealed a decreasing trend in the moral distress mean score in the intervention group, while there was an increasing trend in the control group after the intervention.
It can be concluded that the “4A model” can be used for reducing moral distress and educational interventions can reduce the rate of moral distress among nurses. Authors of this study recommend that more studies with larger sample sizes be conducted in different hospital wards as well.
Keywords: Moral distress, Cardiac care units, Education, Nurse, 4A model
Introduction
Complexity of health care has caused ethical dilemmas and moral distress to be quite unavoidable for nurses (1). Moral distress is a major, highly prevalent problem in the nursing profession (2, 3). In fact, moral distress is defined as a painful feeling and a psychological disequilibrium felt by the nurses when they are not able to do what they believe to be right. In other words, in moral distress, the individuals know what is right, but organizational limitations prevent them from acting upon it (2). Moral distress results from limited financial resources, a decrease in the patient to nurse ratio, and an increase in the severity of diseases (4, 5). Moreover, evidence shows that complexity of the environment, high population of the patients, and the nature of the nurses’ professional role in Critical Care Units (CCU) make them susceptible to moral distress (6, 7). The critical care nurses work in an environment where the patients are specifically faced with life-threatening problems; consequently, they are highly responsible for providing such patients with desirable services (8). In addition, due to the patients’ special conditions and the urgency of the medical measures, critical care nurses are more likely to encounter moral distress (9, 10). Moral distress can lead to the feeling of inability, fatigue, job dissatisfaction, negative self-concept, anger, depression, isolation, guilt, anxiety, changing the department or the hospital, and even quitting the nursing profession. Such nurses neglect the patients, cause them to feel unhappy and offended, and increase their pain as well as length of hospital stay, thus decreasing the care quality and patient satisfaction (1, 8, 11, 12). Overall, moral distress can have negative effects on the patients, nurses, and the healthcare system (13–15), so researchers have emphasized identification of moral distress in the healthcare system and are holding educational courses for reducing this phenomenon in nurses (3, 15–18). Moral education can provide the foundation for empowering systemic responses to moral distress (3, 19). The studies conducted on moral distress have so far focused on Western approaches; however, since the cultural context is quite effective in the creation of moral distress (15, 20), these studies are recommended to culturally take moral distress into account (21).
In general, the growth of research conducted on moral distress shows the international attention to this phenomenon (3) . In Iran, both quantitative (22–24) and qualitative studies (25) have been performed on this issue; nevertheless, while all these studies have emphasized the importance of educational interventions in reducing the nurses’ moral distress, no study has been carried out on the effect of educational intervention on the rate of moral distress. In the international contexts, few studies have been performed on this issue likewise and the researchers studying the effect of educational interventions on moral distress have stressed the necessity to perform more studies and interventions in this field (16, 26, 27). The American Association of Critical-Care Nursing (AACN) provided a model in 2004 entitled the “4A’s to Rise Above Moral Distress” that offers a framework for critical care nurses to identify and deal with moral distress. In review of articles, only Beumer (2008) performed an interventional study by using the AACN’s model on ICU nurses (16). The present study aims to investigate the effect of education based on the “4A model” on the rate of moral distress among the nurses working in Cardiac Care Units (CCU).
Method
In this randomized controlled trial study, the intervention was performed through holding an educational workshop based on the “4A model” for the Cardiac Care Units (CCU) nurses and a moral distress questionnaire was completed by both the intervention and the control groups before and after the intervention.
The present study was conducted on 60 nurses working in Cardiac Care Units (CCU) of Shiraz Heart Center. The participants expressed their consent to take part in the study and after reaching the quorum, enrolled nurses were randomly assigned to the intervention (n=30) or the control group (n=30) with the use of a randomization list (random permuted blocks with length 4). The inclusion criteria of the study were having at least a bachelor degree in nursing, having at least 6 months of working experience (22) in Cardiac Care Units, willingness to participate in the research, not suffering from anxiety disorders, and not using anti-anxiety drugs, based on self-report forms.
In the present study, the researchers used Corley’s Moral Distress Scale (MDS) whose reliability and validity were assessed in Iran’s nursing community in 2008 (9). This questionnaire included 30 items with a 7-point Likert scale, 1 and 7 representing the lowest and the highest levels of tension respectively. In addition, it consisted of 3 domains of “Ignorance of the patient” (16 items), “Patient’s decision making power” (8 items), and “Practical-professional competency” (6 items). A researcher-made questionnaire including demographic information such as age, years of nursing experience, average working hours in a week, and marital status was also applied in this study.
The 30 nurses in the intervention group took part in the educational workshop that was held in the conference hall of the Heart Center in two 4-hour sessions during two consecutive weeks. At the beginning of the workshop, the intervention group was asked to avoid transferring the information about the contents of the educational workshop to the other colleagues up to the end of the study, and then questions were posed regarding the concept of moral distress and the nurses revealed to have no information about this concept. After providing explanations about the concept of moral distress, the participants were asked about the situations that could result in this phenomenon and they stated the exact same instances resulting in moral distress as mentioned in most of the studies. Next, the causes and symptoms of moral distress were mentioned and the participants discussed their experiences of this phenomenon. They said that before getting familiar with the concept of moral distress, they did not know what to name their feeling and considered it as an uncommon, unavoidable, and unsolvable feeling. When the participants asked about a way to eliminate or decrease the effect of moral distress, they were instructed to think about the strategies for reducing or eliminating this phenomenon in nurses and discuss them in the next session. In the second session, the nurses were asked about the strategies for reducing moral distress and they emphasized continuation of training courses, establishing ethical committees in the hospitals, and holding such workshops for the managers and head nurses. Afterwards, the participants were presented with the AACN model, which consists of 4 stages of ask, affirm, assess, and act. In the first stage (ask), the nurse asks him/herself whether the stress he/she feels is a sign of moral distress or just a feeling of suffering. The aim of this stage is awareness of the existence of moral distress. In the second stage (affirm), the nurse makes sure about the existence of moral distress by sharing his/her feelings with others and promises to reduce it. In the third stage (assess), the nurse identifies the source of moral distress, which might be personal or environmental, estimates the intensity of his/her stress, and makes himself/herself ready for the act stage. In the last stage (act), the nurse both personally and professionally attempts to reduce moral distress and uses strategies in order to reach this goal. It is not uncommon for a nurse to regress to the previous stages; what is important, however, is that he/she enters the act stage and attempts to maintain his/her personal integrity (28).
At this point, the participants were required to form 5-person groups and representatives were selected from each group to talk about the strategies used in Cardiac Care Units as well as in CCUs and exchange ideas. After that, each group’s representative explained his/her opinion to the others. The strategies for reducing moral distress were extracted from the articles and the stages of the model were also explained to the participants. Finally, for the participants’ better understanding of the model stages, 5 volunteers performed a role-play that was directed by one of the researchers, a professor of psychiatric nursing in Shiraz University of Medical Sciences, Shiraz, Iran. In this role-play, the participants suggested a situation creating moral distress in CCU and the “4A model” was performed for that situation. The participants stated that it was the first time that they felt someone was taking their feelings into account and requested further meetings to discuss their ethical dilemmas. They also asked for establishment of committees in hospitals so that the personnel could share and solve their ethical issues.
After the intervention, the participants were informed that they could contact the researcher by phone in case they had any questions regarding the performance of the “4A model” or their feeling of moral distress. Furthermore, the moral distress questionnaire was completed by both study groups before and 1 and 2 months after the intervention.
Ethical considerations
The present study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran and the hospital authorities’ permission was sought as well. Moreover, the participants signed the written informed consents for voluntarily taking part in the study before completing the questionnaires. Questionnaires were anonymized and the participants’ information was collected privately by the researchers.
Statistical Analysis
The study data were analyzed using the SPSS statistical software (v. 15). Cronbach’s alpha coefficients of 0.898, 0.736, and 0.714 were obtained for internal consistency of the dimensions of Ignorance of the patient, patient’s decision making ability and practical-professional competency, respectively. Moreover, repeated measures analysis of variance was used in order to compute the mean scores and compare the moral distress mean scores before and one and two months after the intervention. In addition, in order to compare the two groups based on the demographic characteristics, i.e. age, years of nursing experience, marital status, and average working hours, Chi-square test and independent sample t-test were used for the qualitative variables and the quantitative ones respectively. The changes in moral distress mean scores were compared between the two groups and based on different demographic variables such as age and marital status using twoway ANOVA.
Results
The present study was conducted on 60 nurses, 30 in the control and 30 in the intervention group. Among the study participants, 2 were male and 58 were female and the two male subjects were in the intervention group. In the intervention group, 56.7% of the participants were single, while 56.7% of the control subjects were married. The mean age of the nurses in the intervention and control groups was 29.63±5.14 and 29.67±4.24 years respectively, and the mean working experience in the intervention and control groups was 5.53±4.42 and 5.67±3.05 years respectively. In addition, the intervention and control groups’ mean working hours were 47.81±14.14 and 41.96±3.70 hours respectively. No difference was found between the two groups regarding the demographic variables and moral distress mean scores before the intervention; the results are presented in Table 1. Moreover, the results of the two-way ANOVA revealed no significant relationship in the differences in mean of the moral distress score in the two groups based on demographic variables including age, marital status, years of nursing experience, and average working hours in a week.
Table 1.
Demographic characteristics of the study participants
| Intervention (%) | Control (%) | P value | ||
|---|---|---|---|---|
| Gender | Female | 28(93.3) | 30(100) | 0.894 |
| Male | 2(6.7) | 0(0) | ||
| Age | 20–30 | 23(76.6) | 18(66.6) | 0.979 |
| 31–40 | 5(16.6) | 9(33.3) | ||
| 40+ | 2(6.6) | 0(0)* | ||
| Marital status | Single | 17(56.7) | 13(43.3) | 0.302 |
| Married | 13(43.3) | 17(56.7) | ||
| Years of nursing experience | (Mean ±SD): 5.539±4/426) | (Mean ±SD): 5.67±3.050) | 0.895 | |
| Average working hours in a week | (Mean ±SD): 47.81±14.40) | (Mean ±SD): 41.96±3.705) | 0.246 | |
|
| ||||
| Total | 30 | 30 | ||
Before the intervention, the two groups’ moral distress scores ranged from 2.30 to 7.50, and the moral distress mean score of the 60 participants was 4.57±1.03 out of 7. Overall, 15 out of 30 items revealed >4 mean scores which shows the high rate of moral distress among the study participants. The study results revealed a decreasing trend in the intervention group’s moral distress mean score in that it had reduced from 4.44±1.24 before the intervention to 3.36±0.996 and 3.048±1.25 one and two months after the intervention, respectively. On the other hand, the control group’s moral distress mean score showed an increasing trend, reaching from 4.712±1.048 before the intervention to 5.275±0.946 and 5.183±1.153 one and two months after the intervention, respectively. After the intervention, the results of repeated measures analysis of variance revealed a significant difference in the moral distress mean scores between the intervention and the control groups (P<0.001) and within the two groups (P<0.001). Furthermore, a significant difference was found between the two study groups regarding the mean score of moral distress 1 and 2 months after the intervention. Similar results were also obtained regarding the domains of moral distress (Figure 1 and Table 2).
figure 1.
trend of moral distress mean in intervention and control groups
Table 2.
Moral distress in both groups during the study period
| Moral distress | Pre intervention | After 1 month | After 2 month | Time | Time-group | group | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Mean ± SD | Mean ± SD | Mean ± SD | |||||||
|
| |||||||||
| Intervention | Control | Intervention | control | Intervention | Control | ||||
|
|
|||||||||
| 4.32±1.02 | 4.62±1.08 | 3.26±1.08 | 5.11±0.89 | 5.01±1.13 | 3.14±1.33 | 0.03 | <0.001 | <0.001 | |
| Domain1* | 3.47±0.09 | 3.85±1.26 | 2.70±0.91 | 4.36±1.16 | 4.32±1.30 | 2.57±1.10 | 0.38 | <0.001 | <0.001 |
| Domain2** | 4.18±1.12 | 4.66±1.05 | 3.27±0.88 | 5.22±0.87 | 5.04±1.00 | 3.07±1.15 | 0.09 | <0.001 | <0.001 |
| Domain3*** | 4.44±1.02 | 4.71±1.04 | 0.36±0.99 | 5.11±0.89 | 5.18±0.15 | 3.20±1.25 | 0.05 | <0.001 | <0.001 |
“Ignorance of the patient”,
“Patient’s decision making power”,
“Practical-professional competency”
Before the intervention, in “Ignorance of the patient” domain, the two items “Give only hemodynamic stabilizing medication intravenously during a Code with no compression or intubation” and “Carry out a work assignment in which I do not feel professionally competent” revealed the highest mean scores in both study groups. In the “Patient’s decision making ability” domain, the statement “Follow the family’s wishes for the patient care when I do not agree with them” had the highest mean score. Finally, in the “Practical-professional competency” domain, the highest mean scores were related to the items “Work in a situation where the number of staff is so low that care is inadequate”, “Assist a physician who in your opinion is providing incompetent care”, and “Work with ‘unsafe’ levels of nurse staff”. Overall, the results of the study showed that the mean score of moral distress regarding the above-mentioned domains had decreased in the intervention group, while they increased in the control group 1 and 2 months after the intervention. Moreover, a statistically significant difference was observed between the intervention and the control groups and within the two groups in this regard.
Discussion
The findings of the current study showed a high mean score of moral distress among the participants before the intervention. Several studies also reported high mean scores of moral distress among nurses (13, 22, 29–31).
In this study, no significant relationship was found between the changes in moral distress mean scores and the demographic characteristics including age, marital status, years of nursing experience, and average working hours in a week, before and after the intervention, which is consistent with the findings of several studies conducted on the issue (18, 31, 32). However, some other studies have revealed a significant relationship between the rate of moral distress and the nurses’ level of education (33), age (34), and years of nursing experience (35). Also, married nurses tended to experience moral distress more in comparison to single ones (9). The researchers who have revealed a negative relationship between moral distress and years of nursing experience point out that as the nurses get older, they have more experience of clinical conditions, develop adaptability mechanisms, and act better in moral distress creating situations (36, 37). Furthermore, as to the absence of a relationship between moral distress and demographic variables, Corley et al. believes that occupational stress, job dissatisfaction, and the role of nursing managers, colleagues, physicians and the ethical environment in creating moral distress are the other factors which need to be investigated (32).
The study findings showed a significant difference between the moral distress mean scores in the two groups 1 and 2 months after the intervention. In fact, the rate of moral distress had changed in the two study groups so that the moral distress mean score had decreased in the intervention group, while it had increased in the control group, 1 and 2 months after the intervention. This shows the effect of the nurses’ training and awareness about this phenomenon on reducing their moral distress. Similarly, Beumer’s study (2008) showed positive outcomes of educational interventions revealing that educational workshops and continuous education were of great value in reducing the nurses’ moral distress (16). Educational courses bring about an increase in the individuals’ ability to cope with moral distress and enrichment of healthcare environments through the use of effective strategies (38). On the other hand, the increasing trend of moral distress in the control group shows that in case moral distress is not recognized or diminished, its complexity and severity are enhanced, leading to irreversible effects over time. A large number of researchers have also mentioned the adverse effects of unresolved moral distress, including loss of self-esteem, change in interpersonal relationships, and psychological signs such as anger, fatigue, feeling of guilt, and lack of trust in others (11, 18, 37, 39) . These findings show the necessity of more consideration on the part of the managers of the healthcare systems in order to prevent the increasing trend of moral distress among critical care nurses.
The results of the present study showed that before the intervention, the highest mean score in “Ignorance of the patient” domain was related to the items “Give only hemodynamic stabilizing medication intravenously during a Code with no compression or intubation” and “Carry out a work assignment in which I do not feel professionally competent”, which is in agreement with the results obtained in the study by Merghati Khoei et al. (9). It should be noted that these two items had the highest mean score among all the domains. These findings show that in cases where the patients’ rights are ignored due to the nurses’ lack of professional competence or the physicians’ incorrect orders, the critical care nurses experience the highest level of moral distress. In fact, the nurses experience moral distress when they feel that they cannot provide care in a proper, principle-based manner (2). In general, nursing competence and performance are moral principles (40). On the other hand, patient care offered by novice, inexperienced individuals highly affects the quality of care (25) and together with the feeling of being inefficient as a nurse and the inability to provide care for the patients will lead to moral distress (6, 33). Thus, in Iran, it is necessary to assess the nurses’ clinical competence upon employment and over time and focus on their educational needs for in-service training courses in order to enhance their capabilities and skills. Also, considering the effectiveness of the educational workshop trainings in reducing the moral stress mean scores in the intervention group, such workshops need to be held for nurses in Iran and in other clinical departments as well.
Considering “Ignorance of the patient” domain, the item “Carry out orders or institutional policies to discontinue treatment because the patient can no longer pay” revealed the highest mean score in the study conducted by Abbas Zadeh et al (2011)(22), while this statement was ranked the third in the present study. In the “Patient’s decision making ability” domain, the highest mean score was related to the item “Follow the family’s wishes for the patient care when I do not agree with them”, which is in line with the studies by Merghati Khoei et al. (9) and Corley et al. (32). Zuzelo (2007)(41) has also stated that in case what the patients want is ignored because of their families’ requests or hospital requirements, the nurses will experience moral distress (41). Furthermore, observing the patients suffering due to the physicians’, hospitals’, or families’ decisions is quite painful for the nurses. As patient advocates, when the nurses see that their attempts are fruitless and they have no power to modify the physicians’ decisions in the healthcare systems, they experience moral distress (8).
In the “Practical-professional competency” domain, the highest mean score was obtained in the items “Work in a situation where the number of staff is so low that care is inadequate”, “Assist the physician who in your opinion is providing incompetent care”, and “Work with ‘unsafe’ levels of nurse staff”. In the study performed by Merghati Khoei et al. (9), the item “Assist the physician who in your opinion is providing incompetent care” was consistent with the results of the present study. In addition, the item “Work in a situation where the number of staff is so low that care is inadequate” showed the highest mean score in Corley’s study (32). Studies have shown that when, the nurses do not have enough time for providing patient care and cannot fulfill their professional duties due to the low number of staff, they feel exhausted, weak, and guilty (42, 43). Lack of sufficient nurses results in the nurses’ stress, burnout, job dissatisfaction, and physical as well as mental illness which all lead to absenteeism from work, high turnover, and low-quality care (15, 44). Moreover, delay in taking effective measures due to the physicians’ inability or their slow response in critical situations also results in the nurses’ moral distress (41).
The findings of the current study revealed a decreasing trend in the moral distress mean score in the intervention group, while there was an increasing trend in the control group after the intervention. Furthermore, a significant difference was observed in the moral distress mean score between the control and intervention groups and within the two groups over time, which shows the effectiveness of the educational interventions in reducing the rate of moral distress among the nurses under study. Corley’s scale consists of 3 domains of “Individual responsibility”, “Not in the patient’s best interest”, and “Deception” (32). The items which had the highest mean scores in Corley’s study are quite different from those showing the highest mean scores in the present study; the highest mean scores were related to the items of “Ignorance of the patient” domain in this study, while the items related to the “Patient’s decision making ability” showed the highest mean scores in Corley’s study (32). According to Merghati Khoei et al. (9), these differences result from socio-cultural variations in different nursing communities as well as the policies and regulations of the hospitals and the nurses’ working environment. He also mentions the necessity of a cultural focus on this issue in new studies.
One of the limitations of the present study was sampling from one hospital, which is, of course, the main Heart Disorders Center in Shiraz, and therefore the results cannot be generalized to all nurses. Another limitation of the study was its small sample size, which was due to the nurses’ working in rotational shifts as well as their high workload. Finally, researchers did not have adequate control over the exchange of information between the two groups as the study was conducted on both groups simultaneously.
Conclusion
Cardiac Care Unit nurses experience moral distress to a great extent which will increase in case no intervention is performed to tackle it. Educational interventions are necessary for identification and reduction of moral distress and ethical education can improve the adaptability strategies. In fact, Cardiac Care Unit nurses need to recognize moral distress in their working environment and be aware of its adverse effects on themselves as well as on patient care. Overall, each institute should identify and utilize the mechanisms of controlling moral distress (2, 8, 15). The “4A model” can be used for reducing moral distress, and committees can be established in hospitals in order for the nurses to discuss and solve their ethical dilemmas. Authors of this study recommend that more studies with larger sample sizes be conducted in different hospital wards in the future.
Acknowledgments
This article is the result of a research proposal approved by the Shiraz University of Medical Sciences and Health-Treatment Services numbered 6106-91. We would like to hereby express our gratitude to all patients and their families who assisted us in performing this proposal.
References
- 1.Kälvemark S, Höglund AT, Hansson MG, Westerholm P, Arnetz B. Living with conflicts-ethical dilemmas and moral distress in the health care system. Soc Sci Med. 2004;58(6):1075–84. doi: 10.1016/s0277-9536(03)00279-x. [DOI] [PubMed] [Google Scholar]
- 2.Gallagher A. Moral distress and moral courage in everyday nursing practice. Online J Issues Nurs. 2010;16(2) [PubMed] [Google Scholar]
- 3.Pauly B, Varcoe C, Storch J. Framing the issues: moral distress in health care. Hec Forum. 2012;24(1):1–11. doi: 10.1007/s10730-012-9176-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown K. The power of one: moral distress is common in critical care nursing. AACN News. 2003;20(3) [Google Scholar]
- 5.Wlody GS. Nursing management and organizational ethics in the intensive care unit. Criti Care Med. 2007;35(2):S29–S35. doi: 10.1097/01.CCM.0000252910.70311.66. [DOI] [PubMed] [Google Scholar]
- 6.McClendon H, Buckner EB. Distressing situations in the intensive care unit: a descriptive study of nurses’ responses. Dimens Crit Care Nurs. 2007;26(5):199–206. doi: 10.1097/01.DCC.0000286824.11861.74. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy J, Deady R. Moral distress reconsidered. Nurs Ethics. 2008;15(2):254–62. doi: 10.1177/0969733007086023. [DOI] [PubMed] [Google Scholar]
- 8.Huffman DM, Rittenmeyer L. How professional nurses working in hospital environments experience moral distress: a systematic review. Crit Care Nurs Clin North Am. 2012;24(1):91. doi: 10.1016/j.ccell.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Merghati Khoiee E, Alizadegan S, Motevallian SA, Goushegir SA, Ghoroubi J. Developing the moral distress scale in the population of Iranian nurses. Iranian J Psychiatr. 2008;3(2):55–8. [Google Scholar]
- 10.Pendry PS. Moral distress: recognizing it to retain nurses. Nurs Econ. 2007;25(4):217. [PubMed] [Google Scholar]
- 11.Elpern EH, Covert B, Kleinpell R. Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care. 2005;14(6):523–30. [PubMed] [Google Scholar]
- 12.Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit care med. 2007;35(2):422–9. doi: 10.1097/01.CCM.0000254722.50608.2D. [DOI] [PubMed] [Google Scholar]
- 13.Fry ST, Harvey RM, Hurley AC, Foley BJ. Development of a model of moral distress in military nursing. Nurs Ethics. 2002;9(4):373–87. doi: 10.1191/0969733002ne522oa. [DOI] [PubMed] [Google Scholar]
- 14.Corley MC. Nurse moral distress: a proposed theory and research agenda. Nurs Ethics. 2002;9(6):636–50. doi: 10.1191/0969733002ne557oa. [DOI] [PubMed] [Google Scholar]
- 15.Maluwa VM, Andre J, Ndebele P, Chilemba E. Moral distress in nursing practice in Malawi. Nurs Ethics. 2012;19(2):196–207. doi: 10.1177/0969733011414968. [DOI] [PubMed] [Google Scholar]
- 16.Beumer CM. Innovative solutions: the effect of a workshop on reducing the experience of moral distress in an intensive care unit setting. Dimens Crit Care Nurs. 2008;27(6):263–7. doi: 10.1097/01.DCC.0000338871.77658.03. [DOI] [PubMed] [Google Scholar]
- 17.Schluter J, Winch S, Holzhauser K, Henderson A. Nurses’ moral sensitivity and hospital ethical climate: a literature review. Nurs Ethics. 2008;15(3):304–21. doi: 10.1177/0969733007088357. [DOI] [PubMed] [Google Scholar]
- 18.McAndrew NS, Leske JS, Garcia A. Influence of moral distress on the professional practice environment during prognostic conflict in critical care. J Trauma Nurs. 2011;18(4):221–30. doi: 10.1097/JTN.0b013e31823a4a12. [DOI] [PubMed] [Google Scholar]
- 19.Hamric AB. Empirical research on moral distress: issues, challenges, and opportunities. Hec Forum. 2012;24(1):39–49. doi: 10.1007/s10730-012-9177-x. [DOI] [PubMed] [Google Scholar]
- 20.Harrowing JN, Mill J. Moral distress among Ugandan nurses providing HIV care: a critical ethnography. Int J Nurs Stud. 2010;47(6):723. doi: 10.1016/j.ijnurstu.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Hamric AB. Moral distress and nurse-physician relationships. Virtual Mentor. 2010;12(1):6. doi: 10.1001/virtualmentor.2010.12.1.ccas1-1001. [DOI] [PubMed] [Google Scholar]
- 22.Abbas A, Borhani F, Kalantari S. Moral distress in nurses of treatment centers,Bam,2011. Medical ethic. 2011;5(17):119–40. [in persion] [Google Scholar]
- 23.Joolaee S, Jalili HR, Rafii F, Hajibabaee F, Haghani H. Relationship between moral distress and job satisfaction among nurses of Tehran University of Medical Sciences Hospitals. Hayat. 2012;18(1):42–51. [in Persion] [Google Scholar]
- 24.Shakerinia I. Relationship between moral distress, psychological hardiness and occopational burnout in the nursing. Iranian J Med Ethics Hist Med. 2010;4:56–69. [in Persion] [Google Scholar]
- 25.Shoorideh FA, Ashktorab T, Yaghmaei F. Response of ICUs nurses to moral distress: a qualitative study. Iranian J Crit Care Nurs. 2012;4(4):159–68. [in Persion] [Google Scholar]
- 26.Hamric AB. Empirical research on moral distress: issues, challenges, and opportunities. Hec Forum. 2012;24(1):39–49. doi: 10.1007/s10730-012-9177-x. [DOI] [PubMed] [Google Scholar]
- 27.Rogers S, Babgi A, Gomez C. Educational interventions in end-of-life care: Part I: An educational intervention responding to the moral distress of NICU nurses provided by an ethics consultation team. Adv Neonat Care. 2008;8(1):56–65. doi: 10.1097/01.ANC.0000311017.02005.20. [DOI] [PubMed] [Google Scholar]
- 28.McCue C. Using the AACN framework to alleviate moral distress. Online J Issues Nurs. 2010;16(1) doi: 10.3912/OJIN.Vol16No01PPT02. [DOI] [PubMed] [Google Scholar]
- 29.McAndrew NS. Experiences of nurses and physicians when making end-of-life decisions in intensive care units. Clin Nurse Spec. 2010;24(4):215–6. doi: 10.1177/1054773814533791. [DOI] [PubMed] [Google Scholar]
- 30.Maiden J, Georges JM, Connelly CD. Moral distress, compassion fatigue, and perceptions about medication errors in certified critical care nurses. Dimens Crit Care Nurs. 2011;30(6):339–45. doi: 10.1097/DCC.0b013e31822fab2a. [DOI] [PubMed] [Google Scholar]
- 31.Corley MC. Moral distress of critical care nurses. Am J Crit Care. 1995;4(4):280–5. [PubMed] [Google Scholar]
- 32.Corley MC, Elswick RK, Gorman M, Clor T. Development and evaluation of a moral distress scale. J Adv Nurs. 2001;33(2):250–6. doi: 10.1046/j.1365-2648.2001.01658.x. [DOI] [PubMed] [Google Scholar]
- 33.Meltzer LS, Huckabay LM. Critical care nurses’ perceptions of futile care and its effect on burnout. Am J Crit Care. 2004;13(3):202–8. [PubMed] [Google Scholar]
- 34.Corley MC, Minick P, Elswick R, Jacobs M. Nurse moral distress and ethical work environment. Nurs Ethics. 2005;12(4):381–90. doi: 10.1191/0969733005ne809oa. [DOI] [PubMed] [Google Scholar]
- 35.Mobley MJ, Rady MY, Verheijde JL, Patel B, Larsona JS. The relationship between moral distress and perception of futile care in the critical care unit. Intensive Crit Care Nurs. 2007;23:256–63. doi: 10.1016/j.iccn.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 36.Jameton A. Dilemmas of moral distress: moral responsibility and nursing practice. AWHONNS Clin Issues Perinat Womens Health Nurs. 1993;4(4):542. [PubMed] [Google Scholar]
- 37.Wilkinson JM. Moral distress in nursing practice: experience and effect. Nurs Forum. 2007;23:16–29. [PubMed] [Google Scholar]
- 38.Storch J, Rodney P, Varcoe C, et al. Leadership for ethical policy and practice (LEPP): participatory action project. Can J Nurs Leadersh. 2009;22(3):68. doi: 10.12927/cjnl.2009.21155. [DOI] [PubMed] [Google Scholar]
- 39.Cronqvist A, Nyström M. A theoretical argumentation on the consequences of moral stress. J Nurs Manag. 2007;15(4):458–65. doi: 10.1111/j.1365-2834.2007.00764.x. [DOI] [PubMed] [Google Scholar]
- 40.Silén M, Tang PF, Ahlström G. Swedish and Chinese nurses’ conceptions of ethical problems: a comparative study. J Clin Nurs. 2009;18(10):1470–9. doi: 10.1111/j.1365-2702.2008.02422.x. [DOI] [PubMed] [Google Scholar]
- 41.Zuzelo PR. Exploring the moral distress of registered nurses. Nurs Ethics. 2007;14(3):344–59. doi: 10.1177/0969733007075870. [DOI] [PubMed] [Google Scholar]
- 42.Laschinger HKS, Leiter MP. The impact of nursing work environments on patient safety outcomes: the mediating role of burnout engagement. J Nurs Adm. 2006;36(5):259–67. doi: 10.1097/00005110-200605000-00019. [DOI] [PubMed] [Google Scholar]
- 43.Manojlovich M, Laschinger HKS. Application of the nursing worklife model to the ICU setting. Crit Care Nurs Clin North Am. 2008;20(4):481. doi: 10.1016/j.ccell.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 44.Ohnishi K, Ohgushi Y, Nakano M, et al. Moral distress experienced by psychiatric nurses in Japan. Nurs Ethics. 2010;17(6):726–40. doi: 10.1177/0969733010379178. [DOI] [PubMed] [Google Scholar]