Abstract
Objective
To determine whether alterations in diet and/or activity patterns during weekends contribute to weight gain or hinder weight loss.
Methods and Procedures
Randomized, controlled trial comparing 1 year of caloric restriction (CR) with 1 year of daily exercise (EX). Subjects included 48 healthy adults (30F, 18M) aged 50–60 years with BMI 23.5–29.9 kg/m2. Body weight was measured on 7 consecutive mornings for a total of 165 weeks at baseline and 437 weeks during the 1-year interventions. Daily weight changes were calculated for weekends (Friday to Monday) and weekdays (Monday to Friday). Daily energy intake was estimated using food diaries; daily physical activity was measured using accelerometers. Both measures were validated against doubly labeled water (DLW).
Results
At baseline, participants consistently gained weight on weekend days (+0.06 ± 0.03 kg/day, (mean ± s.e.), P = 0.02), but not on weekdays (−0.02 ± 0.02 kg/day, P = 0.18). This was attributable to higher dietary intake on Saturdays and lower physical activity on Sundays relative to weekdays (both P < 0.05). During the interventions, both CR and EX participants were in negative energy balance on weekdays (P < 0.005). On weekends, however, CR participants stopped losing weight, and EX participants gained weight (+0.08 ± 0.03 kg/day, P < 0.0001) due to higher dietary intakes on weekends. This helps to explain the slower-than-expected rate of weight loss during the interventions.
Discussion
Alterations in lifestyle behaviors on weekends contribute to weight gain or cessation of weight loss on weekends. These results provide one explanation for the relatively slow rates of weight loss observed in many studies, and the difficulty with maintaining significant weight loss.
INTRODUCTION
Daily fluctuations in body weight are common due to changes in hydration status, dietary intake, and daily physical activity patterns. For many adults, diet and activity patterns differ substantially on weekends as compared to weekdays, with potential consequences on body weight that could promote the development or maintenance of overweight and obesity if the pattern is repeated throughout the year. Dietary patterns and body weight have been shown to vary during the Thanksgiving weekend (1,2), the holiday period between Thanksgiving and early January (3), and between different seasons of the year (4), but little is known regarding the influence of weekends on short- and long-term body weight. The best evidence that weekend eating patterns influence weight control is based upon prospective data from 1,429 participants in the National Weight Control Registry who had successfully maintained a weight loss of at least 13.6 kg for an average of 7.9 ± 9.3 years (5). Participants who reported greater dieting consistency (i.e., maintaining the same diet regimen on weekends as on weekdays) were more likely to maintain their weight within 2.3 kg during the subsequent year, whereas participants with lower dieting consistency scores were more likely to regain weight during the subsequent year. Therefore, in addition to contributing to the development of obesity, high dietary intake on weekends relative to weekdays may hinder weight loss and contribute to weight regain following weight loss.
Although the National Weight Control Registry study (5) was prospective and involved a large sample size, the body weights were self-reported on only two occasions (at the beginning and end of the year). Numerous studies have involved measurements of body weight longitudinally under carefully controlled conditions, but we are not aware of any studies in which weights were measured daily in the free-living environment over a long period of time, leaving the question of a potential weekend effect unanswered. Furthermore, if there is indeed a propensity for weight gain during the weekends, it is important to determine whether dietary intake is primarily responsible, or if physical activity patterns also play a critical role.
The purpose of this analysis was first to assess daily body weight changes during weekends and weekdays, both before and during weight loss interventions, and second to determine whether changes in dietary intake and/or physical activity on weekends were responsible for any observed weight changes. We hypothesized that weight gain would occur during the weekends at baseline, but that this effect would be blunted during the intervention.
METHODS AND PROCEDURES
Participants
Healthy adults between 50 and 60 years of age with a BMI between 23.5 and 29.9 kg/m2 were recruited from the St. Louis metropolitan area to participate in the National Institutes of Health (NIH)-funded CALERIE study (Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy), as described previously (6). Participants were nonsmokers and did not exercise regularly; all women were postmenopausal. The study was approved by the Washington University School of Medicine Human Studies Committee and the General Clinical Research Center Scientific Advisory Committee. Written, informed consent was obtained from each participant before enrollment.
Study design
Eligible participants were randomly assigned to 1 year of a calorie-restricted (CR) diet, a comparable energy deficit induced by daily exercise (EX), or a healthy lifestyle (HL) control group in a 2:2:1 randomization scheme, as described in detail previously (6). Briefly, the goal of the CR and EX interventions was to induce a comparable energy deficit of 16% during the first 3 months, and 20% during the subsequent 9 months, so that the physiological effects of weight loss induced by CR vs. exercise could be compared. The CR group was instructed to modify their daily energy intake without changing their physical activity patterns, whereas the EX group was instructed to increase their daily physical activity energy expenditure without changing their dietary intake. The diet and exercise prescriptions were individualized based upon baseline total energy expenditure (TEE) as determined using doubly labeled water (DLW) (7). HL participants did not receive a diet or exercise prescription and served as a control group.
Body weight
Body weight was measured at the participant’s home each morning for 2–4 weeks at baseline and for 2 weeks at each assessment time point throughout the year-long intervention (i.e., months 1, 3, 6, 9, and 12). Measurements were taken in kilograms on the LifeSource UC-321 Precision Personal Health Scale (A&D Medical, Milpitas, CA), which has a 31-weight memory function. Participants weighed themselves unclothed in the fasted state after voiding, and recorded their weight on log sheets which they turned in with the scale at the end of each recording period. Weight changes were calculated for weekends (Friday to Monday), weekdays (Monday to Friday), and for each day individually. In order to assess the validity of the home weights, participants were weighed on a calibrated clinic scale on several days for which home weights were recorded. The clinic weights were measured in duplicate by research staff in the morning, with the participant fasted and wearing only a hospital gown.
Anthropometrics and body composition
Height was measured to the nearest 0.1 cm. BMI was calculated as weight/height2 (kg/m2). Body composition was assessed using dual-energy X-ray absorptiometry (Delphi W, software version 11.2; Hologic, Waltham, MA) on three occasions at baseline and twice at each subsequent time point (i.e., months 1, 3, 6, 9, and 12). The results were expressed as an average at each time point.
Energy intake
Seven-day food diaries were used to estimate self-reported energy intake at baseline and at months 1, 3, 6, 9, and 12 during the intervention. Participants received detailed instructions on how to weigh, measure, and record all food and beverages consumed. Research dietitians reviewed the diaries with participants and then analyzed them using Nutrition Data System for Research (software versions 4.05, 4.06 and 5.0; Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN).
Physical activity energy expenditure
Daily physical activity was estimated using RT3 triaxial accelerometers (Stayhealthy, Monrovia, CA), which participants were instructed to wear on the hip during all waking hours for 2 to 4 weeks at baseline and for 2 weeks at months 1, 3, 6, 9, and 12. The accelerometers were set to mode 4 with a vector magnitude of 1 min to capture minute-by-minute activity counts, which were used to generate physical activity energy expenditure (i.e., activity above resting values, expressed in kcal/d) using the manufacturer’s proprietary formula and participant-specific values for sex, age, height, and weight. Accelerometer data were used only for days on which weight was recorded, and for which at least 720 min (i.e., 12 h) of accelerometer activity data were recorded. Data were excluded for days on which physical activity energy expenditure was <100 kcal or >4,000 kcal, due to the implausibility of these values.
Validity measures
To assess the validity of the self-reported food diary data and the accelerometer-derived physical activity data, we compared these outcomes with objectively determined energy intake and physical activity based upon the DLW method (7). TEE was assessed with DLW during 2-week periods at baseline and during 2-week periods at each subsequent time point (i.e., months 1, 3, 6, 9, and 12), as described previously (6). Two baseline urine samples were collected, after which an oral dose of DLW was administered (0.20 g H2 18O and 0.12 g 2H2O per kg of total body water), and postdose urine samples were collected at 4.5 h, 6 h, 7 days (two samples), and 14 days (two samples). Samples were analyzed by isotope ratio mass spectrometry at Pennington Biomedical Research Center (8). Energy intake was calculated as TEE plus changes in body energy stores measured by dual-energy X-ray absorptiometry. Physical activity was calculated by subtracting resting metabolic rate and the thermic effect of food from TEE. Resting metabolic rate was measured by indirect calorimetry using a DeltaTrac II Metabolic Monitor (SensorMedics, Yorba Linda, CA) in the morning in the fasted state after the participant spent the evening in the General Clinical Research Center; thermic effect of food was estimated to be 10% of TEE.
Statistical analyses
Analyses were performed using SAS software, version 9.1.3 of the SAS System for Linux (SAS Institute, Cary, NC). The primary analysis was a comparison of average weight changes during weekends vs. weekdays using generalized estimating equation models to account for the correlation of multiple measurements within each participant. Least squares means from the generalized estimating equation model were used to determine whether there were significant changes in weight during weekends and during weekdays. Secondary analyses included comparisons of weekend and weekday self-reported energy intake and accelerometer-based physical activity using generalized estimating equation analysis. Subsequent generalized estimating equation models included daily values with specific contrasts comparing each weekend day to the average weekday value. Due to skewed data distributions and the presence of outliers, energy intake and physical activity data during the intervention were analyzed using rank-transformed data. Pearson correlation coefficients (r) were calculated to assess the degree of agreement between self-reported and objectively determined energy intake, and between accelerometer-based physical activity and physical activity determined using DLW. Statistical tests were two-tailed, with significance accepted at P < 0.05. Data are presented as means ± s.e., except in Figure 3a,b, in which the median and interquartile ranges are presented.
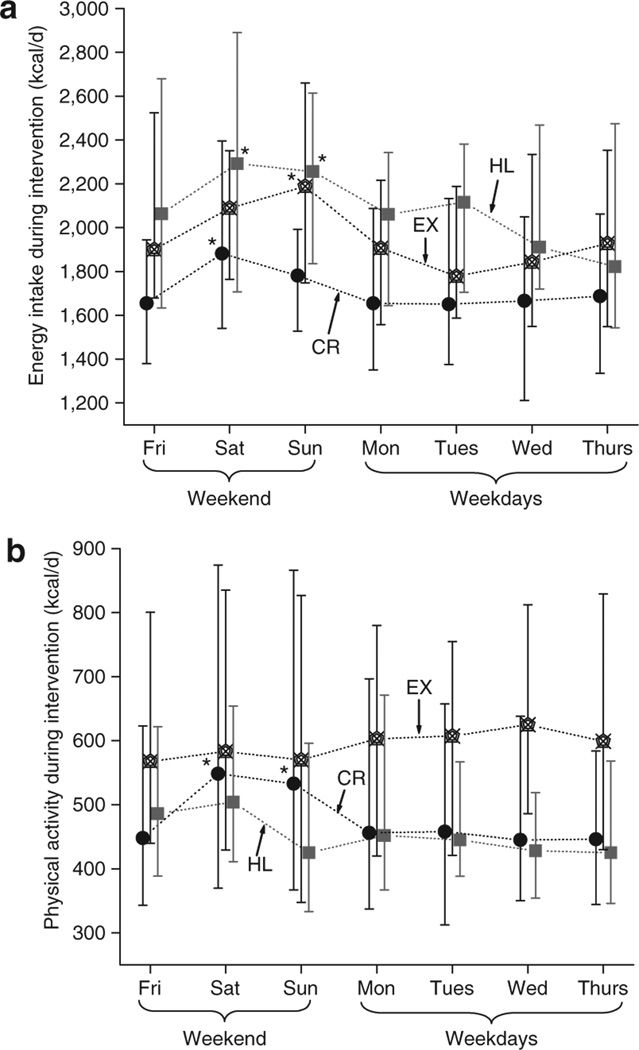
Figure 3.
(a) Daily energy intake and (b) physical activity during the 1-year interventions. Symbols represent median values and interquartile ranges for the caloric restriction (CR) group (filled circles), exercise (EX) group (hexagons), and healthy lifestyle (HL) group (filled squares). *P < 0.05 vs. median weekday value.
RESULTS
Forty-eight adults (30 women, 18 men) began the intervention, with 19 in the CR group, 19 in the EX group, and 10 in the HL group. At baseline, the mean age was 57 ± 1 years, and BMI was 27.3 ± 0.3 kg/m2, with the majority of participants overweight (39 ± 1% fat mass in females; 25 ± 1% fat mass in males). Forty-six participants (96%) completed 1 year, with weight changes of −8.0 ± 0.9 kg in the CR group, −6.4 ± 0.9 kg in the EX group, and −1.3 ± 0.9 kg in the HL group, as reported previously (6).
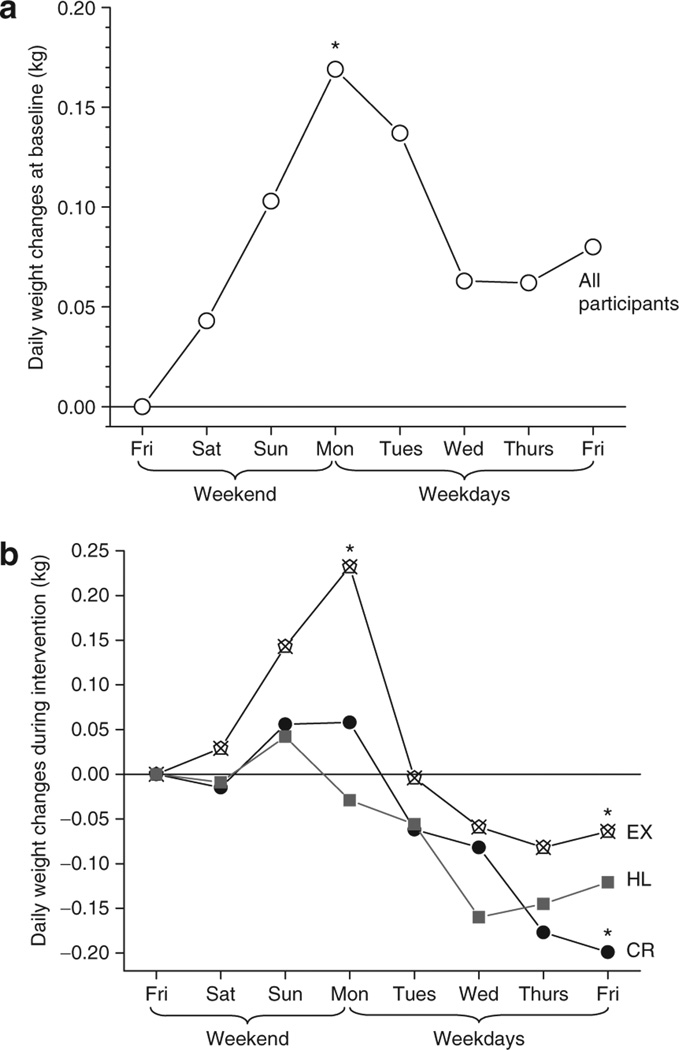
Daily weight changes
During the baseline period, daily weights were available for 45 participants, who contributed a total of 1,156 days, or 165 weeks of data. During the 1-year intervention, 47 participants contributed a total of 3,064 daily weights, or 437 weeks (177 weeks in the CR group, 176 weeks in EX, and 84 weeks in HL). As shown in Figure 1a, body weight at baseline increased significantly during the weekend days (+0.06 ± 0.03 kg/day, P = 0.02, all participants combined), with a nonsignificant trend downward on weekdays (−0.02 ± 0.02 kg/day, P = 0.18). This difference between weekend and weekday weight changes was significant (P = 0.04), resulting in a net increase of 0.077 kg per week.
Figure 1.
(a) Daily weight changes at baseline and (b) during the 1-year interventions. Symbols represent the mean for all participants (open circles, n = 48), caloric restriction (CR) group (filled circles, n = 18), exercise (EX) group (hexagons, n = 18) and healthy lifestyle (HL) control group (filled squares, n = 10). *P = 0.02 for daily weight change on weekends at baseline; *P < 0.005 for weight change on weekends or weekdays during the intervention year.
During the 1-year intervention, a weekend effect was still evident (Figure 1b). As prescribed, the CR and EX participants were in negative energy balance during the weekdays (CR: −0.07 ± 0.02 kg/day, P < 0.001; EX: −0.08 ± 0.02 kg/day, P = 0.004). During the weekends, however, CR participants stopped losing weight (+0.02 ± 0.02 kg/day, P = 0.38), whereas EX participants gained weight (+0.08 ± 0.03 kg, P < 0.0001). The HL control group did not have significant weight changes on weekends (−0.01 ± 0.00 kg/day, P = 0.94) or weekdays (−0.02 ± 0.03 kg/day, P = 0.23).
On 598 occasions, participants’ body weights were measured on the clinic scale on the same day that they weighed themselves at home on their study scales. Intraclass correlation coefficients between the home scale weights and the clinic scale weights were 0.99 at baseline and for each time point during the intervention.
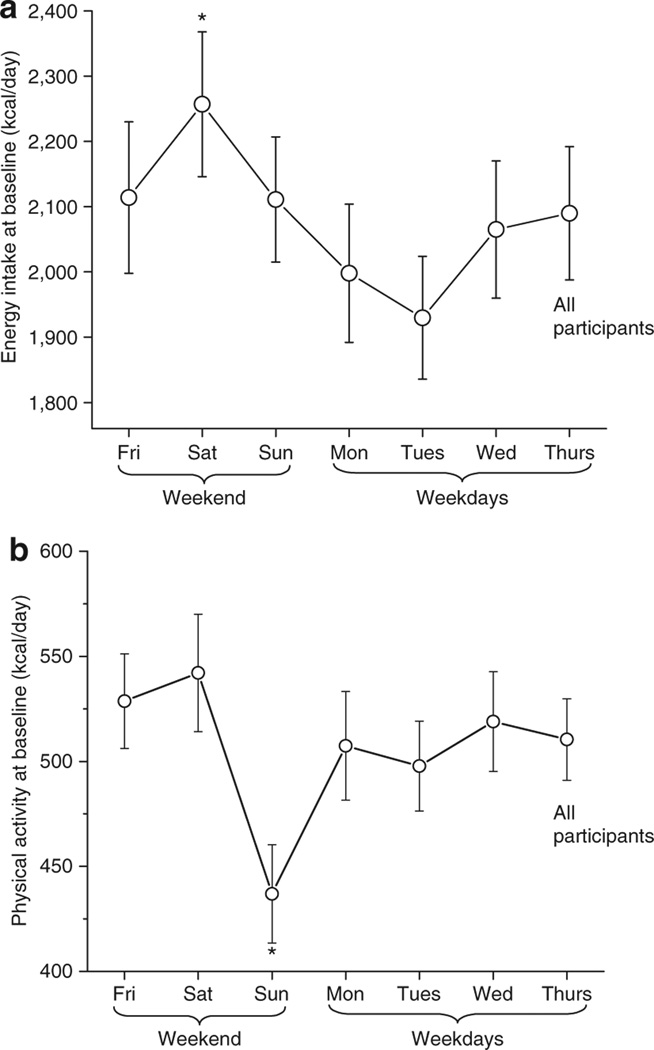
Energy intake
At baseline, energy intake was highest on Saturdays (Figure 2a), with the average Saturday intake (2,257 ± 111 kcal/d) significantly greater than the average intake during the weekdays (2,021 kcal/d; P = 0.03 Saturday vs. weekdays). The higher energy intake on weekends was attributable to greater consumption of fat (36.5% of total kcal on weekends vs. 34.7% on weekdays, P = 0.05), and relative but not absolute reductions in the consumption of carbohydrate (46.7% vs. 48.8%, P = 0.04) and protein (15.7% vs. 16.5%, P = 0.02). Sodium intake did not differ significantly between weekends (3,605 mg) and weekdays (3,345 mg, P = 0.24).
Figure 2.
(a) Daily energy intake and (b) physical activity at baseline. Symbols represent mean values ± s.e.m. for all participants. *P < 0.05 vs. mean weekday value.
During the 1-year intervention, energy intake for all 3 study groups was significantly higher on weekends as compared to weekdays (Figure 3a). In the CR group, energy intake on Saturday exceeded the weekday average (P = 0.001); EX participants had higher intakes on both Saturday (P = 0.035) and Sunday (P = 0.012) as compared to weekdays, whereas the HL group ate more on Sundays relative to weekdays (P = 0.04). The correlation between self-reported energy intake and objectively determined energy intake was 0.58 (P < 0.0001) at baseline. During the intervention, the correlations within each group were: CR group r = 0.67, P < 0.0001; EX group r = 0.60, P < 0.0001; HL group r = 0.49, P = 0.009.
Physical activity
Of the 3,653 days of accelerometer records that coincided with daily weight measurements, 24% were excluded for insufficient data (i.e., <720 min), with no difference between weekends and weekdays. Subjects wore the accelerometers for an average of 1,003 ± 172 min each weekend day and 1,018 ± 159 min each weekday (P = 0.36), for an average of 20.4 days at baseline and 11.2 days at the subsequent time points, with no differences between groups.
At baseline, physical activity was lowest on Sundays and highest on Saturdays (Figure 2b), with Sunday’s activity significantly lower than the average weekday activity (P = 0.010 Sunday vs. weekdays), and a trend for Saturday’s activity to be higher than the average weekday activity (P = 0.082). Due to these opposite trends on Saturdays and Sundays, the average weekend physical activity did not differ significantly from the average weekday activity (P = 0.24). During the intervention (Figure 3b), physical activity was greater on weekends than weekdays for the CR group (P = 0.040), due to higher activity on Saturdays (P = 0.045) and Sundays (P = 0.041) relative to weekdays. The EX group did not display different activity patterns on weekends relative to weekdays (P = 0.56), whereas a trend for higher activity on weekends was observed in the HL group (P = 0.06). The correlation between accelerometer-derived physical activity and physical activity determined from DLW was 0.53 (P = 0.0005) at baseline. During the intervention, the correlations within each group were: CR group r = 0.49, P < 0.0001; EX group r = 0.57, P < 0.0001; HL group r = 0.49, P = 0.005.
DISCUSSION
This is the first study to demonstrate that weight gain occurs during weekend days relative to weekdays, and that this effect is attributable predominantly to higher energy intake during weekends. Before the interventions began, the consistent and significant increase in body weight from Friday through Monday morning was due to both higher dietary intake and lower physical activity on weekends relative to weekdays, and the resultant weekly weight gain was 0.077 kg. Although small on a weekly basis, this rate of weight gain could result in an annual increase of 4.0 kg, or almost 9 lb, if it continued in a similar pattern throughout the year. However, the anticipation of beginning a long-term CR or exercise intervention may have contributed to overeating during the baseline period in the present study, as the annual rate of weight gain generally is <1 kg/year (9–11). During the year-long interventions, the CR group stopped losing weight on weekends and the exercise group gained weight, which was solely attributable to higher dietary intake on weekends.
Given the large increase in the prevalence of obesity throughout the past two decades, it is important to understand the influence that weekend lifestyle patterns have on long-term weight control. The main finding of the present study was that weekend dietary indulgences contribute to weight gain or cessation of weight loss. These data are consistent with those of Gorin et al. (5) from the National Weight Control Registry, which indicate that people whose diets were less consistent between weekdays and weekends were more likely to gain weight during the subsequent year. Our observation that the extra weekend calories were attributable to increases in dietary fat are consistent with data from the 1994–1996 Continuing Survey of Food Intakes by Individuals (12).
Our accelerometer results at baseline reveal low physical activity levels on Sundays, which support the pedometer-based findings of Clemes et al. (13), in which there was a significant reduction in steps on Sundays among overweight adults. Interestingly, physical activity levels during the weight loss interventions were consistent or even higher on weekends relative to weekdays. Taken together, our results support the importance of maintaining consistent dietary and physical activity patterns throughout the week to avoid unwanted weight gain and to facilitate consistent weight loss.
Despite the strengths of the present analysis, including the correlations between our main outcome measures (i.e., home weights, self-reported dietary intake, and accelerometer-based physical activity) and more validated methodology (i.e., clinic weights, and DLW assessments of energy intake and expenditure, which incorporate dual-energy X-ray absorptiometry-determined changes in body composition), there are limitations. First, we cannot determine with certainty what proportion of the weekend weight increase was attributable to higher dietary intake or lower physical activity relative to weekdays, as the accuracy of self-reported dietary intake is variable between individuals (14–16), and the accelerometers may not be sensitive enough to detect small day-to-day differences in physical activity (17,18). However, the food diaries were kept for 1 week, and the accelerometers were worn for nearly 2 weeks at each assessment time point, thereby minimizing intra-subject variability. Another limitation is that participants contributed differentially to the data, with some participants missing data at a follow-up time point and therefore being underrepresented relative to participants with data at all study time points. By design, the control group was smaller than the intervention groups, which may explain why they did not display the weekend weight effect during the year-long study that was observed among the whole sample at baseline. Despite these limitations, the large number of days included in these analyses and the statistical controls used should have minimized sampling biases.
In summary, our results demonstrate the adverse effect of weekend lifestyle behaviors on daily body weight, and indicate that higher dietary intake on weekends is the greatest contributor to weekend weight gain or cessation of weight loss, with physical activity playing a smaller role. This information has important implications from a public health perspective and in clinical trials when the rate of weight loss may not be as great as expected.
ACKNOWLEDGMENTS
We are grateful to the study participants for their cooperation, the staff of the Applied Physiology Laboratory at Washington University School of Medicine for their skilled assistance, Manjushri Bhapkar of Duke Clinical Research Institute for analyzing the accelerometer data, and James P. DeLany at the Pennington Biomedical Research Center for the doubly labeled water analyses. This research was supported by the NIH Cooperative Agreement 5-U01-AG20487, Clinical Nutrition Research Unit Grant DK56341, and General Clinical Research Center Grant RR00036. E.P.W. was supported by Institutional National Research Service Award AG00078. The manuscript was written by S.B.R. and edited by S.B.R., E.P.W., K.B.S., K.S.-M., D.T.V., and J.O.H.; data collection was performed by S.B.R., E.P.W., D.T.V., and K.O.; data analyses and interpretation were performed by K.S.-M, K.B.S, S.B.R., and E.P.W.; the overall study was designed by J.O.H.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.Klesges RC, Klem ML, Bene CR. Effects of dietary restraint, obesity, and gender on holiday eating behavior and weight gain. J Abnorm Psychol. 1989;98:499–503. doi: 10.1037//0021-843x.98.4.499. [DOI] [PubMed] [Google Scholar]
- 2.Hull HR, Radley D, Dinger MK, Fields DA. The effect of the Thanksgiving holiday on weight gain. Nutr J. 2006;5:29. doi: 10.1186/1475-2891-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yanovski JA, Yanovski SZ, Sovik KN, et al. A prospective study of holiday weight gain. N Engl J Med. 2000;342:861–867. doi: 10.1056/NEJM200003233421206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma Y, Olendzki BC, Li W, et al. Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr. 2006;60:519–528. doi: 10.1038/sj.ejcn.1602346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorin AA, Phelan S, Wing RR, Hill JO. Promoting long-term weight control: does dieting consistency matter? Int J Obes Relat Metab Disord. 2004;28:278–281. doi: 10.1038/sj.ijo.0802550. [DOI] [PubMed] [Google Scholar]
- 6.Racette SB, Weiss EP, Villareal DT, et al. One year of caloric restriction in humans: feasibility and effects on body composition and abdominal adipose tissue. J Gerontol A Biol Sci Med Sci. 2006;61:943–950. doi: 10.1093/gerona/61.9.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schoeller DA. Measurement of energy expenditure in free-living humans by using doubly labeled water. J Nutr. 1988;118:1278–1289. doi: 10.1093/jn/118.11.1278. [DOI] [PubMed] [Google Scholar]
- 8.DeLany JP, Schoeller DA, Hoyt RW, Askew EW, Sharp MA. Field use of D2 18O to measure energy expenditure of soldiers at different energy intakes. J Appl Physiol. 1989;67:1922–1929. doi: 10.1152/jappl.1989.67.5.1922. [DOI] [PubMed] [Google Scholar]
- 9.Lewis CE, Jacobs DR, Jr, McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151:1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 10.Quatromoni PA, Pencina M, Cobain MR, Jacques PF, D’Agostino RB. Dietary quality predicts adult weight gain: findings from the Framingham Offspring Study. Obesity (Silver Spring) 2006;14:1383–1391. doi: 10.1038/oby.2006.157. [DOI] [PubMed] [Google Scholar]
- 11.Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM. The influence of smoking cessation on the prevalence of overweight in the United States. N Engl J Med. 1995;333:1165–1170. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- 12.Haines PS, Hama MY, Guilkey DK, Popkin BM. Weekend eating in the United States is linked with greater energy, fat, alcohol intake. Obes Res. 2003;11:945–949. doi: 10.1038/oby.2003.130. [DOI] [PubMed] [Google Scholar]
- 13.Clemes SA, Griffiths PL, Hamilton SL. Four-week pedometer-determined activity patterns in normal weight and overweight UK adults. Int J Obes (Lond) 2007;31:261–266. doi: 10.1038/sj.ijo.0803420. [DOI] [PubMed] [Google Scholar]
- 14.Schoeller DA. Limitations in the assessment of dietary energy intake by self-report. Metabolism. 1995;44:18–22. doi: 10.1016/0026-0495(95)90204-x. [DOI] [PubMed] [Google Scholar]
- 15.Schoeller DA, Bandini LG, Dietz WH. Inaccuracies in self-reported intake identified by comparison with the doubly labelled water method. Can J Physiol Pharmacol. 1990;68:941–949. doi: 10.1139/y90-143. [DOI] [PubMed] [Google Scholar]
- 16.Bandini LG, Schoeller DA, Cyr HN, Dietz WH. Validity of reported energy intake in obese and nonobese adolescents. Am J Clin Nutr. 1990;52:421–425. doi: 10.1093/ajcn/52.3.421. [DOI] [PubMed] [Google Scholar]
- 17.Crouter SE, Churilla JR, Bassett DR., Jr Estimating energy expenditure using accelerometers. Eur J Appl Physiol. 2006;98:601–612. doi: 10.1007/s00421-006-0307-5. [DOI] [PubMed] [Google Scholar]
- 18.Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35:867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]